Back to Journals » Local and Regional Anesthesia » Volume 15
Positioning the Catheter Tip Anterior or Posterior to the Saphenous Nerve in Continuous Adductor Canal Block: A Mono-Centric Retrospective Comparative Study
Authors Coviello A , Bernasconi A , Balato G, Spasari E, Ianniello M, Mariconda M, Vargas M, Iacovazzo C, Smeraglia F, Tognù A, Servillo G
Received 10 August 2022
Accepted for publication 9 December 2022
Published 29 December 2022 Volume 2022:15 Pages 97—105
DOI https://doi.org/10.2147/LRA.S383601
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Stefan Wirz
Antonio Coviello,1 Alessio Bernasconi,2 Giovanni Balato,2 Ezio Spasari,1 Marilena Ianniello,1 Massimo Mariconda,2 Maria Vargas,1 Carmine Iacovazzo,1 Francesco Smeraglia,2 Andrea Tognù,3 Giuseppe Servillo1
1Department of Neurosciences, Reproductive and Odontostomatological Sciences, University of Naples “Federico II”, Naples, 80100, Italy; 2Department of Public Health, School of Medicine, University of Naples “Federico II”, Unit of Orthopedics and Traumatology, Naples, Italy; 3Department of Anesthesiology and Intensive Care Medicine, Istituto Ortopedico Rizzoli IRCCS, Bologna, 40136, Italy
Correspondence: Antonio Coviello, Department of Neurosciences, Reproductive and Odontostomatological Sciences, University of Naples “Federico II”, Via Vitruvio, 3, Naples, 80100, Italy, Email [email protected]
Background and Aim: Ultrasound-guided continuous adductor canal block (cACB) is a conventional choice in patients undergoing total knee arthroplasty (TKA) for the management of the postoperative pain. This study aims to compare different catheter tip locations for cACB relative to the saphenous nerve (anteriorly vs posteriorly) in terms of efficacy and complications.
Methods: At the department of Surgical Sciences, Orthopedic Trauma and Emergencies of the University of Naples Federico II (Naples, Italy), between January 2020 and November 2021, retrospective comparative study was executed. Patients planned for TKA were included in the study if they met the follow inclusion criteria: patients undergone TKA; aged 50– 85 years; body mass index (BMI) of 18– 35 kg/m2; American Society of Anesthesiologists (ASA) physical status classification from I to III; subarachnoid technique for anesthesiology plane; continuous adductor canal block performed by an anesthetist with considerable experience. Patients were assigned to receive cACB with the catheter tip located anteriorly (Group 1, G1) or posteriorly to the saphenous nerve (Group 2, G2). Postoperative pain, ambulation ability, episodes of pump block and rate of catheter dislodgement and leakage were evaluated and analyzed.
Results: Altogether, 102 patients were admitted to the study (48 in G1 and 54 in G2). After the first 8 postoperative hours, in G1 17 patients (35.4%) had a VAS greater than 4, while in group 2 only 3 patients (5.6%) had a VAS greater than 4 (p-value < 0.01). All patients of both groups showed ambulation ability in the postoperative period. No episode of leakage was recorded. While the catheter displacement rate was similar in the two groups (2.1% for G1 vs 3.7% for G2; p-value > 0.05), the episodes of pump block were significantly less in G2 than in G1 (3.7% vs 20.8%; p-value < 0.01).
Conclusion: In cACB for TKA, we found that positioning the catheter tip posteriorly to the saphenous nerve may lead to a greater postoperative analgesia and reduce the risk of pump block compared to placing the catheter tip anteriorly to the nerve.
