Back to Journals » International Journal of General Medicine » Volume 16
Post-Acute Care for Traumatic Brain Injury Patients in Taiwan
Authors Huang HC, Bih LI, Tsai MM, Chang TL, Liao WC, Lai CL
Received 22 February 2023
Accepted for publication 20 April 2023
Published 4 May 2023 Volume 2023:16 Pages 1653—1659
DOI https://doi.org/10.2147/IJGM.S407532
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Hsing-Ching Huang,1,* Liu-Ing Bih,1,* Ming-Miau Tsai,1 Tzu-Ling Chang,1 Wan-Chun Liao,1 Chung-Liang Lai2
1Department of Physical Medicine and Rehabilitation, Taichung Hospital, Ministry of Health and Welfare, Taichung, Taiwan; 2Department of Occupational Therapy, Asia University, Taichung, Taiwan
*These authors contributed equally to this work
Correspondence: Chung-Liang Lai, Department of Occupational Therapy, Asia University, 500, Lioufeng Rd., Wufeng, Taichung 41354, Taiwan, Email [email protected]
Background: Traumatic brain injury (TBI) can result in functional impairments. Many patients with TBI require post-acute care to improve their functional skills and allow for greater self-independence and a better quality of life. Taiwan’s National Health Insurance proposed a nationwide post-acute care program in 2017 for patients with traumatic brain injury. The program’s goal was to maximize patients’ functional recovery and make it possible for them to return to their homes and communities. This study aimed to explore the effectiveness of such programs in Taiwan.
Methods: This pilot study retrospectively evaluated a de-identified database that contained the scores of various assessments evaluated at admission and discharge. It used the data to determine the functional improvement of patients with traumatic brain injury after participating in post-acute care programs.
Results: This study collected complete data from 27 patients. After an average of 45.11 days in the program, the patients showed significant improvement in the Barthel Activity Daily Living Index, the Lawton–Brody Instrumental Activity Daily Living Scale, the Mini Nutrition Assessment, the EuroQol Five Dimensions Questionnaire, the Berg Balance Scale, the Galveston Orientation and Amnesia Test, the Rancho Los Amigos Scale, the Concise Chinese Aphasia Test, and the Mini Mental State Examination. After discharge, 96% of the patients could return to their community.
Conclusion: This pilot study concluded that the program significantly promoted functional recovery for patients and could help patients with traumatic brain injury return to their communities and reduce the risk of institutionalization. Thus, patients with the potential for functional recovery could receive post-acute care in regional or community hospitals immediately after being discharged from acute wards. In the future randomized controlled trials are needed to further confirm the clinical impact of this program.
Keywords: traumatic brain injury, rehabilitation, post-acute care
Introduction
Traumatic brain injury (TBI) is one of the leading causes of health loss and disability around the world. TBI is mainly caused by injuries from falls and car accidents. The incidence of TBI is likely to continue to increase over time due to the increase in population density, the aging population, and the use of automobiles, motorcycles, and bicycles.1 The estimated incidence of TBI per year globally is 27 to 69 million,2 and the incidence in Taiwan is 52,000 per year. TBI may result in severe life-long cognitive, physical, and behavioral impairments that require long-term healthcare and disability assistance services.3 Rehabilitation is an effective treatment for patients with TBI, as it can reduce TBI-related morbidity and increase the possibility for patients to return to work. Many studies have proven that acute rehabilitation can improve the prognosis of patients with TBI.4
Taiwan’s National Health Insurance (NHI) proposed a post-acute care (PAC) program in 2017 for traumatic brain injury patients. The objectives of this program are to maximize functional recovery, reduce disability, improve quality of life, and enable patients to return to their homes and communities. In this program, patients with TBI who have rehabilitation potential and are willing to undergo rehabilitation are referred from the acute ward to the rehabilitation ward of a regional or community hospital to receive post-acute care and rehabilitation. In order to implement a vertically integrated healthcare system, patients need to achieve a stable state in the acute ward of a medical center, undergo an initial assessment, and then be referred to a regional or community hospital to participate in the TBI PAC program. It is expected that this integrated and continuous care model can help patients restore functions and reduce disability. Although the PAC program has existed since 2017, no studies have probed into the therapeutic effectiveness of PAC programs for TBI patients in Taiwan. This study explored the improvement of function and quality of life for patients with traumatic brain injury through participating in PAC programs by comparing the scores of various assessments evaluated at admission and discharge. We hypothesized that TBI patients who received this PAC program would have functional recovery and a better quality of life.
