Back to Journals » Clinical Interventions in Aging » Volume 18
Physical Activity Mediates the Relationship Between Sarcopenia and Cognitive Function Among Older Adults in Nursing Homes
Authors Yao X, Liu B, Hua N, Huang J, Zhao X
Received 9 June 2023
Accepted for publication 5 November 2023
Published 13 November 2023 Volume 2023:18 Pages 1863—1871
DOI https://doi.org/10.2147/CIA.S425271
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Prof. Dr. Nandu Goswami
Xuemei Yao,1 Beibei Liu,2 Nan Hua,2 Jiaoling Huang,2 Xin Zhao1
1Neurosurgical Intensive Care Unit, the First Affiliated Hospital of Xi’an Jiaotong University, Xi’an, Shanxi Province, People’s Republic of China; 2Xiangya School of Nursing, Central South University, Changsha, Hunan Province, People’s Republic of China
Correspondence: Xin Zhao, Tel +86-173-9387-4096, Email [email protected]
Purpose: Sarcopenia and physical activity are significant factors influencing cognitive function. However, few studies have examined their underlying mechanisms between the three conditions. The aim of the study is to examine the mediating role of physical activity in the relationship between sarcopenia and cognitive function in elderly nursing home residents.
Materials and Methods: A total of 420 older adults aged 60 years and above in nursing homes participated in this study. Sarcopenia was defined following the Asian Sarcopenia Working Group (AWGS) 2019 criteria. Cognitive function was assessed by the Mini-Mental State Examination (MMSE). Multiple linear regression analysis was employed to explore the relationships between sarcopenia, cognitive function and physical activity. Mediation analyses were performed to examine whether physical activity moderates the relationship between sarcopenia and cognitive function, with the use of PROCESS macro version 4.0.
Results: A total of 386 older adults were included in the analysis (mean age 80.30 years), 175 (45.3%) were assessed as cognitive impairment, and sarcopenia was more common in those with cognitive impairment (p < 0.01). The linear regression analysis indicated that there were significant associations between sarcopenia and physical activity (β = − 0.285, p = 0.012), physical activity and cognitive function (β = 0.218, p < 0.001), and sarcopenia and cognitive function (β = − 0.245, p = 0.021). Mediating effects of physical activity on the association between sarcopenia and cognitive function were observed in participants, with 20.2% of partial mediating effect.
Conclusion: The results of the study suggest physical activity may partially buffer the adverse effects of sarcopenia on cognitive impairment among the older adults in nursing homes. Accordingly, engagement in physical activity can help to preserve cognitive function among those with sarcopenia.
Keywords: cognitive impairment, sarcopenia, physical activity, older adults
Introduction
The elderly population is growing steadily around the world, including in China.1 The extension of average life expectancy and the advancement of the birth cohort have led to changes in the internal structure of the elderly population. After 2030, there will be a rapid increase in the proportion of elderly individuals over the age of 80 in China.2 With changes in family models, the traditional family care model has become increasingly challenging to fulfill new functions. Moreover, older adults with lower self-care abilities are more likely to opt for nursing homes that can provide professional care due to poorer health and increased life expectancy.3 Nursing homes in China play a crucial role in providing care for the older adults.