Keywords: continuous adductor canal block, catheter displacement, catheter location, saphenous nerve, total knee arthroplasty
Introduction
Nowadays, total knee arthroplasty (TKA) is recognized as gold standard for end-stage osteoarthritis treatment.1,2 Multiple studies have suggested that over 60% of patients undergone TKA may experience from moderate to severe pain immediately after surgery,3–6 which in turn may limit early mobilization and recovery of the knee function while increasing the risk of adverse effects related to being bed-bound.7–9 Considering that the number of TKAs in progressively increasing worldwide, it becomes crucial to implement anesthesiologic strategies for the control of postoperative pain.10
Among different techniques, ultrasound guided Adductor Canal Block (ACB) has emerged as an effective procedure to relieve postoperative pain after knee surgery.11–13 Compared with common methods, such as epidural and intravenous analgesia, ACB can provide a satisfactory control of pain and reduce opioid use. As compared to a femoral nerve block, ACB allows to spare the quadriceps motor function, helping anticipate the rehabilitation of the patient.14–17 Additionally, the possibility to perform a continuous adductor canal block (cACB) with delivery of the local anesthetic for 24–48 hours after surgery is a further advantage of this technique to ensure optimal pain control for a longer period.18–20 While the effectiveness of the cACB block positioned at different levels in the adductor canal has been investigated by many authors, to the best of our knowledge none of them has evaluated its efficacy in relation to the anatomical closeness of the tip of the catheter to the saphenous nerve and to the femoral artery.
With this background, we performed a retrospective study aiming to compare two different catheter tip locations in relation to the saphenous nerve for cACB technique, ie, anteriorly or posteriorly to the nerve. We hypothesized that an anterior positioning might be less effective in terms of pain control and carry a higher incidence rate of pump block due to the tension of the deep fascia and subsequent compression of the tip of the catheter.
Material and Methods
This was a Level III mono-centric retrospective comparative study performed at the Department of Surgical Sciences, Orthopedic Trauma and Emergencies of the University of Naples Federico II (Naples, Italy). The study protocol was approved by the ethical committee of the University of Naples Federico II. Patient consent was not required (as confirmed by the ethical committee) because of the retrospective nature of the study and the use of data collected in daily clinical practice. All data regarding patients were handled as confidential by the authors of the study. The design of this study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement. All procedures performed in the study were in accordance with the ethical standards as laid down in the Declaration of Helsinki (1964) and its later amendments or comparable ethical standards.
Data about patients who underwent TKA between January 2020 and November 2021 were recovered from our departmental archive. All data, using MS Office Excel 2007 (Microsoft, Redmond, WA, USA), were registered on a pre-filled form and stored in a computerized database.
Inclusion Criteria
- Patients undergone TKA;
- Aged 50–85 years;
- Body mass index (BMI) of 18–35 kg/m2;
- American Society of Anesthesiologists (ASA) physical status classification of I to III;
- Subarachnoid technique for anesthesiology plane;
- Continuous adductor canal block performed by an anesthetist with considerable experience. We considered an anesthetist with considerable experience who had at least 5 years of experience with loco-regional anesthesia as main operator and an average of over 100 procedures per year.
- Patients whose medical charts are fully accessible.
Exclusion Criteria
- Contraindications to subarachnoid technique;
- Failure to perform the pre-operative mobilization test;
- Neurologic defects in the block site;
- Surgical procedures longer than 3 hours;
- Patients in whom the treatment protocol could not be fully applied.
Study Population
In the timeframe highlighted, 120 patients (120 knees) underwent TKA.12 cases with surgical procedures longer than 3 hours, 2 cases with neurologic defects in the block site and 4 cases of failure to perform the pre-operative mobilization test were excluded, 102 patients were included in the study.