Methods
Subjects
This study analyzed the de-identified data of patients enrolled in the PAC program of a regional hospital in central Taiwan. To be included in the PAC program, the patients needed to: 1) be greater than or equal to 20 years old; 2) be within 60 days of suffering a traumatic brain injury; 3) have significant and persistent moderate function impairment, defined as having a Barthel index score ranging from 40 to 70; 4) have a stable medication condition; and 5) have the potential for functional recovery after rehabilitation. The stable medication conditions were: 1) a stable neurological condition that had not deteriorated for more than 72 hours after the patients had recovered from nerve injury shock; 2) stable vital signs for the past 72 hours, including blood pressure, heart rate, body temperature, respiration rate, and blood oxygen saturation; and 3) complications, such as deep vein embolism or pulmonary embolism, autonomic dysreflexia, blood pressure and heartbeat instability, infection, blood abnormalities, decubitus ulcers, seizures, hydrocephalus, convulsions, gastrointestinal bleeding, or adynamic ileus, had been stable or controllable. The potential for functional recovery after rehabilitation should be followed by the principles which included: 1) having basic cognition, learning ability, and intention; 2) having the sufficient physical strength to maintain a sitting posture with the support of a wheelchair or bed edge for at least one hour; 3) having achievable treatment goals; and 4) having the ability to actively participate in the rehabilitation program. The discharge regulations of the PAC program were based on the patients meeting any of the following conditions: 1) functional improvement and the ability to receive rehabilitation in the community; 2) a hospital stay longer than 12 weeks; 3) self-discontinuation of the program; 4) the inability to continue the program due to disease progression.
This study complies with the Declaration of Helsinki. All TBI patients signed an informed consent before enrolling in the PAC program, and this informed consent included the permission to use anonymized medical data for research. This study was approved by the Institutional Review Board of Ministry of Health and Welfare, Tasotun Psychiatric Center (No. 111040), which was the same hospital alliance with first author’s hospital and in charge of IRB work for first author’s hospital and listed at www.chictr.org.cn under registration number ChiCTR2300067864.
Study Design
This retrospective cohort study mainly analyzed the de-identified data containing the scores of various assessments evaluated at admission and discharge, which were used to determine the functional improvement of patients in the PAC programs. According to the NHI’s rules for the PAC program, all TBI patients received comprehensive post-acute care in a hospital by a multidisciplinary team consisting of physiatrists, nurses, physical therapists, occupational therapists, speech therapists, case managers, dietitians, pharmacists, and social workers. All TBI patients in the PAC program received daily 1.5- to 3-hour-long intensive rehabilitation programs that included physical therapy, occupational therapy, and speech therapy. The multidisciplinary team summoned regular weekly meetings to report the initial, interim, and final evaluations of the patients and discuss the treatment goals, plans, and effectiveness, as well as create a discharge plan.
The patients’ basic information included records on gender, age, brain injury mechanism, onset time and length of stay. Functional recovery, improvement of quality of life, and effectiveness of rehabilitation were assessed by comparing differences between the admission and discharge outcome scales. The outcome scales were assessed at admission, every three weeks and at discharge by members of a multidisciplinary team (Figure 1).
 |
Figure 1 Flow diagram of healthcare pathway. Abbreviation: PAC, post-acute care. |
The outcome scales included the Barthel Activity Daily Living Index (B-ADL, scored from 0–100, with a higher score indicating better performance, represent the severity of ADL function);5 the Lawton–Brody Instrumental Activity Daily Living scale (LB-IADL, scored from 0–8, with a higher score indicating better performance);6 the EuroQol Five Dimensions Questionnaire (EQ-5D, scored from 1–3, with a lower score indicating better performance);7 the Mini Nutrition Assessment (MNA, scored from 0–30, with a higher score indicating better performance);8 the Berg Balance Scale (BBS, scored from 0–56, with a higher score indicating better performance);9 the Mini Mental State Examination (MMSE, scored from 0–30, with a higher score indicating better performance);10 the Galveston orientation and amnesia test (GOAT, scored from 0–100 with a higher score indicating better performance);11 the Rancho Los Amigos Scale (RLAS, scored from 1–10, with a higher score indicating better performance, represent the severity of cognitive function);12 and the Concise Chinese Aphasia Test (CCAT, scored from 1–12, with a higher score indicating better performance).13
Statistical Analysis
All data were collected and analyzed retrospectively. All statistical analyses and procedures were performed using SPSS WIN version 18. The descriptive statistics included the percentage, mean, and standard deviation. This study used a paired t-test to compare the functional status and quality of life before and after the PAC program, and P <0.05 was defined as the level of statistical significance in the two-tailed analysis.
