Back to Journals » Journal of Inflammation Research » Volume 15
Plasma and Urine Indoleamine 2,3-Dioxygenase Activity: Promising Biomarkers for Chronic Kidney Disease and Inflammation Status
Authors Hong H, Zhou S, Shi H, Li M
Received 15 June 2022
Accepted for publication 30 August 2022
Published 7 September 2022 Volume 2022:15 Pages 5129—5139
DOI https://doi.org/10.2147/JIR.S378594
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ning Quan
Hao Hong,1 Suya Zhou,2 Haimin Shi,3 Ming Li3
1Intensive Care Unit, The First Affiliated Hospital of Soochow University, Soochow, People’s Republic of China; 2Laboratory Nephrology, Department of Nephrology, Jinshan Hospital of Fudan University, Shanghai, People’s Republic of China; 3Laboratory Nephrology, The First Affiliated Hospital of Soochow University, Soochow, People’s Republic of China
Correspondence: Ming Li, Tel +86 13656237709, Fax +0512-67972681, Email [email protected]
Purpose: Our aim was to determine the relationship between plasma and urine indoleamine 2.3-dioxygenase (IDO) activity and stage of chronic kidney disease (CKD).
Patients and Methods: Demographic and clinical parameters, including plasma and urine IDO activity, were recorded in 47 CKD patients and 30 controls. One-way ANOVA with the least significant difference method was used to compare means of variables that had normal distributions and homogeneous variance. Variables with non-normal distributions were log-transformed and compared using the rank sum test Pearson or Spearman correlation coefficients were determined. Binary logistic regression and ordinal logistic regression were used to identify independently significant factors. Receiver operating characteristic (ROC) analysis was performed.
Results: The control group had higher levels of hemoglobin and albumin and lower levels of creatinine and blood urea nitrogen (BUN; all P< 0.01). The level of highly sensitive C reactive protein (hs-CRP) increased as CKD stage increased (P< 0.01). Plasma and urine IDO activity were positively correlated (r=0.7, P< 0.01). Plasma IDO activity correlated with age, creatinine, BUN, triglycerides, uric acid, albumin, and hemoglobin (all P< 0.05); urine IDO activity correlated with age, BMI, creatinine, BUN, and hemoglobin (all P< 0.05). There were positive correlations of hs-CRP level with plasma IDO activity and urine IDO activity (both P< 0.01). After adjusting for CKD-related factors, plasma IDO activity, urine IDO activity, and hs-CRP were independent risk factors for CKD (all P< 0.05). Ordinal logistic regression also indicated that plasma and urine IDO activity were significantly associated with CKD stage. ROC analysis indicated that plasma and urine IDO activity were good predictors of CKD and distinguished different stages of CKD. There was a strong correlation between plasma IDO activity and inflammatory status in patients with CKD (OR=1258.908, P< 0.01).
Conclusion: Plasma and urine IDO activity have potential use as biomarkers for early-stage CKD, progression of CKD, and inflammation status.
Keywords: tryptophan rate-limiting enzyme, inflammatory, hs-CRP, liquid chromatography-mass spectrometry
Introduction
Chronic Kidney Disease (CKD) is a major threat to public health throughout the world, and it has a prevalence of about 10.8% in China.1 Thus, CKD is one of the most common non-communicable chronic diseases, is associated with high morbidity, and is responsible for extensive healthcare costs. As CKD progresses, patients experience significant somatic symptoms, reduced health-associated life quality, and extensive lifestyle limitations.2,3 Clinicians commonly measure the serum levels of creatinine and cystatin C to assess CKD severity. However, these markers are not sensitive enough for the early diagnosis of CKD and do not have high diagnostic specificity. The pathogenesis and progression of CKD is complex and incompletely elucidated, but CKD is related to many factors, such as the chronic inflammatory state and immune disorders. Therefore, it is very important to develop improved methods for early detection of CKD and to further examine the mechanism of CKD progression.
