Back to Journals » International Journal of Women's Health » Volume 15
Perinatal Outcomes of Pregnancy in Women with Scarred Uteri
Authors Wang S, Hu Q, Liao H, Wang K, Yu H
Received 20 May 2023
Accepted for publication 9 September 2023
Published 19 September 2023 Volume 2023:15 Pages 1453—1465
DOI https://doi.org/10.2147/IJWH.S422187
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Everett Magann
Si Wang,1,2 Qing Hu,1,2 Hua Liao,1,2 Kana Wang,1,2 Haiyan Yu1,2
1Department of Obstetrics and Gynecology, West China Second University Hospital, Sichuan University, Chengdu, People’s Republic of China; 2Key Laboratory of Birth Defects and Related Diseases of Women and Children (Sichuan University), Ministry of Education, Chengdu, People’s Republic of China
Correspondence: Haiyan Yu, Department of Obstetrics and Gynecology, West China Second University Hospital; Key Laboratory of Birth Defects and Related Diseases of Women and Children, Sichuan University, No. 20, 3rd Section, South Renmin Road, Chengdu, Sichuan, 610041, People’s Republic of China, Email [email protected]
Objective: Uterine scarring is risky for the pregnancy and is closely associated with adverse pregnancy outcomes. Here, we investigated risk factors and associated perinatal outcomes in singleton pregnant women with uterine scars.
Methods: This retrospective cohort study was conducted on singleton pregnant women who delivered at the West China Second University Hospital between January 1, 2021, and December 31, 2021.
Results: The control group included 13,433 cases without uterine scars. The study group involved 2397 cases with one previous cesarean delivery (PCD), 163 cases with two PCDs, 12 cases with three PCDs, and 184 cases with non-cesarean uterine scars. The study group had a significantly higher incidence of placenta previa (6.4%), placenta percreta (5.3%), preterm delivery (10.3%), postpartum hemorrhage (3.4%), uterine rupture (9.4%), hysterectomy (0.18%), and bladder injury (0.4%) when compared with the control group (P < 0.05). The scarred uterus cases with 1, 2, or 3 PCDs had significantly different complications, with the higher PCD frequency correlating with increased rates of placenta previa, placenta percreta, postpartum hemorrhage, uterine rupture, and uterine resection. Moreover, the hospitalization time, cesarean operation time, and intrapartum bleeding in the current pregnancy significantly increased with increasing PCD frequency (P < 0.05). Analysis of the association between the duration of the interval between PCD and re-pregnancy and pregnancy complication revealed that the incidence of pernicious placenta previa was statistically higher in cases with intervals of < 2 years or ≥ 5 years (4.7%) than in cases with 2 years ≤ interval time < 5 years (2.5%) (P < 0.05).
Conclusion: Pregnancies with uterine scars may experience higher rates of adverse perinatal outcomes. This calls for increased observation during pregnancy and delivery to reduce maternal and fetal complications.
Keywords: scarred uterus, perinatal outcomes, singleton pregnancy, uterine rupture, pernicious placenta previa
Introduction
Uterine scars are often associated with a history of uterine surgery and are most common after cesarean delivery (CD). Other causes of uterine scars include myomectomy, cornual pregnancy resection, or uterine malformation correction. CD, a life-saving intervention, is central to resolving dystocia and serious pregnancy complications and therefore reduces maternal and child mortality and morbidity. The World Health Organization recommends that the ideal rate of CD should be between 10%–15%.1 The improved safety of CD, advances in anesthetic techniques, and the wide availability of hysteroscopy and laparoscopy, have significantly increased the number of CDs and other uterine surgeries in women of reproductive age.2 Studies show that cesarean rates are rising globally, and they now account for >20% of all births.3 In China, the rate of cesarean section (CS) increased from 28.8% to 34.9% between 2008 and 2014, and then to 36.7% in 2018, making it the highest among Asian countries.4 The steady increase in the rate of CDs is driven by various factors, including increased senile gravida, increased use of assisted reproductive technology (ART), and increased detection of fetal distress using electronic fetal heart monitors.5,6 The higher rates of CSs upon maternal request are attributable to limited knowledge of the advantages and disadvantages of CD by pregnant women and their families.7 As a result, an increasing proportion of women with a history of CS are having subsequent pregnancies. A retrospective cohort study found that having a CS at the first delivery markedly increases the risk of repeat CS (with 97.3% of CSs being done on women with previous CS vs 13.2% in women without a previous CS), as well as fetal–maternal complications in subsequent pregnancies, especially in women with non-indicated CSs.8
Uterine myomas are common benign gynecological tumors that affect 3–10% of women of reproductive age.9 Although uterine myomas are commonly treated using myomectomy, this operation may damage the uterus and affect subsequent pregnancies.10 Other procedures, such as cornual pregnancy resection and uterine malformation correction surgery, including uterine septum resection and residual horn hysterectomy, may increase the risk of uterine rupture and pelvic adhesion in subsequent pregnancies, thereby affecting maternal and child safety.11,12
Pregnancies with uterine scars are closely associated with adverse pregnancy outcomes. Clark and Silver found that long-term maternal morbidity is associated with repeat CD.13 This observation concurs with those of Getahun et al, who reported that previous CD is associated with an increased risk of placenta previa and placental abruption.14 Given the increase in new family planning policies in China, the increasing rate of pregnancies with uterine scars is becoming a significant health challenge.