Interventions
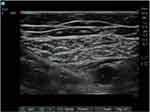
The cACB was performed immediately after surgery in a dedicated room, while vital signs were monitoring. Ultrasound (US) transducer (Sonosite HLF38x 13–6 MHz, Fujifilm Sonosite Europe, Amsterdam, Netherlands) was used for scanning the medial aspect of the thigh in a transverse axial plane. The femoral artery was identified underneath the sartorius muscle using the color Doppler in the proximal third of the thigh, then the transducer was moved caudally along the long axis of the thigh. At the beginning of the adductor canal, the needle entry point was marked on the skin. The femoral vein was then found in a lower position and the saphenous nerve, as a hyper-echoic structure with a round cross-section, was lateral to the artery. A needle (Vygon Value Life, Italy) 18-Gauge 30° tip with a split cannula 85-mm long was inserted through the sartorius muscle, along the same anatomical plane from lateral-to-medial orientation of the transducer. The procedure was performed with real-time ultrasound guidance toward the targeted nerve. A 20-gauge Silverstim (Vygon Value Life, Italy) echogenic and stimulating catheter was inserted 2–3 cm beyond the tip through a split cannula anteriorly or posteriorly to the nerve after the administration of 20 mL of 0.5% ropivacaine in all patients under US guidance.
A before-and-after study was performed. A correct placement of the catheter tip was obtained by retracting the catheter slowly while injecting 5-mL of a saline solution under US-guidance. Tegaderm chlorhexidine gluconate transparent securement dressing protects catheter site and secures devices to the skin.
At the end of the procedure, postoperative analgesia was initiated through intermittent bolus PIB/PCA (programmed intermittent bolus/patient-controlled analgesia) pump with boluses of Ropivacaine 0,2% (6 mL per hour) and rescue bolus (5 mL per hours, with 60 minutes of lock-out time).
Data Extraction
Demographic patients data (age, sex, BMI), postoperative pain every 8 hours after surgery measured with Visual Analog Scale (VAS) (scale 0–10, where 0 = no pain and 10 = worst imaginable pain), ambulation ability, pump block and the rate of catheter dislodgement and leakage were detected from medical charts (Figure 1).
 |
Figure 1 Flowchart. |
Statistical Analysis
Patients were divided into two groups based on the position of the catheter tip relative to the saphenous nerve, ie, Group 1 (G1) if the tip was anterior (Figure 2) and Group 2 (G2) if the tip was posterior (Figure 3) to the nerve. The chi-square test was used to compare the groups with respect to categorical variables. A Student’s t-test was used to compare continuous variables as mean and standard deviation for the patients in both groups. Statistical significance was set with a p-value of 0.05. A post-hoc analysis was run considering the proportion of patient with VAS > 4 points as main outcome of the study. The statistical analysis was carried out using the IBM SPSS software (version 20.0, IBM Corporation, New York, USA).
Results
Overall, 48 patients (48 knees) were included in G1 and 54 patients (54 knees) in G2. The two groups were comparable in terms of demographics except for the BMI which was higher in G2 compared to G1 (26.5 vs 29.4; p-value <0.01) (Table 1). Ambulation ability, while analgesia was performed with continuous adductor canal catheter, occurred in all patients of both groups in the postoperative period (Table 2). Analgesia was optimal in the first 8 hours for all patients of both groups; in fact, all patients reported a VAS of zero. After the first 8 postoperative hours in Group 1, 17 patients (35.4%) had a VAS greater than 4, while in group 2 only 3 patients (5.6%) had a VAS greater than 4 (p-value <0.01) (Table 3). The episodes of pump block were significantly less in G2 than in G1 (3.7% vs 20.8%; p-value <0.01). On the other hand, the catheter displacement rate was similar in the two groups (2.1% for G1 vs 3.7% for G2; p-value >0.05). No episode of leakage was recorded. The post-hoc analysis (proportion G1: 0.36 vs proportion G2: 0.05; α = 0.05) detected that a total sample of 102 (ratio: 0.85) patients led to a power (1-β) of 0.99, which was considered satisfactory.
 |
Table 1 Characteristics of Patients |
 |
Table 2 Outcomes |
 |
Table 3 VAS After Surgery |
Discussion
In this study, we found that in cACB for TKA the position of the catheter tip relative to the saphenous nerve played a role in terms of efficacy and incidence of complication for the block. As a matter of fact, the catheter tip posterior to the nerve led to a better postoperative analgesia and a reduced risk of episodes of pump block compared to catheter tip anterior location. As far as we know, this is the first study to assess and compare the outcome of cACB based on different positions of the tip of the catheter around the saphenous nerve.