As a consequence of the rise in numbers of older adults, age-related diseases or syndromes are expected to affect more older adults. Cognitive impairment is characterized by a decline in cognition involving one or more cognitive domains, such as attention, memory, reasoning, executive ability, directivity and language.4 Cognitive impairment affects quality of life and health,5,6 increases the risk of progression to dementia, and creates burdens on families,7 which is one of the most important risk factor of the need for long-term care and institutionalization of older adults.8
Sarcopenia is an age-related muscle disease characterized by general and progressive loss of skeletal muscle mass and declined muscle function.9 Accumulating evidence reported that sarcopenia and its defining components, mainly low muscle strength and low physical performance, are associated with worse performance in global cognitive function, and various aspects of cognition, including language, memory,10 directivity,11 recall and executive function.12 In addition, several studies have confirmed that older adults with impaired cognition are at higher risk of developing sarcopenia.8,9
In view of considerable health consequences of sarcopenia and cognitive impairment and associations between the two variables, researchers have been working to seek factors that may help prevent sarcopenia and cognitive decline during the aging. Whilst cognitive impairment and dementia are prevalent among the older adults, no curative treatments or approved drugs by the US Food and Drug Administration for these conditions are available.13,14 There is also no definitive medication for sarcopenia.9 Therefore, researchers are interested in identifying modifiable factors that may protect older population from cognitive decline and sarcopenia. Such modifiable variables could serve as a basis for developing interventions. As a simple and safe behavior modality, physical activity, moderate-to-vigorous physical activity in particular, has been found to be beneficial for cognitive function in older adults as well as for delaying development and slow down the rate of sarcopenia.9,13–15 Robust findings on exercise and brain health also suggest that a muscle-brain endocrine loop exists, which at least in part may be mediated by myokine signaling.16,17 Myokines are cytokines produced and released by skeletal muscle, an endocrine organ.16 It has been found that physical activity and exercise can facilitate an increase in the circulating levels of myokines in the bloodstream, which have beneficial effects on the brain, such as cognition, memory, and learning and mood.16,18 However, in addition to reduced myokine production due to muscle mass damage and muscle weakness, older adults with sarcopenia tend to have lower muscle strength and poorer physical performance, which may negatively affect their motor function and the production of myokines, and subsequently have an impact on cognition.
Thus, we hypothesized that physical activity levels mediate the relationship between sarcopenia and cognitive impairment. A mediation analysis was performed among elderly people to examine whether sarcopenia influences cognitive function through the indirect effect of the mediating variable of physical activity. Elucidation of the relationship between these three variables may facilitate the widespread adoption of physical activity- related interventions in older adults with sarcopenia.
Materials and Methods
Participants
During June to November 2021, we invited the older adults living in nursing homes in Changsha city, Hunan province, China, to participate in this study. The inclusion criteria for participants were residents who had been in a nursing facility for 1 month and more, and age ≥60 years. The following were the exclusion criteria: (1) unable to communicate with the study staff; (2) inability to perform the handgrip strength test; (3) had a severe hearing impairment or blindness; (4) had a known diagnosis of dementia. According to the principle that the sample size should be 5 to 10 times the number of independent variables, the estimated sample size was 75 to 150. Considering a 20% of invalid questionnaires and measurements, we increased the sample size to 180. The study was conducted in accordance with the Declaration of Helsinki and had been approved by the Research Ethics Committee of Central South University (E2021132). All participants also signed written informed consent after they were provided with a detailed explanation of the study protocol.
Sarcopenia Screening
Sarcopenia was defined following the Asian Sarcopenia Working Group (AWGS) 2019 criteria, ie participants with low skeletal muscle mass and low muscle strength or low physical performance were considered to have sarcopenia.9 Skeletal muscle mass was measured with a multifrequency Bioelectrical Impedance Analysis (BIA) (Inbody S10, South Korea), expressed as Skeletal Muscle mass Index (SMI). SMI was calculated by dividing Appendicular Skeletal Muscle mass (ASM) by the square of height (in meter). SMI <7.0 kg/m2 for males and <5.7kg/m2 for females indicated low muscle mass. Handgrip strength (HGS) was measured with a digital hand dynamometer (Xiangshan, Guangdong, China) to evaluate muscle strength. Participants were instructed to squeeze the dynamometer 2 times with their dominant hand with 30-second pauses in seated position, and the higher value was recorded.19 HGS <28kg in males and <18kg in females were considered to have low muscle strength. Usual gait speed (GS) was the most frequently used test of physical performance.9 Participants were asked to walk 10-m straight course at their usual pace, permitting the use of a walking aid if necessary. Researchers recorded middle 6-m uniform pass time. The gait speed is equal to 6 m divided by the recorded time. Low physical performance was defined as usual gait speed <1m/s.
