Back to Journals » International Journal of Women's Health » Volume 15
Perspectives on the Use of Placental Growth Factor (PlGF) in the Prediction and Diagnosis of Pre-Eclampsia: Recent Insights and Future Steps
Authors Creswell L, O'Gorman N, Palmer KR, da Silva Costa F , Rolnik DL
Received 11 November 2022
Accepted for publication 3 February 2023
Published 13 February 2023 Volume 2023:15 Pages 255—271
DOI https://doi.org/10.2147/IJWH.S368454
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Elie Al-Chaer
Lyndsay Creswell,1 Neil O’Gorman,1 Kirsten Rebecca Palmer,2 Fabricio da Silva Costa,3 Daniel Lorber Rolnik2
1Coombe Women and Infants University Hospital, Dublin, Ireland; 2Department of Obstetrics and Gynaecology, Monash University, Melbourne, Victoria, Australia; 3Maternal Fetal Medicine Unit, Gold Coast University Hospital and School of Medicine and Dentistry, Griffith University, Gold Coast, Queensland, Australia
Correspondence: Lyndsay Creswell, Coombe Women and Infants University Hospital, Cork Street, Dublin, D08XW7X, Ireland, Tel +44 7754235257, Email [email protected]
Abstract: Pre-eclampsia (PE) is a complex multisystem disease of pregnancy that is becoming increasingly recognized as a state of angiogenic imbalance characterized by low concentrations of placental growth factor (PlGF) and elevated soluble fms-like tyrosine kinase (sFlt-1). PlGF is a protein highly expressed by the placenta with vasculogenic and angiogenic properties, which has a central role in spiral artery remodeling and the development of a low-resistance placental capillary network. PlGF concentrations are significantly lower in women with preterm PE, and these reduced levels have been shown to precede the clinical onset of disease. Subsequently, the clinical utility of maternal serum PlGF has been extensively studied in singleton gestations from as early as 11 to 13 weeks’ gestation, utilizing a validated multimarker prediction model, which performs superiorly to the National Institute for Health and Care Excellence (NICE) and American College of Obstetricians and Gynecologists (ACOG) guidelines in the detection of preterm PE. There is extensive research highlighting the role of PlGF-based testing utilizing commercially available assays in accelerating the diagnosis of PE in symptomatic women over 20 weeks’ gestation and predicting time-to-delivery, allowing individualized risk stratification and appropriate antenatal surveillance to be determined. “Real-world” data has shown that interpretation of PlGF-based test results can aid clinicians in improving maternal outcomes and a growing body of evidence has implied a role for sFlt-1/PlGF in the prognostication of adverse pregnancy and perinatal events. Subsequently, PlGF-based testing is increasingly being implemented into obstetric practice and is advocated by NICE. This literature review aims to provide healthcare professionals with an understanding of the role of angiogenic biomarkers in PE and discuss the evidence for PlGF-based screening and triage. Prospective studies are warranted to explore if its implementation significantly improves perinatal outcomes, explore the value of repeat PlGF testing, and its use in multiple pregnancies.
Keywords: pre-eclampsia, biomarkers, PlGF, sFlt-1, screening, aspirin, prevention, prediction, pregnancy complications
Introduction
Pre-eclampsia (PE) is a complex multisystem disorder of pregnancy, characterized by the new onset or progression of hypertension with signs of maternal end-organ or fetoplacental dysfunction, at or after 20 weeks’ gestation, and complicates 2–8% of pregnancies.1 PE is an important cause of global maternal and perinatal morbidity and mortality, with an estimated 70,000 maternal deaths directly attributable to the condition each year.1,2 PE is a disorder that encompasses a wide spectrum of disease, with variable onset and clinical course. Women who meet the diagnostic criteria for PE can range from asymptomatic at term with mildly elevated blood pressure and proteinuria, to patients at a periviable gestation with seizures and evidence of multi-organ failure. Whilst delivery of the fetus and placenta is the definitive treatment for PE, there is growing evidence of significant long-term morbidity for affected women, who remain at greater risk of cardiovascular and cerebrovascular disease years after pregnancy.3–5 It is uncertain presently if these long-term health consequences are due to underlying risk factors associated with PE, or the disease mechanism itself.
The definition of PE is constantly evolving; the International Society for the Study of Hypertension in Pregnancy (ISSHP) recommends that significant proteinuria is no longer essential for the diagnosis in the presence of neurological, biochemical, or hematological abnormalities or severe uteroplacental disease (Box 1). In comparison to the traditional description of PE, this broader definition encompassing evidence of uteroplacental dysfunction appears to better identify women and fetuses at risk of adverse outcomes including major maternal and perinatal morbidity,1,6 but also captures women with milder disease phenotypes.7
 |
Box 1 International Society for the Study of Hypertension in Pregnancy (ISSHP) Definition of Pre-Eclampsia (2018) |
Diagnosis based on clinical signs including hypertension and proteinuria is subject to observer error and poorly predicts adverse outcomes.8–10 Many features of the condition are non-specific and thus it is estimated that approximately 30% of all pregnancies will undergo evaluation for PE.11 This necessitates repeat hospital attendances and resource utilization for women with ambiguous presentations who require additional antenatal surveillance.12
PE is also the most common cause of iatrogenic prematurity and is implicated in over one-fifth of preterm births.13 Morbidity and mortality in prematurity is inversely related to the gestational age at birth, with infants born extremely premature at greatest risk of severe complications including cerebral palsy, neurodevelopmental delay and bronchopulmonary dysplasia.14,15 Early, effective identification of women at high risk for PE is a clinical priority, given the known benefits of aspirin prophylaxis, commenced prior to 16 weeks’ gestation, in preventing preterm PE in this cohort.16 Efforts should be concentrated on moving the focus of antenatal surveillance from reactive to predictive, thus inverting the pyramid of prenatal care.17
The exact etiology of PE is incompletely understood; however, it is largely accepted that malperfusion of the uteroplacental unit is central to its pathophysiology. The “two-stage model” has been postulated to explain the pathophysiology of preterm PE, occurring secondary to inadequate trophoblastic remodeling of the spiral arteries.18–20 It is this defective placentation, and failure to establish a high volume, low-resistance uteroplacental blood supply, which triggers a resultant “maternal syndrome” of endothelial dysfunction and intravascular inflammation, altering the equilibrium of placental angiogenic factors, including PlGF and culminating in the clinical signs of PE including hypertension and proteinuria.21,22 It has also been hypothesized that PE may not be a primary placental disorder, with uteroplacental hypoperfusion and endothelial dysfunction occurring secondary to suboptimal maternal cardiovascular adaptation.23 This is biologically plausible, as both PE and cardiovascular disease share multiple risk factors including obesity, advanced maternal age, diabetes mellitus and chronic kidney disease,23, and there is emerging evidence from clinical echocardiographic studies that maladaptation of the maternal cardiovascular system precedes the development of term PE.24 Indeed, villous and vascular placental lesions, previously assumed to be characteristic of PE, have been shown to be neither sensitive nor specific markers for the disease and found in greater abundance in placentae from uncomplicated gestations.25
Studies have demonstrated that circulating angiogenic proteins have an important biological role in the pathophysiology of PE and may be utilized in the prediction, screening, diagnosis, and prognostication of adverse disease outcomes.26–28 PlGF has been shown to have a particularly important role in first trimester prediction of PE and has a good diagnostic capacity in symptomatic women after 20 weeks’ gestation.27,28
This literature review will appraise and evaluate the evidence for PlGF testing in the prediction and diagnosis of PE and discuss its potential future applications including serial biomarker testing and use in twin pregnancies.
Angiogenic Factors
PlGF is a member of the VEGF family and potentiates the angiogenic response of VEGF.29 PlGF exists structurally as a glycosylated dimeric protein with both angiogenic and vasculogenic properties influencing trophoblastic growth, differentiation, and invasion into the maternal decidua.30–33 The plgf gene, located on chromosome 14q.14, encodes four isoforms of PlGF, of which PlGF-1 and -2 are most abundant during pregnancy and are prominently expressed in villous trophoblast cells.34 Whilst PlGF shows 53% homology in structure to VEGF-A, there are structural differences between the various isoforms with PlGF-2 and PlGF-4 possessing additional heparin-binding domains.34
sFlt-1, a splice variant of the VEGFR-1 receptor, is a circulating anti-angiogenic protein that acts as a potent VEGF and PlGF antagonist, inducing endothelial dysfunction.21 The placenta is the major source of sFlt-1 in the maternal circulation with serum levels in PE up to five times greater than those in normotensive women.21 Whilst this excess of sFlt-1 is mediated by the placenta in PE, exogenously administered sFlt-1 induces the clinical and pathological findings of PE in both pregnant and non-pregnant animal models, indicating the direct effect of sFlt-1 is on the endothelium irrespective of the presence of a placenta.21
Placental expression of PlGF increases in the second trimester corresponding to a “second wave” of spiral artery remodeling at 16 to 18 weeks’ gestation.34 From 25 weeks’ PlGF is believed to contribute to a change in branching to non-branching angiogenesis, controlling the expansion of a low-resistance placental capillary network.35–37
PlGF concentrations reach a peak between 29 and 32 weeks, then fall progressively until term.38,39 Whilst PlGF expression is upregulated in response to pathological injury in non-trophoblastic cells, the expression of trophoblastic PlGF is specifically inhibited in response to placental hypoxia, a consequence of uteroplacental ischemia.34
Accurate and early detection of high-risk patients provides a significant opportunity for clinicians to implement an effective screen-and-prevent protocol in contrast to reacting to the clinical signs of PE, which are late features of the disease. Reduced levels of PlGF are evident from as early as 11–13 weeks’ gestation which provides an opportunity for screening at the time of the first trimester booking appointment.39–41
First Trimester Prediction of PE Utilizing PlGF
Serum concentrations of PlGF vary considerably with maternal characteristics and comorbidities; levels are greater in parous women, cigarette smokers, and in individuals of Afro-Caribbean, South Asian, and East Asian origin, and are lower in women with obesity or insulin-dependent diabetes mellitus.42–44 Consequently, it is necessary to adjust for these variables and other variations in biomarker testing and assay analysis to standardize results and enable comparisons between research studies.40 To achieve standardization of results, PlGF values can be expressed in multiples of the expected median (MoM). This is an essential step in applying a competing risks model to prediction of PE in the first trimester utilizing Bayes’ theorem, which necessitates the combination of the a priori risk from the maternal history with measurements of the uterine artery Doppler pulsatility index (UtPI), mean arterial blood pressure (MAP) and the PlGF MoM result to calculate a patient-specific risk for PE.45,46 The prior risk estimated from maternal characteristics and history is then modified with the incorporation of these biomarkers to produce an adjusted estimate of the probability of delivery with PE. This survival time approach assumes that if pregnancy was to continue indefinitely, all women would develop PE, and the experience of this outcome before a specified gestation is dependent on competition between delivery before or after the development of PE.45,46 The incorporation of individual maternal characteristics and biomarker levels (MAP, UtPI and PlGF) modifies the mean distribution of gestational age at delivery with PE. In low-risk pregnancies, the gestational age distribution is shifted to the right which implies that delivery is likely to occur prior to a diagnosis of PE. In high-risk women, the gestational age distribution is shifted to the left indicating that delivery is likely to occur after the development of PE.45,46 This allows for individualized risk calculation, incorporating not only maternal risk factors but protective factors, such as a previous normal pregnancy.45 Another advantage of this approach is that partial combinations can be used to calculate patient-specific risks when not all biomarkers are available.