Postoperative pain management is always and no matter what the challenge. An adequate analgesia facilitates early rehabilitation and reduces postoperative incidence of complication.21,22 Dong et al managed a meta-analysis regarding analgesic regimen after TKA, and they concluded that continuous Femoral Nerve Block (cFNB) was the most effective analgesia method.23 However, FNB was also associated with weakness of the quadriceps muscle, which delayed ambulation and therefore slowed down the whole rehabilitation phase.24,25 On the other side, the ACB was a technique widely applied as a postoperative analgesic treatment in patients undergoing TKA, defining a purely sensory block.26,27 ACB is considered as a more appropriate analgesic method for patients undergoing TKA compared to FNB because it confers better ambulation ability. Moreover, it is well accepted by both anesthetist and orthopedic surgeon.28,29 Furthermore, in a recent meta-analysis, Chen et al confirmed that cACB was the most effective method for alleviating pain and promoting ambulation ability in patients after TKA. These results suggest that postoperative analgesia for patients undergoing TKA should always have a longtime effect.30 The ACB can provide reliable sensory blockade in the innervation saphenous nerve area. In addition, it has variable effects on the sensory components of the knee, in fact, extension of this block by diffusion to other nerves like the peroneal and tibial nerves or even femoral nerve has been described in the literature. An injection into the distal part of the adductor canal would spread alongside the femoral artery and vein through the adductor hiatus and into the popliteal fossa, thereby reaching the popliteal plexus and the genicular branch of the posterior obturator nerve.31 None of our patients had pain in the back of the knee after 20 mL of anaesthetic mixture bolus.32
From a technical standpoint, when performing the in-plane technique, the needle tip must always be in real-time ultrasound vision.33–35 Before positioning the perineural catheter, the injection of an anesthetic mixture bolus and the subsequent spread of liquid within the targeted fascial plane allowed to get a separation of the two fasciae of the compartment, hence the catheter positioning was easier.36,37 Catheter displacement is common in continuous peripheral nerve blocks, and improper positioning of the distal tip of catheters may occur frequently.38 We believe that the low incidence of postoperative catheter displacement in our cohort was related to the technique adopted. Regardless of its position around the saphenous nerve, the catheter was always inserted more laterally into the adductor canal so that at least 3–4 cm of it were placed between the two fasciae of the compartment which contributed to keep it more stable in its position. Furthermore, the catheter through split cannula method allowed to advance more easily the catheter 2–3 cm beyond the same cannula and to retract it in real-time ultrasound vision versus the target nerve,39 which in turn reduced the risk of secondary displacement.
Before 2020, in our department cACB was always performed placing the catheter tip in a sub sartorial position, anterior to the saphenous nerve. In our experience, this often led to episodes of pump block with mandatory/automatic bolus, which we thought being secondary to an increased tension of the upper fascia of the adductor canal.40 These cases prompted us to reflect upon the positioning of the catheter, hence we decided to perform cACB by positioning the catheter tip posterior to the saphenous nerve and a before-and-after study was performed. The study involves evaluating the effects of an intervention comparing the previous outcomes with those measured afterwards.41 In our clinical context, although bolus pumps had been used for a long time instead of continuous infusion pumps, there was still a high incidence of pumps block especially in the adductor canal. This prompted us to look for a more adequate position of the catheter tip with respect to the saphenous nerve. In fact, we thought that the sub sartorial fascia by closing obstructed the catheter tip anteriorly to the saphenous nerve and this prompted us to position it posteriorly to the nerve.
Our study has some limitations. Firstly, the retrospective design of the study, with risk of bias based on the interpretation of results. Secondly, the small number of patients included. Even if no power analysis was led at the beginning of the study, we believe that the lack of previous comparative analysis investigating the outcome after cACB taking into account the position of the catheter tip and the saphenous nerve increases the value of our results. We advocate further prospective and comparative studies to confirm or disprove our findings. Thirdly, the two groups differed by BMI, which theoretically might affect our findings as well. However, based on previous literature, we would have expected a worse outcome in G2 (with a higher BMI), therefore we deduced that this variable likely played a negligible role in the comparison of the two groups.