In this study, we evaluated the risk factors and perinatal outcomes associated with uterine scarring in singleton pregnant women with the aim of identifying clinical management strategies that can improve maternal and neonatal outcomes.
Methods
This retrospective cohort study involves 16,189 cases of singleton pregnant women who delivered at the West China Second University Hospital, a tertiary hospital in western China, between January 1, 2021, and December 31, 2021. Ethical approval for the study was granted by the ethics committee of the West China Second University Hospital (approval no. 2023–043). The study authors reviewed the medical records of pregnant women (Figure 1).
 |
Figure 1 Graphical representation of the population. |
Inclusion and Exclusion Criteria
Only singleton pregnant women with a delivery gestational ≥28 weeks were included in the study. Pregnant multigravida women, as well as those with severe medical and surgical complications, stillbirth, history of classical CS, delivery at <28 weeks of gestation, and those with missing medical records information, were excluded.
The study group involved patients with uterine scars, including patients with a history of lower transverse uterine incision CD or a history of myometrial surgery, such as myomectomy, cornual pregnancy resection, and correction of uterine malformation. Patients without uterine scars were included as the control group.
Data Collection
The following clinical data on the included patients were collected: age, gestational age, body mass indexes (BMI) of >30 (obesity), hospitalization time and cost, and perinatal outcomes, including preterm deliveries (PTDs), malpresentation, premature rupture of membranes (PROM), placenta previa, placental abruption, pernicious placenta previa (PPP, where the placenta previa is attached to the lower uterine segment of the cesarean section scar, with or without placenta percreta),15 hypertensive disorder complicating pregnancy (HDCP), polyhydramnios, oligohydramnios, fetal growth restriction, assisted reproductive technology (ART), placenta accreta, postpartum hemorrhage (PPH), hysterectomy, abnormal fetal development, newborn birthweight and sex, and uterine rupture (including complete uterine rupture and uterine dehiscence). Complete uterine rupture is the rupture of the entire myometrium and the uterine cavity is connected to the abdominal cavity. Uterine dehiscence is the disruption of the uterine muscle with intact visceral peritoneum.16
Statistical Analyses
Quantitative normally distributed variables are expressed as mean ± SD. Statistical differences between two groups were compared using an independent t-test. Statistical differences between three groups were compared using one-way ANOVA. Non-normally distributed data (expressed as M [P25, P75]) were compared between two groups using the Mann–Whitney U-test, or between three groups using the Kruskal–Wallis test. Categorical variables were assessed using the chi-squared test, with continuity correction and Fisher’s exact test where appropriate. Fitting curve analysis and curve fitting were done using curvilinear regression analysis. Statistical analyses were done on SPSS version 24.0 (SPSS Inc., Chicago, IL, USA). P <0.05 indicated statistically significant differences.
Results
The study involved 16,189 pregnant women and of these, 2756 (17.0%), who had scarred uteri formed the study group, whereas the 13,433 (83.0%) with unscarred uteri formed the control group. The study group included 2397 cases with one PCD, 163 cases with two PCDs, 12 cases with three PCDs, and 184 cases with non-cesarean-associated uterine scars. In the cases with cesarean-associated uterine scars, the interval between the last menstrual period of the current pregnancy and the previous CD ranged from 5 months to 21 years. In cases with non-cesarean uterine scars, the interval time between the last menstrual period of the current pregnancy and the previous operation ranged from 2 months to 19 years. In the study group, based on ultrasound measurement (up to 3 days before pregnancy termination), the thickness of the lower uterine scar muscle layer ranged from 0.6 mm to 5.5 mm.
In the study group, uterine rupture occurred in 258 cases (9.4%). Of these, five cases had complete uterine rupture, whereas 253 cases had uterine dehiscence. Of the 258 uterine rupture cases, 43 (16.7%) had a suspected risk of uterine rupture due to preoperative pressure pain in the lower uterine segment, while 215 cases (83.3%) were identified during the CS. Uterine rupture occurred in 23 (18.1%, 23/127) cases with an interval of <2 years from the previous CD when compared with 235 cases (9.6%, 235/2445) with an interval of ≥2 years from the previous CD (χ2 = 9.662, P = 0.002). Based on ultrasound measurements, the thickness of the lower uterine scar muscle layer ranged from 0.9 mm to 4.0 mm in pregnant women with uterine rupture.
CS re-delivery in cases with uterine scarring predisposes to intraoperative organ injury, especially bladder injury. Of the 2756 cases in the study group, 11 (0.4%) had bladder injury during the operation and underwent bladder repair, including one case that had undergone laparotomy myomectomy, one case with two previous CDs, and nine cases with one previous CD.
