Back to Journals » Risk Management and Healthcare Policy » Volume 16
Policy Disparities Between Singapore and Israel in Response to the First Omicron Wave
Received 11 January 2023
Accepted for publication 14 March 2023
Published 2 April 2023 Volume 2023:16 Pages 489—502
DOI https://doi.org/10.2147/RMHP.S402813
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Mecit Can Emre Simsekler
Rongcai Ma,1 Leiyu Shi,2 Gang Sun1,2
1Department of Health Management, School of Health Management, Southern Medical University, Guangzhou, Guangdong, 510515, People’s Republic of China; 2Department of Health Policy and Management, Bloomberg School of Public Health, Johns Hopkins University, Baltimore, MD, 21205, USA
Correspondence: Gang Sun, Department of Health Management, School of Health Management, Southern Medical University, Guangzhou, Guangdong, 510515, People’s Republic of China, Email [email protected]
Purpose: The purpose of this study is to evaluate public health measures during the first Omicron wave in Singapore and Israel to inform other countries confronted by COVID-19 outbreaks.
Methods: A comparative analysis was conducted using epidemiological data from Singapore and Israel between November 25th, 2021 and May 2nd, 2022 and policy information to examine the effects of public health measures in the two countries during the COVID-19 pandemic.
Results: Public health measures implemented by Singapore and Israel in response to the first Omicron wave were primarily intended to mitigate the effects of the COVID-19 pandemic. In Singapore, the pandemic led to more than 910,000 confirmed cases, a mortality rate of approximately 0.047%, a hospitalization rate of approximately 10.95%, and a severe illness rate of approximately 0.48%, without a second peak. In Israel, the pandemic not only resulted in over 2.74 million confirmed cases, a mortality rate of 0.095%, a hospitalization rate of about 7.39%, and a severe illness rate of approximately 2.30% but also returned after the significant relaxation of prevention regulations from March 1st, 2022.
Conclusion: Early and strict border control measures and surveillance measures are more effective in preventing and controlling the rapid spread of new strains of COVID-19 in the early stage. Furthermore, to prevent and control this highly infectious disease, COVID-19 vaccinations and booster shots must be promoted as soon as possible, medical service capacity must be enhanced, the hierarchical medical system must be improved, and non-pharmacological interventions must be implemented.
Keywords: COVID-19, Omicron, public health policy, Singapore, Israel
Introduction
Since the outbreak of the COVID-19 pandemic, the entire world has experienced tremendous changes. Different strains of SARS-CoV-2 have emerged as a result of the continuous evolution of the virus, exhibiting varied levels of pathogenicity and infectivity. The B.1.1.529 strain, also known as Omicron, is one of the SARS-CoV-2 variants. Initially detected in samples collected in South Africa on November 9th, 2021, the Omicron variant was reported to the WHO on November 24th, 2021.1,2 Due to its high infectivity and strong ability to evade immune defenses acquired from vaccination, the Omicron variant with over 30 mutations in the stinger protein has attracted worldwide attention.3,4 Models have been used to conduct calculations, which suggest that Omicron may be up to 10 times more infectious than the original strain and about 2.8 times more infectious than Delta.5 At the beginning of the outbreak, the rise in the number of Omicron infections was very significant: there was a 2.5% increase in the US within two weeks and a doubling every 2–3 days in the UK.1 With its high infectivity and asymptomatic carriage rate, the Omicron variant was rapidly replacing the Delta variant as the most prevalent strain worldwide in 2022.
Consequently, the Omicron variant posed new challenges to pandemic control in various countries, and the socioeconomic implications of different control strategies and measures varied. To better balance public health event control with socioeconomic development, countries have adjusted their COVID-19 control strategies accordingly. The likelihood of infectious disease transmission is decided by the ratio of the human flow to the population.6 Located on the Mediterranean coast, Israel has a total land area of about 22,000 square kilometers and a population of more than 9.3 million.7,8 By contrast, at the entrance of the Straits of Malacca, Singapore has a land area of about 724 square kilometers and a population of over 5.64 million.9 As a result of the well-developed transportation network in Singapore and Israel, along with the high density of their populations,10 preventing and controlling the rapid spread of the epidemic was challenging. Among various methods for preventing and controlling infectious diseases, controlling the sources of infection and blocking areas infected has been proven to be effective.11 Therefore, the two countries adopted strict containment strategies at the beginning of the outbreak of the COVID-19 pandemic in 2020 and achieved positive outcomes in both the prevention and control of the disease.12,13 Israel took relatively strict measures, implementing three lockdowns in 2020. The first two lockdowns achieved good prevention and control results quickly, while the third lockdown required a slightly longer time to take effect.14 However, a long-term lockdown usually has a negative economic impact on families and businesses, as well as mental health.15 On the other hand, the countermeasures taken by Singapore were relatively mild, without lockdown measures throughout the process, primarily implemented to reduce the infection and mortality rates. Specifically, its measures were strictly aimed at preventing the spread of the pandemic, focusing on safety management to cut off transmission routes and ensure vulnerable group protection. However, due to the increased infectivity of COVID-19, implementing a strict containment strategy became more challenging and costly under the constraints of limited resources. A high incidence of COVID-19 infection rendered the important pandemic containment measure, Test-Trace-Isolate-Support, ineffective.16 Besides, limitations on personnel, material, and logistical resources may impede the implementation of disease control measures in a variety of ways.17 Therefore, Israel and Singapore loosened their COVID-19 mitigation strategies in 2021 following the launch of a COVID-19 vaccination program in December 2020.