Conclusion
In cACB for TKA, we found that positioning the catheter tip anterior to the saphenous nerve may lead to a greater postoperative analgesia and reduce the risk of pump block compared to placing the catheter tip posterior to the nerve. We encourage further studies on this subject in order to define which variables might influence the success and complication rate of cACB in the setting of lower limb surgery.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Acknowledgements
The authors would like to thank the reviewer, Anna Onza, for the effort and the time spent in the linguistic revision of the manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosure
The authors declare no competing interests in this work.
References
1. Price AJ, Alvand A, Troelsen A, et al. Knee replacement. Lancet. 2018;392(10158):1672–1682. PMID: 30496082.2018. doi:10.1016/S0140-6736(18)32344-4
2. Popescu R, Haritinian EG, Cristea S. Relevance of finite element in total knee arthroplasty - literature review. Chirurgia. 2019;114:437–442. doi:10.21614/chirurgia.114.4.437
3. Parvizi J, Miller AG, Gandhi K. Multimodal pain management after total joint arthroplasty. J Bone Joint Surg Am. 2011;93:1075–1084. doi:10.2106/JBJS.J.01095
4. Husted H, Lunn TH, Troelsen A, et al. Why still in hospital after fast-track Hip and knee arthroplasty? Acta Orthop. 2011;82:679–684. doi:10.3109/17453674.2011.636682
5. Sardana V, Burzynski JM, Scuderi GR. Adductor canal block or local infiltrate analgesia for pain control after total knee arthroplasty? A systematic review and meta-analysis of randomized controlled trials. J Arthroplasty. 2019;34:183–189. doi:10.1016/j.arth.2018.09.083
6. Wu CL, Richman JM. Postoperative pain and quality of recovery. Curr Opin Anaesthesiol. 2020;17(5):455–460. PMID: 17023905. doi:10.1097/00001503-200410000-00017
7. Liu SS, Buvanendran A, Rathmell JP, et al. A cross-sectional survey on prevalence and risk factors for persistent postsurgical pain 1 year after total Hip and knee replacement. Region Anesth Pain Med. 2012;37:415–422. doi:10.1097/AAP.0b013e318251b688
8. Lindberg MF, Miaskowski C, RustoEn T, et al. Factors that can predict pain with walking, 12 months after total knee arthroplasty. Acta Orthop. 2016;87:600–606. doi:10.1080/17453674.2016.1237440
9. Lindberg MF, Rustoen T, Miaskowski C, et al. The relationship between pain with walking and self-rated health 12 months following total knee arthroplasty: a longitudinal study. BMC Musculosk Disord. 2017;18:75. doi:10.1186/s12891-017-1430-7
10. Puolakka PA, Rorarius MG, Roviola M, Puolakka TJ, Nordhausen K, Lindgren L. Persistent pain following knee arthroplasty. Eur J Anaesthesiol. 2010;27(5):455–460. PMID: 20299989. doi:10.1097/EJA.0b013e328335b31c
11. Hanson NA, Allen CJ, Hostetter LS, et al. Continuous ultrasound-guided adductor canal block for total knee arthroplasty: a randomized, double-blind trial. Anesth Analg. 2014;118:1370–1377. doi:10.1213/ANE.0000000000000197
12. Kim MK, Moon HY, Ryu CG, et al. The analgesic efficacy of the continuous adductor canal block compared to continuous intravenous fentanyl infusion with a single-shot adductor canal block in total knee arthroplasty: a randomized controlled trial. Korean J Pain. 2019;32:30–38. doi:10.3344/kjp.2019.32.1.30
13. Tao Y, Mao Q, Wang J. Continuous versus single shot adductor canal block for postoperative pain relief after total knee arthroplasty: a protocol for randomized controlled trial. Medicine. 2022;99(17):e19918. doi:10.1097/MD.0000000000019918