Indoleamine 2.3-dioxygenase (IDO) is a heme-containing monomeric enzyme that catalyzes the conversion of tryptophan (TRP) into kynurenine (KYN) and is the rate-limiting enzyme in the TRP-KYN pathway. IDO has immunomodulatory effects due to its important role in tryptophan metabolism. These effects include down-regulation of T cells, control of inflammation, and immune tolerance. Recent studies of cancer patients suggested that innate responses during tumorigenesis can up-regulate IDO, and that IDO can increase the response to immunotherapy. For example, Thüring et al reported that urine IDO had prognostic value in patients undergoing radical prostatectomy. These same mechanisms are also important in the development and progression of CKD.4,5
Huttunen et al found that the level of IDO was closely related to inflammatory status and mortality in patients with sepsis.6 Some studies in China found that the inhibition of IDO may ameliorate renal fibrosis.7 Some individuals who have heart failure or infectious diseases, or are vegetarians may have altered immune status and elevation of IDO,8 and IDO is elevated in diabetes patients who have CKD.9 An elevated plasma IDO level is indicative of the inflammatory state and immune disorders, and there is also a positive association of plasma IDO activity with CKD progression.10
Previous research that examined the relationship of IDO with CKD mainly focused on changes of plasma IDO activity. There is little is known about the changes of urine IDO activity during the onset and progression of CKD. In the present study, we used liquid chromatography-mass spectrometry (LC-MS) to examine changes of plasma and urine IDO activity during CKD.
Materials and Methods
Subject Screening
A total of 47 patients and 30 controls were recruited from the First Affiliated Hospital of Soochow University (Suzhou, Jiangsu) from March to June 2018. These two groups were matched for age and BMI. Subjects who had any of the following characteristics were excluded: age less than 18 years; acute kidney injury; severe arrhythmia or heart failure; severe hemodynamic disorder; active infectious disease or use of an antibiotic; strict vegetarianism; a solitary kidney; participation in professional athletics; pregnancy, lactating, or having a menstrual period; mental illness or inability to cooperate; cancer; or autoimmune-related nephritis. All included patients (but none of the controls) had confirmed diagnoses of CKD based on the Kidney Disease Improving Global Outcome (KDIGO) guideline.11
This study was approved by the Ethics Committee of the First Affiliated Hospital of Soochow University (Ethics Research Association No. 079). Each study subject signed an informed consent document. Our study was complied with the Declaration of Helsinki.
Laboratory Measurements
Routine laboratory parameters were measured. Creatinine, uric acid, blood urea nitrogen, triglycerides, total cholesterol, albumin, and blood glucose were determined using the OLYMPUS AU2700 automatic biochemical analyzer (Olympus, Japan). Hemoglobin was determined using the Beckman LH750 automatic blood analyzer (Beckman, U.S.A.). Highly sensitive C reactive protein (hs-CRP) was measured using the OLYMPUS AU2700 Automatic Biochemical Analyzer (Olympus, Japan). TRP and KYN levels in plasma and urine samples were determined by LC (Ultimate 3000, Thermo, USA) and MS (Q Exactive, Thermo, U.S.A.). Chromatographic separation was accomplished in an Thermo Ultimate 3000 system equipped with an ACQUITY UPLC® HSS T3 (150×2.1 mm, 1.8 µm, Waters) column maintained at 40°C. The temperature of the autosampler was 8°C. Gradient elution of analytes was carried out with 0.1% formic acid in water (A) and 0.1% formic acid in acetonitrile (B) or 5mM ammonium formate in water (C) and acetonitrile (D) at a flow rate of 0.25mL/min. Injection of 2μL of each sample was done after equilibration. An increasing linear gradient of solvent B (v/v) was used as follows: 0~1 min, 2% B/D; 1~9 min, 2%~50% B/D; 9~14 min, 50%~98% B/D; 14~15 min, 98% B/D; 15~15.5 min, 98%~2% B/D; 15.5~17 min, 2%B/D. The ESI-MSn experiments were executed on the Thermo Q Exactive Focus mass spectrometer with the spray voltage of 3.8 kV and −2.5 kV in positive and negative modes, respectively. Sheath gas and auxiliary gas were set at 45 and 15 arbitrary units, respectively. The capillary temperature was 325 °C, respectively. The Orbitrap analyzer scanned over a mass range of m/z 81–1000 for full scan at a mass resolution of 70,000. Data dependent acquisition (DDA) MS/MS experiments were performed with HCD scan. The normalized collision energy was 30 eV. Dynamic exclusion was implemented to remove some unnecessary information. IDO activity was expressed as the ratio of KYN to TRP, as previously described.12,13