Demographics and Perinatal Outcomes in Women with and without Uterine Scarring
Demographic data analysis revealed that age, delivery age, hospitalization time, hospitalization cost, and newborn birthweight differed significantly in the study vs control groups (P <0.05, Table 1).
 |
Table 1 Demographics and Perinatal Outcomes in Women with and without Scarred Uteri |
The incidence of placenta previa, placenta percreta, PTDs, PPH, uterine rupture, meconium-stained amniotic fluid (MSAF), hysterectomy, and bladder injury was significantly higher in the study group (scarred uterus) than in the control group (unscarred uterus) (P <0.05). In contrast, the incidence of PROM, placental abruption, oligohydramnios, FGR, and ART was significantly higher in the control group than in the study group (P <0.05). Malpresentation, HDCP, anemia, hypothyroidism, arrhythmia, and neonatal sex did not differ significantly between the two groups (P >0.05). Detailed information on perinatal outcomes is shown in Table 1.
Perinatal Outcomes in Women with Cesarean-Associated and Non-Cesarean-Associated Uterine Scarring
Uterine rupture (including complete and incomplete uterine rupture) occurred in 258 cases with cesarean-associated uterine scarring. The rate of uterine rupture in women with cesarean-scarred pregnancies was 10.1% (258/2572). No cases of uterine rupture were observed in those with non-cesarean-scarred uteri. The other perinatal conditions and pregnancy outcomes did not differ significantly between the cesarean-scarred and non-cesarean-scarred uteri groups (P >0.05). Our analysis found that five cases (0.19%, 5/2572) with cesarean-scarred uteri underwent hysterectomy due to PPP. Detailed information is presented in Table 2.
 |
Table 2 Perinatal Outcomes Between the Cesarean Scarred Uterus and Non-Cesarean Scarred Uterus |
Perinatal Outcomes of Women with Scarred Uteri and Varying Frequencies of Previous CDs
Among patients with a history of one CD, there were 24 cases of placental abruption (1.0%, 24/2397) and 31 cases of oligohydramnios (1.3%, 31/2397). There were no cases of placental abruption and oligohydramnios in patients with a history of two and three CDs.
Analysis of the incidence of placenta previa, placenta percreta, PTDs, PPH, uterine rupture, anemia, malpresentation, and hysterectomy revealed that they differed significantly with the number of CDs (P <0.05), with the incidence of adverse pregnancy outcomes, including placenta previa and placenta implantation, increasing significantly as the number of CDs increased. Moreover, the rate of hospitalization time, operation time, and intrapartum hemorrhage in the re-pregnant women differed significantly with the history of pregnancy termination by CD (P <0.05). However, PROM, HDCP, MSAF, intrahepatic cholestasis of pregnancy, hypothyroidism, arrhythmia, fetal abnormality, and ART did not differ significantly with the number of CDs (P >0.05). Detailed information is shown in Table 3.
 |
Table 3 Perinatal Outcomes in Scarred Uteri with Different Numbers of Cesarean Delivery |
Relationship Between Cesarean-Scarred Uteri and Pernicious Placenta Previa
Of the 2572 pregnant women with cesarean-scarred uteri, 104 (4.0%) had PPP, 76 (3.0%) had placenta accreta, 47 (1.8%) had postpartum hemorrhage (average blood loss: 1488.6 ± 1322.6 mL, including one case of hemorrhagic shock blood loss of 7590 mL), and five (0.2%) had undergone hysterectomy. In women with one, two, and three previous CDs, the incidence of PPP was 3.5% (83/2397), 11.7% (19/163), and 16.7% (2/12), respectively. PPP and non-pernicious placenta previa correlated significantly with the number of CDs, pregnancies, and deliveries (P <0.05). The results are shown in Table 4.
 |
Table 4 Characteristics of Pregnant Women with Cesarean-Scarred Uteri and Pernicious Placenta Previa |
The patients were divided into 11 groups based on the interval between the last menstrual period of the current pregnancy and the previous CS. The proportion of PPP varied with the re-pregnancy interval and was ranked by incidence rate (Table 5). Fitting curve analysis and curve fitting were done using curvilinear regression analysis. All four curve fitting models were statistically significant and the fitting effect was satisfactory (linear: R2 = 0.959, F = 212.909, P =0.000; logarithm: R2 = 0.959, F = 212.783, P =0.000; quadratic: R2 = 0.988, F = 332.840, P = 0.000; power function: R2 = 0.989, F = 216.208, P = 0.000; Figure 2).
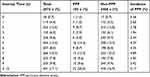 |
Table 5 The Relationship Between the Time of the Second Pregnancy and the Occurrence of Pernicious Placenta Previa |
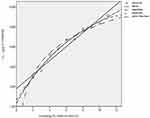 |
Figure 2 Fitted curve of the interval between re-pregnancy and incidence of pernicious placenta previa. |
The patients were divided into two groups based on the interval between the previous cesarean section and re-pregnancy: cases with 2 years ≤ interval time <5 years (725 cases) and cases with interval time <2 years or ≥5 years (1847 cases). The incidence of PPP in the two groups was as follows: 2.5% (18/725) and 4.7% (86/1847) and the PPP incidence differed significantly between the two groups (χ2 = 6.339, P <0.05).
