Back to Journals » Vascular Health and Risk Management » Volume 17
Population-Based Epidemiologic Study in Venous Diseases in Germany – Prevalence, Comorbidity, and Medical Needs in a Cohort of 19,104 Workers
Authors Kirsten N , Mohr N , Gensel F, Alhumam A, Bruning G, Augustin M
Received 3 June 2021
Accepted for publication 7 October 2021
Published 29 October 2021 Volume 2021:17 Pages 679—687
DOI https://doi.org/10.2147/VHRM.S323084
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Konstantinos Tziomalos
Natalia Kirsten,1 Nicole Mohr,1 Franziska Gensel,1 Aminah Alhumam,1,2 Guido Bruning,3 Matthias Augustin1
1Institute for Health Services Research in Dermatology and Nursing (IVDP), University Medical Center Hamburg-Eppendorf (UKE), Hamburg, Germany; 2Department of Dermatology, College of Medicine, King Faisal University, Hofuf, Al Ahsa, Saudi Arabia; 3Department of Vein and Dermatosurgery, Tabea Hospital GmbH and Co KG, Hamburg, Germany
Correspondence: Natalia Kirsten
Institute for Health Services Research in Dermatology and Nursing (IVDP), University Medical Center Hamburg-Eppendorf (UKE), Martinistr. 52, Hamburg, D-20246, Germany
Tel +49-40-7410-55428
Fax +49-40-7410-55348
Email [email protected]
Introduction: Data on the prevalence of chronic venous disorders (CVD) at the national level in Germany are scarce.
Methods: We performed a population-based observational study based on clinical examinations, personal history, and technical examinations. Data were collected from 2006 to 2015. Descriptive data analysis was done to determine CVD and chronic venous insufficiency (CVI) prevalence and occurrence of potential risk factors. Chi-squared tests were performed to estimate the influence of risk factors on the prevalence of CVD.
Results: In total, 19,104 employees from different branches were included. The majority of the examined people were doing office work (n = 8157; 80.2%). A total of 4038 persons (21.1%) show at least one sign of CVD. At least one sign of CVI could be found in 679 persons (3.6%). Being female was found to be protective with an odds ratio of 0.66 (95% CI 0.59– 0.73).
Conclusion: There is clear indication for active venous treatment in 22.3% of the adult working population in Germany.
Keywords: venous insufficiency, epidemiology, prevalence
Introduction
Chronic venous disorders (CVD), especially chronic venous insufficiency (CVI), are common and challenging conditions worldwide.1–4 They can markedly affect the quality of life and represent a considerable socioeconomic burden.5 CVD comprises the entire spectrum of anatomical and functional abnormalities of the venous system of the lower extremities, ranging from spider veins and telangiectasias to venous leg ulcers. In contrast, CVI refers to venous disease characterized by oedema, skin changes or venous ulcers.6
Interestingly, the prevalence of CVI is higher in Western countries.1 Lifestyle factors play a major role as a risk factor. In recent years, average body mass index (BMI) values have increased in Western countries,7 with obesity being a known risk factor of CVI.8 Furthermore, smoking, lack of physical activity, and often associated hypertension9 are other factors that promote the occurrence of CVI.
Both, CVD and CVI are very common conditions in the general population, usually starting in young adulthood and increasing in frequency and severity in older people.1 Many large-scale studies use secondary data analyses to determine prevalence. For example, the study by Homs-Romero et al 2021, using data sets of 5.8 million individuals, found a prevalence of CVD of 9.5% and CVI of 3.9% in the Catalan population.10 The analysis of health data has the advantage of being able to include a very large number of patients. However, the prevalence found may be underestimated since it depends on the quality of the coding performed.
Few studies on the prevalence of CVD have been conducted at the national level. In contrast, some very well-designed studies such as the Edinburgh Vein Study,11 the Basle study,12 and the Bonn study13 have only been conducted at regional level. Clinical phlebological examinations and duplex sonographic findings were used to assess the nationwide prevalence of venous disease.
The aim of our study was to obtain representative and robust large-scale data from the general working population on the prevalence of CVD, especially CVI. Furthermore, we analyzed the proportion of people with CVD who received a treatment recommendation.