Definition of CKD
All CKD patients had CKD stage 1 to 4 (CKD1–4), determined using the KIDGO guideline. The Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation was used to calculate eGFR.14
Statistical Analysis
Statistical analysis was performed using SPSS version 22.0. Data with normal distributions were expressed as means ± SDs, and data with non-normal distributions as medians and interquartile ranges (IQRs). A one-way ANOVA was used to compare means when variables had normal distributions and homogeneous variance, followed by the least significant difference (LSD) test. The rank sum test was used for comparisons of variables that had non-normal distributions. Pearson or Spearman correlation analysis was used to determine the correlations of IDO activity with other indices. Binary logistic regression and ordinal logistic regression were used to determine the independent relationship of different factors with CKD. Receiver operating characteristic (ROC) curves were plotted to evaluate the accuracy of IDO activity in the diagnosis of CKD. The best cut-off for the ROC curve was calculated using Youden’s index. P values below 0.05 (*) and below 0.01 (**) were considered statistically significant.
Results
Clinical Characteristics of CKD Patients and Controls
We examined 77 subjects, 47 patients with different stages of CKD and 30 controls without CKD (Table 1). All CKD patients were initially diagnosed from March to June 2018 and a very small number of them had CKD4 with mild hypertension and gastrointestinal symptoms. We initially assessed the normality and homogeneity of variance of all clinical variables in the control and CKD groups. Age, hemoglobin, and uric acid had normal distributions with homogeneous variances, so we used the LSD method for comparisons. After natural log transformation, body mass index (BMI), creatinine, BUN, and triglycerides had normal distributions and homogeneous variances, so we used the LSD method for comparisons. Albumin, total cholesterol, and blood glucose did not have normal distributions after natural logarithm transformation, so we used the rank sum test for comparisons. Thus, relative to all 47 CKD patients, the control group had higher levels of hemoglobin and albumin, and lower levels of Ln (creatinine) and Ln (BUN) (all P < 0.01).
 |
Table 1 Clinical Characteristics of CKD Patients and Controls |
IDO Activity in CKD Patients and Controls
Measurements of plasma and urine IDO activity indicated significant differences between controls and patients with early-stage CKD, and that the levels of both markers increased with the progression of CKD stage (Figure 1). However, the controls and patients with CKD1 had no significant differences in plasma or urine IDO activity.
Correlations of IDO Activity with Clinical Indices
Logistic regression analysis indicated that there was a strong curvilinear correlation between plasma IDO activity and urine IDO activity (r = 0.7, P < 0.01, Figure 2). We also examined the correlation of plasma and urine IDO with other clinical indices (Figure 3). The results indicated plasma IDO activity had positive correlations with age (r = 0.3, P < 0.05), creatinine (r = 0.8, P < 0.01), BUN (r = 0.8, P < 0.01), triglycerides (r = 0.3, P < 0.05), and uric acid (r = 0.4, P < 0.01), and negative correlations with albumin (r = –0.4, P < 0.01) and hemoglobin (r = –0.5, P < 0.01). Urine IDO activity had positive correlations with age (r = 0.3, P < 0.05), BMI (r = 0.3, P < 0.05), creatinine (r = 0.6, P <0.01), and BUN (r = 0.6, P < 0.01), and a negative correlation with hemoglobin (r = –0.4, P < 0.01).