Studies have consistently shown that women who develop preterm PE have significantly lower PlGF levels in the first trimester than those with normal pregnancies (Table 1). Furthermore, a significant association is seen between serum PlGF concentrations and the severity of PE, defined by both the gestation at the time of iatrogenic delivery and the neonatal birthweight percentile.40 PlGF as an independent biomarker has detection rates (DR) of 55% and 33% for the identification of early- and late-onset PE, respectively (at a fixed false-positive rate (FPR) of 10%).40 However, there is now significant evidence that the DR of preterm PE can be improved using the aforementioned competing risks model, known as the Fetal Medicine Foundation (FMF) triple test between 11 and 13 weeks’ gestation.28
 |
Table 1 Studies Comparing First Trimester Serum PlGF Levels in Women Who Develop Pre-Eclampsia and Normotensive Controls |
The model was first developed from a study of 58,884 women which showed its accuracy in the detection of preterm PE (DR 77.3% at a fixed FPR of 10%).46 This algorithm encompassed maternal factors, MAP, UtPI and PlGF and additionally included serum pregnancy-associated plasma protein A (PAPP-A) levels, which are also known to be decreased in the first trimester in pregnancies later affected by PE.28 Including PAPP-A yielded a similar DR of 76.6%.46 Prospective data from first trimester screening of 35,948 women was used to update the original algorithm and assess its performance in the detection of preterm and term PE, which was 75% and 47%, respectively, with an FPR of 10%.28 The inclusion of PAPP-A to this combined model including PlGF did not improve the screening performance, a finding which has been replicated by Tan et al.47 A subsequent systematic review and meta-analysis has also demonstrated that PlGF is superior to PAPP-A in the first trimester prediction of PE.48 Whilst PAPP-A may be utilized in the FMF model if PlGF is unavailable, it results in reduced detection of preterm PE with DRs reported to be up to 7.1% (95% CI, 3.8–10.6%) lower with PAPP-A compared to using PlGF.49,50
The FMF prediction models have been prospectively evaluated in multiple studies worldwide which have reported comparable predictive performances. O’Gorman et al performed a prospective, multicenter study to validate the FMF algorithm in 8775 first trimester singleton pregnancies including 239 women (2.7%) with PE. This study reported DRs of 100%, 75% and 43% for very early (<32 weeks’), preterm and term PE with a 10% FPR, in keeping with the results of the preceding studies.51 The algorithm was also subsequently employed in the multicenter, double-blind, placebo-controlled Aspirin for Evidence-Based Preeclampsia Prevention (ASPRE) trial which reported DRs of preterm and term PE of 77% and 43% respectively with a 9.2% FPR.52
The largest study assessing the performance of the FMF triple test in the first trimester included 61,174 pregnant women and 1770 cases of PE (2.9%), and aimed to identify differences in the detection of PE between women of Caucasian and Afro-Caribbean racial origins.48 Previous evidence has demonstrated a significant association between maternal ethnicity and the risk of PE, which is highest amongst Afro-Caribbean and South Asian women, and lowest in the East Asian population.53 Women of Afro-Caribbean racial origin constituted 16.5% of the study population but contributed 48.3%, 37.1% and 30.2% of the cases of early, preterm and term PE, respectively, in keeping with the known increased risk of PE in this population. The DRs for early, preterm and term PE were also higher in this group (100%, 92% and 75%, respectively). Comparatively in Caucasian women, the DRs for early, preterm and term PE were 88%, 69% and 40% of cases, respectively.48
The performance of the FMF algorithm has also been evaluated in a prospective multicenter study in Asia, achieving DRs of 64.0% and 71.8% for preterm PE at 10% and 15% FPRs, respectively, which is comparable to previously published data in this population, but inferior to those achieved in Caucasian and Afro-Caribbean women.28,54,55 These findings have validated the FMF algorithm amongst populations that are vastly different from the original British and mixed-European cohorts. It must, however, be noted that the risk cut-off and screen positive rate to achieve a given fixed DR of preterm PE may vary according to the race of the study population and whether PlGF or PAPP-A is used in the FMF model.49
Subsequently, the International Federation of Gynecology and Obstetrics (FIGO)56 and the International Society of Ultrasound in Obstetrics and Gynecology (ISUOG)57 guidelines recommend the use of the multimarker FMF model to screen for PE in the first trimester. However, despite the volume of high-quality evidence for the FMF algorithm, the UK National Institute for Health and Clinical Excellence (NICE) and the American College of Obstetricians and Gynecologists (ACOG) currently endorse screening for PE by the identification of maternal risk factors from the woman’s demographic characteristics and medical history.58,59 Whilst ISSHP supports the use of the FMF algorithm for first trimester PE prediction when available, it otherwise also recommends the use of clinical risk factors to identify high-risk women.1 All pregnancies deemed to be at high risk of PE, defined by one high-risk factor or two moderate-risk factors, are recommended to be offered low-dose aspirin prophylaxis until delivery (Table 2).
 |
Table 2 Maternal Factors Categorized by Moderate or High Risk according to recommendations of the National Institute for Health and Clinical Excellence (NICE), the American College of Obstetricians and Gynecologists (ACOG) and the International Society for the Study of Hypertension in Pregnancy (ISSHP)1,58,59 |
These approaches treat each risk factor as a separate screening test with additive DR and screen positive rate.51 Whilst the listed risk factors have statistically significant associations with PE, their individual likelihood ratios (LR) are low and thus the utilization of this checklist method performs poorly.60 O’Gorman et al demonstrated that two-thirds of women classify as high-risk for PE when following the ACOG checklist with a 64.2% FPR.51 The DR of preterm PE was also shown to be low at only 39% when utilizing NICE guidance.51 The SPREE study also reported a similarly low DR of 40.8% preterm PE using the NICE checklist, in comparison to using the FMF method (DR 81.7% <37 weeks, 42.6% >37 weeks).54
These findings indicate that the FMF algorithm is superior to the method advocated by NICE and ACOG. Indeed, the use of risk factors, determined by their historic association with PE as opposed to a strong prospective evidence base, poorly discriminates between women who develop PE and those who do not. This has implications for patient compliance with aspirin administration, which is lower when recommended for a larger, less targeted population in comparison to a carefully selected group of women who receive specific counseling on their individual risk of PE.61 The SPREE study demonstrated this by reporting a 23% rate of compliance with aspirin prophylaxis when it was recommended by the NICE guidance.54 This is significant given the abundance of robust evidence that treatment of high-risk women with aspirin reduces the risk of preterm PE if the prescribed dose is greater than 100 mg and the treatment is commenced prior to 16 weeks.16,28,52,54 In the ASPRE study, participants identified as high risk by the FMF algorithm had 79.9% compliance to at least 85% of the prescribed 150 mg aspirin tablets.62 Rates of preterm PE were significantly lower in the aspirin group when compared to the placebo group (1.6% vs 4.3%, adjusted odds ratio (OR) 0.38; 95% CI 0.20–0.74, p=0.004), with no significant reduction in term PE.51 A secondary analysis of the ASPRE study specifically stressed the importance of compliance to aspirin prophylaxis in the successful prevention of PE, as results showed that the reduction in the incidence of preterm PE is reliant on good adherence to treatment; a 75% reduction was seen in those with compliance ≥90% compared to only a 40% reduction in those with compliance <90%.63 Comparatively, women with lower adherence to prophylaxis (<90%) appear to have a greater rate of PE (OR 2.3; 95% CI 1.2–11.6, p=0.03), fetal growth restriction (FGR) (OR 5.8; 95% CI 1.2–8.3, p=0.001) and preterm birth (OR 5.2; 95% CI 1.5–8.7, p=0.008).64 Guy et al have shown that use of the FMF algorithm also results in a statistically significant increase in targeted aspirin use by clinicians (99% vs 28.9%, OR 241.6; 95% CI 89.6–652) with a subsequent reduction in the rate of overall PE compared to those screened by the NICE guidelines (2.8% vs 3.6% p=0.016).60 Notably, the implementation of a first trimester screening program for the detection of preterm PE and targeted aspirin prescription in women identified as high risk has the potential for substantial cost savings to healthcare systems. A secondary analysis of the ASPRE study reported a statistically significant 68% reduction in the length of neonatal unit stay in the aspirin group compared to the placebo group (11.1 vs 31.4 days p=0.008).65 The cost savings from implementing screening were estimated to be in excess of $5.6 million due to shorter neonatal stays.65 A Canadian cost-effectiveness analysis further estimated that national integration of the FMF model into routine antenatal could save an estimated C$140 million over a 10-year period.66
Similarly to ASPRE, Guy et al’s study did not identify any significant reduction in the incidence of term PE, and it is notable from the above evidence that the first trimester FMF model is poor in predicting term PE compared to preterm PE. These findings support the possibility that there are varying pathophysiological mechanisms contributing to the PE syndrome. The influence of different contributors in both early onset and late onset PE has been debated and, consequently, it has been theorized that term PE is not an isolated placental-mediated condition, instead developing secondary to underlying maternal cardiovascular and metabolic disease, thus explaining why it is largely unaffected by aspirin prophylaxis.23,67,68 An alternative hypothesis centers on preterm PE and term PE being graduations of the same disease process, with aspirin administration delaying the clinical presentation of PE to a later gestational age.69 As term PE constitutes over 80% of PE cases, it has a large impact on healthcare systems given that maternal morbidity remains significantly increased in this group compared to women without PE.68,70 Thus, there remains a substantial need for effective predictive strategies to identify and treat women at risk of term PE.