Vaginal Delivery in Cases with Scarred Uteri
In the study group, there were 2683 cases (97.35%, 2683/2756) of CD, and 73 cases (2.65%, 73/2756) had successful vaginal birth (the number of women who underwent vaginal trial of labor with scarred uteri was 79), including 57 cases of vaginal delivery after one CS and 16 cases of vaginal delivery with non-cesarean scarred uteri. All cases with two and three previous CDs were terminated by CD.
Among the 73 cases of successful vaginal delivery, 64 (87.7%) had spontaneous labor and nine underwent cervical ripening and induced labor, including using a COOK balloon, artificial membrane rupture, and oxytocin induction.
Six women, who underwent vaginal trials of labor after CS, were transferred to emergency cesarean sections during labor. Of these women, three were transferred because they required CS, one because of fetal head descending stagnation, one because of suspected fetal distress, and one because bloody amniotic fluid was observed with incomplete uterine rupture during the operation.
In the scarred uteri group, hospitalization time and cost, intrapartum hemorrhage, and neonatal weight differed significantly in women who underwent vaginal delivery vs those who underwent CS (P <0.05). However, neonatal 5 min Apgar scores did not differ significantly (P >0.05, Table 6).
 |
Table 6 Comparison of the Perinatal Outcomes of Cesarean Delivery vs Vaginal Delivery in Pregnancies with Scarred Uteri |
Discussion
Previous studies have found that in subsequent pregnancies, women with uterine scarring are at increased risk of adverse perinatal outcomes, such as placenta previa, placenta percreta, uterine rupture, postpartum hemorrhage, preterm birth, neonatal infection, hypoxic–ischemic encephalopathy, and meconium aspiration syndrome.8,14,17,18 Additionally, the incidence of preterm birth, placenta previa, placenta percreta, postpartum hemorrhage, uterine rupture, and hysterectomy increased with the number of cesarean sections (CSs), which is consistent with previous reports.19,20 In the present study, we observed that uterine scarring is associated with an increased risk of adverse perinatal outcomes, including preterm delivery, placenta previa, placenta percreta, postpartum hemorrhage, and uterine rupture, which is consistent with previous findings. Moreover, our analyses revealed that the incidence of premature rupture of membranes (PROM) was higher in unscarred uteri (control group), which is consistent with the study by Hu et al.8 However, Getahun et al found an increased risk of placental abruption in scarred uteri,14 which is consistent with our observation that placental abruption was high in the unscarred uteri group. This is probably because planned elective CSs were chosen more often by patients in the scarred uteri group, while the control group contained a higher number of women who underwent spontaneous vaginal delivery, and who were likely to have premature rupture of membranes and placental abruption while waiting for natural labor and contraction. Therefore, the incidence of premature rupture of membranes and placental abruption was relatively high in the control group.
Although several past studies have shown that uterine scarring is strongly associated with adverse pregnancy outcomes, in recent decades the use of CS has increased worldwide.3 Our study revealed that the incidence of uterine scarring in the study group was 17.0% (2756/16,189) and that uterine scarring was mainly associated with CSs, which accounted for 93.3% (2572/2756) of the cases. The rate of repeat CS deliveries was 97.4% (2683/2756) in cases with scarred uteri, which is consistent with a previous retrospective cohort study.5 In China, a high proportion of first-time cesarean deliveries (CDs) are performed upon maternal request without medical indications. According to a 2010 study published in The Lancet, 25% of the CSs carried out in China are not for medical reasons.21 In 2018, the American College of Obstetricians and Gynecologists (ACOG) cited a large case study in Shanghai, China, which found that 24.7% of pregnant women had medically unindicated CD.22 Therefore, reducing the rate of unindicated CD and the overall rate of CD is key to reducing the incidence of scarred uterine pregnancies, as well as the associated adverse maternal and infant pregnancy outcomes.23
PPP is one of the most dangerous CS-associated pregnancy complications.15 Chen et al reported that in China, the incidence of PPP ranges from 0.31% to 0.89%.24 In this study, we found that the PPP proportion at our hospital was 4.0%, which was higher than is reported in the literature. This discrepancy may be because our hospital is a tertiary hospital in western China, and most of the patients with PPP were transferred there from other hospitals. Additionally, we found the PPP incidence to be higher in patients with a cesarean scar on their uterus at intervals of <2 years or ≥5 years than those at intervals of ≥2 years or <5 years. Probably because of the short interval between pregnancies, tender granulation tissue, fibrous tissue at the uterine incision, extensive tender connective tissue between smooth muscle cells, poor muscularization of the uterine scar during re-pregnancy, and the lack of elasticity at the scar. These factors can easily cause uterine rupture during late pregnancy or delivery.25,26 Additionally, the gestational sac may enter the muscular layer through tiny fissures on the scar, and there is a high risk of placental adhesion and accreta.27
In this study, the incidence of uterine rupture in re-pregnant women with an interval of <2 years after the previous CS was significantly higher than in women with an interval of ≥2 years (18.1% vs 9.6%). Previous studies have associated both short and long interpregnancy intervals with several adverse pregnancy outcomes in cases with scarred uteri. A single-center analysis of the relationship between gestational interval and adverse pregnancy outcomes in women who had re-pregnancy after CS associated long gestational intervals (>5 years) with increased risk of preterm delivery, PROM, and HDCP, whereas short gestational intervals (<1 year) was associated with higher risk of PTDs. Moreover, the risk of adverse pregnancy outcomes did not differ significantly between those with intervals of 13–24 months and 25–60 months.28 Furthermore, Gonzalez29 and Bujold30 found that the risk of uterine rupture, placenta previa, placenta accreta, and placental abruption was lowest in women with intervals of 18–24 months. Schummers also suggested that short interpregnancy intervals were associated with an increased risk of adverse pregnancy outcomes in women of all ages.31 Considering the fertility of older women, the Chinese expert consensus recommends that older women with CS-associated scarred uteri should get pregnant again within 12–24 months of surgery.32
Although we did not identify any cases of uterine rupture in cases with myomectomy-associated scarred uterine pregnancies, there is still a risk of uterine rupture in post-myomectomy pregnancies.33 Women with very short postoperative intervals between pregnancies are prone to uterine rupture, whereas women with very long intervals are prone to fibroid recurrence. Therefore, comprehensive case-by-case assessments are recommended. The recommended interval between re-pregnancies ranges from 6 months to 2 years.34,35 Additionally, pregnancies after cornual pregnancy resection and hysteroplasty have a higher uterine rupture risk and a higher risk of pregnancy. Regrettably, there is no evidence-based medical guidance for the optimal pregnancy interval after cornual pregnancy resection and hysteroplasty.