14. Koh IJ, Choi YJ, Kim MS, et al. Femoral nerve block versus adductor canal block for analgesia after total knee arthroplasty. Knee Surg Related Res. 2017;29:87–95. doi:10.5792/ksrr.16.039
15. Li D, Ma GG. Analgesic efficacy and quadriceps strength of adductor canal block versus femoral nerve block following total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2016;24(8):2614–2619. PMID: 26611901. doi:10.1007/s00167-015-3874-3
16. Rousseau-Saine N, Williams SR, Girard F, et al. The effect of adductor canal block on knee extensor muscle strength 6 weeks after total knee arthroplasty: a randomized, controlled trial. Anesth Analg. 2018;126(3):1019–1027. PMID: 28799964. doi:10.1213/ANE.0000000000002338
17. Thobhani S, Scalercio L, Elliott CE, et al. Novel regional techniques for total knee arthroplasty promote reduced hospital length of stay: an analysis of 106 patients. Ochsner J. 2017;17(3):233–238. PMID: 29026354; PMCID: PMC5625980. doi:10.1097/ALN.0b013e3182475c35
18. Canbek U, Akgun U, Aydogan NH, Kilinc CY, Uysal AI. Continuous adductor canal block following total knee arthroplasty provides a better analgesia compared to single shot: a prospective randomized controlled trial. Acta Orthop Traumatol Turc. 2019;53(5):334–339. doi:10.1016/j.aott.2019.04.001
19. Yu R, Wang H, Zhuo Y, Liu D, Wu C, Zhang Y. Continuous adductor canal block provides better performance after total knee arthroplasty compared with the single-shot adductor canal block?: an updated meta-analysis of randomized controlled trials. Medicine. 2020;99(43):e22762. PMID: 33120783; PMCID: PMC7581050. doi:10.1097/MD.0000000000022762
20. Sun C, Zhang X, Song F, et al. Is continuous catheter adductor canal block better than single-shot canal adductor canal block in primary total knee arthroplasty?: a GRADE analysis of the evidence through a systematic review and meta-analysis. Medicine. 2020;99(20):e20320. doi:10.1097/MD.0000000000020320
21. Dong CC, Dong SL, He FC. Comparison of adductor canal block and femoral nerve block for postoperative pain in total knee arthroplasty: a systematic review. J Clin Anesth. 2016;95:e2983.
22. Goyal N, McKenzie J, Sharkey PF, Parvizi J, Hozack WJ, Austin MS. The 2012 Chitranjan Ranawat award: intraarticular analgesia after TKA reduces pain: a randomized, double-blinded, placebo-controlled, prospective study. Clin Orthop Relat Res. 2013;471:64–75. doi:10.1007/s11999-012-2596-9
23. Dong P, Tang X, Cheng R, Wang J. Comparison of the efficacy of different analgesia treatments for total knee arthroplasty: a network meta-analysis. Clin J Pain. 2018;34:1047–1060. doi:10.1097/AJP.0000000000000631
24. Salinas FV, Liu SS, Mulroy MF. The effect of single-injection femoral nerve block versus continuous femoral nerve block after total knee arthroplasty on hospital length of stay and long-term functional recovery within an established clinical pathway. Anesth Analg. 2006;102:1234–1239. doi:10.1213/01.ane.0000198675.20279.81
25. Elkassabany NM, Antosh S, Ahmed M, et al. The risk of falls after total knee arthroplasty with the use of a femoral nerve block versus an adductor canal block: a double-blinded randomized controlled study. Anesth Analg. 2016;122:1696–1703. doi:10.1213/ANE.0000000000001237
26. Basques BA, Tetreault MW, Della Valle CJ. Same-day discharge compared with inpatient hospitalization following Hip and knee arthroplasty. J Bone Joint Surg Am. 2017;99:1969–1977. doi:10.2106/JBJS.16.00739