Second and Third Trimester Prediction of PE
Screening for PE in the second and third trimesters aims to estimate the patient-specific risk, determining the frequency and content of an individual’s future antenatal surveillance. It is not primarily directed towards prevention of PE, given the diminished window of opportunity for current prophylactic intervention.16 Combining maternal risk factors, mean UtPI, MAP and PlGF has a similar, if not superior, predictive value to first trimester screening for early and preterm PE. Studies have demonstrated that this combined screening between 19 and 24 weeks’ gestation predicts 99% of early PE, 85% of preterm PE and 46% of term PE with a 10% FPR, outperforming the DRs achieved by maternal factors alone (52%, 47% and 37%, respectively).71
Screening in the third trimester between 30 and 34 weeks can also predict 98% of preterm PE but still fails to detect over half of term PE cases.72 The best DR of term PE by combined testing is achieved at 35 to 37 weeks’ (70%) and includes sFlt-1 levels in addition to MAP, PlGF and maternal factors, as the addition of UtPI does not improve detection at this gestation.73 To facilitate the clinical risk assessment of asymptomatic women in the first, second and third trimesters, the FMF has developed a free online PE risk calculator which is accessible on their website (https://fetalmedicine.org/research/assess/preeclampsia). Whilst first trimester screening by the FMF model has been established to be cost-effective in high resource settings, it is unclear presently if there are economic benefits with second and trimester screening for PE in asymptomatic women.
Screening for PE in Low- and Middle-Income Settings
Pregnant women in low- and middle-income countries (LMIC) are disproportionally affected by serious maternal morbidity and mortality, thus any meaningful strategies to reduce the global burden of PE must also be applicable to these settings.74 However, there are significant barriers to implementing screening for PE utilizing the FMF algorithm as these models rely on dependent access to ultrasound and laboratory testing, and additionally skilled clinicians who are competent in performing, and interpreting these results. This is a significant challenge given that most women in these low-income settings are not supervised by medical experts at any stage of their pregnancy.75 Therefore, there are strategies of equal importance that should be implemented, including workforce and provider education, accurate blood pressure measurement, the availability of essential drugs for prophylaxis and treatment of PE, and financing of healthcare provision in LMIC.56 FIGO recommends that in LMIC, when resources are limited, the FMF algorithm can be considered combining maternal characteristics and medical history with MAP.56 Whilst the DR for preterm PE will be reduced, the risk calculation can still be performed, allowing targeted aspirin prescription.56 Validation of this prediction model in LMIC is paramount and may be limited by populations with low health literacy.75
Serum PlGF and sFlt-1 in the Screening and Diagnosis of PE in Women with Suspected Disease
There are four commercially available PlGF-based assays recommended by NICE to rule-in or out PE between 20 and 36+6 weeks’ gestation.76 These tests may measure PlGF alone or additionally quantify sFlt-1 levels providing an sFlt-1/PlGF ratio. As the assays have different affinities for each PlGF isomer, the thresholds for diagnosing PE vary between each test. Similarly, the manufacturers indicate different gestational ranges for testing and thus each assay should be used per its product guidance. Conversion of second trimester raw data values to MoM may also be performed, eliminating significant variations amongst different commercial testing platforms and allowing direct comparison of inter-assay results.77 More recently, the ISSHP, NICE and German (AWMF) guidelines have included angiogenic testing as part of PE diagnosis.
Elecsys® Immunoassay sFlt-1/PlGF Ratio (Roche Diagnostics, Mannheim, Germany)
The Elecsys® sFlt-1/PlGF ratio is formed by combining the results from two electrochemiluminescence immunoassays. It is not available as a point-of-care test and analysis requires the use of a large-scale automated laboratory analyzer. The measurement ranges have been defined as 10–85,000 pg/mL and 3–10,000 pg/mL for sFlt-1 and PlGF, respectively.78 The sFlt-1/PlGF ratio is recommended for use in conjunction with clinical information in triaging (rule-out and rule-in) women suspected to have PE (Table 3).
 |
Table 3 Recommended sFlt-1/PlGF Ratio Cut-Offs Utilizing the Elecsys® Immunoassay, data from the NICE Guidance76 |
Rana et al first identified that using the Elecsys® sFlt-1/PlGF ratio was superior in the prediction of adverse maternal outcomes than traditional late clinical parameters of PE, including systolic blood pressure, proteinuria, deranged liver transaminases and elevated serum creatinine measurements with an area under the receiver-operating characteristics (ROC) curve (AUC) of 0.899.79 This study established a threshold of 85 for predicting adverse outcomes in women with early-onset PE (sensitivity 72.9%, specificity 94%) and identified that the sFlt-1/PlGF ratio was inversely correlated with time-to-delivery.79 Dröge et al have also shown that hypertension and proteinuria are not sufficiently predictive of PE-related adverse outcomes unless integrated into a multimarker regression model with the sFlt-1/PlGF ratio (AUC 0.69 vs 0.887) and that patients with a ratio >85 have a significantly shorter time-to-delivery than patients with values lower than 85 (median 4 vs 29 days, p<0.001).26
The PROGNOSIS prospective, multicenter, observational study reported that a ratio <38 accurately rules out the diagnosis of PE for 1 week (negative predictive value (NPV) 99.3%).80 An exploratory post-hoc analysis of data collected from the PROGNOSIS study has subsequently identified that an sFlt-1/PlGF ratio of ≤38 can rule-out the onset of PE for up to 4 weeks (NPV 94.3%), thus providing both clinicians and symptomatic women reassurance about the appropriateness of outpatient management.80,81 The INSPIRE prospective, randomized interventional trial investigated the impact of revealed sFlt-1/PlGF testing on inpatient hospitalization. Whilst the number of admissions did not differ between groups, a “revealed” ratio of >38 correctly identified all women that developed PE within 7 days demonstrating 100% sensitivity and 100% NPV, in comparison to a sensitivity of 83.3% and NPV of 97.8% in the concealed cohort.82 Stumpf et al have since demonstrated that routine clinical use of sFlt-1/PlGF testing can improve prognostic accuracy for women with PE which results in shorter hospital stays with potential economic benefits for healthcare systems (median 1 vs 4 days, p=0.009).83
However, the positive predictive value (PPV) for ruling in a diagnosis of PE within 4 weeks when utilizing an sFlt-1/PlGF ratio >38 is low (36.7%).80 Subsequently, higher thresholds for ruling in a diagnosis of suspected PE have been established dependent on gestation: ratios ≥85 between 20 and 33+6 weeks’ gestation and >110 between 34 weeks and birth.76
Multiple studies utilizing the Elecsys® immunoassays have shown that the sFlt-1/PlGF threshold of 85 reflects a state of severe angiogenic imbalance, detecting preterm PE with high sensitivity and specificity and significantly predicting adverse maternal and perinatal outcomes.24,79,84–86 The performance of an sFlt-1/PlGF ratio of ≥85 was analyzed as a secondary endpoint of the INSPIRE study which noted a significantly higher PPV of 71.7% to rule-in preterm PE within the following 4 weeks.87 Similarly, the ROPE study recorded a PPV of 74.4% for the presence of severe PE amongst symptomatic patients <34 weeks with a ratio >85 (NPV=91.0%).88
A higher cut-off of 110 at later gestations improves the specificity and the LR of the sFlt-1/PlGF ratio in the diagnosis of PE in these patients (specificity 95.5% and positive LR 13; 95% CI 7.3–23.0).85 Whilst many studies have utilized a ratio threshold of 38, NICE have employed a cut-off of 33 for diagnosing PE as Verlohren et al demonstrated that this result was highly sensitive and specific for PE in both early and late gestations and had the lowest negative likelihood ratio in women with PE (sensitivity and specificity of 95% and 94%, respectively, between 20 and 33+6 weeks, and 89.6% and 73.1%, respectively, after 34 weeks; negative LR 0.05, 95% CI 0.02–0.13).85
Triage® PlGF Test (Quidel Cardiovascular Inc., San Diego, CA)
The Triage® PlGF test is a single-use fluorescence immunoassay recommended by NICE to either rule-in or rule-out the diagnosis of PE in symptomatic women between 20 and 35 weeks’ gestation.76 The analyzer can be installed as a point-of-care test in a clinical area or in a laboratory, producing a test result in 15 minutes. The assay quantifies PlGF concentrations in the range of 12–3000 pg/mL with a result <100 pg/mL used as the threshold for a positive diagnosis.76,89 Angiogenic biomarkers appear to be less useful in discriminating the need for delivery in later PE given that most women in this cohort will have abnormal PlGF and sFlt-1 levels.90 The PEACOCK study assessed their diagnostic performance in determining the need for delivery within 7 days in women with late-onset preterm PE (34–36+6 weeks’). Whilst PlGF levels <100 pg/mL have high sensitivity for PE (97.9%), testing at this gestation poorly discriminates which individuals are at greatest risk (specificity 8.4%).90 The trial subsequently reported AUCs of less than 0.70 for PlGF, hence the NICE recommendation to screen until 35 weeks’ gestation.76,90