Assessment of Cognitive Function
Cognitive function was assessed by the Mini-Mental State Examination (MMSE) in the study, which was validated for Chinese older adults.20 MMSE is a 30-item test covering five dimensions of orientation, memory, calculation, recall and language and is widely used to screen cognitive function in the older adults. Scores of MMSE range from 0 to 30, and cognitive impairment was defined as a score of <17 for illiterate participants, <20 for participants who had undergone education for 1 to 6 years, and <24 for participants who had undergone education for more than 7 years. The Chinese version of the MMSE is highly sensitive and specific in the detection of dementia in the Chinese population.21
Assessment of Physical Activity
Physical activity levels were assessed by the Chinese Version of the Physical Activity Scale for the Elderly (PASE). The PASE is a valid and applicable scale that is often used in practice. The scale evaluates the physical activities of the elderly within the previous one week and covers the physical components of leisure, household, and occupational activities. It consists of 10 categories and 26 specific questions. PASE scores are calculated by multiplying activity weights and activity frequency, and the total PASE score is the sum of the scores for each activity.22 Qiu J et al verified the validity and reliability of the Chinese version of PASE in Chinese older adults, and its reliability and validity were 0.505 and 0.897, respectively, indicating that the scale can effectively and objectively measure the physical activity level of Chinese older adults.23
Covariates
A face-to-face, one-on-one personal interview was performed to collect general information of the participants regarding age, gender, education level, smoking status, alcohol consumption, and disease-related information. The education of participants was classified into three levels: illiteracy and primary school, junior high school, and senior high school and above. Participants were divided into three groups based on whether or not they smoked: non-smokers, quitters, and current smokers.
Current smokers were defined as smoking at least one cigarette per day for at least the past 6 months, and quitters were defined as having quitting smoking for more than the 6 months prior to the survey.24 Drinking status was classified as above, ie, never, quitters, and current drinkers.
Current drinkers were defined as drinking regularly and lasted at least 6 months, and quitters were defined as drinking regularly in the past and not drinking with the previous year.24 Also, the following three common chronic diseases were also evaluated: hypertension, diabetes, and coronary heart disease. Participants were considered as having chronic illness if they self-reported having been told by a physician that they have above conditions. Weight (kg) was measured with a standard electronic scale and height (m) with an infrared height meter, and the values were accurate to 0.1cm and 0.1kg. Body mass index (BMI) is the ratio of weight to height squared. Nutrition status was assessed by the Mini Nutritional Assessment Short-Form (MNA-SF). The MNA-SF is a validated nutritional assessment tool designed for the elderly. It consists of six questions related to weight loss, food intake, mobility, psychological stress or acute diseases, and body mass index (BMI) or calf circumference.25 The total score of the MNA-SF is 14 points, with ≥12 points being nourished, 8–11 points being at risk of malnutrition, and ≤7 being malnourished.
Statistical Analyses
All statistical analyses were done by using IBM SPSS version 25.0 (IBM SPSS Inc, Chicago, IL), and p<0.05 was considered statistically significant. Continuous variable data with a normal distribution were expressed as mean ± standard deviation, whereas data with a non-normal distribution were expressed by median and quartile. Categorical variable data were represented by frequency and percentage. Differences in variables were compared between participants with and without cognitive impairment using independent t-test, chi-square test and Mann–Whitney U-test. Multiple linear regression analysis was conducted to investigate the relationships between sarcopenia, cognitive function and physical activity.
Mediation analyses were performed to examine whether physical activity (mediator) moderates the relationship between sarcopenia (independent variable) and cognitive function (dependent variable), with the use of Hayes’ PROCESS macro version 4.0 for SPSS. PROCESS is a statistical tool for path analysis-based mediation, moderation, and conditional indirect effect analyses.26 Statistical mediation analysis was conducted using nonparametric bootstrapping with 5000 replications to calculate bias-corrected bootstrapped 95% confidence intervals (CIs). An indirect effect was considered significant if the 95% CI excluded zero.