The policy changes made by these two countries, from strict containment strategies to flexible prevention and control strategies, full liberalization, and coexistence with COVID-19, have significant implications for pandemic control policy-making. Thus, the main research objects of this article are Singapore and Israel, whose objective data on epidemiology from the first Omicron wave was compared and analyzed, along with a discussion about public health prevention and control measures. It is expected that the prevention and control strategies adopted by these two countries and the results they achieved will provide examples for countries severely affected by the COVID-19 epidemic to refer to.
Methods
Data Collection
The epidemiological data of the first wave of Omicron infection cases in Singapore and Israel was mainly obtained from the Ministry of Health (MOH) of Singapore and Israel,18,19 as well as the website Our World In Data.20 It was collected between November 25th, 2021 and May 2nd, 2022 as the first cases of Omicron infection were confirmed in Israel and Singapore on November 26th, 2021 and December 2nd, 2021, respectively. Daily new cases, daily mortality, daily hospitalization cases, cumulative confirmed cases, and cumulative mortality are the main indicators used in the data collection. It is worth noting that the subdivided data in the indicator of daily hospitalization cases differ slightly in the two countries. Singapore’s data primarily consist of the number of patients receiving oxygen administration in general wards and the number of patients in intensive care units every day. The Israeli data includes three categories of cases: mild, moderate, and severe cases, among which severe cases can be further divided into critical, ECMO, and ventilated cases. Moderate cases are defined as pneumonia patients who may require palliative care in a task-specific COVID-19 ward.21 Given the clear demand for medical resources and the test of medical service capacity, in this paper, two data values of moderate cases and severe cases were extracted from the Israeli data and the Singaporean data, respectively, for comparison and analysis.
Policy Information
For information on prevention and control policies during the first Omicron wave, we searched national documents, official announcements, and televised speeches by the prime minister/health minister of Singapore and Israel through official websites of institutions such as the Ministry of Health and the government.22,23 The collected data was divided chronologically into two general categories: border control measures and domestic prevention and control measures.
Results
Prior to the first Omicron wave, the implementation of COVID-19 control strategies in Singapore was generally divided into three phases: the strict clearance phase (January 23rd, 2020-June 23rd, 2021), the preparation phase for the shift in control strategy (June 24th, 2021-August 9th, 2021), and the initial phase for the formal shift in control strategy (August 10th, 2021-November 21st, 2021).24 In Israel, this process was divided into two phases, namely the containment strategy phase and the mitigation strategy phase, in which June 1st, 2021 was determined as the cut-off date.25 During the containment strategy phase, Israel experienced three significant peaks of infection.19 At the same time, Singapore did not reach a clear peak of infection until August 2020. After June 2021, both countries were affected by the Delta outbreak, with Israel experiencing infection peaks much earlier than Singapore. The infection peak occurred in September 2021 and October 2021 in Israel and Singapore, respectively.
Singapore’s Major Policies in Response to the First Omicron Wave
Upon the release of a warning by the WHO on November 26th, 2021 that the Omicron variant would pose a “very high” global health risk,2 the Government of Singapore reacted swiftly by strengthening the country’s border control measures. In response to the discovery of two cases of Omicron infection among passengers arriving on December 1st, 2021, Singapore immediately tightened detection and isolation measures for incoming passengers to closely monitor and prevent the Omicron outbreak. Specifically, all incoming passengers were required to undergo a polymerase chain reaction (PCR) or antigen rapid test (ART) on their arrival, and those infected with the Omicron variant were kept in quarantine for ten days at the National Center for Infectious Diseases. On December 27th, 2021, Singapore lifted the centralized quarantine imposed on cases infected with Omicron.