Levels <100 pg/mL have been shown to have high sensitivity and NPV for diagnosing PE necessitating delivery within 14 days (Table 4).26,91,92 The PELICAN study showed that the AUC for low PlGF <5th percentile was superior to all other standard tests for PE requiring delivery within 14 days including blood pressure, proteinuria, uric acid and alanine transaminase measurements (AUC 0.87).27 Chappell et al additionally demonstrated in this study that very low PlGF results <12 pg/mL have a much higher specificity for PE requiring delivery within 14 days compared to levels <100 pg/mL (90%, 95% CI 85%–94%).27
 |
Table 4 A Summary of the Results from Prospective Clinical Studies Utilizing the Quidel Triage® PlGF Assay and a Threshold of <100 Pg/Ml in PE Requiring Delivery within 14 Days |
PlGF levels of normal (>100 pg/mL), low (12–100 pg/mL) and very low (<12 pg/mL) concentrations were shown in the PETRA study to independently predict time-to-delivery with median values of 45,10 and 2 days, respectively.92
“Real-world” PlGF testing was implemented in a multicenter stepped-wedge cluster-randomized cluster trial (PARROT) to investigate the clinical effects of revealed PlGF testing on time-to-diagnosis and both maternal and perinatal outcomes.91 The median time to PE diagnosis was significantly reduced in the revealed testing cohort (4.1 vs 1.9 days, p=0.027) and there was also significantly less maternal adverse outcomes (as defined by the fullPIERS consensus) in this group (5% vs 4%, adjusted OR 0.32; 95% CI 0.11–0.96, p=0.043) with no evidence of increased adverse perinatal outcomes.91 This specifically highlights the potential benefits of real-time PlGF testing as a diagnostic adjunct when women present to hospital with suspected PE.
DELFIA Xpress® PLGF 1-2-3 (PerkinElmer Life and Analytical Sciences, Waltham, USA)
The DELFIA Xpress® PlGF 1-2-3 assay is a solid phase, two-site fluoroimmunometric sandwich assay, which quantifies serum levels of PlGF isoforms 1–3 between 1.9 and 4000 pg/mL. Prior to the 2022 update, the NICE guidelines on PlGF testing did not recommend the adoption of the DELFIA Xpress® PlGF 1-2-3 test into clinical practice for diagnosing or predicting time-to-delivery in PE, given that research remained limited and primarily focused on its use in first trimester prediction.76 DELFIA® PlGF cut-offs have subsequently been validated to rule-in and rule-out the diagnosis and aid short-term prediction of PE93–95 and are now advocated by NICE for this purpose from 20 weeks’ gestation.76
Whilst the different assays perform similarly,77 the rule-out threshold of 150 pg/mL was derived following the results of the COMPARE study which aimed to compare the performances of the commercially available PlGF-based tests in the prediction of time-to-delivery in women with PE prior to 35 weeks.94 DELFIA Xpress® PlGF 1-2-3 concentrations <150 pg/mL were noted to identify the same proportion of positive test results as the Triage® test and thus this cut-off was used for comparisons between assays. All three assays provided similar test performances in the prediction of time-to-delivery in women with PE prior to 35 weeks’ gestation (DELFIA® AUC 0.846, Quidel Triage® AUC 0.847, Elecsys® AUC 0.863) with no significant differences observed in AUCs (p=0.795), sensitivities (p=0.249), positive predictive values (p=0.765) or negative predictive values (p=0.92).94
Giblin et al also conducted a further secondary analysis of the COMPARE study demonstrating the optimal rule-in threshold of 50 pg/mL for the DELFIA Xpress® PlGF 1-2-3 assay.93 The specificities for the established Triage® PlGF and Elecsys® sFlt-1/PlGF rule-in thresholds (<12 and >85, respectively) were utilized to calculate the corresponding rule-in threshold for PE requiring delivery within 14 days using the DELFIA® test with an equivalent specificity (Table 5). The cut-off of 50 pg/mL for the DELFIA Xpress® test demonstrated a positive LR of over 10 suggesting good predictive ability for the population and endpoint studied, with a specificity of 95% indicating its suitability as a rule-in threshold.93 Despite variation in the quantitative thresholds for all of the commercially available assays, their individual clinical performances in the prediction of delivery in women with suspected PE have thus been demonstrated to be equivalent.76,93 Bremner et al have provided new prospective evidence of the diagnostic accuracy of the DELFIA Xpress® PlGF 1-2-3 test to rule-in and rule-out PE at the previously established thresholds (Table 6).95 Their findings show that between 20 and 33+6 weeks’ gestation, a PlGF level of >150 pg/mL is highly predictive in ruling out PE for up to four weeks, which is a significant advantage of the DELFIA® test as other studies have not investigated the use of PlGF alone to predict PE at 28 days.95
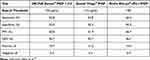 |
Table 5 The Performance of PlGF-Based Testing Assays in Predicting PE Requiring Delivery within 14 Days in 305 Women Presenting Prior to 35 Weeks’ Gestation93 |
 |
Table 6 Absolute Sensitivity and Specificity Values for PerkinElmer DELFIA Xpress PlGF 1-2-3 Levels and sFlt-1/PlGF Ratios, Showing High Specificity for Rule-in Thresholds of <50 Pg/Ml and sFlt-1/PlGF ≥70, and High Sensitivity for Rule-Out Thresholds of ≥150 Pg/Ml and sFlt-1/PlGF ≥90. Areas Under the Receiver-Operating Characteristics Curves Are Also Shown to Compare the Test Performances95 |
DELFIA Xpress® sFlt/PlGF 1-2-3 Ratio (PerkinElmer Life and Analytical Sciences, Waltham, USA)
The DELFIA Xpress PlGF 1-2-3® test can be used in combination with the PerkinElmer DELFIA Xpress sFlt-1® kit to determine the sFlt-1/PlGF ratio for both the diagnosis and short-term prediction of suspected PE. Bremner et al determined that an sFlt-1/PlGF ratio of <50 most accurately rules out a PE diagnosis within seven and 28 days, whilst the best performing cut-offs for ruling in a diagnosis are ≥70 between 20 and 33+6 weeks’ and ≥90 over 34 weeks’ gestation (Table 6).95
Notably, the performance of biomarker testing does not appear to be improved by the additional measurement of sFlt-1 levels with the DELFIA Xpress sFlt-1® kit.95 Thus, using the DELFIA Xpress PlGF 1-2-3® assay alone to determine PlGF levels may provide a competitive and cheaper alternative to other market competitors with similar clinical accuracy. However, NICE have concluded that compared with standard assessment, the DELFIA Xpress® sFlt-1/PLGF 1-2-3 ratio is a cost-effective measure and have subsequently recommended its use in clinical practice based upon locally available resources.76
Use of PlGF-Based Testing to Predict Adverse Maternal and Perinatal Outcomes
“Real-world” data from the PARROT trial demonstrated significant reductions in serious adverse maternal outcomes with revealed PlGF testing, with clear clinical benefits in utilizing angiogenic biomarkers as diagnostic adjuncts to target increased antenatal surveillance to high-risk women.91 Recent evidence has confirmed that compared to women who experience PE without severe features, individuals who experience the potentially life-threatening complications of hemolysis, elevated liver enzymes and low platelets (HELLP) syndrome, disseminated intravascular coagulation, severe renal involvement or eclampsia, have the most significant alterations in serum sFlt-1 and PlGF levels. Women with HELLP syndrome appear to acquire the greatest derangement in angiogenic factor levels with a 74% reduction in PlGF levels and a ten-fold increase in the sFlt-1/PlGF ratio, followed by those who experience eclampsia with 57% lower PlGF levels and a four-fold increase in the sFlt-1/PlGF ratio.96 The number of maternal complications also appears to correlate to the extent of angiogenic markers derangement, as when compared to women without severe features, those with PE and ≥2 adverse outcomes including severe hypertension, left ventricular failure, stroke and coma in addition to those detailed above, have significantly elevated sFlt-1/PlGF levels (5.70-fold change; 95% CI: 3.37–9.63, p<0.001).96
Altered levels of sFlt-1 and PlGF have also been associated with fetal complications including SGA, preterm birth and intrauterine death.79,92,97–99 Low maternal PlGF concentrations appear to have an excellent predictive performance for the detection of SGA fetuses with a sensitivity of 93.2% and NPV of 89.7% in women presenting with suspected PE, outperforming ultrasound assessment alone (sensitivity 71.2%, NPV 78.5%) and suggesting a role for PlGF in the detection of presumed growth restriction.99 PlGF has further been suggested as a potential discriminator between placentally mediated FGR and constitutionally small fetuses as a significant independent relationship has been demonstrated between PlGF levels <5th percentile and histological placental features of malperfusion.95 In a multicenter study, low PlGF levels outperformed gestational age, abdominal circumference measurement and umbilical artery resistance index in predicting FGR with an AUC of 0.96, NPV of 99.2%, 98.2% sensitivity, and 75.1% specificity.98 PlGF levels <5th percentile also demonstrated a significantly higher proportion of intrauterine deaths compared with normal levels (p<0.05).98 A systematic review by Sherell et al investigating maternal PlGF levels as a predictor of adverse intrapartum and perinatal outcomes further demonstrated that lower concentrations of PlGF are consistently associated with fetal compromise necessitating Caesarean delivery, neonatal intensive care admission, and stillbirth.97