Results
Characteristics of Participants
Of 420 older adults originally enrolled in the study, 34 were excluded due to incomplete questionnaire and anthropometric data. Ultimately, 386 were included in the current analysis. The mean age of participants was 80.3 ± 9.18 years and 219 (56.7%) were female. Table 1 shows the characteristics of participants according to cognitive status. Of all the participants, 175 (45.3%) were assessed as cognitively impaired based on the MMSE scores. Individuals with cognitive impairment were older and less educated (p < 0.05), but the differences in gender were not significant (p = 0.953). The differences in smoking and alcohol consumption between the two groups were not significant (p > 0.05). As for the chronic diseases, differences in the frequency of cognitive impairment were significant for whether participants had hypertension (p = 0.008) but not for the presence of diabetes mellitus (p = 0.323) and coronary heart disease (p = 0.181). Participants with cognitive impairment had lower levels of physical activity in comparison to those without cognitive impairment (p < 0.001), but there was no difference in the frequency of malnutrition or risk of malnutrition (p = 0.106).
 |
Table 1 Characteristics of Participants According to Cognitive Impairment |
The prevalence of sarcopenia was 49.7% in the present study, and higher in the participants with cognitive impairment (p < 0.001). Participants with cognitive impairment had lower grip strength, SMI and gait speed (p < 0.05).
Associations Between Sarcopenia, Physical Activity, and Cognitive Function
Table 2 represents the results of linear regression analysis in the mediation model adjusted for age, gender, educational levels, smoking, alcohol consumption, hypertension, diabetes mellitus, coronary heart disease, BMI, and nutritional status. The results suggested that there were significant associations between sarcopenia and physical activity (β = −0.285, p = 0.012), physical activity and cognitive function (β = 0.218, p < 0.001), and sarcopenia and cognitive function (β = −0.245, p = 0.021). Figure 1 shows the mediation model.
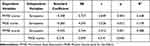 |
Table 2 Multiple Linear Regression Analysis in Mediation Model |
 |
Figure 1 Mediation model of MMSE score (cognitive status). *p<0.05; **p<0.005. |
As shown in Table 3, the bootstrap 95% CI of direct effect (−3.185, −0.258) and indirect effect (−0.831, −0.100) exclude zero, which suggested a partial mediating effect of physical activity. The percentage of the total effect mediated by physical activity was 20.2%.
 |
Table 3 Mediation Models: Total, Direct and Indirect Effects |
Discussion
The results of the study demonstrated that sarcopenia may negatively influence the cognitive function among the older adults in nursing home, but this adverse association could be counteracted if there is more physical activity. Therefore, physical activity may positively influence the detrimental effect of sarcopenia for cognitive function. Older adults with sarcopenia who are more physically active are less likely to develop cognitive impairment, because the association between sarcopenia and cognitive impairment was mediated for physical activity.
Cognitive impairment seriously affects the daily activities and quality of life of the older adults, leading to an increase in their care needs, which is also one of the major contributing factors for the older adults to live in nursing homes.8 In this study, the prevalence of cognitive impairment was 45.3%, indicating that approximately half of nursing home residents have cognitive impairment of varying degrees. The prevalence of cognitive impairment and dementia among older adults in nursing homes varied widely in previous studies, ranging from 4% to 87.4%.27,28 A meta-analysis of 53 observational studies reported that the overall prevalence of cognitive impairment among elderly people in nursing homes was 21.2%,29 higher than 12.2% in the community populations.30 There are several reasons for this discrepancy. Cognitive impairment is one of the most common reasons for admission to nursing homes, which will result in a higher rate of cognitive impairment in nursing home residents than community-dwelling populations. In addition, older adults in nursing homes are known to have worse overall health, with many physical and psychiatric disorders that contribute to cognitive decline, such as diabetes,31 chronic pain,28 and depression.32
Sarcopenia has been found to be associated with poorer cognitive performance in both cross-sectional and longitudinal studies.33,34 Moreover, sarcopenia is prevalent in individuals with cognitive impairment or dementia.35,36 The present study also discovered similar results, with sarcopenia negatively associated with cognitive function as assessed by the MMSE, and more than half of the participants with cognitive impairment (60%) were considered to have sarcopenia. The results suggest that the concomitant presence of sarcopenia and cognitive impairment is common among elderly people in nursing facilities. Thus, appropriate interventions for these two common geriatric syndromes are needed.
