Back to Journals » Vascular Health and Risk Management » Volume 18
Peripheral Arterial Disease Prevalence in a Population-Based Sample of People with Diabetes on the Caribbean Island of Barbados
Authors Adams OP , Herbert JR , Unwin N , Howitt C
Received 8 March 2022
Accepted for publication 16 May 2022
Published 31 May 2022 Volume 2022:18 Pages 387—395
DOI https://doi.org/10.2147/VHRM.S364993
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Prof. Dr. Pietro Scicchitano
O Peter Adams,1 Joseph R Herbert,1 Nigel Unwin,2– 4 Christina Howitt2
1Faculty of Medical Sciences, University of the West Indies, Cave Hill Campus, St Michael, Barbados; 2George Alleyne Chronic Disease Research Centre, University of the West Indies, St. Michael, Barbados; 3MRC Epidemiology Unit, University of Cambridge, Cambridge, UK; 4European Centre for Environment and Human Health, University of Exeter, Truro, UK
Correspondence: O Peter Adams, Faculty of Medical Sciences, University of the West Indies, Cave Hill Campus, St. Michael, Barbados, Tel +1 246 417 4260, Fax +1 246 438 9170, Email [email protected]
Background: Peripheral arterial disease (PAD) is a risk factor for amputation and systemic atherosclerotic disease. Barbados has a high diabetes prevalence, and 89% of diabetes-related hospital admissions are for foot problems. Foot examination is infrequent in Barbados primary care. The prevalence and potential risk factors for PAD in people with diabetes in Barbados were studied.
Methods: Multistage probability sampling was used to select a representative population sample of people ≥ 25 years of age with known diabetes or fasting blood glucose ≥ 7 mmol/L or HbA1c ≥ 6.5%. We administered the Edinburgh claudication questionnaire and assessed the ankle brachial pressure index (ABI) and Doppler waveform in both dorsalis pedis and posterior tibial arteries. Participants were classified into categories based on ABI as follows: PAD ≤ 0.90 in any leg; borderline 0.91 to 0.99 in one leg and the other not ≤ 0.90 or > 0.4; normal 1.00 to 1.40 in both legs; and non-compressible > 1.40 in one leg and the other not ≤ 0.9. Waveforms crossing the zero-flow baseline were categorised as normal. Multivariable logistic regression assessed the associations of potential risk factors with PAD.
Results: Of 236 participants (74% response rate, 33% male, median age 58.6 years), 51% had previously diagnosed diabetes. Of nine people with symptoms of definite or atypical claudication, four had PAD and one had non-compressible arteries. ABI prevalence (95% CI) was PAD 18.6% (13.8, 24.6), borderline 21.9% (16.6, 28.4), normal 55.5% (49.4, 61.5) and non-compressible 3.9% (1.6, 9.3). Increasing age and female gender were independently associated with PAD. Over 80% of normal legs (ABI 1.00 to 1.40) had normal posterior tibial and dorsalis pedis waveforms, while only 23% legs with PAD (ABI ≤ 0.90) had normal waveforms in both arteries (Kappa = 0.43).
Conclusion: Asymptomatic PAD is common in people with diabetes and requires ABI screening to detect it. Female gender is associated with PAD.
