Back to Journals » Therapeutics and Clinical Risk Management » Volume 18
Percutaneous Internal Ring Suturing (PIRS) – The Benefits of Laparoscopic Inguinal Hernia Repair
Authors Wolak PK , Strzelecka A, Piotrowska - Gall A , Wolak PP, Piotrowska I , Dąbrowska K, Wróbel J , Nowak-Starz G
Received 11 November 2021
Accepted for publication 17 January 2022
Published 22 February 2022 Volume 2022:18 Pages 135—144
DOI https://doi.org/10.2147/TCRM.S348197
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Garry Walsh
Przemysław Karol Wolak,1,2 Agnieszka Strzelecka,1 Aneta Piotrowska - Gall,1,2 Piotr Przemysław Wolak,3 Ilona Piotrowska,4 Katarzyna Dąbrowska,5 Joanna Wróbel,1 Grażyna Nowak-Starz1
1Collegium Medicum, Jan Kochanowski University of Kielce, Kielce, Poland; 2Department of Pediatric Surgery, Urology and Traumatology, Regional Hospital in Kielce, Kielce, Poland; 3City Hospital of Zabrze, Zabrze, Poland; 4Regional Hospital in Kielce, Kielce, Poland; 5Department of Neonatology and Neonatal Intensive Care, Polish Mother’s Memorial Hospital Research Institute, Łódź, Poland
Correspondence: Przemysław Karol Wolak, Tel +48 501 525 549, Email [email protected]
Introduction: The laparoscopic inguinal hernia repair in children using the PIRS technique is a well-established method. However, there are still opinions that this method does not bring more benefits than open surgery.
Purpose: The study aims to demonstrate the benefits of laparoscopic technique over conventional, open techniques.
Patients and Methods: We conducted a retrospective study that included children aged 0– 18 treated using the PIRS technique in 2008– 2016. The control group consisted of patients treated with the traditional, open method of inguinal hernia repair. A total of 276 children were qualified for laparoscopic surgery, and there were 274 patients in the control group. A full laparoscopic procedure was performed on 247 patients. Assessment of the pathology of the internal inguinal ring was done in all patients during the laparoscopic procedure. Intraoperatively 79 children had bilateral inguinal hernia diagnosed, 133 right-sided inguinal herniae, and 57 left-sided inguinal herniae. The occurrence of hernia was not confirmed in 7 children, whereas 53 patients had open contralateral patent processus vaginalis. In a case of contralateral patent processus vaginalis, the repair was performed using the PIRS method.
Results: The recurrence of the inguinal hernia was observed in 10 children in the laparoscopic group and in 5 cases in control group. The duration of the procedure was noted and compared to open inguinal hernia repair. There was a statistically shorter duration of the laparoscopic method. In the control group, there were 16 patients with a metachronous contralateral inguinal hernia.
Conclusion: The laparoscopic inguinal hernia repair was associated with a better assessment of hernia pathology, shorter operative time, and lower risk of contralateral hernia repair.
Keywords: inguinal hernia, PIRS, children, laparoscopy
Introduction
Inguinal hernia in children is one of the most common conditions faced by pediatric surgeons in everyday practice. It is estimated that the possibility of occurrence of inguinal hernia is 0.8–4.4% of the total number of children.1 The majority of children report congenital oblique inguinal hernia.
Even though inguinal hernia repair is one of the most commonly performed procedures in pediatric surgery, there is still a lack of consensus on which technique: laparoscopic or open, is superior. There are plenty of technical variations of laparoscopic hernia repair, which differ in their outcomes. The laparoscopic approach comes with obvious advantages like better visualization of the inguinal canal, better cosmesis, faster recovery, and the ability to detect contralateral patent processus vaginalis. There are fewer technical variations in open inguinal hernia repair, and their outcomes differ significantly. Despite the described benefits of the laparoscopic approach, open inguinal hernia repair is still preferable in most pediatric surgery centers.
There were several systematic reviews published comparing laparoscopic versus open repair. However, a limited number of studies provide level 1a evidence, and many outcome parameters have not been addressed. As a result, the debate about the best treatment strategies is still ongoing.2–6
One of the most commonly used laparoscopic approaches in Poland is the percutaneous internal ring suturing technique (PIRS) proposed by Patkowski in 2006.7,8 Our analysis addresses parameters that make this approach superior to conventional methods used in inguinal hernia repair in children.