Insufficient physical activity is known to be an important risk factor for sarcopenia,9,37 however, few studies have considered the influence of sarcopenia on physical activity among older adults. The study found that sarcopenia was negatively associated with physical activity levels, suggesting older adults with sarcopenia engaged in less physical activity. The finding is consistent with a previous study in which Mijnarends et al observed during a five-year follow-up that older adults with sarcopenia tended to engage significantly less in physical activity.38 This is not surprising, as older adults with sarcopenia tend to have significantly reduced muscle strength and muscle mass, which diminishes their physical function and may affect their ability to perform physical activities. A population-based longitudinal study found a linear positive correlation between handgrip strength and physical activity levels in older adults, and those with improved handgrip strength were more likely to increase their time spent in physical activity.39 In addition, several studies reported that older adults with sarcopenia experienced more falls,40,41 which may also be preventing them from being physically active.
The present study investigated the role of physical activity between sarcopenia and cognitive function. A significant mediating effect of physical activity on the correlation between sarcopenia and cognitive impairment was observed. The results suggested that physical activity may buffer the adverse effects of sarcopenia on cognitive function. Multiple studies have shown that physical activity and exercise serve to positively influence cognitive function throughout the lifespan, and that great physical activity is associated with a reduced likelihood of cognitive decline and dementia.13,14 It has been reported that physical exercise increases the volume and intensifies the prefrontal cortex function, hippocampus, which are neuronal regions related to cognition and memory.42 The presence of the muscle-brain endocrine ring may also support the finding. Myokines secreted by skeletal muscle play a crucial role in regulating brain functions such as mood, learning, motor activity, and also provide protection against neuronal damage.16,18 Research has demonstrated that physical activity stimulates the secretion and release of myokines, which in turn enhances and sustains brain functions, including cognition.16,17 However, due to the loss of muscle mass and muscle weakness, individuals with sarcopenia experience a decrease in myokines, as well as less physical activity. These links between sarcopenia, physical activity and cognitive function may provide evidence for this mediating pathway.
The mediating effect of physical activity accounts for 20.2% of the total effect, indicating the partial mediating effect of physical activity in the relationship between sarcopenia and cognitive function. Partial mediation may imply that it is not the only relationship path. Other mediating variables are worth exploring in the future. It has been found that nutritional status also has a significant mediating effect on the relationship between sarcopenia and cognitive function.43 In addition to physical activity and nutritional status, other mediating variables, such as emotion and sleep quality, may also exist in the influence path of sarcopenia on cognitive function, which requires further research.
There were certain limitations in the study. First, this was a cross-sectional observational study, so we could not clearly elucidate a causal relationship between sarcopenia and cognitive function in older adults. Future longitudinal studies are warranted to provide more stronger evidence of causality. Second, the study only included the older adults in nursing homes and the sample size was relatively small, so the results should be interpreted with caution. Additional researches in other populations with larger sample size are needed to validate our findings. Third, cognitive function is a broad term encompasses various aspects of how individuals acquire and process information. Physical activity may be associated with various cognitive domains in different manners. This current study only explored the relationships between sarcopenia, physical activity and global cognition as assessed by the MMSE and did not analyze the relationship with specific cognitive domains, such as memory and executive function.
Conclusion
In summary, the study found that sarcopenia was associated with cognitive impairment among the older adults in nursing homes, and the relationship was partially mediated by physical activity levels. Accordingly, engagement in physical activity can help to preserve cognitive function among those with sarcopenia. These findings may identify underlying the relationships between sarcopenia and cognitive function, as well as provide an opportunity for early detection and intervention of cognitive decline among the older adults.