Keywords: diabetes, peripheral arterial disease, peripheral artery disease, claudication, waveform, Doppler ultrasound
Introduction
Neuropathy prevalence in people with diabetes1 and the annual diabetes-related lower extremity amputation rate2 are high in Barbados. Diabetic foot disease accounts for 89% of diabetes-related admissions to the island’s main hospital.3 Peripheral arterial disease (PAD) is a major risk factor for lower extremity amputation in people with diabetes especially when associated with neuropathy, deformity and trauma.4 Diabetes increases the risk for PAD5–7 and with diabetes, PAD often affects distal limb vessels,6,8 making the condition more difficult to treat.8 Risk increases with age, duration of diabetes, dyslipidaemia, elevated C-reactive protein, cigarette smoking and the presence of peripheral neuropathy.6,9,10 Vessels above the knee are more likely to be affected when PAD is due to risk factors such as smoking and hypertension rather than diabetes.10 Even when asymptomatic, PAD is a marker for systemic vascular disease and is associated with increased rates of myocardial infarction, stroke and death.10
The classic symptom of PAD is intermittent claudication characterized by a cramping or aching pain in the calves, thighs or buttocks that starts when walking and is relieved by rest. Severe PAD can cause rest pain, non-healing ulcers and gangrene.10,11 The Edinburgh claudication questionnaire was developed for the detection of intermittent claudication in epidemiological surveys.11 However, PAD is asymptomatic or has atypical symptoms in many people with diabetes.10 Peripheral neuropathy may blunt pain perception and make the presence of symptoms indicative of claudication insensitive to the presence of PAD.10
Foot pulses, while being a sensitive method for detecting PAD, has a reduced sensitivity and poor specificity when peripheral neuropathy is detectable.12 The ankle brachial pressure index (ABI), the ratio of the ankle and brachial systolic blood pressures, may be more useful. An ABI 0.90 or less, determined using a hand-held Doppler, has been validated against angiographically confirmed disease and has been found to be 95% sensitive and almost 100% specific for the detection of PAD.10 However, calcified arteries that are poorly compressible may lead to elevated ABI values in the presence of PAD.12 This is more likely in those with diabetes or chronic kidney disease.13,14 Some consider an ABI of >1.30 to indicate calcified arteries,4,10 while others use an ABI of >1.40.13,14 When the ABI is elevated, Doppler ankle waveforms depicting blood flow velocities can detect PAD masked by calcified arteries.14 A normal waveform is triphasic, representing rapid forward flow peaking during systole, reversal of flow during early diastole and slow forward flow during late diastole.15 Atherosclerotic disease results in a loss of reverse blood flow and produces first a biphasic and then a monophasic waveform.14 However, biphasic waveforms have been inconsistently defined in the literature. They may be considered normal when defined as including flow reversal and abnormal when including only forward flow.16 Waveform interpretation has also been found to be inconsistent among sonography professionals.17
Several studies suggest a higher PAD risk in people of African origin based on ABI measurements, although many of the larger studies have not included this group.6,18 In the USA, using National Health and Nutrition Examination Survey data the overall PAD prevalence as determined by ABI in people 40 years of age and over was 4.3%, with non-Hispanic Black race (OR 2.83) and diabetes (OR 2.71) positively associated with the condition.19 In a random sample of a 50- to 74-year-old Caucasian population in the Netherlands, the prevalence was 7.0% without diabetes, 15.1% in newly diagnosed diabetes cases and 20.9% in known cases.20
PAD prevalence in people with diabetes in Barbados is unknown and many people with chronic disease do not have an adequate clinical assessment, including regular foot examination, in the primary care setting.21–24 The objectives of this study were to estimate the prevalence of PAD and to identify factors associated with PAD in a population-based sample of people with known and newly identified diabetes on the Caribbean Island of Barbados. ABI with handheld Doppler and waveform analysis were utilised. The prevalence of intermittent claudication was also determined using the Edinburgh claudication questionnaire.
Methods
The Setting
Barbados is a Caribbean Island with a predominantly African origin population. This study was conducted between September 2011 and May 2013 and was part of a foot study that also determined peripheral neuropathy prevalence.1 The foot study was nested within the Barbados Health of the Nation (HotN) study, which identified, through multistage probability sampling, a representative sample of the population ≥25 years of age.25
Inclusion Criteria
HotN participants reporting a physician diagnosis of diabetes or who had a fasting plasma glucose of ≥7 mmol/l or an HBA1c of ≥6.5% were eligible to take part in the foot study. Individuals unable to comply with the physical examination were excluded.1
Study Procedure
Recruitment was previously described.1 Signed informed consent was obtained. A pre-tested questionnaire was administered. Six physicians, including JRH, were trained and conducted the foot examination.
Questionnaire
The questionnaire collected demographic data and assessed and graded intermittent claudication by means of the Edinburgh claudication questionnaire.11 Pain in the calf that started after beginning to walk, occured when walking uphill or hurrying and usually disappears in 10 minutes or less after stopping was indicative of definite claudication. Atypical claudication is defined as pain in the thigh or buttock, in the absence of calf pain.