27. Essving P, Axelsson K, Kjellberg J, Wallgren O, Gupta A, Lundin A. Reduced morphine consumption and pain intensity with local infiltration analgesia (LIA) following total knee arthroplasty. Acta Orthop. 2010;81:354–360. doi:10.3109/17453674.2010.487241
28. Zhao X-Q, Jiang N, Yuan -F-F, Wang L, Yu B. The comparison of adductor canal block with femoral nerve block following total knee arthroplasty: a systematic review with meta-analysis. J Anesthesia. 2016;30(5):745–754. doi:10.1007/s00540-016-2194-1
29. Webb CA, Mariano ER. Best multimodal analgesic protocol for total knee arthroplasty. Pain Manag. 2015;5:185–196. doi:10.2217/pmt.15.8
30. Chen J, Zhou C, Ma C, et al. Which is the best analgesia treatment for total knee arthroplasty: adductor canal block, periarticular infiltration, or liposomal bupivacaine? A network meta-analysis. J Clin Anesth. 2021;68:110098. PMID: 33129063. doi:10.1016/j.jclinane.2020.110098
31. Runge C, Moriggl B, Børglum J, Bendtsen TF. The spread of ultrasound-guided injectate from the adductor canal to the genicular branch of the posterior obturator nerve and the popliteal plexus: a cadaveric study. Reg Anesth Pain Med. 2017;42(6):725–730. PMID: 28937534. doi:10.1097/AAP.0000000000000675
32. Raddaoui K, Radhouani M, Bargaoui A, et al. Adductor canal block: effect of volume of injectate on sciatic extension. Saudi J Anaesth. 2020;14(1):33–37. PMID: 31998017; PMCID: PMC6970348. doi:10.4103/sja.SJA_410_19
33. Coviello A, Golino L, Maresca A, Vargas M, Servillo G. Erector spinae plane block in laparoscopic nephrectomy as a cause of involuntary hemodynamic instability: a case report. Clin Case Rep. 2021;5:1–4.
34. Coviello A, Vargas M, Castellano G, Maresca A, Servillo G. Ultrasound guided Erector Spinae Plane Block (US-ESPB)— anesthetic block: case report. Clin Case Rep. 2020;5 1–4.
35. Coviello A, Esposito D, Galletta R, et al. Opioid-free anesthesia—dexmedetomidine as adjuvant in erector spinae plane block: a case series. J Med Case Reports. 2021;15:276. doi:10.1186/s13256-021-02868-5
36. Milone M, Di Minno MN, Musella M, Maietta P, Iacovazzo C, Milone F. Ultrasound-guided transversus abdominis plane block for retroperitoneal varicocele repair. Could it be an anesthesia method? Updates Surg. 2013;65(3):225–230. PMID: 23619829. doi:10.1007/s13304-013-0211-6
37. Di Minno MN, Milone M, Russolillo A, et al. Ropivacaine infusion in diabetics subject with peripheral arterial disease. A prospective study. Exp Clin Endocrinol Diabetes. 2013;121(2):91–93. PMID: 23147211. doi:10.1055/s-0032-1327757
38. Pham-Dang C, Kick O, Collet T, Gouin F, Pinaud M. Continuous peripheral nerve blocks with stimulating catheters. Reg Anesth Pain Med. 2003;28:83–88. doi:10.1097/00115550-200303000-00002
39. Coviello ES, Ianniello M, Mariconda M, et al. Intra-procedural catheter displacement for continuous adductor canal block: catheter-through needle method vs catheter-through-split-cannula method. Perioper Care Oper Room Manag. 2022;100255. doi:10.1016/j.pcorm.2022.100255
40. Ilfeld BM. Continuous peripheral nerve blocks: a review of the published evidence. Anesth Analg. 2011;113:904–925. doi:10.1213/ANE.0b013e3182285e01
41. Sedgwick P. Before and after study designs. BMJ. 2014;349:g5074. PMID: 25106742. doi:10.1136/bmj.g5074
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.