Materials and Methods
Study Design
The study is a population-based observational study based on data from clinical examinations, personal history, and technical examinations according to a structured protocol.
Patients and Centers
Between 2006 and 2015, large-scale venous examinations of employees were carried out in companies as part of occupational health screenings. Medium to large size companies were included in the study. The companies belong to industrial sectors such as car manufacturing, metal and chemical processing, but also banks and insurance agencies. All employees were offered vein screening during working hours. Participation was voluntary. The only exclusion criterion was that the patients had not given consent to participate in the study. All procedures were in line with the ethical standards of the institutional and national research committee. Formal consent is not required for this type of study. Nevertheless, an ethics vote was obtained from the Ethics Committee of the University of Hamburg and all patients gave their informed consent. This study was in accordance with the Declaration of Helsinki.
Thirty minutes were scheduled for each screening. During the clinical examination, people were examined in a standing position for clinical signs of CVD, followed by duplex sonography of the superficial veins and perforators in the lower extremities. An examination of the entire vascular system was not possible due to time constraints. All findings were recorded electronically in a standardized data set. Duplex sonography was performed in standing position according to current international standards. Reflux in the area of the superficial veins and the perforators was defined and documented with a reflux time of more than 0.5 seconds.
The interviews and examinations were conducted by well-trained phlebologists who underwent additional specific training before starting the exams.
In addition to the clinical findings, data were collected on personal medical history, demographics, type of occupation, physical stress, and current complaints related to the varicose veins. The questions related to the complaints were asked openly without influencing the patient’s ability to answer them.
All CVD-related diagnoses were classified according to the Classification Of Venous Disorders (CEAP) classification system as follows:6
- C0 = no visible or palpable signs of venous disease
- C1 = telangiectasia or reticular veins
- C2 = varicose veins
- C3 = oedema
- C4a = pigmentation or eczema
- C4b = lipodermatosclerosis or atrophie blanche
- C5 = healed venous ulcer
- C6 = active venous ulcer
CVI was considered advanced CVD and included stages C3–C6 according to CEAP classification. At the end of the screening, the investigator made and documented treatment recommendations based on the clinical findings and duplex sonography. This decision was at the discretion of the investigator. The reasons for the decision were not documented and could not be further evaluated in this study.
Statistical Analysis
Descriptive data analysis was conducted to determine the prevalence of CVD and CVI and the occurrence of potential risk factors. In a second step, nonparametric tests were conducted to determine how people with and without CVD differ in terms of age and BMI. Chi-squared tests were used to estimate the influence of risk factors on the prevalence of CVD and CVI. Finally, a logistic regression analysis controlling for age, sex, and BMI was performed. All statistical analyses were performed using SPSS 23.0 (IBM, Armonk, NY, US) for Windows 10.
Results
Sociodemographic Data
Data were collected between 2006 and 2015. A total of 19,104 employees from different sectors were included. Mean age was 46.1 years ± 9.8, 53.5% were male and mean BMI was 26.1 kg/m2 ± 4.4 (Table 1).
 |
Table 1 Sociodemographic Factors of Study Population |
Personal History and Occupation
Personal history and current complaints were assessed from 2012 (n = 10,514). Figure 1 and S1 show the occurrence of the parameters collected. The proportion of people with own children and the use of birth control pills only refer to women (n = 4053), as they are potential risk factors for women only.
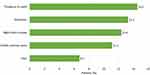 |
Figure 1 Current complaints (n = 10,514). |
The majority of the people examined had an office job (n = 8157; 80.2%). A total of 7640 (n = 75.2%) persons had predominantly sitting occupations, 681 (6.7%) persons had predominantly standing occupations, and 1844 (18.1%) persons had alternating occupational activities. Most of the people examined had occupations that did not involve physical work (n = 7866; 77.4%). Only a minority of the studied population had an activity that involved heavy physical work (n = 487; 4.8%).