Results
A total of 30 participants were admitted to the hospital and participated in the PAC program. Most of them were referred from the acute wards of two medical centers in Taiwan. Three patients discontinued the PAC program: one had hydrocephalus and was transferred to the neurosurgery ward for a surgical intervention, one had a severe intra-abdominal infection with septic shock and was transferred to the acute ward, and one presented with hearing impairment and was transferred to the otorhinolaryngology ward for surgical management. Therefore, 27 patients completed the PAC program and all evaluations.
The basic information about the patients is presented in Table 1. The mean patient age was 55.8 ± 17.42 years. Fourteen patients (42.4%) were men, and 13 patients (39.4%) were women. A total of 18 patients (54.5%) were injured in traffic accidents, and 9 patients (27.3%) were injured by falls. The average number of days post-injury at admission was 30.81 ± 14.06 days. The mean length of stay in the PAC hospital was 45.11 ± 21.09 days.
 |
Table 1 Baseline Data of the Patients |
With the comparison between the outcomes of this program and the initial values, Table 2 shows the Mean ± SD of each outcome scale score of the patients with TBI at admission and discharge. There were significant improvements in the B-ADL, LB-IADL, EQ-5D (self-care, usual activities, and anxiety/depression), MNA, BBS, MMSE, GOAT, RLAS, and CCAT (P <0.05). There was no significant improvement in the EQ-5D (mobility and pain/discomfort) only.
 |
Table 2 Outcome Scores at Admission and Discharge and Effect of Functional Performance and Quality of Life in Patients with TBI |
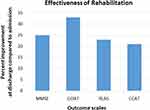
Figure 2 compares the progress in the cognitive and language functions of the patients with TBI before and after receiving the PAC programs. The results showed that the improvements in the GOAT, MNA, RLAS, and CCAT all exceeded 20%.
After completing the PAC programs, most of the patients (96%) returned to the community and continued rehabilitation, either at home (n = 15, 55.6%) or in an outpatient clinic (n = 11, 40.7%) and only one patient went to the long-term care institution (Table 3).
 |
Table 3 Post-PAC Disposition |
Discussion
TBI may cause physical dysfunction and cognitive impairments that affect patients’ quality of life. TBI also imposes an economic burden on society. It is estimated to cost USD 60 billion per year in the United States.14–16 Therefore, how to maximize the functional recovery of TBI patients and reduce the medical and economic burden are important issues around the world. The mean age of the patients with TBI in this study was 55.81 years old, and the patients participated in the PAC program for a mean of 45.11 days. After receiving the PAC programs, the patients showed significant improvements in the functional outcome scales, including the B-ADL, LB-IADL, EQ-5D (self-care, usual activities, and anxiety/depression), MNA, BBS, MMSE, GOAT, RLAS, and CCAT. The results demonstrated that after the patients with TBI completed the PAC programs, they had significant improvements in their activities of daily living, quality of life, nutritional state, balance ability, cognitive functions, and language functions. The results of this study were consistent with the hypotheses. Moreover, most of the patients could successfully return to their homes and communities after being discharged from the hospital. Similar results have been obtained in many past studies, where the patients with TBI significantly improved several functions, reduced their dependence, and increased the possibility of returning to community life after receiving post-acute rehabilitation.17,18 Although progress was made in the EQ-5D scores for mobility, pain and discomfort, the difference was not significant in this study. Based on the results of these subjective assessment scales, this study discovered the importance of pain and discomfort issues for patients with TBI and the patients’ high expectations for the recovery of their original mobility.