 |
Figure 3 Relationship of plasma and urine IDO activities with different clinical indices. Pearson correlation coefficients was applied. Abbreviation: IDO, indoleamine 2,3-dioxygenase. |
Logistic Regression Analysis of Factors Associated with CKD
We performed binary logistic regression analysis to assess the relationship of plasma and urine IDO with CKD. Before adjustment for confounding, CKD was associated with plasma IDO activity (OR = 1144.061, P < 0.01) and urine IDO activity (OR = 2.438, P < 0.01). After adjustment for confounding by hemoglobin, Ln (BUN), plasma IDO, and urine IDO, ordinal logistic regression (Table 2) indicated that CKD had a very strong and significant relationship with IDO activity (OR = 283.157, P < 0.01), and also had significant relationships with Ln (BUN) (OR = 7.660, P = 0.025), and urine IDO activity (OR = 1.231, P < 0.05).
 |
Table 2 Ordinal Logistic Regression Analysis of Risk Factors Independently Associated with CKD |
Plasma and Urine IDO Activity for Prediction of CKD and CKD Stage
We performed ROC analysis to determine the value of plasma and urine IDO activity in predicting CKD by comparing all 47 CKD patients with the 30 controls (Figure 4A). For plasma IDO activity, the area under the curve (AUC) was 0.833 (95% CI: 0.744–0.923, P < 0.01), the best cut-off value was 0.563, the sensitivity was 69.6%, and the specificity was 86.7%. For urine IDO activity, the AUC was 0.742 (95% CI: 0.633–0.851, P<0.01), the best cut‐off value was 0.413, the sensitivity was 41.3%, and the specificity was 100%. Thus, plasma IDO activity and urine IDO activity each provided reliable predictions of CKD.
We also used ROC analysis to determine the value of plasma and urine IDO activity in distinguishing different stages of CKD. Analysis of the control and CKD2 groups indicated that plasma IDO activity had an AUC of 0.839 (95% CI: 0.714–0.965, P < 0.01), best cut‐off value of 0.618, sensitivity of 81.8%, and specificity of 80.0% (Figure 4B). Analysis of the CKD1 and CKD2 groups indicated plasma IDO activity had an AUC of 0.783 (95% CI: 0.595–0.971, P < 0.05), best cut‐off value of 0.587, sensitivity of 81.8%, and a specificity of 76.9% (Figure 4C). Analysis of the CKD2 and CKD3 groups indicated that plasma IDO activity had an AUC of 0.942 (95% CI: 0.852–1.000, P < 0.01), best cut‐off value of 0.727, sensitivity of 90.9%, and specificity of 81.8% (Figure 4D). Analysis of CKD3 and CKD4 groups indicated that plasma IDO activity had an AUC of 0.769 (95% CI: 0.556–0.981, P < 0.05), best cut‐off value of 0.545, sensitivity of 72.7%, and specificity of 81.8% (Figure 4E). Notably, urine IDO activity also reliably distinguished the different stages of CKD (Figure 4B–E), with AUC values ranging from 0.748 to 0.793, sensitivity ranging from 72.7% to 90.9%, and specificity ranging from 69.2% to 72.7%.
Relationship of Hs-CRP with CKD Stage
We also compared the levels of hs-CRP (a widely used inflammatory indicator) in different patients (Figure 5). The results indicated significant differences between the CKD1 and CKD2 groups, and between the CKD1 and CKD4 groups (both P < 0.01).
 |
Figure 5 Hs-CRP in CKD patients. Changes of hs-CRP in CKD stage 1–4. **P<0.01. Abbreviations: hs-CRP, highly sensitive C reactive protein; CKD, chronic kidney disease. |
Hs-CRP for Prediction of CKD Stage
We performed ROC analysis to assess the value of hs-CRP for the diagnosis of CKD stage. Comparison of CKD1 and CKD2 groups indicated the AUC was 0.951 (95% CI: 0.873–1.000, P < 0.01), best cut‐off value was 0.769, sensitivity was 100%, and specificity was 76.9% (Figure 6A). Comparison of the CKD2 and CKD3 groups indicated the AUC was 0.760 (95% CI: 0.528–0.992, P < 0.05), best cut‐off value was 0.636, sensitivity was 81.8%, and specificity was 81.8% (Figure 6B).