Ethics Approval and Informed Consent
The study was conducted in accordance with the Declaration of Helsinki and had been approved by the Research Ethics Committee of Central South University (E2021132). All participants also signed a written informed consent after they were provided with a detailed explanation of the study protocol.
Acknowledgments
We thank all participants for the time dedicated to the study, and we are also grateful to professor Xiuhua Wang for her advice and guidance.
Funding
This study was funded by the Hunan Provincial Development and Reform Commission (number: 212).
Disclosure
All authors declared that they have no conflicts of interest in this work.
References
1. Liu D. Development status, causes and countermeasures of population aging in China. Chine J Gerontol. 2022;42(16):4123–4126. doi:10.3969/j.issn.1005-9202.2022.16.071
2. Chen W. Prediction of negative population growth and aging trend in China. Social Sci j. 2022;2022(5):133–144. doi:10.13262/j.bjsshkxy.bjshkx.230810
3. Chu LW, Chi I. Nursing homes in China. J Am Med Dir Assoc. 2008;9(4):237–243. doi:10.1016/j.jamda.2008.01.008
4. Gao M, Kuang W, Qiu P, Wang H, Lv X, Yang M. The time trends of cognitive impairment incidence among older Chinese people in the community: based on the CLHLS cohorts from 1998 to 2014. Article Age and Ageing. 2017;46(5):787–793. doi:10.1093/ageing/afx038
5. Hoang CL, Ha GH, Pham KTH, et al. Global Mapping of Interventions to Improve Quality of Life of Patients with Alzheimer’s Disease during 1990-2018. Dement Geriatr Cogn Disord. 2019;48(5–6):221–233. doi:10.1159/000505741
6. Kobayashi LC, Wardle J, Wolf MS, von Wagner C. Cognitive Function and Health Literacy Decline in a Cohort of Aging English Adults. J Gen Intern Med. 2015;30(7):958–964. doi:10.1007/s11606-015-3206-9
7. Roberts R, Knopman DS. Classification and Epidemiology of MCI. Clin Geriatr Med. 2013;29(4):753. doi:10.1016/j.cger.2013.07.003
8. Peng TC, Chen WL, Wu LW, Chang YW, Kao TW. Sarcopenia and cognitive impairment: a systematic review and meta-analysis. Clin Nutr. 2020;39(9):2695–2701. doi:10.1016/j.clnu.2019.12.014
9. Chen LK, Woo J, Assantachai P, et al. Asian Working Group for Sarcopenia: 2019 Consensus Update on Sarcopenia Diagnosis and Treatment. J Am Med Dir Assoc. 2020;21(3):300–307.e2. doi:10.1016/j.jamda.2019.12.012
10. Szlejf C, Suemoto CK, Lotufo PA, Benseñor IM. Association of Sarcopenia With Performance on Multiple Cognitive Domains: results From the ELSA-Brasil Study. J Gerontol a Biol Sci Med Sci. 2019;74(11):1805–1811. doi:10.1093/gerona/glz118
11. Wang H, Zhang H, Chen Y, Cai M, Guo C, Chen P. Association between walking speed and cognitive domain functions in Chinese suburban-dwelling older adults. Front Aging Neurosci. 2022;14:935291. doi:10.3389/fnagi.2022.935291
12. Bai A, Xu W, Sun J, et al. Associations of sarcopenia and its defining components with cognitive function in community-dwelling oldest old. BMC Geriatr. 2021;21(1):292. doi:10.1186/s12877-021-02190-1
13. Lissek V, Suchan B. Preventing dementia? Interventional approaches in mild cognitive impairment. Neurosci Biobehav Rev. 2021;122:143–164. doi:10.1016/j.neubiorev.2020.12.022