Elevated sFlt-1/PlGF ratios have also been reported in pregnancies complicated by early-onset FGR and appear to correlate well with ultrasound Doppler findings of absent or reversed end-diastolic flow in the umbilical arteries.100 Garcia-Manau et al identified statistically significant differences in Elecsys® sFlt-1/PlGF levels with increasing FGR severity, defined by the extent of resistance in the umbilical artery Doppler (p<0.05).100 Optimal sFlt-1/PlGF thresholds were calculated to identify the severity of early-onset FGR, with a value <97.46 (AUC 0.852, 95% CI 0.772–0.932) ruling out absent or reversed end-diastolic flow with a sensitivity and specificity of 78.3% and 97.1% respectively, and a ratio ≥523.78 (AUC 0.751; 95% CI 0.578–0.924) identifying reversed end-diastolic flow with a sensitivity of 70.6% and specificity of 87.2%.100 Significant correlations were also found between higher sFlt-1/PlGF values and adverse outcomes including preterm birth (p<0.001), time-to-delivery (p<0.001), lower birthweight (p=0.026), and neonatal intensive care unit stay (p=0.006).100 Associations between low serum levels of PlGF and elevated sFlt-1 levels have also been observed in small studies investigating late-onset FGR;101 however, there are no proposed sFlt-1/PlGF cut-offs. Currently, biomarker testing as an adjunct to ultrasound for detecting FGR is not recommended outside of clinical research, given the paucity of prospective, interventional trial data and larger multicenter studies are recommended to investigate their role in fetal growth surveillance.102
The association of elevated sFlt-1/PlGF values with adverse perinatal events has been echoed by other studies, including a retrospective, “real world” study of 1117 women <36+6 weeks’ gestation, which reported that integrating sFlt-1/PlGF with maternal information aids the prediction of unfavorable outcomes including preterm birth, respiratory distress syndrome and fetal death with an AUC of 0.887.26 Significantly, the sFlt-1/PlGF ratio in suspected or confirmed PE has been shown to perform well in predicting a composite of other adverse perinatal outcomes including intraventricular hemorrhage, hypoxic-ischemic encephalopathy, necrotizing enterocolitis, and retinopathy of prematurity (AUC 0.87, 95% CI 0.81–0.93).103
Recognition that low PlGF levels and elevated sFlt-1/PlGF ratio correlate with poor perinatal outcomes is significant as this is arguably more clinically relevant than prediction of time-to-delivery, which may be influenced by a different threshold to deliver with advancing gestational age.
Repeat PlGF Testing
NICE do not currently recommend repeat PlGF testing for women at risk of or suspected to have PE.76 However, they have explicitly recommended further research to investigate if serial testing offers additional clinical and economic benefits compared to performing a single PlGF measurement. Notably, 10.9% of the women with normal PlGF levels in the PARROT study (>100 pg/mL) subsequently received a PE diagnosis later in pregnancy.104 Indeed, a multicenter case-series of 289 women undergoing repeated PlGF measurements identified that nearly one-third of women with suspected PE and an initial normal PlGF level >100 pg/mL (Triage®) have an abnormal result on repeat testing, indicating the dynamic changes in PlGF levels at the onset of clinical disease.104 The diagnostic accuracy of repeat PlGF testing was high and performed similarly to the cohort’s first test showing high sensitivity and NPV in predicting PE requiring delivery within 14 days (AUC 0.78, 95% CI 0.72–0.84 vs 0.80, 95% CI 0.68–0.89, respectively).104 Zeisler et al’s post-hoc analysis of the PROGNOSIS study additionally demonstrated that women who develop PE and/or adverse perinatal outcomes have significantly higher median increases in interval sFlt-1/PlGF ratio results when repeated after 2 and 3 weeks, compared to those who do not (p<0.001).81 However, this study was limited by its retrospective design, a lack of validation for the optimal interval between tests and the absence of performance statistics for repeat tests which were indeterminable due to the small sample size. Thus, serial testing may have a role in the risk stratification of women with ongoing clinical suspicion of PE despite an initial normal PlGF result, but prospective studies are needed to determine the benefit of repeat PlGF testing.
The PARROT-2 study aims to address this research gap and is recruiting participants to a prospective multicenter randomized controlled trial to investigate whether knowledge of serial repeat PlGF results (using either Elecsys® sFlt-1/PlGF or Triage® quantitative PlGF) in symptomatic women decreases the incidence of severe perinatal and maternal adverse outcomes. The investigators additionally aim to perform a cost-effectiveness analysis of repeat testing, including additional attendances, mode of delivery and neonatal care in addition to the price of PlGF tests.105
Use of PlGF-Based Testing in Twin Pregnancies
Twin pregnancies are at increased risk of gestational hypertension (relative risk (RR) 2.04, 95% CI 1.6–2.59) and PE (RR 2.62; 95% CI 2.03–3.38) compared to singleton gestations.106 Previous research has primarily addressed the prognostic value of angiogenic biomarkers in predicting and diagnosing PE in singleton pregnancies, excluding multiple gestations. Women with normal twin pregnancies appear to have at least double the levels of sFlt-1 compared to singleton pregnancies.107,108 This is theorized to be a result of the enlarged placental mass in twin gestations, which subsequently increases the placental expression of sFlt-1 out of proportion of the circulating PlGF levels, thus potentiating the characteristic maternal endothelial dysfunction associated with PE.20,107
In keeping with singletons, women with twin pregnancies and PE have significantly lower PlGF levels and greater sFlt-1 levels when compared to gestational age-matched cohorts with uneventful twin pregnancies (p<0.001).108 Thus, median sFlt-1/PlGF ratios are also significantly higher in these patients (p<0.001).108 Dröge et al determined an optimal sFlt-1/PLGF threshold of 53 for ruling in PE in twin pregnancies in a European multicenter study utilizing the Elecsys® assay (sensitivity 94.4%, specificity 74.2%).108 Use of the NICE recommended singleton lower cut-off of 33, initially established by Verlohren et al,85 resulted in a sensitivity of 100% but lower specificity (67.7%) in the twin cohort in comparison with singleton pregnancies <34 weeks (95% sensitivity, 94% specificity) suggesting a need to establish reference ranges for PlGF testing for twin pregnancies.108 De La Calle et al subsequently published an analysis which reported comparable sFlt-1/PlGF ratios between singletons and twins until 29 weeks’ when levels rise substantially more in twin gestations.109 In this study, an exploratory analysis of the sFlt-1/PlGF ratio threshold of ≤38 had a NPV of 91.9% and 83.8% to rule-out PE within a week and 4 weeks respectively.109 Binder et al also demonstrated that a cut-off of 38 can rule-out PE requiring delivery due to maternal complications of PE within one and 2 weeks with NPVs of 98.8% and 96.4%, respectively.110 Indeed, sFlt-1/PlGF performed better than PlGF alone for predicting delivery due to maternal complications within 2 weeks (AUC 0.88 vs 0.80, p=0.001) and had a stronger linear relationship with the sampling-delivery interval compared with PlGF.110
However, PPVs using this threshold appear to be much lower; 20% at 1 week and 44% at 4 weeks, which may be explained by the rising sFlt-1/PlGF ratios seen in normal twin pregnancies after 29 weeks’ which often surpasses the cut-off of 38 even in the absence of PE.108 Higher PPVs are reported when using cut-offs of 80 and 67 to predict delivery within one and 2 weeks, respectively (54.5% and 61.0%).110 Thus, an sFlt-1/PlGF cut-off of 38 is not clinically useful to accurately rule-in or sufficiently screen for PE but appears promising to rule-out a diagnosis of PE in twin pregnancies and identify women eligible for expectant management. Further analysis and particularly prospective studies are required to understand the differences in angiogenic marker levels in multiple gestations and to validate sFlt-1/PlGF cut-offs before implementation into clinical practice.
Conclusion
A state of angiogenic imbalance is central to the pathogenesis of PE and this knowledge is increasingly informing the use of angiogenic biomarkers to improve the prediction, diagnosis and management of the disease. The use of PlGF testing, combined with maternal characteristics, medical history and other biomarkers, is superior to current national guidance in first trimester risk prediction performance, allowing individualized antenatal care from the first hospital visit. This ensures targeted aspirin use by clinicians and patient understanding of the purpose of pharmacological prophylaxis, with resultant positive effects on treatment adherence and prevention of preterm PE. The value of PlGF and sFlt-1/PlGF as rule-out tests in the diagnosis and short-term prediction of PE has been clearly established in singleton pregnancies, outperforming traditional clinical parameters in determining time-to-delivery and predicting adverse perinatal outcomes.