The PAC program in this study provided the patients with TBI with comprehensive multidisciplinary team-based healthcare services to improve the quality of care and therapeutic effect. A previous study showed that many current guidelines strongly recommend the implementation of comprehensive multidisciplinary treatment for TBI.19 The use of a multidisciplinary approach to implement rehabilitation programs can more effectively treat patients with TBI.4,20,21 This PAC program emphasized that patients with TBI in acute wards would be directly referred to rehabilitation wards in regional or community hospitals to receive comprehensive rehabilitation treatment as soon as possible after their medical condition was stable, if they met the inclusion criteria according to the assessment of the medical centers. Moreover, according to the program requirements, the time since the onset of TBI needed to be less than 60 days. As a result, the PAC program allowed the patients to receive rehabilitation treatment as soon as possible, thereby reducing the length of time in disability and gaining significant progress. Past research has indicated that patients who participate in post-acute rehabilitation within three months after injury make significant functional progress. In addition, early intervention can maximize the reduction of functional limitations.17 Another study showed that the implementation of rehabilitation within the first year after TBI can achieve the best rehabilitation effect, while greatly reducing medical costs.4
This PAC program provided the patients with TBI with high-intensity rehabilitation treatment. The frequency of rehabilitation was 1.5–3 hours per day, five days per week. Previous studies have indicated that compared with low-intensity rehabilitation, early intervention using high-intensity rehabilitation can accelerate the functional recovery of patients and increase the opportunity for patients to return to the workplace.22 TBI can cause many cognitive impairments, including attention, information processing speed, memory, executive function, and communication.23 The results in this study showed significant improvement in the GOAT, MNA, RLAS, and CCAT scores after the patients with TBI completed the PAC program, suggesting the patients had significant improvements in cognitive and language functions. Depression is the most common psychiatric illness in patients with TBI, with an incidence of 10%-70%.24 One study indicated that compared with TBI patients without depression symptoms, the quality of life, health status, and psychosocial function of TBI patients with depression symptoms are poorer.25 Past research has also showed that exercise training can effectively reduce the depression of patients with TBI.25,26 This study found significant improvements in the scores for anxiety and depression in the EQ-5D for the patients with TBI participating in the PAC program.
This study performed a retrospective analysis on samples collected from only one hospital. Some studies have suggested that geographic variations may affect the implementation of PAC programs.27 Therefore, the research results cannot represent the overall effectiveness of all TBI PAC programs in Taiwan. Moreover, there was a higher proportion of younger subjects (<65 years old) in the patients with TBI enrolled in this study. As a result, better outcomes may have been obtained compared with those found in the older population. This study excluded TBI patients with severe dysfunction (Barthel index score <40) in the acute phase. However, some of these patients may have rehabilitation potential. Prospective studies are suggested in the future to randomize patients into participating groups and non-participating groups of the PAC program to further confirm the effectiveness and clinical impact of the PAC program.
Conclusion
This study concluded that the TBI PAC program significantly promoted functional recovery for patients in Taiwan, helped them return to their communities, and reduced the risk of institutionalization. Thus, TBI patients with the potential for functional recovery could receive PAC in regional or community hospitals immediately after being discharged from acute wards. In the future randomized controlled trials are needed to further confirm the clinical impact of this program.
Acknowledgments
This study was supported by the PAC team of Taichung Hospital, Ministry of Health, and Welfare.
Disclosure
The authors report no conflicts of interest in this work.
References
1. GBD 2016 Traumatic Brain Injury and Spinal Cord Injury Collaborators. Global, regional, and national burden of traumatic brain injury and spinal cord injury, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016 [published correction appears in Lancet Neurol. 2021 Dec;20(12):e7]. Lancet Neurol. 2019;18(1):56–87. doi:10.1016/S1474-4422(18)30415-0
2. Dewan MC, Rattani A, Gupta S, et al. Estimating the global incidence of traumatic brain injury [published online ahead of print, 2018 Apr 1]. J Neurosurg. 2018;130:1–18.
3. Shi HY, Hwang SL, Lee IC, Chen IT, Lee KT, Lin CL. Trends and outcome predictors after traumatic brain injury surgery: a nationwide population-based study in Taiwan. J Neurosurg. 2014;121(6):1323–1330. doi:10.3171/2014.8.JNS131526
4. Griesbach GS, Kreber LA, Harrington D, Ashley MJ. Post-acute traumatic brain injury rehabilitation: effects on outcome measures and life care costs. J Neurotrauma. 2015;32(10):704–711. doi:10.1089/neu.2014.3754