Ankle Brachial Pressure Index
An aneroid sphygmomanometer and a Huntleigh Dopplex® bidirectional Doppler with an 8 MHz probe connected to a computer with software to record waveforms were used. With the patient lying supine and resting quietly, a sphygmomanometer cuff with a bladder encircling at least 80% of the limb was placed above the point of pulse measurement and inflated above the systolic pressure. As the cuff pressure was slowly decreased, the Doppler was used to obtain the systolic pressure in the right and left brachial arteries and then the right and left dorsalis pedis and posterior tibial arteries. The systolic pressure was recorded to the nearest 2 mmHg. The right ankle brachial index was calculated by dividing the highest ankle systolic pressure (posterior tibial or dorsalis pedis) of the right leg by the highest brachial systolic pressure (right or left arm). The left ankle brachial index was similarly calculated. The leg with the lower ABI was used as the index.10,14,26
Doppler Velocity Waveform Analysis
A tracing of the waveform for both the posterior tibial and dorsalis pedis arteries was recorded on a computer for analysis. Waveforms were classified independently by OPA and JRH and then discrepancies in classification were resolved after discussion. Waveforms that crossed the zero-flow baseline were considered multiphasic and classified as normal. Waveforms not crossing the zero-flow baseline or that were not detectable were considered monophasic and abnormal.16 Uninterpretable waveforms were classified as missing data.
Anthropometric and Biological Measurements
These included height, weight, waist and hip circumference, blood pressure, fasting blood glucose, lipids and HbA1c. The methods used have been described elsewhere.1,25,27
Analysis
Data were analysed using the Stata software package (version 16, StataCorp, College Station, Texas). PAD symptoms were scored according to the Edinburgh claudication questionnaire.11 Participants with symptoms of intermittent claudication were classified as having definite or atypical claudication. For each leg ABI was categorised as (a) ≤0.90 = PAD, (b) 0.91 to 0.99 = borderline, (c) 1.00 to 1.40 = normal and (d) >1.40 = non-compressible based on the 2016 AHA/ACC guideline.13 Participants were classified as having PAD if one or both legs had PAD; normal if the ABI in both legs were normal; having non-compressible arteries if at least one leg was in the non-compressible range and the other was not in the decreased range; and borderline if at least one leg was in the borderline range and the other was not in the decreased or non-compressible range. For participants with one leg only, classification was based on that leg. Estimates of prevalence for PAD categories were weighted to account for the sampling design and non-response, and to match the age and sex distribution of the Barbadian population with known and unknown diabetes, according to the Health of the Nation Study.25 Proportions are presented as numbers and percentages. A Kappa coefficient was calculated to assess the agreement between ABI and arterial waveforms for categorising arterial status as decreased vs normal. Potential risk factors, such as age, sex, anthropometric and biological characteristics, were compared in those with and without PAD. Differences were assessed by the t-test for mean summaries and z test for proportions. Poisson regression models with robust variance were used to calculate prevalence ratios (PRs) before and after controlling for potential confounders. Variables were considered potential confounders if their univariate association with ABI was statistically significant at the 5% level. Estimates are presented with 95% confidence intervals (95% CI).
Results
There were 320 eligible persons identified by the HotN study. Of these 236 participated in this study giving a response rate of 73.8%. The characteristics of responders and non-responders were similar except that a greater proportion of non-responders (66.7%) compared to responders (50.8%) reported a physician diagnosis of diabetes prior to the HotN study (p = 0.012). The characteristics of participants were as follows: 33.1% men, median age 58.6 years (IQR 50.6 to 69.4, range 29.6–95.7), 90.7% of African descent, mean BMI 30.1 kg/m2, mean waist circumference 97.7 cm, 52.1% on medication for hypertension, mean total cholesterol 4.9 mmol l−1, mean HDL 1.3 mmol l−1, mean fasting blood glucose 7.2 mmol l−1 and mean HbA1c 54 mmol/mol (7.1%).1 The characteristics of participants with a reported previous physician diagnosis of diabetes and those newly detected by the HotN study have been reported elsewhere.1
Nine people were identified as having claudication by the Edinburgh claudication questionnaire. Six were classified as “definite” and 3 as “atypical” claudication. Of the 6 with definite claudication, 2 had grade 2 claudication (pain on walking at an ordinary pace on the level) and the rest had grade 1 claudication (requiring more exertion than walking at an ordinary pace on the level to cause pain). Of those with definite claudication 1 had PAD with an ABI ≤0.90 in the right leg only and 1 had non-compressible arteries with the ABI >1.40 in both legs, but all 6 had at least one abnormal waveform. All 3 people with atypical claudication had PAD.