14. Dominguez LJ, Veronese N, Vernuccio L, et al. Nutrition, Physical Activity, and Other Lifestyle Factors in the Prevention of Cognitive Decline and Dementia. Nutrients. 2021;13(11). doi:10.3390/nu13114080
15. Huang X, Zhao X, Li B, et al. Comparative efficacy of various exercise interventions on cognitive function in patients with mild cognitive impairment or dementia: a systematic review and network meta-analysis. J Sport Health Sci. 2022;11(2):212–223. doi:10.1016/j.jshs.2021.05.003
16. Pedersen BK. Physical activity and muscle-brain crosstalk. Nat Rev Endocrinol. 2019;15(7):383–392. doi:10.1038/s41574-019-0174-x
17. Severinsen MCK, Pedersen BK. Muscle-Organ Crosstalk: the Emerging Roles of Myokines. Endocr Rev. 2020;41(4):bnaa016. doi:10.1210/endrev/bnaa016
18. Scisciola L, Fontanella RA. Sarcopenia and Cognitive Function: role of Myokines in Muscle Brain Cross-Talk. Life-Basel. 2021;11(2):173. doi:10.3390/life11020173
19. Duan Y, Wang N. Advance in Hand Grip Measurement. Chine J Rehabilitation Theory Practice. 2009;15(10):948–951. doi:10.3969/j.issn.1006-9771.2009.10.015
20. Katzman R, Zhang MY, Ouang Ya Q, et al. A Chinese version of the Mini-Mental State Examination; impact of illiteracy in a Shanghai dementia survey. J Clin Epidemiol. 1988;41(10):971–978. doi:10.1016/0895-4356(88)90034-0
21. Zhang ZX, Zahner GE, Román GC, et al. Socio-demographic variation of dementia subtypes in China: methodology and results of a prevalence study in Beijing, Chengdu, Shanghai, and Xian. Neuroepidemiology. 2006;27(4):177–187. doi:10.1159/000096131
22. Washburn RA, Smith KW, Jette AM, Janney CA. The Physical Activity Scale for the Elderly (PASE): development and evaluation. J Clin Epidemiol. 1993;46(2):153–162. doi:10.1016/0895-4356(93)90053-4
23. Hongjun Y, Jun Q. Physical Activity Scale for Elderly (PASE): a Reliability-Validity Study for Physical Activity of Chinese Elderly. J Shanghai Univ Sport. 2014;38(05):45–49+60. doi:10.16099/j.cnki.jsus.2014.05.027
24. He H, Pan L, Pa L, et al. Data Resource Profile: the China National Health Survey (CNHS). Int J Epidemiol. 2018;47(6):1734–1735f. doi:10.1093/ije/dyy151
25. Kaiser MJ, Bauer JM, Ramsch C, et al. Validation of the Mini Nutritional Assessment short-form (MNA-SF): a practical tool for identification of nutritional status. J Nutr Health Aging. 2009;13(9):782–788. doi:10.1007/s12603-009-0214-7
26. Preacher KJ, Rucker DD, Hayes AF. Addressing Moderated Mediation Hypotheses: theory, Methods, and Prescriptions. Multivariate Behav Res. 2007;42(1):185–227. doi:10.1080/00273170701341316
27. Hayajneh AA, Rababa M, Alghwiri AA, Masha’al D. Factors influencing the deterioration from cognitive decline of normal aging to dementia among nursing home residents. BMC Geriatr. 2020;20(1):479. doi:10.1186/s12877-020-01875-3
28. Björk S, Juthberg C, Lindkvist M, et al. Exploring the prevalence and variance of cognitive impairment, pain, neuropsychiatric symptoms and ADL dependency among persons living in nursing homes; a cross-sectional study. BMC Geriatr. 2016;16(1):154. doi:10.1186/s12877-016-0328-9
29. Chen P, Cai H, Bai W, et al. Global prevalence of mild cognitive impairment among older adults living in nursing homes: a meta-analysis and systematic review of epidemiological surveys. Transl Psychiatry. 2023;13(1):88. doi:10.1038/s41398-023-02361-1