In recent years, vaginal delivery after re-pregnancy with uterine scarring has gained attention. In this study, 73 cases with scarred uteri had successful vaginal deliveries, accounting for 92.4% (73/79). Previous studies have found that repeat CS is unnecessary for women with only one previous transverse CS or subserosal or submucosal myomectomy without myometrial injury.36,37 Vaginal birth has many benefits, such as faster recovery, potentially fewer risks in future pregnancies, and lower risk of childhood diseases, like asthma, allergies, and obesity.38 Hence, after strict risk assessment, the vaginal trial of labor is both safe and feasible for women with scar re-pregnancy.39–41
Previous studies indicate that the incidence of uterine rupture during vaginal delivery in patients with previous CD with transverse incision of the lower segment of the uterus is only 0.1%–1.5%.42,43 In this study, only one pregnant woman underwent emergency CD due to suspected uterine rupture. However, the short- and long-term risks of CD, including anesthesia accidents, severe bleeding, infection, adhesion injury, and increased risk of future pregnancy complications, such as uterine scar pregnancy, uterine rupture, dangerous placenta previa, and uterine scar diverticulum, cannot be ignored. Moreover, there is no evidence that CS for women who do not meet the indications has any benefits to the mother or child.44,45 Nevertheless, the relationship between uterine rupture and lower uterine thickness remains controversial and there are no guidelines on how to predict the risk of uterine rupture based on the lower uterine segment thickness. Based on previous reports, the cut-off values of the full and muscular thicknesses of the lower uterine segment are 2.0–3.5 mm and 1.4–2.0 mm, respectively.46,47 A prospective observational study of women with one prior low-transverse CS and a singleton gestation, who underwent a trial of labor, found an increased risk of uterine rupture after labor induction only in women with no prior vaginal delivery (1.5% vs 0.8%, P = 0.02).48
Regarding the timing of pregnancy termination, current studies recommend elective CD for re-pregnancy in women with a history of one CD after 39 weeks, except for those with placenta previa, placenta accreta, and other conditions that require emergency CD. In contrast, the optimal delivery time for women with a history of two previous CDs remains controversial, with some studies suggesting that elective delivery at 38–39 weeks likely represents the optimal balance between neonatal and maternal risk, while decreasing the likelihood of unplanned CD for women with two CDs. Elective CD is feasible at 38 weeks in pregnant women with scarred uteri, such as myomectomy-associated scarring.49,50
To manage re-pregnancies with scarred uteri, it is necessary to formulate a continuous management system before, during, and after pregnancy to improve maternal and infant outcomes. Attention should be paid to the following aspects. (1) Women with scarred uteri should be evaluated before re-pregnancy, including to determine the risk associated with re-pregnancy and to evaluate the information about operation time, operation method, and perioperative conditions of the previous operation. In cases where the scar is poorly healed, the incision diverticulum or the defect is large, or the residual muscle layer thickness of the defect is thin, it is important to wait for the scar to heal or perform surgical repair before planning pregnancy. (2) It is also important to carefully screen for cesarean scar pregnancies during early pregnancy. Once diagnosed as a cesarean scar pregnancy, it is recommended that the pregnancy be terminated as soon as possible to minimize the risk of massive bleeding or uterine rupture.51–53 (3) The risk of placenta previa, placenta accreta, and uterine rupture increases significantly in women with scarred uteri re-pregnancies. The occurrence of uterine rupture, PPP, placenta accreta, and other complications should be recognized in early pregnancy, and the possibility of vaginal delivery in case of re-pregnancy with scarred uteri should be evaluated during pregnancy. (4) For patients with PPP and placenta accreta, an individualized multidisciplinary collaborative treatment plan should be formulated according to the standard diagnosis and treatment process, and the pregnancy should be terminated promptly. (5) Moreover, postpartum hemorrhage, thrombosis, pelvic and abdominal adhesion, as well as other related complications should be monitored closely.