Correlations of Plasma and Urine IDO Activity with Hs-CRP
Pearson correlation analysis (Table 3) indicated that there were significantly positive correlations of hs-CRP with plasma IDO activity (r = 0.658, P < 0.01) and urine IDO activity (r = 0.534, P < 0.01).
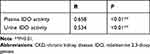 |
Table 3 Pearson Correlation of Plasma and Urine IDO Activity with Hs-CRP |
Logistic Regression Analysis of the Association of Inflammation with CKD
Ordinal logistic regression (Table 4) indicated that CKD was associated with three inflammatory factors: plasma IDO activity (OR = 1258, P < 0.01), urine IDO activity (OR = 1.334, P = 0.013), and hs-CRP (OR = 1.557, P = 0.012).
 |
Table 4 Ordinal Logistic Regression Analysis of the Association of Inflammatory Factors with CKD |
Discussion
We used LC-MS to measure plasma and urine IDO activity in healthy controls and patients who had different stages of CKD. To our knowledge, this is the first study to determine the relationship of plasma and urine IDO activity with CKD stage. Our comparison of controls with all CKD patients indicated CKD had a strong association with plasma IDO activity (OR = 1144.061, P < 0.01) and urine IDO activity (OR = 2.438, P < 0.01). Moreover, our ROC analysis indicated that plasma and urine IDO activity distinguished patients with different stages of CKD. We also found positive associations of hs-CRP with plasma IDO activity and urine IDO activity (both P < 0.01), and that hs-CRP was also associated with CKD stage. Our results suggest that changes in plasma and urine IDO activity may help to identify patients with early-stage CKD and to monitor the progression of CKD. We suggest that additional studies should measure the effect of different cutoffs and detection methods. Our results also suggest that IDO activity may indicate the immune-inflammatory status of CKD patients. Very few studies have examined the effect of IDO inhibitors or agonists on CKD. We suggest careful examination of this topic in the future, because IDO inhibitors appear to have promise as a new treatment of CKD-related immune disorders and inflammation. Moreover, because IDO itself has immunomodulatory effects, caution should be used when interpreting IDO levels in CKD patients who are using immunomodulatory agents.
IDO is the rate-limiting enzyme of the TRP-KYN pathway, and disruption of this pathway is associated with several renal diseases and other conditions. In particular, abnormalities of this pathway, presumably due to alterations of IDO activity, are present in patients with IgA nephropathy, diabetic nephropathy, and renal cell carcinoma.15 However, very few previous studies examined changes of urine IDO activity in CKD patients. We found that plasma and urine IDO activity were significantly up-regulated in CKD patients, and that patients with more advanced CKD had greater elevations (all P < 0.05). The elevation of IDO activity in the plasma and urine of CKD patients suggests that a change of IDO activity and an abnormality of the TRP-KYN pathway may function in the pathogenesis of CKD.
Based on AUC values, we found that plasma and urine IDO levels reliably distinguished controls from patients with CKD. It is well known that patients with CKD1 and CKD2 have mostly normal or only slightly impaired renal function with no symptoms, and those with CKD3 and CKD4 have moderate to severe disruption of renal function. If patients with early-stage CKD are not promptly identified and given timely treatment, they could eventually progress to later-stage CKD or even end-stage renal disease. Our findings suggest that measurements of plasma and urine IDO activity may help to identify patients with early-stage CKD, and thereby allow clinicians to take appropriate steps to prevent further deterioration of renal function.