Data on CVD/CVI
Diagnoses
In general, 3.6% (n = 679) had at least one clinical sign of CVI. See Table 2 for the individual diagnoses.
 |
Table 2 People with Clinical Signs of Chronic Venous Insufficiency (N = 19,104) |
Other superficial and perforating vein diagnoses assessed by duplex sonography are listed in Table 3. The summaries are not based on cases but on persons, i.e. it was counted how many people have at least one listed diagnosis. The summary of all diagnoses of the superficial and perforating venous system, with the exception of reticular veins and telangiectasia, compose the prevalence of CVD in the current study of 21.1% (n = 4038).
 |
Table 3 Summarized Diagnoses of the Superficial and Perforating Veins (N = 19,104) |
Treatment Recommendations
22.3% (4260) of the participants were recommended further treatment. Compression therapy was mentioned most frequently with 17.1% (3267), followed by venous surgery with 10.5% (n = 2004), and sclerotherapy with 2.0% (n = 380).
Multivariate Analysis
The Mann–Whitney U-test showed that there was a significant difference between people with and without CVD in terms of age and BMI. The mean BMI in the group of people with at least one CVD diagnosis was 26.64 kg/m2 ± 4.26 and 25.96 kg/m2 ± 4.40 in the group without CVD diagnosis. The mean age of examined population with at least one CVD diagnosis was 48.74 years ± 9.17 and in the group without CVD diagnosis 45.40 years ± 9.79. Both parameters were significantly higher among participants with CVD.
Table 4 shows the prevalence of CVD dependent on different potential risk factors. The significance of group differences was calculated via chi-squared tests. According to this, working in storage area, standing at work, physical strain, varicose veins, and leg ulcers in the family history as well as diabetes and hypertension can be classified as risk factors. However, these findings are not controlled for age, gender, and BMI.
 |
Table 4 Differences Between People with and without at Least One Chronic Venous Disorder (CVD) Diagnosis (N = 19,104) |
Logistic Regression Analysis
Logistic regression analysis was performed to estimate the impact of previously identified risk factors controlling for age, gender, and BMI.
For men and women in the regression model and CVD as dependent variable age, BMI and sex were found to be significant predictors. See Table 5 for other independent variables used in the regression model. The model was significant (p < 0.001), explaining 6% of the total variation in the prevalence of CVD (Nagelkerke R2 = 0.06). In terms of gender, being female was found to be protective, with an odds ratio (OR) = 0.66 (95% CI 0.59–0.73). In addition, a significantly increased risk was present for varicose veins in family history (OR = 1.08 (95% CI 1.07–1.09)), physical strain at work (OR = 1.26 (95% CI 1.12–1.42)), and standing at work (OR = 1.30 (95% CI 1.08–1.57)).
 |
Table 5 Risk Factors to Develop Chronic Venous Disorder – Results of the Logistic Regression Analysis, Both Sexes (n = 10,163) |
Divided by sex, BMI was significant only in women (OR = 1.04 (95% CI 1.02–1.05)) and standing at work was significant only in men (OR = 1.46 (95% CI 1.18–1.81)).
An additional model was calculated only for women with own children and use of contraceptive pill as additional predictors. The latter factor had no significant influence, but pregnancy was found to be a risk factor with OR = 1.03 (95% CI 1.01–1.06). The model explained 4.8% of the variation in the prevalence of CVD.
Discussion
It has long been known that a significant proportion of the general population suffers from chronic venous disease.1–4 Lack of early treatment can lead to disease progression and the development of skin lesions such as lipodermatosclerosis and to venous leg ulcers. Even before escalation to ulcers, there is a significant disease burden from chronic venous disorders such as pain or oedema.
Although the opinion on the need for early treatment is highly controversial, early treatment of such conditions related with chronic venous disorders can reduce the risk of escalation and help to improve quality of life.14
Nevertheless, many people are not referred to vein examination even in the active disease stage.