To the best of our knowledge, this is one of a few studies that have comprehensively studied the association between scarred and unscarred uteri. Our study included a comparison of perinatal outcomes of scarred uteri with different causes and a comparison of the perinatal outcomes of second pregnancies after different CSs. In addition, we analyzed the risk factors underlying pernicious placenta previa after CS and the perinatal outcome of vaginal delivery in women with scarred uteri. However, because this is a single-center retrospective case study, our findings should be validated using larger sample sizes in prospective randomized controlled multicenter studies.
Conclusions
Our data indicate that pregnancy with uterine scarring is associated with increased adverse perinatal outcomes. This calls for increased monitoring during pregnancy and delivery to reduce the risk of maternal and fetal complications.
Abbreviations
PCD, previous cesarean delivery; CD, cesarean delivery; ART, assisted reproductive technology; CS, cesarean section; PTDs, preterm deliveries; PROM, premature rupture of membranes; HDCP, hypertensive disorder complicating pregnancy; FGR, fetal growth restriction; PPH, postpartum hemorrhage; LMP, last menstrual period; MSAF, meconium-stained amniotic fluid; PPP, pernicious placenta previa; ICP, intrahepatic cholestasis of pregnancy; ACOG, American College of Obstetricians and Gynecologists; DM, diabetes mellitus; GDM, gestational diabetes mellitus; PGDM, pregestational diabetes mellitus.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Ethical Approval and Informed Consent
The study was approved by the ethics committee of West China Second University Hospital (No. 2023-043). Informed consent was obtained from all participants. Our study complies with the Declaration of Helsinki.
Acknowledgments
We are grateful to the doctors and staff who have been involved in this work.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by the Natural Science Foundation of Sichuan (2022NSFSC0659) and the Science Foundation of Chengdu (No. 2021-YF05-01532-SN).
Disclosure
The authors report no conflicts of interest associated with this work.
References
1. Betran AP, Torloni MR, Zhang JJ, Gülmezoglu AM; WHO Working Group on Caesarean Section. WHO statement on Caesarean section rates. BJOG. 2016;123(5):667–670. doi:10.1111/1471-0528.13526
2. Betrán AP, Ye J, Moller AB, Zhang J, Gülmezoglu AM, Torloni MR. The increasing trend in caesarean section rates: global, regional and national estimates: 1990–2014. PLoS One. 2016;5(2):e0148343. doi:10.1371/journal.pone.0148343
3. Boerma T, Ronsmans C, Melesse DY, et al. Global epidemiology of use of and disparities in caesarean sections. Lancet. 2018;392(10155):1341–1348. doi:10.1371/journal.pone.0148343
4. Qiao J, Wang Y, Li X, et al. A Lancet Commission on 70 years of women’s reproductive, maternal, newborn, child, and adolescent health in China. Lancet. 2021;397(10293):2497–2536. doi:10.1016/S0140-6736(20)32708-2
5. Betran AP, Ye J, Moller AB, Souza JP, Zhang J. Trends and projections of caesarean section rates: global and regional estimates. BMJ Glob Health. 2021;6(6):e005671. doi:10.1136/bmjgh-2021-005671
6. Li HT, Hellerstein S, Zhou YB, Liu JM, Blustein J. Trends in Cesarean delivery rates in China, 2008–2018. JAMA. 2020;323(1):89–91. doi:10.1001/jama.2019.17595
7. Jenabi E, Khazaei S, Bashirian S, Aghababaei S, Matinnia N. Reasons for elective cesarean section on maternal request: a systematic review. J Matern Fetal Neonatal Med. 2020;33(22):3867–3872. doi:10.1080/14767058.2019.1587407
8. Hu HT, Xu JJ, Lin J, et al. Association between first caesarean delivery and adverse outcomes in subsequent pregnancy: a retrospective cohort study. BMC Pregnancy Childbirth. 2018;18(1):273. doi:10.1186/s12884-018-1895-x
9. Borgfeldt C, Andolf E. Transvaginal ultrasonographic findings in the uterus and the endometrium: low prevalence of leiomyoma in a random sample of women age 25–40 years. Acta Obstet Gynecol Scand. 2000;79(3):202–207.