ABI was not recorded for 1 participant in both legs, for 2 participants for the right leg only and 1 participant did not have a recording for the left leg because of a below knee amputation on that side. For the 235 participants with at least an ABI reading for one limb, 41 had PAD, 51 borderline, 134 normal and 9 non-compressible arteries. The weighted PAD prevalence (ABI 0.9 or less) was 18.6% (95% CI = 13.8 to 24.6) and non-compressible prevalence was 3.9% (95% CI 1.6 to 9.3). Only 55.5% (95% CI 49.4 to 61.5) had ABIs in the normal range in both legs (Table 1).
 |
Table 1 Prevalencea of Ankle Brachial Index (ABI) in Participants by 2016 American Heart Association/American College of Cardiology Categories13 N = 235 |
Just over 80% of legs with a normal ABI had normal posterior tibial and dorsalis pedis waveforms in that leg. Most legs (73%) with PAD had at least one abnormal dorsalis pedis and posterior tibial waveform (Table 2). Within the PAD and normal ABI categories, the difference in the proportion of normal vs abnormal waveforms was statistically significant (p values: <0.001). The Kappa coefficient for agreement between ABI and arterial waveform for categorising arterial status as PAD vs normal was 0.43 (95% CI 0.29 to 0.57).
 |
Table 2 Dorsalis Pedis (DP) and Posterior Tibial (PT) Waveform Analysis by Ankle Brachial Pressure Index (ABI) Category13 for Each Leg (N = 473 Legs). Kappa Coefficient for Agreement Between ABI and Arterial Waveform for Categorising Arterial Status as PAD vs Normal = 0.43 (95% CI 0.29 to 0.57) |
Those with PAD were more likely to be older and to be female than those with a normal ABI in both legs (Table 3). Regression models indicated that both factors were independently associated with PAD (Table 4). There was no difference in the prevalence of PAD by whether diabetes was previously diagnosed or newly detected: for previously diagnosed study participants, 18% had PAD, compared with 19% for those newly diagnosed (p value = 0.661).
 |
Table 3 Comparison of Characteristics of Participants with a Normal Range (1.00 to 1.40) vs Peripheral Arterial Disease (0 to 0.90) Ankle/Brachial Pressure Index (ABI)a |
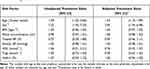 |
Table 4 Unadjusted and Adjusted Prevalence Ratios for Peripheral Arterial Disease According to Ankle Brachial Indexa |
Discussion
This is the first population-based study of PAD prevalence in people with diabetes conducted in a predominantly African Descent Caribbean population. There are few published studies estimating PAD prevalence in a population-based sample of people with diabetes in other populations. In our study, PAD prevalence was 18.6% (95% CI = 13.8 to 24.6) with a further 3.9% having an ABI indicating non-compressible arteries due to atherosclerotic disease. Increasing age and female gender were associated with the presence of PAD. Only four of the 41 people with PAD had symptoms of intermittent claudication. These findings are important in Barbados, where there is a high diabetes prevalence,25 inadequate foot examination in the primary care setting23 and a high amputation rate in people with diabetes, which is not only associated with PAD and neuropathy but also associated with open-toed footwear common in tropical countries.2 The findings will also be of relevance to other similar countries.