For this reason, the present study was conducted to obtain large-scale data on the prevalence of CVD in the general working population in Germany. Another aim was to analyze the frequency of treatment recommendations. For this purpose, phlebological screenings were carried out on more than 19,000 persons of working age in large and medium-sized companies throughout Germany. In terms of gender and BMI, the dataset is representative of the German working population (51.5% male, mean BMI 25.7 kg/m2).15
Regarding the prevalence of CVD, we found at least one CVD-related diagnosis in 21.1% of the studied population using duplex sonography. The prevalence of CVI (C3–C6 according to CEAP) was 4.3%. Compared to the Edinburgh Vein Study (prevalence of CVI in men 9.4% and in women 6.6%), the prevalence of CVI in our cohort is lower.11 This may be due to the fact that we studied a rather healthy population. Ulcus cruris is a life changing experience for many patients. In one survey study, 12.7% reported that the ulcer prevented them from doing their usual work.16 However, data on the prevalence of CVI is inconsistent. Cesarone et al 2002 describe a prevalence of CVI of only 1% in a population of 30,000 volunteers.17
In another international study, a total of 63.9% were found to have C1–C6 CVD in outpatient services. The high prevalence in the group studied could be due to a selection bias. Patients who had presented to the doctor, i.e. had a medical need for treatment and were therefore to be assessed as pathological, were studied.4
This contrasts with the results of Homs-Romero et al 2021, where a CVD prevalence of 9.5% and a CVI prevalence of 3.9% were identified.10 But this is consistent with the methodological approach. It is to be expected that prevalences determined from secondary data analyses would be lower from the direct instrument-based clinical examinations.
In our study, men showed a significantly higher incidence of at least one sign of CVD. However, in most studies, women show higher prevalence than men of CVD and CVI. In contrast, the Edinburgh Vein Study reports equal prevalence in men and women.18
The most important factor for developing CVI seems to be age.19 This may have been a bias in our study because only patients up to an age of 70 years were included.
Another factor is hormonal influences. Especially the postmenopausal changes are an important pathogenetic factor.20 It has been shown that estrogen receptors are found in the endothelium, and their number is significantly increased in postmenopausal women with varicosis.21 Estrogen receptors are also found in men, but their number is significantly lower than in women. Similarly, progesterone levels are elevated in CVI positive patients compared to healthy controls.20 How the hormones are involved in the modification of the vascular walls, however, has not yet been clarified. Not to be forgotten at this point, of course, are the genetic factors that can promote varicosis.22 If we apply these findings to our study, we can state that postmenopausal women are somewhat underrepresented in our cohort, which may have favored the results for the male gender.
A total of 22.3% of the patients in our study received a treatment recommendation. In most cases (17.1%), patients were advised to wear compression stockings. Even though the necessity of invasive vein therapy is controversial for medical and socioeconomic reasons, experts agree that causal therapy is useful even in the early stages of venous disease and can prevent complications and the progression.23 On the other hand, a recommendation for venous surgery was made in 10.5% of the persons examined based on the clinical examination and also on the duplex sonography. This suggests that the purely clinical diagnosis of CVI is not sufficient and supports the international recommendation to use duplex sonography as the gold standard for the diagnosis of CVD.
These results suggest that the good experiences with such a screening program should be followed up systematically.
Logistic regression analysis identified varicose veins in family history, standing occupation, physical strain at work, and pregnancy in women as risk factors for CVI. Several studies have already found that standing at work contributes to a higher risk of developing CVI.24–31
It should be noted that the current study is limited to people up to 70 years of age and thus underestimates the overall need for healthcare in the general population, as older people usually have higher rate of venous disease. Since the data came from occupational screenings, the healthy worker effect needs to be discussed. In this case, the prevalence in the total population would be underestimated, as the seriously ill and chronically disabled are not represented in the cohort. The same applies to age, which is a typical risk for varicose veins. Nevertheless, the results indicate a very large number of people affected in the general population. A potential limitation is that response bias cannot be ruled out as all participants were volunteers, as in all such studies. Therefore, it cannot be ruled out that people with specific complaints tended to participate to a higher degree. On the other hand, people undergoing active treatment for venous disease may not have participated because they do not expect any further benefit from participation. Nevertheless, this study contributes to understanding the extent of CVI as a problem in the general adult working age population.
In total, there is a significant need for the detection and treatment of venous disease in the general population and obviously a significant proportion of patients have not yet been referred to a specialist. Continued screening programs would be recommended.
Conclusion
21.1% of the German working population has been diagnosed with at least one CVD-related condition. Early detection of the need for treatment can lead to long-term relief for the healthcare system and positively influence the quality of life of those affected. Therefore, there is a high need for adapted detection methods.
Abbreviations
CVD, chronic venous disorders; CVI, chronic venous insufficiency; CEAP, Classification of Venous Disorders; BMI, body mass index.
Data Sharing Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to restrictions e.g. their containing information that could compromise the privacy of research participants.