10. Lu B, Wang Q, Yan L, Yu K, Cai Y. Analysis of pregnancy outcomes after laparoscopic myomectomy: a retrospective cohort study. Comput Math Methods Med. 2022;2022:9685585. doi:10.1155/2022/9685585
11. Jansa V, Laganà AS, Ferrari F, et al. Uterine rupture in pregnancy after hysteroscopic septum resection: a 20-year retrospective analysis. Minim Invasive Ther Allied Technol. 2022;31(3):448–455. doi:10.1080/13645706.2020.1837884
12. Hurrell A, Jayalath GKC, Gorry A, Gupta M, Odejinmi F. Placenta percreta after laparoscopic excision of intersitial ectopic pregnancy: a case for elective caesarean section after cornual resection? Eur J Obstet Gynecol Reprod Biol. 2015;194:257–258. doi:10.1016/j.ejogrb.2015.08.017
13. Clark EA, Silver RM. Long-term maternal morbidity associated with repeat cesarean delivery. Am J Obstet Gynecol. 2011;205(6):S2–10. doi:10.1016/j.ajog.2011.09.028
14. Getahun D, Oyelese Y, Salihu HM, Ananth CV. Previous cesarean delivery and risks of placenta previa and placental abruption. Obstet Gynecol. 2006;107(4):771–778. doi:10.1097/01.AOG.0000206182.63788.80
15. Jauniaux E, Ayres-de-Campos D, Langhoff-Roos J. FIGO consensus guidelines on placenta accreta spectrum disorders: introduction. Int J Gynecol Obstet. 2019;145(1):1–2. doi:10.1002/ijgo.12839
16. Landon MB, Hauth JC, Leveno KJ, et al. Maternal and perinatal outcomes associated with a trial of labor after prior cesarean delivery. N Engl J Med. 2004;351(25):2581–2589. doi:10.1056/NEJMoa040405
17. Zhang L, Li H, Li J, et al. Prediction of iatrogenic preterm birth in patients with scarred uterus: a retrospective cohort study in Northeast China. BMC Pregnancy Childbirth. 2020;20(1):490. doi:10.1186/s12884-020-03165-7
18. Liu S, Liston RM, Joseph KS, et al. Maternal mortality and severe morbidity associated with low-risk planned cesarean delivery versus planned vaginal delivery at term. CMAJ. 2007;176(4):455–460. doi:10.1503/cmaj.060870
19. Silver RM, Landon MB, Rouse DJ, et al. Maternal morbidity associated with multiple repeat cesarean deliveries. Obstet Gynecol. 2006;107(6):1226–1232. doi:10.1097/01.AOG.0000219750.79480.84
20. Wu S, Kocherginsky M, Hibbard JU. Abnormal placentation: twenty-year analysis. Am J Obstet Gynecol. 2005;192(5):1458–1461. doi:10.1016/j.ajog.2015.06.163
21. Lumbiganon P, Laopaiboon M, Gülmezoglu AM, et al. Method of delivery and pregnancy outcomes in Asia: the WHO global survey on maternal and perinatal health 2007–08. Lancet. 2010;375(9713):490–499. doi:10.1016/S0140-6736(09)61870-5
22. Liu X, Landon MB, Cheng W, Chen Y. Cesarean delivery on maternal request in China: what are the risks and benefits? Am J Obstet Gynecol. 2015;212(6):817. doi:10.1016/j.ajog.2015.01.043
23. Chen I, Opiyo N, Tavender E, et al. Non-clinical interventions for reducing unnecessary caesarean section. Cochrane Database Syst Rev. 2018;9(9):CD005528. doi:10.1002/14651858.CD005528.pub3
24. Chen Y, Liu H. Changes of indications for cesarean section. Chin J Obstet Emerg Electron. 2020;2:65–68. doi:10.3877/cma.j.issn.2095-3259.2020.02.001
25. Zwart JJ, Richters JM, Öry F, de Vries JI, Bloemenkamp KW, van Roosmalen J. Uterine rupture in the Netherlands: a nationwide population-based cohort study. BJOG. 2009;116(8):1069–1078. doi:10.1111/j.1471-0528.2009.02136.x
26. Guise JM, McDonagh MS, Osterweil P, Nygren P, Chan BKS, Helfand M. Systematic review of the incidence and consequences of uterine rupture in women with previous caesarean section. Br Med J. 2004;329(7456):19–25. doi:10.1136/bmj.329.7456.19
27. Miller DA, Chollet JA, Goodwin TM. Clinical risk factors for placenta previa-placenta accreta, clinical expert series. Am J Obstet Gynecol. 2017;217(4):422–429. doi:10.1016/j.ajog.2017.05.007
28. Gao -L-L, Huang Z-J, Shen K, Xu H, Yan S-Q, Muryy A. The optimal timing of the subsequent pregnancy after cesarean section: a systematic review and meta-analysis. Sci Rep. 2016;6:35805. doi:10.1038/srep35805
29. Gonzalez N, Tulandi T. Cesarean scar pregnancy: a systematic review. J Minim Invasive Gynecol. 2017;24(5):731–738. doi:10.1016/j.jmig.2017.02.020
30. Bujold E, Gauthier RJ. Risk of uterine rupture associated with an interdelivery interval between 18 and 24 months. Obstet Gynecol. 2010;115(5):1003–1006. doi:10.1097/AOG.0b013e3181d992fb
31. Schummers L, Hutcheon JA, Hernandez-Diaz S, et al. Association of short interpregnancy interval with pregnancy outcomes according to maternal age. JAMA Intern Med. 2018;178(12):1661–1670. doi:10.1001/jamainternmed.2018.4696