5. Mahoney FI, Barthel DW. Functional evaluation: the Barthel index. Md State Med J. 1965;14:61–65.
6. Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9(3):179–186. doi:10.1093/geront/9.3_Part_1.179
7. EuroQol Group. EuroQol--a new facility for the measurement of health-related quality of life. Health Policy. 1990;16(3):199–208. doi:10.1016/0168-8510(90)90421-9
8. Rubenstein LZ, Harker JO, Salvà A, Guigoz Y, Vellas B. Screening for undernutrition in geriatric practice: developing the short-form mini-nutritional assessment (MNA-SF). J Gerontol Biol Sci Med Sci. 2001;56(6):M366–M372. doi:10.1093/gerona/56.6.M366
9. Maeda N, Kato J, Shimada T. Predicting the probability for fall incidence in stroke patients using the Berg Balance Scale. J Int Med Res. 2009;37(3):697–704. doi:10.1177/147323000903700313
10. Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–198. doi:10.1016/0022-3956(75)90026-6
11. Levin HS, O’Donnell VM, Grossman RG. The Galveston Orientation and Amnesia Test. A practical scale to assess cognition after head injury. J Nerv Ment Dis. 1979;167(11):675–684. doi:10.1097/00005053-197911000-00004
12. Flannery J, Abraham I. Psychometric properties of a cognitive functioning scale for patients with traumatic brain injury. West J Nurs Res. 1993;15(4):465–482. doi:10.1177/019394599301500406
13. Chung YM, Lee SE, Chang MH, Hsu TC. The concise Chinese aphasia test and its application. J Speech Lang Hearing Assoc. 1998;13:119–137.
14. Roozenbeek B, Maas AI, Menon DK. Changing patterns in the epidemiology of traumatic brain injury. Nat Rev Neurol. 2013;9(4):231–236. doi:10.1038/nrneurol.2013.22
15. Bruns J, Hauser WA. The epidemiology of traumatic brain injury: a review. Epilepsia. 2003;44(s10):2–10. doi:10.1046/j.1528-1157.44.s10.3.x
16. Khan F, Baguley IJ, Cameron ID. 4: rehabilitation after traumatic brain injury. Med J Aust. 2003;178(6):290–295. doi:10.5694/j.1326-5377.2003.tb05199.x
17. Hayden ME, Plenger P, Bison K, Kowalske K, Masel B, Qualls D. Treatment effect versus pretreatment recovery in persons with traumatic brain injury: a study regarding the effectiveness of postacute rehabilitation. PM R. 2013;5(4):319–327. doi:10.1016/j.pmrj.2012.12.005
18. Rosenbaum AM, Gordon WA, Joannou A, Berman BA. Functional outcomes following post-acute rehabilitation for moderate-to-severe traumatic brain injury. Brain Inj. 2018;32(7):907–914. doi:10.1080/02699052.2018.1469040
19. Lee SY, Amatya B, Judson R, et al. Clinical practice guidelines for rehabilitation in traumatic brain injury: a critical appraisal. Brain Inj. 2019;33(10):1263–1271. doi:10.1080/02699052.2019.1641747
20. Sander AM, Constantinidou F. The interdisciplinary team. J Head Trauma Rehabil. 2008;23(5):271–272. doi:10.1097/01.HTR.0000336839.68585.0f
21. Ashley MJ. Repairing the injured brain: why proper rehabilitation is essential to recovering function. Cerebrum. 2012;2012:8.
22. Zhu XL, Poon WS, Chan CC, Chan SS. Does intensive rehabilitation improve the functional outcome of patients with traumatic brain injury (TBI)? A randomized controlled trial. Brain Inj. 2007;21(7):681–690. doi:10.1080/02699050701468941
23. Nowell C, Downing M, Bragge P, Ponsford J. Current practice of cognitive rehabilitation following traumatic brain injury: an international survey. Neuropsychol Rehabil. 2020;30(10):1976–1995. doi:10.1080/09602011.2019.1623823
24. Bryant RA, O’Donnell ML, Creamer M, McFarlane AC, Clark CR, Silove D. The psychiatric sequelae of traumatic injury. Am J Psychiatry. 2010;167(3):312–320. doi:10.1176/appi.ajp.2009.09050617
25. Perry SA, Coetzer R, Saville CWN. The effectiveness of physical exercise as an intervention to reduce depressive symptoms following traumatic brain injury: a meta-analysis and systematic review. Neuropsychol Rehabil. 2020;30(3):564–578. doi:10.1080/09602011.2018.1469417
26. Peppel LD, Ribbers GM, Heijenbrok-Kal MH. Pharmacological and non-pharmacological interventions for depression after moderate-to-severe traumatic brain injury: a systematic review and meta-analysis. J Neurotrauma. 2020;37(14):1587–1596. doi:10.1089/neu.2019.6735
27. Oyesanya TO, Moran TP, Espinoza TR, Wright DW. Regional variations in rehabilitation outcomes of adult patients with traumatic brain injury: a uniform data system for medical rehabilitation investigation. Arch Phys Med Rehabil. 2021;102(1):68–75. doi:10.1016/j.apmr.2020.07.011
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.