Whilst the use of biomarkers in delivery planning of women with PE has not yet been adequately investigated and is not recommended, there is evidence that knowledge of PlGF levels can reduce serious maternal morbidity. Further research is required to ascertain the benefits of elective early delivery on perinatal outcomes when utilizing PlGF-based testing as more than just an adjunct to other clinical information in decision-making. There is emerging evidence of the potential advantages of angiogenic biomarkers to diagnose and predict other complications including fetal growth restriction and stillbirth, and this is a research priority given the association of these complications with pre-eclampsia.
Disclosure
Associarte Professor Kirsten Rebecca Palmer reports grants from National Health and Medical Research Council, non-financial support from ThermoFisher, outside the submitted work. Professor Fabricio da Silva Costa reports non-financial support from ThermoFisher, during the conduct of the study. The authors report no other conflicts of interest.
References
1. Brown MA, Magee LA, Kenny LC, et al. The hypertensive disorders of pregnancy: ISSHP classification, diagnosis & management recommendations for international practice. Pregnancy Hypertens. 2018;13:291–310. doi:10.1016/j.preghy.2018.05.004
2. Rana S, Lemoine E, Granger JP, Karumanchi SA. Preeclampsia. Circ Res. 2019;124(7):1094–1112.
3. Breetveld NM, Ghossein-Doha C, van Neer J, et al. Decreased endothelial function and increased subclinical heart failure in women several years after pre-eclampsia. Ultrasound Obstet Gynecol. 2018;52(2):196–204.
4. Bellamy L, Casas JP, Hingorani AD, Williams DJ. Pre-eclampsia and risk of cardiovascular disease and cancer in later life: systematic review and meta-analysis. BMJ. 2007;335(7627):974.
5. Chaiworapongsa T, Chaemsaithong P, Yeo L, Romero R. Pre-eclampsia part 1: current understanding of its pathophysiology. Nat Rev Nephrol. 2014;10(8):466–480.
6. Lai J, Syngelaki A, Nicolaides KH, von Dadelszen P, Magee LA. Impact of new definitions of preeclampsia at term on identification of adverse maternal and perinatal outcomes. Am J Obstet Gynecol. 2021;224(5):518.e1–518.e11.
7. Reddy M, Fenn S, Rolnik DL, et al. The impact of the definition of preeclampsia on disease diagnosis and outcomes: a retrospective cohort study. Am J Obstet Gynecol. 2021;224(2):217e1.
8. Zhang J, Klebanoff MA, Roberts JM. Prediction of adverse outcomes by common definitions of hypertension in pregnancy. Obstet Gynecol. 2001;97(2):261–267.
9. Villar J, Repke J, Markush L, Calvert W, Rhoads G. The measuring of blood pressure during pregnancy. Am J Obstet Gynecol. 1989;161(4):1019–1024.
10. Menzies J, Magee LA, MacNab YC, et al. Current CHS and NHBPEP criteria for severe preeclampsia do not uniformly predict adverse maternal or perinatal outcomes. Hypertens Pregnancy. 2007;26(4):447–462. doi:10.1080/10641950701521742
11. Verlohren S, Brennecke SP, Galindo A, et al. Clinical interpretation and implementation of the sFlt-1/PlGF ratio in the prediction, diagnosis and management of preeclampsia. Pregnancy Hypertens. 2022;27:42–50.
12. Fox A, McHugh S, Browne J, et al. Estimating the cost of preeclampsia in the healthcare system. Hypertension. 2017;70(6):1243–1249.
13. Ananth CV, Vintzileos AM. Maternal-fetal conditions necessitating a medical intervention resulting in preterm birth. Am J Obstet Gynecol. 2006;195(6):1557–1563.
14. Saigal S, Doyle LW. An overview of mortality and sequelae of preterm birth from infancy to adulthood. Lancet. 2008;371(9608):261–269.
15. Moster D, Lie RT, Markestad T. Long-term medical and social consequences of preterm birth. N Engl J Med. 2008;359(3):262–273.
16. Roberge S, Bujold E, Nicolaides KH. Aspirin for the prevention of preterm and term preeclampsia: systematic review and metaanalysis. Am J Obstet Gynecol. 2018;218(3):287–293.e1.
17. Sonek JD, Kagan KO, Nicolaides KH. Inverted pyramid of care. Clin Lab Med. 2016;36(2):305–317.
18. Roberts JM, Hubel CA. The two stage model of preeclampsia: variations on the theme. Placenta. 2009;30:32–37.
19. Khong TY, De Wolf F, Robertson WB, Brosens I. Inadequate maternal vascular response to placentation in pregnancies complicated by pre-eclampsia and by small-for-gestational age infants. BJOG. 1986;93(10):1049–1059.
20. Pijnenborg R, Anthony J, Davey DA, et al. Placental bed spiral arteries in the hypertensive disorders of pregnancy. BJOG. 1991;98(7):648–655.
21. Maynard SE, Min JY, Merchan J, et al. Excess placental soluble fms-like tyrosine kinase 1 (sFlt1) may contribute to endothelial dysfunction, hypertension, and proteinuria in preeclampsia. J Clin Invest. 2003;111(5):649–658.
22. Redman CWG, Sargent IL. Pre-eclampsia, the placenta and the maternal systemic inflammatory response - A review. Placenta. 2003;24(Suppl 1):S21–S27.
23. Thilaganathan B. The placenta is the villain or victim in the pathogenesis of pre-eclampsia. Int J Obstet Gy. 2021;128:148.
24. Falco ML, Sivanathan J, Laoreti A, Thilaganathan B, Khalil A. Placental histopathology associated with pre-eclampsia: systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2017;50:295–301.
25. Garcia-Gonzalez C, Georgiopoulos G, Azim SA, et al. Maternal cardiac assessment at 35 to 37 weeks improves prediction of development of preeclampsia. Hypertension. 2020;76(2):514–522.
26. Dröge LA, Perschel FH, Stütz N, et al. Prediction of preeclampsia-related adverse Outcomes with the sFlt-1 (soluble fms-like tyrosine kinase 1)/PlGF (placental growth factor)-ratio in the clinical routine: a Real-World Study. Hypertension. 2021;77(2):461–471.
27. Chappell LC, Duckworth S, Seed PT, et al. Diagnostic accuracy of placental growth factor in women with suspected preeclampsia: a prospective multicenter study. Circulation. 2013;128(19):2121–2131.
28. O’Gorman N, Wright D, Syngelaki A, et al. Competing risks model in screening for preeclampsia by maternal factors and biomarkers at 11–13 weeks gestation. Am J Obstet Gynecol. 2016;214(1):103.e1–103.e12.
29. Ferrara N, Gerber HP, LeCouter J. The biology of VEGF and its receptors. Nat Med. 2003;9(6):669–676.
30. Khaliq A, Li XF, Shams M, et al. Localisation of placenta growth factor (PlGF) in human term placenta. Growth Factors. 1996;13(3–4):243–250.
31. Vuorela P, Hatva E, Lymboussaki A, et al. Expression of vascular endothelial growth factor and placenta growth factor in human placenta. Biol Reprod. 1997;56(2):489–494.
32. Maglione D, Guerriero V, Viglietto G, Delli-Bovi P, Persico MG. Isolation of a human placenta cDNA coding for a protein related to the vascular permeability factor. Proc Natl Acad Sci USA. 1991;88(20):9267–9271.
33. Iyer S, Leonidas DD, Swaminathan GJ, et al. The crystal structure of human placenta growth factor-1 (PlGF-1), an angiogenic protein (PlGF-1), at 2.0 A resolution. J Biol Chem. 2001;276(15):12153–12161.
34. Chau K, Hennessy A, Makris A. Placental growth factor and pre-eclampsia. J Hum Hypertens. 2017;31(12):782–786.
35. Llurba E, Crispi F, Verlohren S. Update on the pathophysiological implications and clinical role of angiogenic factors in pregnancy. Fetal Diagn Ther. 2015;37(2):81–92.
36. Poon LC, Nicolaides KH. First-trimester maternal factors and biomarker screening for preeclampsia. Prenat Diagn. 2014;34(7):618–627.
37. Vrachnis N, Kalampokas E, Sifakis S, et al. Placental growth factor (PlGF): a key to optimizing fetal growth. J Matern Fetal Neonatal Med. 2013;26(10):995–1002.
38. Saffer C, Olson G, Boggess KA, Beyerlein R, Eubank C, Sibai BM. Determination of placental growth factor (PlGF) levels in healthy pregnant women without signs or symptoms of preeclampsia. Pregnancy Hypertens. 2013;3(2):124–132.
39. Levine RJ, Maynard SE, Qian C, et al. Circulating angiogenic factors and the risk of preeclampsia. N Engl J Med. 2004;350(7):672–683.
40. Akolekar R, Zaragoza E, Poon LCY, Pepes S, Nicolaides KH. Maternal serum placental growth factor at 11 + 0 to 13 + 6 weeks of gestation in the prediction of pre-eclampsia. Ultrasound Obstet Gynecol. 2008;32(6):732–739.
41. Tidwell SC, Ho HN, Chiu WH, Torry RJ, Torry DS. Low maternal serum levels of placenta growth factor as an antecedent of clinical preeclampsia. Am J Obstet Gynecol. 2001;184(6):1267–1272.
42. Lai J, Garcia-Tizon Larroca S, Peeva G, Poon LC, Wright D, Nicolaides KH. Competing risks model in screening for preeclampsia by serum placental growth factor and soluble fms-like tyrosine kinase-1 at 30–33 weeks’ gestation. Fetal Diagn Ther. 2014;35(4):240–248.