Acknowledgments
The authors thank Mr Hagen Heigel for supporting this study in the screening phase. The authors thank the Scientific Communication Team of the IVDP, in particular Sara Tiedemann and Mario Gehoff, for copy editing. The abstract of this paper was presented at the World Congress of Dermatology 2019 as a poster presentation with interim findings. The poster’s abstract was published in the Abstract Book of WCD to upload under following link: Abstracts | Abstract Book | WCD2019 | A new ERA for global Dermatology (wcd2019milan-dl.org).
Funding
This work was supported by an unrestricted research grant from BSN medical GmbH, Hamburg, Germany. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Disclosure
M Augustin has received a research grant and speaker honoraria from BSN medical GmbH. G Bruning has received travel grants from Bauerfeind AG. The authors report no other conflicts of interest in this work.
References
1. Beebe-Dimmer JL, Pfeifer JR, Engle JS, Schottenfeld D. The epidemiology of chronic venous insufficiency and varicose veins. Ann Epidemiol. 2005;15(3):175–184. doi:10.1016/j.annepidem.2004.05.015
2. Carpentier PH, Maricq HR, Biro C, Ponçot-Makinen CO, Franco A. Prevalence, risk factors, and clinical patterns of chronic venous disorders of lower limbs: a population-based study in France. J Vasc Surg. 2004;40(4):650–659. doi:10.1016/j.jvs.2004.07.025
3. Evans C, Fowkes F, Ruckley C, Lee AJ. Prevalence of varicose veins and chronic venous insufficiency in men and women in the general population: Edinburgh vein study. J Epidemiol Community Health. 1999;53(3):149–153. doi:10.1136/jech.53.3.149
4. Rabe E, Guex J, Puskas A, Scuderi A, Fernandez Quesada F; VCP Coordinators. Epidemiology of chronic venous disorders in geographically diverse populations: results from the vein consult program. Int Angiol. 2012;31(2):105–115.
5. Huang Y, Gloviczki P. Relationships between duplex findings and quality of life in long-term follow-up of patients treated for chronic venous disease. Phlebology. 2016;31(1 Suppl):88–98. doi:10.1177/0268355516630868
6. Eklöf B, Rutherford RB, Bergan JJ, et al. Revision of the CEAP classification for chronic venous disorders: consensus statement. J Vasc Surg. 2004;40(6):1248–1252. doi:10.1016/j.jvs.2004.09.027
7. NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet. 2017;390(10113):2627–2642.
8. Belczak CE, de Godoy JM, Belzack SQ, Ramos RN, Caffaro RA. Obesity and worsening of chronic venous disease and joint mobility. Phlebology. 2014;29(8):500–504. doi:10.1177/0268355513492510
9. Prochaska JH, Arnold N, Falcke A, et al. Chronic venous insufficiency, cardiovascular disease, and mortality: a population study. Eur Heart J. 2021:ehab495. doi:10.1093/eurheartj/ehab495.
10. Homs-Romero E, Romero-Collado A, Verdú J, Blanch J, Rascón-Hernán C, Martí-Lluch R. Validity of chronic venous disease diagnoses and epidemiology using validated electronic health records from primary care: a real-world data analysis. J Nurs Scholarsh. 2021;53(3):296–305. doi:10.1111/jnu.12639
11. Lee AJ. Lifestyle factors and the risk of varicose veins: Edinburgh vein study. J Clin Epidemiol. 2003;56(2):171–179. doi:10.1016/S0895-4356(02)00518-8
12. Widmer LK, Da Silva A, Stähelin H. Peripheral Venous Disorders: Prevalence and Socio-Medical Importance Observations in 4529 Apparently Healthy Persons Basle Study III. Bern: Hans Huber; 1978.
13. Rabe E, Pannier-Fischer F, Bromen K, et al. Bonner Venenstudie der Deutschen Gesellschaft für Phlebologie. Phlebologie. 2003;32(1):1–14. doi:10.1055/s-0037-1617353
14. Novak CJ, Khimani N, Kaye AD, Jason Yong R, Urman RD. Current therapeutic interventions in lower extremity venous insufficiency: a comprehensive review. Curr Pain Headache Rep. 2019;23(3):16. doi:10.1007/s11916-019-0759-z
15. Statistisches Bundesamt. Bevölkerung mit Migrationshintergrund - Ergebnisse des Mikrozensus. [Population with migration background - results of the microcensus]; 2013. Available from: https://www.verband-binationaler.de/fileadmin/user_upload/_imported/fileadmin/Dokumente/PDFs/Mikrozensus_2013.pdf.