For patients at low risk of mild infection, a home recovery program was implemented in Singapore from August 2021 when the country entered the phase of coexistence with COVID-19. This program was then further expanded in January 2022. Furthermore, the Public Health Preparedness Clinic (PHPC) scheme provided appropriate medical support. Meanwhile, the Government of Singapore encouraged the public to regularly test themselves with ART kits and motivated employers and businesses to incorporate Roster Routine Testing (RRT) by expanding subsidies for routine testing on mandatory rosters. Through testing, the source of infection can be detected as early as possible, so as to realize the rapid tracing and containment of infection. In response to a rapid increase in Omicron infections, Singapore streamlined its health-care program on February 11st, 2022, shifting the focus from prevention and control to severe case management and vulnerable population protection. Accordingly, those who are responsible for the prevention and control of the pandemic were shifted from the public to individuals who were encouraged to conduct self-management as appropriate. However, it should be noted that throughout the pandemic, community safety management measures were present, which consisted of five primary dimensions: group size, mask wearing, workplace requirements, safe distance, and capacity limit. With the changes in the number of Omicron infections and the capacity of the healthcare system, Singapore readily adapted the implementation requirements for community safety management to minimize the spread of the pandemic. Despite the rapid spread of the pandemic in February 2022 in Singapore, the situation was largely contained by the end of March, and the number of infections declined significantly in April. As a result, Singapore further removed relevant community safety management measures from March 29th, 2022, retaining only the two policies of wearing masks indoors and keeping a safe distance. On April 26th, 2022, Singapore relaxed its prevention and control measures, only emphasizing that masks must be worn indoors and on public transportation. Table 1 shows the main prevention and control policies in Singapore during the first Omicron wave.
 |
Table 1 Major Prevention and Control Policies in Response to the First Omicron Wave in Singapore and Israel |
Israel’s Major Policies in Response to the First Omicron Wave
Compared with Singapore, Israel had its first Omicron case confirmed relatively early, with a relatively slow growth rate of infection in the early stages, a rapid increase in the number of infections in later stages, and the earlier occurrence of the peak of Omicron infection. As opposed to past outbreaks, this wave received a more flexible response from the Government of Israel. As the first case of Omicron infection was confirmed on November 26th, 2021, Israel took the initiative to close its border on November 29th, 2021, prohibiting all unauthorized non-citizens from entering the country. Similar to Singapore, Israel increased the testing and quarantine measures targeted at incoming travelers. To prevent the spread of the Omicron variant within the country, all incomers were required to undergo PCR testing upon arrival and home quarantine whether they were vaccinated or not.
Considering the highly contagious nature of the Omicron variant, the Government of Israel outlined three principles for dealing with it. To begin with, it highlighted the importance of providing as much protection as possible for vulnerable groups. Therefore, on January 2nd, 2022, Israel became the first country to administer the fourth dose of the COVID-19 vaccine to people aged more than 60 in the absence of a widespread medical consensus. Also, Israel adjusted its testing on January 5th, 2022 to encourage the younger population to use rapid antigen testing, thereby reserving the more precise PCR test for the elderly and the most vulnerable. From April 2022, nursing homes and other institutions were required to participate in the Green Pass program, which granted a Green Pass to certain immune populations. Secondly, Israel necessitated maintaining the proper functioning of the educational system. For example, schools in severely affected areas were ordered to offer face-to-face instruction and ensure a vaccination rate of students not lower than 70%. From January 27th, 2022, it became mandatory for all students in Israel to receive an antigen test on a biweekly basis so that infected individuals could be identified early enough to prevent large-scale outbreaks within educational institutions. Thirdly, Israel attempted to maintain a high degree of economic openness during the outbreak. Between November 27th, 2021 and January 20th, 2022, domestic Omicron control measures were implemented in Israel, including upgraded requirements for indoor group activities and increased requirements for access to shopping malls and dine-in restaurants. In response to a gradual decline in the number of Omicron infections, Israel eased its prevention and control measures on February 21st, 2022. Although a majority of its prevention and control regulations had already been eliminated by March 1st, 2022, the second Omicron wave occurred in Israel shortly thereafter, leading to a continuous increase in the number of infections until mid-to-late April 2022. Thus, Israel announced on April 23rd, 2022 the cancellation of all precautionary measures. Table 1 shows the main prevention and control policies in Israel during the first Omicron wave.
Epidemiological Trends of the First Omicron Wave in Singapore and Israel
Table 2 illustrates differences between Singapore and Israel in terms of the prevalence of SARS-CoV-2 variants. At the beginning of the Omicron outbreak, Singapore experienced a greater increase in the number of infections than Israel. Approximately 41% of Singaporeans and 24% of Israelis were infected with the Omicron variant as of December 20th, 2021, after which the number of Omicron infections increased rapidly in Israel. As of January 3rd, 2022, the infection rate exceeded 80% in Israel. As a result, the Omicron variant became the predominant strain of COVID-19 in Singapore and Israel by the end of January 2022.