The specific mechanism underlying the relationship of increased IDO activity with CKD is still not clear. Renal fibrosis is a major factor that contributes to deterioration of renal function, and some previous research showed that IDO activity was gradually up-regulated during the progression of renal fibrosis.16 On the contrary, Matheus et al found that 1-methyl tryptophan (1-MT), an IDO inhibitor, promoted the accumulation of collagen and progression of the epithelial–mesenchymal transition, suggesting that IDO had protective effects.17 Changes in IDO are also associated with renal ischemia-reperfusion injury and hypoxic preconditioning.18,19 Other research reported that the metabolites upstream and downstream of IDO accumulated with the progression of CKD, and these metabolites may contribute to a variety of CKD complications, such as thrombosis and dyslipidemia.20,21 Our previous studies also identified changes in these metabolites.22 These many results suggest that changes of IDO activity and in the levels of metabolites in the TRP-KYN pathway may jointly affect the progression of CKD.
Some evidence suggests that IDO could play an indispensable role in immune regulation and establishment of the inflammatory state.23 The immunosuppression induced by IDO could allow tumor cells to achieve immune escape, leading to increased survival and dissemination of tumor cells.24 Moreover, the IDO-mediated increase of Treg cells can normalize the ratio of Th17/Treg cells, and this may provide protection from the progression of CKD.25 Most studies showed that IDO was an inflammatory factor, and that it was gradually up-regulated with the progression of inflammation.26,27 hs-CRP is a commonly used and easily measured inflammatory marker in CKD patients.28,29 Our measurements of hs-CRP indicated that this marker was upregulated in all stages of CKD, and there were significant differences between groups with different stages of CKD. Notably, the hs-CRP level was greater in CKD2 relative to CKD1 (P < 0.01). We also showed that plasma and urine IDO activity were positively correlated with hs-CRP (both P < 0.01). In agreement, Niinisalo et al also reported a correlation between plasma IDO activity and hs-CRP.30 We also found that plasma IDO activity had a strong correlation with CKD stage (OR = 1258.908, P < 0.01). However, it remains unknown whether an elevated IDO level promoted the pathogenesis of CKD or was a protective response to CKD progression. Recent studies showed that the increase of Treg cells induced by IDO could alleviate the inflammatory state.31,32 Rapamycin can coordinate the immune response of cells and stimulate inflammation due to its interaction with intracellular and extracellular factors.33 IDO can also induce macrophages and dendritic cells to secrete anti-inflammatory factors.34 This suggests that IDO activity may have complex effects on the inflammatory state in patients with CKD.
There were some limitations in the present study. Firstly, our sample size was rather small and all patients were from a single institution. Secondly, we did not examine IDO activity in any patients with CKD5.
Conclusion
Our findings indicated that measurements of plasma and urine IDO activity have potential use for predicting renal inflammation and the progression of CKD.
Acknowledgments
We thank Medjaden Inc. for scientific editing of this manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Zhang L, Wang F, Wang L., et al. Prevalence of chronic kidney disease in China: a cross-sectional survey. Lancet. 2012;379(9818):815–822. doi:10.1016/S0140-6736(12)60033-6
2. Huang CW, Wee PH, Low LL, et al. Prevalence and risk factors for elevated anxiety symptoms and anxiety disorders in chronic kidney disease: a systematic review and meta-analysis. Gen Hosp Psychiatry. 2021;69:27–40. doi:10.1016/j.genhosppsych.2020.12.003
3. Wee HL, Seng BJ, Lee JJ, et al. Association of anemia and mineral and bone disorder with health-related quality of life in Asian pre-dialysis patients. Health Qual Life Outcomes. 2016;14(1):94. doi:10.1186/s12955-016-0477-8