16. Cunha N, Campos S, Cabete J. Chronic leg ulcers disrupt patients’ lives: a study of leg ulcer-related life changes and quality of life. Br J Community Nurs. 2017;22(Suppl 9):S30–S37. doi:10.12968/bjcn.2017.22.Sup9.S30
17. Cesarone MR, Belcaro G, Nicolaides AN, et al. “Real” epidemiology of varicose veins and chronic venous diseases: the san valentino vascular screening project. Angiology. 2002;53(2):119–130. doi:10.1177/000331970205300201
18. Robertson L, Lee AJ, Evans CJ, et al. Incidence of chronic venous disease in the Edinburgh vein study. J Vasc Surg Venous Lymphat Disord. 2013;1(1):59–67. doi:10.1016/j.jvsv.2012.05.006
19. Bergan JJ, Schmid-Schönbein GW, Smith PDC, Nicolaides AN, Boisseau MR, Eklof B. Chronic venous disease. N Engl J Med. 2006;355(5):488–498. doi:10.1056/NEJMra055289
20. García-Honduvilla N, Asúnsolo Á, Ortega MA, et al. Increase and redistribution of sex hormone receptors in premenopausal women are associated with varicose vein remodelling. Oxid Med Cell Longev. 2018;2018:3974026. doi:10.1155/2018/3974026
21. Mashiah A, Berman V, Thole HH, et al. Estrogen and progesterone receptors in normal and varicose saphenous veins. Cardiovasc Surg. 1999;7(3):327–331. doi:10.1016/S0967-2109(98)00132-X
22. Fiebig A, Krusche P, Wolf A, et al. Heritability of chronic venous disease. Hum Genet. 2010;127(6):669–674. doi:10.1007/s00439-010-0812-9
23. Rabe E, Partsch H, Hafner J, et al. Indications for medical compression stockings in venous and lymphatic disorders: an evidence-based consensus statement. Phlebology. 2018;33(3):163–184. doi:10.1177/0268355516689631
24. Abramson J, Hopp C, Epstein L. The epidemiology of varicose veins. A survey in western Jerusalem. J Epidemiol Community Health. 1981;35(3):213–217. doi:10.1136/jech.35.3.213
25. Brand F, Dannenberg A, Abbott R, Kannel W. The epidemiology of varicose veins: the Framingham study. Am J Prev Med. 1988;4(2):96–101. doi:10.1016/S0749-3797(18)31203-0
26. Ebert-Willershausen W, Marshal M. Prävalenz, Risikofaktoren und Komplikationen peripherer Venenerkrankungen in der Münchener Bevölkerung. [Risk factors and complications of peripheral venous diseases in the Munich population]. Hautarzt. 1984;35(2):68–77. German,
27. Krijnen RM, de Boer EM, Adèr H, Bruynzeel DP. Venous insufficiency in male workers with a standing profession. Part 1: epidemiology. Dermatology. 1997;194(2):111–120. doi:10.1159/000246077
28. Lake M, Pratt G, Wright I. Arteriosclerosis and varicose veins: occupational activities and other factors. J Am Med Assoc. 1942;119(9):696–701. doi:10.1001/jama.1942.02830260010004
29. Stvrtinová V, Kolesár J, Wimmer G. Prevalence of varicose veins of the lower limbs in the women working at a department store. Int Angiol. 1991;10(1):2–5.
30. Van den Berg E. Prospektive epidemiologische und experimentelle Studie zur Ätiologie und Pathophysiologie der Primären Varicose. [Prospective epidemiological and experimental study on the aetiology and pathophysiology of primary varicosis]. Phlebol Proktol. 1983;12:91–100. German.
31. Fowkes F, Lee A, Evans C, Allan P, Bradbury A, Ruckley CV. Lifestyle risk factors for lower limb venous reflux in the general population: Edinburgh vein study. Int J Epidemiol. 2001;30(4):846–852. doi:10.1093/ije/30.4.846
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