In the USA, the 1999 to 2000 National Health and Nutrition Examination Survey estimated PAD prevalence in those ≥40 years of age to be 4.3% (95% CI 3.1 to 5.5%). Black race/ethnicity compared to non-Hispanic whites (OR 2.83, 95% CI 1.48 to 5.42) and diabetes compared to no diabetes (OR 2.71, 95% CI 1.03 to 7.12) were among factors positively associated with PAD in that study.19 In a 50- to 74-year-old Caucasian population the prevalence of PAD was 15.1% in people with newly diagnosed diabetes and 20.9% in known cases.20 In Australia, the prevalence was 13.6% in known cases.28 A survey of patients attending 350 primary care practices in the USA chosen on the basis of a history of diabetes, cigarette smoking and age estimated the prevalence to be 29% in those >50 years but the actual percentage of people with diabetes included in that study is not clear.29 A systematic review estimated the odds ratio for PAD in people with diabetes globally to be 1.68 (95% CI 1.53 to 1.84) compared to those without diabetes.5
The finding that increasing age is independently associated with PAD is in keeping with other studies.5,6,19 The determination that female gender is independently associated with PAD in a black Caribbean population with diabetes is a significant finding of this study. The population prevalence of PAD is generally thought to be higher in men than women.18,30 A systematic review that did not include any studies from the Caribbean estimated a higher prevalence of PAD in women compared to men in lower and middle-income countries. In higher-income countries, the prevalence in men was slightly higher than in women.5 Barbados is classified by the World Bank as a high-income country.31 It should be noted that the amputation rate is high especially for women with diabetes in Barbados.2
A high proportion of our sample consisted of people with newly identified diabetes, and we found that there was an insignificant difference in PAD prevalence between people with known and newly diagnosed diabetes. The Hoorn study, conducted in an older Caucasian population, found that known diabetes was associated with PAD, while newly diagnosed diabetes was of borderline significance.6,20 Unlike other studies,5,6 we did not demonstrate an association between systolic BP and PAD or a protective association between HDL and PAD, but this might have been due to the sample size not being large enough.
Of the 6 people with symptoms of definite claudication, only one had PAD as determined by ABI and one had non-compressible arteries. However, the 3 people with atypical claudication all had PAD. This means that approximately 10% of people with PAD confirmed by ABI had symptoms of definite or atypical claudication. The prevalence of definite claudication, which is also referred to as classic claudication, is lower than other studies.5,29 In one study, 11% of patients with PAD had classic claudication.29 That population was, however, different to ours in that it included people who were 70 years and over or who were 50 to 69 years with a history of diabetes or cigarette smoking, and the sample was drawn from primary care clinics.
Over 70% of people with an ABI ≤0.9 had an abnormal Doppler velocity waveform supporting the diagnosis of PAD in one or more of the foot arteries. However, some people with an ABI in the normal range also had an abnormal waveform in the affected limb, raising the possibility that some of these may have calcified arteries masking PAD. The kappa coefficient of 0.43 suggests moderate agreement between ABI and waveform for categorising arterial status as PAD vs normal. In the San Diego Population study, 60 legs had an abnormal ABI (≤0.9) alone, 33 an abnormal waveform but ABI >0.9, and 69 had both abnormal waveform and ABI.18 In our study, 14 legs had an ABI ≤0.9 but normal waveforms, 105 had an abnormal waveform but an ABI >0.9, and 37 legs had both an ABI ≤0.9 and at least one abnormal waveform. Waveform analysis is reportedly more sensitive and specific than ABI in people with diabetes and peripheral neuropathy.12
Strengths and Limitations
The strengths of this study were that it used stringent methods to obtain a population-based sample of people with previously diagnosed and newly identified diabetes in Barbados, who were subsequently objectively tested for PAD using ankle/brachial pressure measurements supplemented by waveform analysis. Limitations also need to be considered. The representativeness of the sample was affected by a non-response bias resulting in an over-representation of women and older people.25 New cases of diabetes were diagnosed with a single fasting blood glucose or HbA1c test and a second confirmatory test, as recommended by the American Diabetes Association,32 was not used. This could result in an over diagnosis of diabetes. Although the response rate was 72% for this study, there was only a 55% response rate to the original Health of the Nation study25 that identified the population with diabetes. This has affected the representativeness of the sample.
Conclusions
The prevalence of peripheral arterial disease is high in this largely African descent Caribbean population with known and newly diagnosed diabetes. Most people with PAD do not have symptoms of claudication, and ABI estimation is therefore necessary to identify PAD. Women with diabetes are at increased risk of PAD compared to men and are therefore at increased systemic atherosclerotic disease risk. Almost one in five people with normal ABIs had waveforms suggestive of atherosclerotic disease. ABI measurement using handheld Doppler ultrasound requires training, practice and time. Automated machines are now available and are easier to use in a busy primary care clinical practice.