4. Munn DH, Mellor AL. IDO in the tumor microenvironment: inflammation, counter-regulation, and tolerance. Trends Immunol. 2016;37(3):193–207. doi:10.1016/j.it.2016.01.002
5. Thüring M, Knuchel R, Picchetta L, et al. The prognostic value of indoleamine-2,3-dioxygenase gene expression in urine of prostate cancer patients undergoing radical prostatectomy as first treatment of choice. Front Immunol. 2020;11:1244. doi:10.3389/fimmu.2020.01244
6. Huttunen R, Syrjänen J, Aittoniemi J, et al. High activity of indoleamine 2,3 dioxygenase enzyme predicts disease severity and case fatality in bacteremic patients. Shock. 2010;33(2):149–154. doi:10.1097/SHK.0b013e3181ad3195
7. Pan B, Zhang H, Hong Y, et al. Indoleamine-2,3-dioxygenase activates wnt/β-catenin inducing kidney fibrosis after acute kidney injury. Gerontology. 2021;67(5):611–619. doi:10.1159/000515041
8. Zhang C, Björkman A, Cai K, et al. Impact of a 3-months vegetarian diet on the gut microbiota and immune repertoire. Front Immunol. 2018;9:908. doi:10.3389/fimmu.2018.00908
9. Zhang Y, Ruan Y, Zhang P, et al. Increased indoleamine 2,3-dioxygenase activity in type 2 diabetic nephropathy. J Diabetes Complications. 2017;31(1):223–227. doi:10.1016/j.jdiacomp.2016.08.020
10. Schefold JC, Zeden JP, Fotopoulou C, et al. Increased indoleamine 2,3-dioxygenase (IDO) activity and elevated serum levels of tryptophan catabolites in patients with chronic kidney disease: a possible link between chronic inflammation and uraemic symptoms. Nephrol Dial Transplant. 2009;24(6):1901–1908. doi:10.1093/ndt/gfn739
11. Inker LA, Astor BC, Fox CH, et al. KDOQI US commentary on the 2012 KDIGO clinical practice guideline for the evaluation and management of CKD. Am J Kidney Dis. 2014;63(5):713–735. doi:10.1053/j.ajkd.2014.01.416
12. Wang W, Huang L, Jin JY, et al. A validation study on IDO immune biomarkers for survival prediction in non-small cell lung cancer: radiation dose fractionation effect in early-stage disease. Clin Cancer Res. 2020;26(1):282–289. doi:10.1158/1078-0432.CCR-19-1202
13. Adu-Gyamfi C, Savulescu D, Mikhathani L, et al. Plasma kynurenine-to-tryptophan ratio, a highly sensitive blood-based diagnostic tool for tuberculosis in pregnant women living with Human Immunodeficiency Virus (HIV). Clin Infect Dis. 2021;73(6):1027–1036. doi:10.1093/cid/ciab232
14. Levey AS, Inker LA, Coresh J. GFR estimation: from physiology to public health. Am J Kidney Dis. 2014;63(5):820–834. doi:10.1053/j.ajkd.2013.12.006
15. Platten M, Nollen EAA, Röhrig UF, et al. Tryptophan metabolism as a common therapeutic target in cancer, neurodegeneration and beyond. Nat Rev Drug Discov. 2019;18(5):379–401. doi:10.1038/s41573-019-0016-5
16. Shi Y, Wang Y, Li Q, et al. Immunoregulatory mechanisms of mesenchymal stem and stromal cells in inflammatory diseases. Nat Rev Nephrol. 2018;14(8):493–507. doi:10.1038/s41581-018-0023-5
17. Matheus LHG, Simão GM, Amaral TA, et al. Indoleamine 2, 3-dioxygenase (IDO) increases during renal fibrogenesis and its inhibition potentiates TGF-β 1-induced epithelial to mesenchymal transition. BMC Nephrol. 2017;18(1):287. doi:10.1186/s12882-017-0702-7
18. Čepcová D, Kema IP, Sandovici M, et al. The protective effect of 1-methyltryptophan isomers in renal ischemia-reperfusion injury is not exclusively dependent on indolamine 2,3-dioxygenase inhibition. Biomed Pharmacother. 2021;135:111180. doi:10.1016/j.biopha.2020.111180
19. Torosyan R, Huang S, Bommi PV, et al. Hypoxic preconditioning protects against ischemic kidney injury through the IDO1/kynurenine pathway. Cell Rep. 2021;36(7):109547. doi:10.1016/j.celrep.2021.109547
20. Walker JA, Richards S, Whelan SA, et al. Indoleamine 2,3-dioxygenase-1, a novel therapeutic target for post-vascular injury thrombosis in CKD. J Am Soc Nephrol. 2021;32(11):2834–2850. doi:10.1681/ASN.2020091310
21. Ketelhuth DFJ. The immunometabolic role of indoleamine 2,3-dioxygenase in atherosclerotic cardiovascular disease: immune homeostatic mechanisms in the artery wall. Cardiovasc Res. 2019;115(9):1408–1415. doi:10.1093/cvr/cvz067
22. Hao H, Suya Z, Yue C, et al. Analysis of tryptophan-kynurenine pathway in 47 non-dialysis patients with chronic kidney disease[J]. Chin J Kidney Dis Investig. 2020;9(6):247–252.