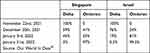 |
Table 2 The Proportion of the Two Prevalent SARS-CoV-2 Variants in Singapore and Israel |
Figure 1 shows 159 days of epidemiological data during the first Omicron wave in Singapore. According to the data, the first Omicron wave can be divided into two phases between which January 2nd, 2022 is the cut-off point. Due to the implementation of the Stabilization Phase of tightening measures in Singapore from October 25th, 2021 to November 21st, 2021, the outbreak in Singapore was well controlled from January 2nd, 2022, with a clear downward trend in the number of daily new cases and deaths, as well as a flattening trend in the number of cumulative cases and deaths. Both the cumulative case curve and the cumulative death curve ascended steeply in February 2022, with a significant increase in the number of both infections and deaths. Then, both the total and daily numbers of confirmed cases reached their peaks, which were more than 910,000 and 25,000, respectively. The total of deaths and the highest number of daily deaths were 428 and 14, respectively, with a mortality rate of approximately 0.047%. After late March 2022, the number of new cases per day in Singapore began to decrease slowly, the number of deaths decreased significantly, and the cumulative case curve and cumulative death curve began to become stable. In response, Singapore began to loosen its safety management measures cautiously. However, its cumulative case curve ascended again after May 2022.
Figure 2 shows 159 days of epidemiological data during the first Omicron wave in Israel, which can be divided into two phases as well. During the period between November 25th, 2021 and December 18th, 2021, the number of new cases per day in Israel increased steadily and the cumulative case curve remained relatively flat. A marked increase in the number of new cases per day began in early January 2022, leading to a significant upward trend in the cumulative case curve in Israel. After January 13th, 2022, there was a significant increase in the number of deaths and a significant upward trend in the cumulative death curve. During this phase, more than 2.74 million confirmed cases were reported, which resulted in the arrival of the fifth wave of the pandemic. The highest number of daily confirmed cases was over 85,000. With a mortality rate of approximately 0.095%, the total number of deaths was 2594, and the highest number of daily deaths reached 74. In March 2022, the number of daily new cases in Israel began to decline gradually. It was on March 13th, 2022 that the death toll began to decrease significantly. As precautionary measures were lifted in March 2022, the virus spread again in Israel, and the cumulative case curve and cumulative death curve ascended again.
Figure 3 shows the data on hospitalized cases during the first Omicron wave in Singapore. Like the upward trend in the number of COVID-19 infections, the number of hospitalized COVID-19 patients in Singapore gradually declined between November 25th, 2021 and January 2nd, 2022. In addition, the number of COVID patients receiving oxygen administration in general wards and intensive care units decreased significantly as well. Then the number of hospitalizations again increased after January 2nd, 2022, but from March 2022 both the number of hospitalizations and serve cases gradually declined. During these 159 days, both the number of hospitalized cases and the number of ICU cases in Singapore reached their peaks, which were 1442 and 86, respectively, and the hospitalization rate and the severe case rate were around 10.95% and 0.48%, respectively.
Figure 4 shows the data on hospitalized cases during the first Omicron wave in Israel. During the period between December 25th, 2021 and early January 2022, Israel experienced a slower increase in the number of hospitalized COVID-19 patients and a decrease in the number of severe cases. From mid-January 2022, the number of hospitalized cases in Israel increased rapidly, with a marked increase in the number of moderate and severe cases. The number of severe cases per day exceeded 1000 from January 30th, 2022 to February 14th, 2022. During these 159 days, the number of hospitalized cases and the number of severe cases in Israel reached their peaks, which were 3501 and 1240, respectively, with a hospitalization rate and a severe case rate of approximately 7.39% and 2.30%, respectively.
Discussion
It has become increasingly difficult to identify and track early infections of SARS-CoV-2 as it continues to evolve. In response to the rapidly spreading epidemic, the increasingly challenging prevention and control situation, the increasing vaccination coverage rate, and greater economic pressures, each country kept adapting its prevention and control strategies according to its national conditions, so as to maintain a balance between the regular fight against the epidemic and the openness of the economy. In this study, epidemiological data on the numbers of new cases, deaths, and hospitalizations during the first Omicron wave in Singapore and Israel were compared to assess the effectiveness of the public health measures taken by the two nations. While both Singapore and Israel experienced the highest number of infections during the first Omicron wave, neither adopted a strict blockade control approach. Instead, both countries focused on mitigation measures, which include but are not limited to encouraging vaccinations and booster shots, monitoring the health system load continuously, identifying and treating severe cases, and conducting non-pharmacological interventions to delay the epidemic’s peak. There are both similarities and differences between the two countries’ prevention and control policies in response to the first Omicron wave.