30. Lu Y, Liu C, Yu D, et al. Prevalence of mild cognitive impairment in community-dwelling Chinese populations aged over 55 years: a meta-analysis and systematic review. BMC Geriatr. 2021;21(1):10. doi:10.1186/s12877-020-01948-3
31. Bo M, Gallo S, Zanocchi M, et al. Prevalence, Clinical Correlates, and Use of Glucose-Lowering Drugs among Older Patients with Type 2 Diabetes Living in Long-Term Care Facilities. J Diabetes Res. 2015;2015:174316. doi:10.1155/2015/174316
32. McCusker J, Cole MG, Voyer P, et al. Observer-rated depression in long-term care: frequency and risk factors. Arch Gerontol Geriatr. 2014;58(3):332–338. doi:10.1016/j.archger.2013.11.010
33. Jacob L, Kostev K, Smith L, et al. Sarcopenia and Mild Cognitive Impairment in Older Adults from Six Low- and Middle-Income Countries. J Alzheimers Dis. 2021;82(4):1745–1754. doi:10.3233/jad-210321
34. Salinas-Rodríguez A, Palazuelos-González R, Rivera-Almaraz A, Manrique-Espinoza B. Longitudinal association of sarcopenia and mild cognitive impairment among older Mexican adults. J Cachexia Sarcopenia Muscle. 2021;12(6):1848–1859. doi:10.1002/jcsm.12787
35. Pacifico J, Geerlings MAJ, Reijnierse EM, Phassouliotis C, Lim WK, Maier AB. Prevalence of sarcopenia as a comorbid disease: a systematic review and meta-analysis. Exp Gerontol. 2020;131:110801. doi:10.1016/j.exger.2019.110801
36. Yang Y, Xiao M, Leng L, et al. A systematic review and meta-analysis of the prevalence and correlation of mild cognitive impairment in sarcopenia. J Cachexia Sarcopenia Muscle. 2023;14(1):45–56. doi:10.1002/jcsm.13143
37. Scott D, Johansson J, Gandham A, Ebeling PR, Nordstrom P, Nordstrom A. Associations of accelerometer-determined physical activity and sedentary behavior with sarcopenia and incident falls over 12 months in community-dwelling Swedish older adults. J Sport Health Sci. 2021;10(5):577–584. doi:10.1016/j.jshs.2020.01.006
38. Mijnarends DM, Koster A, Schols JM, et al. Physical activity and incidence of sarcopenia: the population-based AGES-Reykjavik Study. Age Ageing. 2016;45(5):614–620. doi:10.1093/ageing/afw090
39. Cooper A, Lamb M, Sharp SJ, Simmons RK, Griffin SJ. Bidirectional association between physical activity and muscular strength in older adults: results from the UK Biobank study. Int J Epidemiol. 2017;46(1):141–148. doi:10.1093/ije/dyw054
40. Zhang X, Huang P, Dou Q, et al. Falls among older adults with sarcopenia dwelling in nursing home or community: a meta-analysis. Clin Nutr. 2020;39(1):33–39. doi:10.1016/j.clnu.2019.01.002
41. Matsumoto H, Tanimura C, Tanishima S, Osaki M, Noma H, Hagino H. Sarcopenia is a risk factor for falling in independently living Japanese older adults: a 2-year prospective cohort study of the GAINA study. Geriatr Gerontol Int. 2017;17(11):2124–2130. doi:10.1111/ggi.13047
42. Voss MW, Erickson KI, Prakash RS, et al. Neurobiological markers of exercise-related brain plasticity in older adults. Brain Behav Immun. 2013;28:90–99. doi:10.1016/j.bbi.2012.10.021
43. Hu F, Liu H, Liu X, et al. Nutritional status mediates the relationship between sarcopenia and cognitive impairment: findings from the WCHAT study. Aging Clin Exp Res. 2021;33(12):3215–3222. doi:10.1007/s40520-021-01883-2
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