Data Sharing Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Ethical Approval
The study was approved by the Medical Ethics Committee of the University of the West Indies and the Ministry of Health and Wellness, Barbados, and informed consent was obtained from all participants. It complies with the Declaration of Helsinki ethical principles.
Acknowledgments
The Diabetes Foundation of Barbados provided the equipment used, and we specifically thank Simone Lorde from the Foundation for her assistance in sourcing the equipment from overseas.
Funding
Funding was through grants from the Peter Moores Barbados Trust and the Ministry of Health and Wellness, Barbados.
Disclosure
None of the authors have financial or personal conflicts of interest that can inappropriately influence the contents of this article.
References
1. Adams OP, Herbert JR, Howitt C, et al. The prevalence of peripheral neuropathy severe enough to cause a loss of protective sensation in a population-based sample of people with known and newly detected diabetes in Barbados: a cross-sectional study. Diabet Med. 2019;36(12):1629–1636. doi:10.1111/dme.13989
2. Hennis AJ, Fraser HS, Jonnalagadda R, et al. Explanations for the high risk of diabetes-related amputation in a Caribbean population of black African descent and potential for prevention. Diabetes Care. 2004;27(11):2636–2641. doi:10.2337/diacare.27.11.2636
3. Taylor CG
4. Boulton AJ, Armstrong DG, Albert SF, et al. Comprehensive foot examination and risk assessment: a report of the task force of the foot care interest group of the American Diabetes Association, with endorsement by the American Association of Clinical Endocrinologists. Diabetes Care. 2008;31(8):1679–1685. doi:10.2337/dc08-9021
5. Fowkes FG, Rudan D, Rudan I, et al. Comparison of global estimates of prevalence and risk factors for peripheral artery disease in 2000 and 2010: a systematic review and analysis. Lancet. 2013;382(9901):1329–1340. doi:10.1016/S0140-6736(13)61249-0
6. Criqui MH, Aboyans V. Epidemiology of peripheral artery disease. Circ Res. 2015;116(9):1509–1526. doi:10.1161/CIRCRESAHA.116.303849
7. Song P, Rudan D, Zhu Y, et al. Global, regional, and national prevalence and risk factors for peripheral artery disease in 2015: an updated systematic review and analysis. Lancet Glob Health. 2019;7(8):e1020–e1030. doi:10.1016/S2214-109X(19)30255-4
8. Luscher TF, Creager MA, Beckman JA, et al. Diabetes and vascular disease: pathophysiology, clinical consequences, and medical therapy: part II. Circulation. 2003;108(13):1655–1661. doi:10.1161/01.CIR.0000089189.70578.E2
9. Shammas NW. Epidemiology, classification, and modifiable risk factors of peripheral arterial disease. Vasc Health Risk Manag. 2007;3(2):229–234. doi:10.2147/vhrm.2007.3.2.229
10. American Diabetes Association. Peripheral arterial disease in people with diabetes. Diabetes Care. 2003;26(12):3333–3341. doi:10.2337/diacare.26.12.3333
11. Leng GC, Fowkes FG. The Edinburgh Claudication Questionnaire: an improved version of the WHO/Rose Questionnaire for use in epidemiological surveys. J Clin Epidemiol. 1992;45(10):1101–1109. doi:10.1016/0895-4356(92)90150-L
12. Williams DT, Harding KG, Price P. An evaluation of the efficacy of methods used in screening for lower-limb arterial disease in diabetes. Diabetes Care. 2005;28(9):2206–2210. doi:10.2337/diacare.28.9.2206
13. Gerhard-Herman MD, Gornik HL, Barrett C, et al. AHA/ACC guideline on the management of patients with lower extremity peripheral artery disease: a report of the American college of cardiology/American Heart Association task force on clinical practice guidelines. J Am Coll Cardiol. 2016;2017(69):e71–e126. doi:10.1016/j.jacc.2016.11.007
14. Norgren L, Hiatt WR, Dormandy JA, et al. Inter-society consensus for the management of peripheral arterial disease (TASC II). Eur J Vasc Endovasc Surg. 2007;33(Suppl 1):S1–75. doi:10.1016/j.ejvs.2006.09.024