43. Zaragoza E, Akolekar R, Poon LCY, Pepes S, Nicolaides KH. Maternal serum placental growth factor at 11–13 weeks in chromosomally abnormal pregnancies. Ultrasound Obstet Gynecol. 2009;33(4):382–386.
44. Tsiakkas A, Duvdevani N, Wright A, Wright D, Nicolaides KH. Serum placental growth factor in the three trimesters of pregnancy: effects of maternal characteristics and medical history. Ultrasound Obstet Gynecol. 2015;45(5):591–598.
45. Wright D, Syngelaki A, Akolekar R, Poon LC, Nicolaides KH. Competing risks model in screening for preeclampsia by maternal characteristics and medical history. Am J Obstet Gynecol. 2015;213(1):62.e1–62.e10.
46. Akolekar R, Syngelaki A, Poon L, Wright D, Nicolaides KH. Competing risks model in early screening for preeclampsia by biophysical and biochemical markers. Fetal Diagn Ther. 2013;33(1):8–15.
47. Tan MY, Syngelaki A, Poon LC, et al. Screening for pre-eclampsia by maternal factors and biomarkers at 11–13 weeks’ gestation. Ultrasound Obstet Gynecol. 2018;52(2):186–195.
48. Zhong Y, Zhu F, Ding Y. Serum screening in first trimester to predict pre-eclampsia, small for gestational age and preterm delivery: systematic review and meta-analysis. BMC Pregnancy Childbirth. 2015;15:191.
49. Zumeta AM, Wright A, Syngelaki A, Maritsa VA, Da Silva AB, Nicolaides KH. Screening for pre-eclampsia at 11–13 weeks’ gestation: use of pregnancy-associated plasma protein-A, placental growth factor or both. Ultrasound Obstet Gynecol. 2020;56(3):400–407.
50. Wah YMI, Sahota DS, Chaemsaithong P, et al. Impact of replacing or adding pregnancy‐associated plasma protein‐A at 11–13 weeks on screening for preterm pre‐eclampsia. Ultrasound Obstet Gynecol. 2022;60(2):200–206.
51. O’Gorman N, Wright D, Poon LC, et al. Multicenter screening for pre-eclampsia by maternal factors and biomarkers at 11–13 weeks’ gestation: comparison with NICE guidelines and ACOG recommendations. Ultrasound Obstet Gynecol. 2017;49(6):756–760.
52. Rolnik DL, Wright D, Poon LCY, et al. ASPRE trial: performance of screening for preterm pre-eclampsia. Ultrasound Obstet Gynecol. 2017;50(4):492–495.
53. Khalil A, Rezende J, Akolekar R, Syngelaki A, Nicolaides KH. Maternal racial origin and adverse pregnancy outcome: a cohort study. Ultrasound Obstet Gynecol. 2013;41(3):278–285.
54. Tan MY, Wright D, Syngelaki A, et al. Comparison of diagnostic accuracy of early screening for pre-eclampsia by NICE guidelines and a method combining maternal factors and biomarkers: results of SPREE. Ultrasound Obstet Gynecol. 2018;51(6):743–750.
55. Chaemsaithong P, Pooh RK, Zheng M, et al. Prospective evaluation of screening performance of first-trimester prediction models for preterm preeclampsia in an Asian population. Am J Obstet Gynecol. 2019;221(6):650.e1–650.e16.
56. Poon LC, Shennan A. Hyett, J.A et al. The International Federation of Gynecology and Obstetrics (FIGO) initiative on pre-eclampsia: a pragmatic guide for first-trimester screening and prevention. Int J Gynecol Obstet. 2019;145:1–33.
57. Sotiriadis A, Hernandez-Andrade E, da Silva Costa F, et al. ISUOG Practice Guidelines: role of ultrasound in screening for and follow-up of pre-eclampsia. Ultrasound Obstet Gynecol. 2019;53(1):7–22.
58. National Institute for Health and Care Excellence. Hypertension in pregnancy: diagnosis and management. NICE guideline No. 133; 2019: 1–57. Available from: https://www.nice.org.uk/guidance/ng133.
59. American College of Obstetricians and Gynecologists and the Society for Maternal-Fetal Medicine. Low-dose aspirin use for the prevention of preeclampsia and related morbidity and mortality [Practice Advisory]; 2021. Available from: https://www.acog.org/clinical/clinical-guidance/practice-advisory/articles/2021/12/low-dose-aspirin-use-for-The-prevention-of-preeclampsia-and-related-morbidity-and-mortality.
60. Guy G, Leslie K, Diaz Gomez D, et al. Implementation of routine first trimester combined screening for pre‐eclampsia: a clinical effectiveness study. BJOG. 2021;128(2):149–156.
61. Cuckle H. Strategies for prescribing aspirin to prevent preeclampsia: a cost-effectiveness analysis. Obstet Gynecol. 2020;135(1):217.
62. Rolnik DL, Wright D, Poon LC, et al. Aspirin versus placebo in pregnancies at high risk for preterm preeclampsia. N Engl J Med. 2017;377(7):613–622.
63. Wright D, Poon LC, Rolnik DL, et al. Aspirin for Evidence-Based Preeclampsia Prevention trial: influence of compliance on beneficial effect of aspirin in prevention of preterm preeclampsia. Am J Obstet Gynecol. 2017;217(6):685.e1–685.e5.
64. Shanmugalingam R, Wang X, Motum P, et al. Clinical influence of nonadherence with prophylactic aspirin in preventing preeclampsia in high-risk pregnancies. Hypertension. 2020;75(4):1125–1132.
65. Wright D, Rolnik DL, Syngelaki A, et al. Aspirin for Evidence-Based Preeclampsia Prevention trial: effect of aspirin on length of stay in the neonatal intensive care unit. Am J Obstet Gynecol. 2018;218(6):612.e1–612.e6.
66. Ortved D, Hawkins TL, Johnson JA, Hyett J, Metcalfe A. Cost-effectiveness of first-trimester screening with early preventative use of aspirin in women at high risk of early-onset pre-eclampsia. Ultrasound Obstet Gynecol. 2019;53(2):239–244.
67. Melchiorre K, Sharma R, Thilaganathan B. Cardiovascular implications in preeclampsia. Circulation. 2014;130(8):703–714.
68. Thilaganathan B. Pre-eclampsia is primarily a placental disorder. BJOG. 2017;124(11):1763.
69. Wright D, Nicolaides KH. Aspirin delays the development of preeclampsia. Am J Obstet Gynecol. 2019;220(6):580.e1–580.e6.
70. Lisonkova S, Sabr Y, Mayer C, Young C, Skoll A, Joseph KS. Maternal morbidity associated with early-onset and late-onset preeclampsia. Obstet Gynecol. 2014;124(4):771–781.
71. Gallo DM, Wright D, Casanova C, Campanero M, Nicolaides KH. Competing risks model in screening for preeclampsia by maternal factors and biomarkers at 19–24 weeks’ gestation. Am J Obstet Gynecol. 2016;214(5):619.e1–619.e17.
72. Tsiakkas A, Saiid Y, Wright A, Wright D, Nicolaides KH. Competing risks model in screening for preeclampsia by maternal factors and biomarkers at 30–34 weeks’ gestation. Am J Obstet Gynecol. 2016;215(1):87.e1–87.e17.
73. Panaitescu A, Ciobanu A, Syngelaki A, Wright A, Wright D, Nicolaides KH. Screening for pre-eclampsia at 35–37 weeks’ gestation. Ultrasound Obstet Gynecol. 2018;52(4):501–506.
74. Duley L. The global impact of pre-eclampsia and eclampsia. Semin Perinatol. 2009;33(3):130–137.
75. Von Dadelszen P, Vidler M, Tsigas E, Magee LA. Management of preeclampsia in low- and middle-income countries: lessons to fate, and questions arising from the PRE-EMPT and related initiatives. Maternal Fetal Med. 2021;3(2):136–150.
76. National Institute for Clinical Excellence. PLGF-based testing to help diagnose suspected preterm pre-eclampsia: diagnostics Guidance; 2022:1–27. Available from: http://www.nice.org.uk/guidance/dg49.
77. Black C, Al-Amin A, Rolnik DL, et al. Midpregnancy testing for soluble fms-like tyrosine kinase 1 (sFlt-1) and placental growth factor (PlGF): an inter-assay comparison of three automated immunoassay platforms. Placenta. 2019;86:11–14.
78. Roche Diagnostics GmbH. Elecsys® sFlt-1/PlGF Immunoassay. Available from: https://diagnostics.roche.com/in/en_gb/products/params/elecsys-sflt-1-plgf-preeclampsia.html.
79. Rana S, Powe CE, Salahuddin S, et al. Angiogenic factors and the risk of adverse outcomes in women with suspected preeclampsia. Circulation. 2012;125(7):911–919.
80. Zeisler H, Llurba E, Chantraine F, et al. Predictive value of the sFlt-1: plGFRatio in women with suspected preeclampsia. N Eng J of Med. 2016;374(1):13–22.
81. Zeisler H, Llurba E, Chantraine FJ, et al. Soluble fms-like tyrosine kinase-1 to placental growth factor ratio: ruling out pre-eclampsia for up to 4 weeks and value of retesting. Ultrasound Obstet Gynecol. 2019;53(3):367–375.
82. Cerdeira AS, O’Sullivan J, Ohuma EO, et al. Randomized interventional study on prediction of preeclampsia/eclampsia in women with suspected preeclampsia: INSPIRE. Hypertension. 2019;74(4):983–990.