Border Control Measures
Singapore and Israel adopted strict border control measures and surveillance measures early in response to the Omicron outbreak when the pathogenicity and risk of the variant were not fully understood and achieved good results. In previous studies, travel restrictions have been found to be effective in preventing the importation of COVID-19 cases in the early stages of an outbreak.26 This is why, in most countries, border control measures such as travel restrictions, visa suspensions, and international flight restrictions have been adopted in response to the COVID-19 pandemic.27 As an initial measure, travel restrictions were implemented in Singapore, targeted at countries/regions that were affected by the Omicron outbreak, while Israel closed its only international airport. Moreover, both governments increased comprehensive screening of incoming travelers and tracked and isolated Omicron-infected individuals and at-risk populations to combat the rapid spread of the Omicron variant. It can be seen from the epidemiological curves for Singapore and Israel that the implementation of these measures effectively delayed the spread of the early Omicron variant, leaving sufficient time for policy adjustments in response to the changes in the pandemic. The number of new COVID-19 cases per day in Singapore decreased from 1085 to 146 between November 26th, 2021 and December 20th, 2021. In Israel, although the number of new COVID-19 cases per day gradually increased from 542 to 1331, the pace was slow.
Vaccination Promotion to Achieve Herd Immunity to COVID-19
It is important to note that COVID-19 vaccinations play an extremely important role in reducing the severity of infection and disease and alleviating the economic burden imposed by the pandemic.28 For the Omicron variant, vaccination may not protect against infection or transmission but can reduce severe cases and mortality.29,31 Therefore, both Singapore and Israel used COVID-19 vaccination as a key strategy for achieving herd immunity during this phase of their public health programs. For example, the Green Pass program contributed to the promotion of vaccination in Israel, which initiated the first vaccination campaign, as well as the provision of booster shots. Based on the Israeli MOH report on May 2nd, 2022, 66.05% of Israelis received two doses of the COVID-19 vaccine, and 48.32% received a booster dose. In contrast to Israel, Singapore witnessed a very rapid increase in the COVID-19 vaccination rate, even though the vaccination campaign began almost half a month later, with booster doses administered about three months later. However, with the implementation of vaccination-differentiated safety management measures, a total of 89.28% of Singaporeans have received two doses of the COVID-19 vaccine and 72.18% have received a booster dose as of May 2nd, 2022.20 Compared with Israel, Singapore had a much higher vaccination rate. In addition, it is evident from the number of deaths and the prevalence of severe cases in Singapore and Israel during the first Omicron wave that Singapore performed better in terms of vaccination promotion. Due to the high vaccination rate in Singapore, there were significantly fewer severe cases and deaths during the first Omicron wave than in Israel. However, the high vaccination coverage in many countries cannot be easily replicated due to factors such as vaccine availability and disparities between the rich and the poor, which makes it essential to promote the global distribution of the COVID-19 vaccine on an equitable basis.32,33 Additionally, developing modified vaccines that protect against vaccine-resistant variants should be considered as another important issue.34
Strong Medical Service Capacity and Hierarchical Diagnosis and Treatment
The medical burden during the COVID-19 pandemic was associated with the mortality of hospitalized cases.35 Thus, efforts should be concentrated on the protection of severe cases, for whom early diagnosis and adequate treatment are essential. The implementation of this strategy is affected by two factors: the level of the healthcare system and the level of hierarchical diagnosis and treatment. A high level of healthcare capacity and a sophisticated hierarchical diagnosis and treatment system were instrumental in the success of controlling the pandemic in Singapore and Israel.
In terms of health care, Singapore and Israel rank among the world’s leading countries. Statistics from the WHO indicate that in 2020, the health expenditure per capita reached $3537 and $3867 in Singapore and Israel, respectively, which was well above the global average.36 In response to the SARS-CoV pandemic outbreak in 2002, Singapore has gradually developed a public health system including public health preparedness clinics, public hospitals, and a national infectious disease center.12,37 Also, the healthcare risk prevention and control system in Israel is one of the most advanced emergency response systems in the world, having been tested by wars, terrorist attacks, and outbreaks of infectious diseases.38
Furthermore, in Singapore, the primary care physician was responsible for determining the appropriate treatment for a patient infected with COVID-19 based on the patient’s health status and the severity of his/her symptoms. In Israel, community health care was highlighted to serve as a solid foundation for the implementation of hierarchical diagnosis and treatment for COVID-19 patients. For example, COVID-19 patients in Israel received treatment from a remote management center established by Maccabi Healthcare Services and staffed by a multidisciplinary team.39 Moreover, COVID-19 patients assigned to home recovery might receive medical support from appropriate medical institutions such as Singapore’s public health preparedness clinics and Israel’s community health facilities. Depending on these measures, patients recovering from COVID-19 at home could receive continuous medical monitoring and avoid delays by raising warning signs immediately. If the deterioration of their health was detected, they could be transferred to a higher-level hospital. Although the surge in infections challenged Singapore and Israel to some degree in terms of maintaining basic public health services, the two countries succeeded in avoiding the collapse of their health-care systems by implementing hierarchical diagnosis and treatment, which allows limited medical resources to be oriented toward the treatment of severe cases.