23. Lemos H, Huang L, Prendergast GC, et al. Immune control by amino acid catabolism during tumorigenesis and therapy. Nat Rev Cancer. 2019;19(3):162–175. doi:10.1038/s41568-019-0106-z
24. Zhai L, Bell A, Ladomersky E, et al. Tumor cell IDO enhances immune suppression and decreases survival independent of tryptophan metabolism in glioblastoma. Clin Cancer Res. 2021;27(23):6514–6528. doi:10.1158/1078-0432.CCR-21-1392
25. Li Q, Liu J, Fan H, et al. IDO-inhibitor potentiated immunogenic chemotherapy abolishes primary tumor growth and eradicates metastatic lesions by targeting distinct compartments within tumor microenvironment. Biomaterials. 2021;269:120388. doi:10.1016/j.biomaterials.2020.120388
26. Andersen MH. The T-win® technology: immune-modulating vaccines. Semin Immunopathol. 2019;41(1):87–95. doi:10.1007/s00281-018-0695-8
27. Parra ER, Villalobos P, Zhang J, et al. Immunohistochemical and image analysis-based study shows that several immune checkpoints are co-expressed in non-small cell lung carcinoma tumors. J Thorac Oncol. 2018;13(6):779–791. doi:10.1016/j.jtho.2018.03.002
28. Zheng HJ, Guo J, Wang Q, et al. Probiotics, prebiotics, and synbiotics for the improvement of metabolic profiles in patients with chronic kidney disease: a systematic review and meta-analysis of randomized controlled trials. Crit Rev Food Sci Nutr. 2021;61(4):577–598. doi:10.1080/10408398.2020.1740645
29. Uchiyama K, Adachi K, Muraoka K, et al. Home-based aerobic exercise and resistance training for severe chronic kidney disease: a randomized controlled trial. J Cachexia Sarcopenia Muscle. 2021;12(6):1789–1802. doi:10.1002/jcsm.12775
30. Niinisalo P, Raitakari OT, Kähönen M, et al. IDO activity forecasts obesity in males and premenopausal females in a 10-year follow-up study: the Cardiovascular Risk in Young Finns Study. Atherosclerosis. 2021;336:32–38. doi:10.1016/j.atherosclerosis.2021.09.018
31. Lu J, Liu X, Liao YP, et al. Breast cancer chemo-immunotherapy through liposomal delivery of an immunogenic cell death stimulus plus interference in the IDO-1 pathway. ACS Nano. 2018;12(11):11041–11061. doi:10.1021/acsnano.8b05189
32. Lukas D, Yogev N, Kel JM, et al. TGF-β inhibitor Smad7 regulates dendritic cell-induced autoimmunity. Proc Natl Acad Sci U S A. 2017;114(8):E1480–E1489. doi:10.1073/pnas.1615065114
33. Correale J. Immunosuppressive amino-acid catabolizing enzymes in multiple sclerosis. Front Immunol. 2021;11:600428. doi:10.3389/fimmu.2020.600428
34. Sharma MD, Pacholczyk R, Shi H, et al. Inhibition of the BTK-IDO-mTOR axis promotes differentiation of monocyte-lineage dendritic cells and enhances anti-tumor T cell immunity. Immunity. 2021;54(10):2354–2371.e8. doi:10.1016/j.immuni.2021.09.005
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