32. Glick I, Kadish E, Rottenstreich M. Expert consensus on the management of subsequent pregnancy in advanced age women with scarred uterus. Chin J Pract Gynecol Obstet. 2021;37(5):558–563. doi:10.19538/j.fk2021050114
33. Milazzo GN, Catalano A, Badia V, Mallozzi M, Caserta D. Myoma and myomectomy: poor evidence concern in pregnancy. J Obstet Gynaecol Res. 2017;43(12):1789–1804. doi:10.1111/jog.13437
34. Smith JR, Woodruff JD. Pregnancy following myomectomy. Obstet Gynecol. 2015;125(4):869–874. doi:10.1097/AOG.0000000000000729
35. Dalal A, Sachar N, Nagar D, Choudhary D, Das CJ, Mittal S. Pregnancy outcome after myomectomy. Int J Reprod Contracept Obstet Gynecol. 2017;6(8):3237–3241. doi:10.18203/2320-1770.ijrcog20173290
36. ACOG Practice Bulletin no. 205. ACOG practice bulletin No. 205: vaginal birth after cesarean delivery. Obstet Gynecol. 2019;133(2):e110–127. doi:10.1097/AOG.0000000000003078
37. ACOG Practice bulletin no. 115. ACOG Practice bulletin no. 115: vaginal birth after previous cesarean delivery. Obstet Gynecol. 2010;116(2 Pt 1):450–463. doi:10.1097/AOG.0b013e3181eeb251
38. Okada H, Kuhn C, Feillet H, Bach JF. The hygiene hypothesis’ for autoimmune and allergic diseases: an update. Clin Exp Immunol. 2010;160(1):1–9. doi:10.1111/j.1365-2249.2010.04139.x
39. Martel MJ, MacKinnon CJN. 155-Guidelines for vaginal birth after previous caesarean birth. J Obstet Gynaecol Can. 2018;40(3):e195–207. doi:10.1016/j.jogc.2018.01.014
40. Dy J, DeMeester S, Lipworth H, Barrett J. No. 382-Trial of labour after caesarean. J Obstet Gynaecol Can. 2019;41(7):992–1011. doi:10.1016/j.jogc.2018.11.008
41. Chen YT, Hsieh YC, Shen H, Cheng CH, Lee KH, Torng PL. Vaginal birth after cesarean section: experience from a regional hospital. Taiwan J Obstet Gynecol. 2022;61(3):422–426. doi:10.1016/j.tjog.2022.03.006
42. Spong CY, Landon MB, Gilbert S, et al. Risk of uterine rupture and adverse perinatal outcome at term after cesarean delivery. Obstet Gynecol. 2007;110(4):801–807. doi:10.1097/01.AOG.0000284622.71222.b2
43. Al-Zirqi I, Stray-Pedersen B, Forsén L, Vangen S. Uterine rupture after previous caesarean sections. BJOG. 2010;117(7):809–820. doi:10.1111/j.1471-0528.2010.02533.x
44. Chen B, Zhang L, Wang D, et al. Nomogram to predict postpartum hemorrhage in cesarean delivery for women with scarred uterus: a retrospective cohort study in China. J Obstet Gynaecol Res. 2020;46(9):1772–1782. doi:10.1111/jog.14354
45. Kennare R, Tucker G, Heard A, Chan A. Risks of adverse outcomes in the next birth after a first cesarean delivery. Obstet Gynecol. 2007;109(2 Pt 1):270–276. doi:10.1097/01.AOG.0000250469.23047.73
46. Kok N, Wiersma IC, Opmeer BC, de Graaf IM, Mol BW, Pajkrt E. Sonographic measurement of lower uterine segment thickness to predict uterine rupture during a trial of labor in women with previous Cesarean section: a meta-analysis. Ultrasound Obstet Gynecol. 2013;42(2):132–139. doi:10.1002/uog.12479
47. Martins WP, Barra DA, Gallarreta FM, Nastri CO, Filho FM. Lower uterine segment thickness measurement in pregnant women with previous Cesarean section: reliability analysis using two- and three-dimensional transabdominal and transvaginal ultrasound. Ultrasound Obstet Gynecol. 2009;33(3):301–306. doi:10.1002/uog.6224
48. Grobman WA, Gilbert S, Landon MB, et al. Outcomes of induction of labor after one prior cesarean. Obstet Gynecol. 2007;109(2 Pt 1):262–269. doi:10.1097/01.AOG.0000254169.49346.e9
49. Shinar S, Walsh L, Roberts N, et al. Timing of cesarean delivery in women with ≥2 previous cesarean deliveries. Am J Obstet Gynecol. 2022;226(1):110.e1–110.e10. doi:10.1016/j.ajog.2021.07.018
50. Chiossi G, Lai Y, Landon MB, et al. Timing of delivery and adverse outcomes in term singleton repeat cesarean deliveries. Obstet Gynecol. 2013;121(3):561–569. doi:10.1097/AOG.0b013e3182822193
51. Gulino FA, Ettore C, Ettore G. A review on management of caesarean scar pregnancy. Curr Opin Obstet Gynecol. 2021;33(5):400–404. doi:10.1097/GCO.0000000000000734
52. Noël L, Thilaganathan B. Caesarean scar pregnancy: diagnosis, natural history and treatment. Curr Opin Obstet Gynecol. 2022;34(5):279–286. doi:10.1097/GCO.0000000000000808
53. Timor-Tritsch IE. Cesarean scar pregnancy: a therapeutic dilemma. Ultrasound Obstet Gynecol. 2021;57(1):32–33. doi:10.1002/uog.23549
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