Comprehensive Prevention and Control Through Non-Pharmaceutical Interventions
The importance of non-pharmaceutical interventions in the control of infectious diseases is undeniable. In previous studies, non-pharmacological interventions such as social distancing have been proven to be effective in reducing the basic infection numbers in major metropolitan areas.40 Then research in Saudi Arabia further indicates that physical or social distancing is the most cost-saving but most effective control intervention in the absence of vaccination.41 Despite the high coverage of vaccines against COVID-19, vaccines alone cannot fully stop the spread of the virus and, therefore, must be combined with non-pharmaceutical interventions. The study of optimal control strategies shows that a combination of non-pharmaceutical interventions and vaccination can effectively control the COVID-19 pandemic by minimizing its social and economic costs.42 Early in the development of the epidemic, Israel announced upgraded requirements for gatherings, dinners, educational institutions, etc. and emphasized the necessity of wearing masks, etc. Meanwhile, Singapore always had community safety management measures centered on the 5 elements as an important part of its public health measures, maintaining the policy of wearing masks indoors until May 2nd, 2022. The results of a study on the effect of mask wearing on the transmission of COVID-19 suggest that the higher the rate of mask use was, the more rapidly the cumulative number of confirmed cases would decrease.43 As a result, the implementation of these measures played a significant role in cutting off the transmission route of the virus, preventing outbreaks of aggregated infections, as well as the occurrence of the peak of the epidemic. However, Israel significantly eased its social management measures after March 2022, with the Containment and Health Index decreasing from 58 in December 2021 to 38 in March 2022,44 causing the epidemic rebound. Similarly, the Containment and Health Index of Singapore dropped from 63 in March 2022 to 50 in early May 2022,44 witnessing another epidemic rebound as well. Thus, non-pharmaceutical interventions such as the policy of wearing masks should be retained as SARS-CoV-2 exists widely and new outbreaks may occur occasionally as a result of virus mutations.
Limitations
There are still some limitations in our study. Firstly, although the COVID-19 case data were collected from the official website of the MOH in Singapore and Israel, there could be some deviations due to differences in reporting, update time, data optimization, and other factors. Secondly, when assessing the effectiveness of public health measures, the impacts of factors, such as population structure, per capita GDP, air pollution, and religious beliefs45,48 were not considered.
Conclusion
To sum up, we have analyzed the policies and their effects during the first Omicron wave in Singapore and Israel and found that timely and strict border control measures and surveillance measures were more effective in preventing and controlling the rapid spread of COVID-19 variants in the early stage. Furthermore, promoting COVID-19 vaccination and booster shots as soon as possible, enhancing the capacity of medical services, improving the hierarchical medical system, and implementing non-pharmaceutical interventions are essential for the prevention and control of highly infectious COVID-19.
Data Sharing Statement
All data generated or analyzed during this study are included in this published article.
Ethics Approval and Consent to Participate
The Biomedical Ethics Committee of Southern Medical University confirmed: Gang Sun's paper “Policy Disparities Between Singapore and Israel in response to the First Omicron Wave” does not involve the category of medical ethics, so there is no need for medical ethics review.
Acknowledgement
The authors gratefully acknowledge the financial supports by the Natural Science Foundation of Guangdong Province in 2022: Construction and application of COVID-19 control model PSR-SOR-Haddon in Guangdong Province (No. 2022A1515011112).
Funding
This study was supported by the Natural Science Foundation of Guangdong Province in 2022: Construction and application of COVID-19 control model PSR-SOR-Haddon in Guangdong Province (No. 2022A1515011112).
Disclosure
The authors have no conflicts of interest to declare.
References
1. Araf Y, Akter F, TangY-D, et al. Omicron variant of SARS-CoV-2: genomics, transmissibility, and responses to current COVID-19 vaccines. J Med Virol. 2022;94(5):1825–1832. doi:10.1002/jmv.27588
2. Classification of Omicron (B.1.1.529): SARS-CoV-2 variant of concern. Available from: https://www.who.int/news/item/26-11-2021-classification-of-omicron-(b.1.1.529)-sars-cov-2-variant-of-concern.
3. Torjesen I. Covid-19: omicron may be more transmissible than other variants and partly resistant to existing vaccines, scientists fear. BMJ. 2021;n2943. doi:10.1136/bmj.n2943
4. Cele S, Jackson L, Khoury DS, et al. Omicron extensively but incompletely escapes Pfizer BNT162b2 neutralization. Nature. 2022;602(7898):654–656. doi:10.1038/s41586-021-04387-1
5. Chen J, Wang R, Gilby NB, Wei GW. Omicron variant (B.1.1.529): infectivity, vaccine breakthrough, and antibody resistance. J Chem Inf Model. 2022;62(2):412–422. doi:10.1021/acs.jcim.1c01451
6. Morita S, Nakagawa K. Evaluating the impact of human flow on the spread of infectious diseases. J Theor Biol. 2023;558:111367. doi:10.1016/j.jtbi.2022.111367
7. Health and climate change: country profile 2021: israel. Available from: https://www.who.int/publications-detail-redirect/WHO-HEP-ECH-CCH-22.01.06.