15. Donnelly R, Hinwood D, London NJ. ABC of arterial and venous disease. Non-invasive methods of arterial and venous assessment. BMJ. 2000;320(7236):698–701. doi:10.1136/bmj.320.7236.698
16. Kim ES, Sharma AM, Scissons R, et al. Interpretation of peripheral arterial and venous Doppler waveforms: a consensus statement from the society for vascular medicine and society for vascular ultrasound. Vasc Med. 2020;25(5):484–506. doi:10.1177/1358863X20937665
17. Scissions R. Characterizing triphasic, biphasic, and monophasic Doppler waveforms. J Diagn Med Sonogr. 2008;24(5):269–276. doi:10.1177/8756479308323128
18. Criqui MH, Vargas V, Denenberg JO, et al. Ethnicity and peripheral arterial disease: the San Diego Population Study. Circulation. 2005;112(17):2703–2707. doi:10.1161/CIRCULATIONAHA.105.546507
19. Selvin E, Erlinger TP. Prevalence of and risk factors for peripheral arterial disease in the United States: results from the National Health and Nutrition Examination Survey, 1999–2000. Circulation. 2004;110(6):738–743. doi:10.1161/01.CIR.0000137913.26087.F0
20. Beks PJ, Mackaay AJ, de Neeling JN, et al. Peripheral arterial disease in relation to glycaemic level in an elderly caucasian population: the Hoorn study. Diabetologia. 1995;38(1):86–96. doi:10.1007/BF02369357
21. Adams OP, Carter AO. Diabetes and hypertension guidelines and the primary health care practitioner in Barbados: knowledge, attitudes, practices and barriers–a focus group study. BMC Fam Pract. 2010;11(1):96. doi:10.1186/1471-2296-11-96
22. Adams OP, Carter AO. Are primary care practitioners in Barbados following hypertension guidelines? - A chart audit. BMC Res Notes. 2010;3(1):316. doi:10.1186/1756-0500-3-316
23. Adams OP, Carter AO. Are primary care practitioners in Barbados following diabetes guidelines? - A chart audit with comparison between public and private care sectors. BMC Res Notes. 2011;4(1):199. doi:10.1186/1756-0500-4-199
24. Adams OP, Carter AO. Knowledge, attitudes, practices, and barriers reported by patients receiving diabetes and hypertension primary health care in Barbados: a focus group study. BMC Fam Pract. 2011;12(1):135. doi:10.1186/1471-2296-12-135
25. Howitt C, Hambleton IR, Rose AM, et al. Social distribution of diabetes, hypertension and related risk factors in Barbados: a cross-sectional study. BMJ Open. 2015;5(12):e008869. doi:10.1136/bmjopen-2015-008869
26. Khan NA, Rahim SA, Anand SS, et al. Does the clinical examination predict lower extremity peripheral arterial disease? JAMA. 2006;295(5):536–546. doi:10.1001/jama.295.5.536
27. Unwin N, Howitt C, Rose AM, et al. Prevalence and phenotype of diabetes and prediabetes using fasting glucose vs HbA1c in a Caribbean population. J Glob Health. 2017;7(2):020407. doi:10.7189/jogh.07.020407
28. Norman PE, Davis WA, Bruce DG, et al. Peripheral arterial disease and risk of cardiac death in type 2 diabetes: the Fremantle Diabetes Study. Diabetes Care. 2006;29(3):575–580. doi:10.2337/diacare.29.03.06.dc05-1567
29. Hirsch AT, Criqui MH, Treat-Jacobson D, et al. Peripheral arterial disease detection, awareness, and treatment in primary care. JAMA. 2001;286(11):1317–1324. doi:10.1001/jama.286.11.1317
30. Hirsch AT, Allison MA, Gomes AS, et al. A call to action: women and peripheral artery disease: a scientific statement from the American Heart Association. Circulation. 2012;125(11):1449–1472. doi:10.1161/CIR.0b013e31824c39ba
31. The World Bank. World bank country and lending groups; 2021. Available from: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519.
32. American Diabetes Association. 2. classification and diagnosis of diabetes: standards of medical care in diabetes—2018. Diabetes Care. 2018;41(Supplement_1):S13–S27. doi:10.2337/dc18-S002
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