83. Dathan-Stumpf A, Rieger A, Verlohren S, Wolf C, Stepan H. sFlt-1/PlGF ratio for prediction of preeclampsia in clinical routine: a pragmatic real-world analysis of healthcare resource utilisation. PLoS One. 2022;17(2):e0263443.
84. Verlohren S, Galindo A, Schlembach D, et al. An automated method for the determination of the sFlt-1/PIGF ratio in the assessment of preeclampsia. Am J Obstet Gynecol. 2010;202(2):161.e1–161.e11.
85. Verlohren S, Herraiz I, Lapaire O, et al. New gestational phase–specific cutoff values for the use of the soluble fms-like tyrosine kinase-1/placental growth factor ratio as a diagnostic test for preeclampsia. Hypertension. 2014;63(2):346–352.
86. Leaños-Miranda A, Graciela Nolasco-Leaños A, Ismael Carrillo-Juárez R, et al. Usefulness of the sFlt-1/PlGF (Soluble fms-like tyrosine kinase-1/Placental Growth Factor) ratio in diagnosis or misdiagnosis in women with clinical diagnosis of preeclampsia. Hypertension. 2020;76(3):892–900.
87. Cerdeira AS, O’Sullivan J, Ohuma EO, et al. Performance of soluble fms-like tyrosine kinase-1–to–placental growth factor ratio of ≥85 for ruling in preeclampsia within 4 weeks. Am J Obstet Gynecol. 2021;224(3):322–323.
88. Rana S, Salahuddin S, Mueller A, Berg AH, Thadhani RI, Karumanchi SA. Angiogenic biomarkers in triage and risk for preeclampsia with severe features. Pregnancy Hypertens. 2018;13:100–106.
89. Quidel Cardiovascular Inc. Triage PLGF Test Product Insert: rapid quantitative test for placental growth factor (PlGF). Available from: https://www.quidel.com/sites/default/files/5BEBE4BC0C6100466B.pdf.
90. Duhig KE, Seed PT, Placzek A, et al. Prognostic indicators of severe disease in late preterm pre-eclampsia to guide decision making on timing of delivery: the PEACOCK study. Pregnancy Hypertens. 2021;24:90–95.
91. Duhig KE, Myers J, Seed PT, et al. Placental growth factor testing to assess women with suspected pre-eclampsia: a multicentre, pragmatic, stepped-wedge cluster-randomized controlled trial. Lancet. 2019;393(10183):1807–1818.
92. Barton JR, Woelkers DA, Newman RB, et al. Placental growth factor predicts time to delivery in women with signs or symptoms of early preterm preeclampsia: a prospective multicenter study. Am J Obstet Gynecol. 2020;222(3):259.e1–259.e11.
93. Giblin L, McCarthy FP, Gill C, et al. Rule-in thresholds for DELFIA Xpress PlGF 1-2-3 test for suspected pre-eclampsia. Pregnancy Hypertens. 2020;21:35–37.
94. McCarthy FP, Gill C, Seed PT, Bramham K, Chappell LC, Shennan AH. Comparison of three commercially available placental growth factor‐based tests in women with suspected preterm pre‐eclampsia: the COMPARE study. Ultrasound Obstet Gynecol. 2019;53(1):62–67.
95. Bremner L, Gill C, Seed PT, et al. Rule-in and rule-out of pre-eclampsia using DELFIA Xpress PlGF 1-2-3 and sFlt-1: plGF ratio. Pregnancy Hypertens. 2022;27:96–102.
96. Hastie R, Bergman L, Walker SP, et al. Associations between soluble fms-like tyrosine kinase-1 and placental growth factor and disease severity among women with preterm eclampsia and preeclampsia. J Am Heart Assoc. 2022;11(16):e024395.
97. Sherrell H, Dunn L, Clifton V, Kumar S. Systematic review of maternal Placental Growth Factor levels in late pregnancy as a predictor of adverse intrapartum and perinatal outcomes. Eur J Obstet Gynecol Reprod Biol. 2018;225:26–34.
98. Benton SJ, McCowan LM, Heazell AEP, et al. Placental growth factor as a marker of fetal growth restriction caused by placental dysfunction. Placenta. 2016;42:1–8.
99. Griffin M, Seed PT, Duckworth S, et al. Predicting delivery of a small-for-gestational-age infant and adverse perinatal outcome in women with suspected pre-eclampsia. Ultrasound Obstet Gynecol. 2018;51(3):387–395.
100. Garcia‐Manau P, Mendoza M, Bonacina E, et al. Soluble fms‐like tyrosine kinase to placental growth factor ratio in different stages of early‐onset fetal growth restriction and small for gestational age. Acta Obstet Gynecol Scand. 2021;100(1):119–128. doi:10.1111/aogs.13978
101. Birdir C, Droste L, Fox L, et al. Predictive value of sFlt-1, PlGF, sFlt-1/PlGF ratio and PAPP-A for late-onset preeclampsia and IUGR between 32 and 37 weeks of pregnancy. Pregnancy Hypertens. 2018;12:124–128. doi:10.1016/j.preghy.2018.04.010
102. Lees CC, Stampalija T, Baschat AA, et al. ISUOG Practice Guidelines: diagnosis and management of small-for-gestational-age fetus and fetal growth restriction. Ultrasound Obstet Gynecol. 2020;56::298–312. doi:10.1002/uog.22134
103. Reddy M, Palmer K, Rolnik DL, Wallace EM, Mol BW. Da Silva Costa F. Role of placental, fetal and maternal cardiovascular markers in predicting adverse outcome in women with suspected or confirmed pre-eclampsia. Ultrasound Obstet Gynecol. 2022;59:596–605. doi:10.1002/uog.24851
104. Duhig KE, Webster LM, Sharp A, et al. Diagnostic accuracy of repeat placental growth factor measurements in women with suspected preeclampsia: a case series study. Acta Obstet Gynecol Scand. 2020;99(8):994–1002. doi:10.1111/aogs.13818
105. Hurrell A, Sparkes J, Duhig K, et al. Placental growth fActor Repeat sampling for Reduction of adverse perinatal Outcomes in women with suspecTed pre-eclampsia: study protocol for a randomized controlled trial (PARROT-2). Trials. 2022;23(1):722. doi:10.1186/s13063-022-06652-8
106. Sibai BM, Hauth J, Caritis S, et al. Hypertensive disorders in twin versus singleton gestations. Am J Obstet Gynecol. 2000;182(4):938–942. doi:10.1016/S0002-9378(00)70350-4
107. Maynard SE, Moore Simas TA, Solitro MJ, et al. Circulating angiogenic factors in singleton vs multiple-gestation pregnancies. Am J Obstet Gynecol. 2008;198(2):200.e1–200.e7.
108. Dröge L, Herraìz I, Zeisler H, et al. Maternal serum sFlt-1/PlGF ratio in twin pregnancies with and without pre-eclampsia in comparison with singleton pregnancies. Ultrasound Obstet Gynecol. 2015;45(3):286–293.
109. de La Calle M, Delgado JL, Verlohren S, et al. Gestational age-specific reference ranges for the sFlt-1/PlGF immunoassay ratio in twin pregnancies. Fetal Diagn Ther. 2021;48(4):288–296.
110. Binder J, Palmrich P, Pateisky P, et al. The prognostic value of angiogenic markers in twin pregnancies to predict delivery due to maternal complications of preeclampsia. Hypertension. 2020;76(1):176–183.
111. Ong C, Liao AW, Cacho AM, Spencer K, Nicolaides KH. First-trimester maternal serum levels of placenta growth factor as predictor of preeclampsia and fetal growth restriction. Obstet Gynecol. 2001;98(4):608–611.
112. Thadhani R, Mutter WP, Wolf M, et al. First trimester placental growth factor and soluble fms-like tyrosine kinase 1 and risk for preeclampsia. J Clin Endocrinol Metab. 2004;89(2):770–775.
113. Erez O, Romero R, Espinoza J, et al. The change in concentrations of angiogenic and anti-angiogenic factors in maternal plasma between the first and second trimesters in risk assessment for the subsequent development of preeclampsia and small-for-gestational age. J Matern Fetal Neonatal Med. 2008;21(5):279–287.
114. Wortelboer E, Koster M, Cuckle H, Stoutenbeek P, Schielen P, Visser G. First-trimester placental protein 13 and placental growth factor: markers for identification of women destined to develop early-onset pre-eclampsia. BJOG. 2010;117(11):1384–1389.
115. Poon LCY, Akolekar R, Lachmann R, Beta J, Nicolaides KH. Hypertensive disorders in pregnancy: screening by biophysical and biochemical markers at 11–13 weeks. Ultrasound Obstet Gynecol. 2010;35(6):662–670.
116. Akolekar R, Syngelaki A, Sarquis R, Zvanca M, Nicolaides KH. Prediction of early, intermediate and late pre-eclampsia from maternal factors, biophysical and biochemical markers at 11–13 weeks. Prenat Diagn. 2011;31(1):66–74.
117. Kuc S, Koster MP, Franx A, Schielen PC, Visser GH. Maternal characteristics, mean arterial pressure and serum markers in early prediction of preeclampsia. PLoS One. 2013;8(5):e63546.
118. Crovetto F, Figueras F, Triunfo S, et al. First trimester screening for early and late preeclampsia based on maternal characteristics, biophysical parameters, and angiogenic factors. Prenat Diagn. 2015;35(2):183–191.
119. Diguisto C, Piver E, Gouge A, et al. First trimester uterine artery Doppler, sFlt-1 and PlGF to predict preeclampsia in a high-risk population. J Matern Fetal Neonatal Med. 2017;30(13):1514–1519.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