8. Country statistical profile: israel 2022/4 | country statistical profiles: key tables from OECD | OECD iLibrary. Available from: https://www.oecd-ilibrary.org/economics/country-statistical-profile-israel-2022-4_f4d0bd25-en.
9. Singapore Department of Statistics (DOS). Base. Available from: http://www.singstat.gov.sg/.
10. Division UNP. United Nation|By Location | pivot Table | data Portal|Population density. Population Division Data Portal. Available from: https://population.un.org/dataportal/data/indicators/54/locations/376/start/2020/end/2023/table/pivotbylocation.
11. SunG-Q, ZhangH-T, Chang-L-L, Jin Z, Wang H, Ruan S. On the dynamics of a diffusive foot-and-mouth disease model with nonlocal infections. SIAM J Appl Math. 2022;82(4):1587–1610. doi:10.1137/21M1412992
12. Kuguyo O, Kengne AP, Dandara C. Singapore COVID-19 pandemic response as a successful model framework for low-resource health care settings in Africa? Omics J Integr Biol. 2020;24(8):470–478. doi:10.1089/omi.2020.0077
13. Last M. The first wave of COVID-19 in Israel-Initial analysis of publicly available data. PLoS One. 2020;15(10):e0240393. doi:10.1371/journal.pone.0240393
14. Muhsen K, Na’aminh W, Lapidot Y, et al. A nationwide analysis of population group differences in the COVID-19 epidemic in Israel, February 2020–February 2021. Lancet Reg Health - Eur. 2021;7:100130. doi:10.1016/j.lanepe.2021.100130
15. Delavari S, Jamali Z, Bayati M. Lockdown effect on COVID-19 incidence and death: Iran experience. Disaster Med Public Health Prep. 2021;1–3. doi:10.1017/dmp.2021.222
16. Czypionka T, Iftekhar EN, Prainsack B, et al. The benefits, costs and feasibility of a low incidence COVID-19 strategy. Lancet Reg Health Eur. 2022;13:100294. doi:10.1016/j.lanepe.2021.100294
17. Bolzoni L, Bonacini E, Della marca R, Groppi M. Optimal control of epidemic size and duration with limited resources. Math Biosci. 2019;315:108232. doi:10.1016/j.mbs.2019.108232
18. Singapore Ministry of Health. Available from: https://www.moh.gov.sg/.
19. Israel Ministry of Health. Available from: https://datadashboard.health.gov.il/COVID-19/general.
20. Mathieu E, Ritchie H, Rodés-Guirao L, et al. Coronavirus Pandemic (COVID-19). Our World Data; 2020. Available from: https://ourworldindata.org/coronavirus.
21. COVID-19 Symptoms. Corona Traffic Light Model (Ramzor) Website. Available from: https://corona.health.gov.il/en/confirmed-cases-and-patients/common-symptoms/.
22. Israel services and government information website. Available from: https://www.gov.il/en.
23. Singapore Government Agency Website. Available from: https://www.gov.sg/.
24. Living normally, with Covid-19: task force ministers on how S’pore is drawing road map for new normal | the Straits Times. Available from: https://www.straitstimes.com/opinion/living-normally-with-covid-19.
25. Green Pass and Purple Badge Restrictions Lifted – public Updates and Guidance. GOV.IL. Available from: https://www.gov.il/en/departments/news/01062021-01.
26. Gwee SXW, Chua PEY, Wang MX, Pang J. Impact of travel ban implementation on COVID-19 spread in Singapore, Taiwan, Hong Kong and South Korea during the early phase of the pandemic: a comparative study. BMC Infect Dis. 2021;21(1):799. doi:10.1186/s12879-021-06449-1
27. Jiao J, Shi L, Chen H, et al. Containment strategy during the COVID-19 pandemic among three Asian low and middle-income countries. J Glob Health. 2022;12:05016. doi:10.7189/jogh.12.05016
28. Haas EJ, Angulo FJ, McLaughlin JM, et al. Impact and effectiveness of mRNA BNT162b2 vaccine against SARS-CoV-2 infections and COVID-19 cases, hospitalisations, and deaths following a nationwide vaccination campaign in Israel: an observational study using national surveillance data. Lancet Lond Engl. 2021;397(10287):1819–1829. doi:10.1016/S0140-6736(21)00947-8
29. Nyberg T, Ferguson NM, Nash SG, et al. Comparative analysis of the risks of hospitalisation and death associated with SARS-CoV-2 omicron (B.1.1.529) and delta (B.1.617.2) variants in England: a cohort study. Lancet Lond Engl. 2022;399(10332):1303–1312. doi:10.1016/S0140-6736(22)00462-7
30. Pérez-Then E, Lucas C, Monteiro VS, et al. Neutralizing antibodies against the SARS-CoV-2 Delta and Omicron variants following heterologous CoronaVac plus BNT162b2 booster vaccination. Nat Med. 2022;28(3):481–485. doi:10.1038/s41591-022-01705-6
31. Andrews N, Stowe J, Kirsebom F, et al. Covid-19 vaccine effectiveness against the Omicron (B.1.1.529) variant. N Engl J Med. 2022;386(16):1532–1546. doi:10.1056/NEJMoa2119451
32. Leshem E, Wilder-Smith A. COVID-19 vaccine impact in Israel and a way out of the pandemic. Lancet. 2021;397(10287):1783–1785. doi:10.1016/S0140-6736(21)01018-7
33. Yang M, Shi L, Chen H, et al. Comparison of COVID-19 vaccine policies in Italy, India, and South Africa. Vaccines. 2022;10(9):1554. doi:10.3390/vaccines10091554
34. Vuong QH, Le TT, La VP, et al. Covid-19 vaccines production and societal immunization under the serendipity-mindsponge-3D knowledge management theory and conceptual framework. Humanit Soc Sci Commun. 2022;9(1):1–12. doi:10.1057/s41599-022-01034-6
35. Rossman H, Meir T, Somer J, et al. Hospital load and increased COVID-19 related mortality in Israel. Nat Commun. 2021;12(1):1904. doi:10.1038/s41467-021-22214-z
36. Global Health Expenditure Database. Available from: https://apps.who.int/nha/database/ViewData/Indicators/en.
37. Chen H, Shi L, Zhang Y, et al. Response to the COVID-19 pandemic: comparison of strategies in six countries. Front Public Health. 2021;9:708496. doi:10.3389/fpubh.2021.708496
38. Zou H, Guo Y, Hu M, Ding J, Zheng N, Lu J. Construction and enlightenment of Israel′s medical and health care risk prevention system. Chin J Hosp Adm. 2019;11:966–967–968. doi:10.3760/cma.j.issn.1000-6672.2019.11.020
39. Shapiro Ben David S, Cohen D, Karplus R, et al. COVID-19 community care in Israel-a nationwide cohort study from a large health maintenance organization. J Public Health Oxf Engl. 2021;43(4):723–730. doi:10.1093/pubmed/fdab055
40. Pei S, Kandula S, Shaman J. Differential effects of intervention timing on COVID-19 spread in the United States. MedRxiv Prepr Serv Health Sci. 2020. doi:10.1101/2020.05.15.20103655
41. Asamoah JKK, Okyere E, Abidemi A, et al. Optimal control and comprehensive cost-effectiveness analysis for COVID-19. Results Phys. 2022;33:105177. doi:10.1016/j.rinp.2022.105177
42. Das P, Upadhyay RK, Misra AK, Rihan FA, Das P, Ghosh D. Mathematical model of COVID-19 with comorbidity and controlling using non-pharmaceutical interventions and vaccination. Nonlinear Dyn. 2021;106(2):1213–1227. doi:10.1007/s11071-021-06517-w
43. Ma X, Luo XF, Li L, Li Y, Sun GQ. The influence of mask use on the spread of COVID-19 during pandemic in New York City. Results Phys. 2022;34:105224. doi:10.1016/j.rinp.2022.105224
44. COVID-19 Containment and Health Index. Our World in Data. Available from: https://ourworldindata.org/grapher/covid-containment-and-health-index.
45. O’Driscoll M, Ribeiro Dos Santos G, Wang L, et al. Age-specific mortality and immunity patterns of SARS-CoV-2. Nature. 2021;590(7844):140–145. doi:10.1038/s41586-020-2918-0
46. Imam T, Uddin S. How do economic and public finance statuses affect policy responses during a pandemic? - learning from the COVID-19 first wave. BMC Public Health. 2022;22(1):785. doi:10.1186/s12889-022-13209-6
47. Sheridan C, Klompmaker J, Cummins S, James P, Fecht D, Roscoe C. Associations of air pollution with COVID-19 positivity, hospitalisations, and mortality: observational evidence from UK Biobank. Environ Pollut Barking Essex. 2022;308:119686. doi:10.1016/j.envpol.2022.119686
48. Gozum IE, Capulong HG, Gopez JM, Galang JR. Culture, religion and the state: towards a multidisciplinary approach to ensuring public health during the COVID-19 pandemic (and beyond). Risk Manag Healthc Policy. 2021;14:3395–3401. doi:10.2147/RMHP.S318716
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.