Materials and Methods
Study Design
All patients presenting with a complaint of inguinal hernia were interviewed for the clinical symptoms and examined. The examination included a physical exam, and abdominal and inguinal ultrasonography, which neither confirmed nor excluded the possibility of hernia’s occurrence. An experienced surgeon was proposing surgical treatment in cases with evident inguinal hernia. In cases with inconclusive diagnosis and strong guardians’ desire to opt for the surgery, the laparoscopic approach was advised. Similarly, patients diagnosed with bilateral hernia were offered a laparoscopic method.
Guardians were informed about the proposed type of treatment by the surgeon who was going to perform the inguinal hernia repair. The team consisted of one experienced surgeon operating with the PIRS technique and eleven experienced surgeons operating with the open technique. Guardians’ requests for the preferred technique were always respected, and in those cases, the operating surgeon was changed. All surgeries were performed under general anesthesia with endotracheal intubation.
Description of the Study Group
The study group included 276 children treated for an inguinal hernia between May 2008 and December 2016 in the Department of Pediatric Surgery, Urology, and Traumatology in Kielce (Poland). Two hundred and forty-seven patients were operated using the laparoscopic PIRS method. Twenty-nine patients initially planned for the laparoscopic method underwent conversion due to inability to secure the proper closure. In cases of the wide opening of the internal inguinal ring, the attempt of closure with 1–2 stitches was taken. When incomplete closure was observed, the decision of conversion was made in order to create a tight closure, additionally guarded by surrounding tissue. All of the PIRS operations were performed by one experienced surgeon. The access to the abdominal cavity was obtained by the open Hasson technique. The majority of the patients were operated with the 3.5 mm telescope. In cases where the umbilical ring was dilated, the telescope 5 mm was used. In two cases of boys over the age of 15, the 3D 10 mm telescope was introduced. All laparoscopic hernia repairs were performed with a 30° angle view. The CO2 insufflation pressure in the peritoneal cavity was maintained at 8 to 12 mmHg depending on the patients’ age. The procedure was performed as described by Patkowski.7,8 This involves placing an injection needle with a non-absorbable thread inside the barrel of the needle through the abdominal wall into the peritoneal cavity under laparoscopic-guided vision. The thread passes under the peritoneum around the entrance into the hernia sac by moving the injection needle. The knot is tightened from the outside and placed in the subcutaneous space. In 14 cases, an additional 3.5-mm or 5.0-mm port was placed in the right lower abdominal quadrant, and a supplementary instrument (grasper or dissector) was used. Further, an inspection of the abdominal cavity was performed for other anomalies (assessment of pelvic organs, bowel, and gonads in cases of strangulated hernia). Routinely before the surgery, the bladder was not emptied. If the visibility was compromised, catheterisation of the bladder was performed during the procedure. The duration of anesthesia and surgery was recorded.
Description of the Control Group
The control group consisted of 274 patients operated with the open inguinal repair method between January 2013 and December 2014 in our department by other experienced surgeons. All children were operated using the same open method, which included dissection of the vas deferens and vessels and ligation of the hernia sac. Additionally, the anterior wall of the inguinal canal was repaired (using modified Girard method).
The data on feasibility, duration of the procedures, and additional findings were recorded and compared. The aspect of recurrence rate and contralateral patent processus vaginalis was also analyzed for both groups.
The Statistical Analysis
The type of analyzed variables was the criterion for selecting analytic methods. The measures of location (mean, median, quartiles) and the measure of statistical dispersion (standard deviation) were calculated for quantitative variables to compare several means – average duration of surgery (depending on the type of hernia) – ANOVA test was used. The χ2 test was used to find the differences between the studied populations. The level of significance was set at α = 0.05 in the studies. The data were collected in an Excel spreadsheet (Microsoft MS Office). Statistical data analyses were carried out using STATISTICA ver. 13.1 software (StatSoft).
Results
Patients Demographics
The study consisted of 131 girls and 145 boys and (sex ratio: 0.9:1) and in control group: 40 girls and 234 boys (sex ratio: 0.17:1). Operated patients were aged 0–18, with an average age of 4 years 10 months. The youngest patient was 3-week old and the oldest 17 years 5 months (Table 1).
 |
Table 1 Patients’ Demographics |
Preoperative and Intraoperative Diagnosis
There were 317 PIRS procedures performed in 276 patients. All preoperative diagnoses were compared to the intraoperative findings.
The most common preoperative diagnosis in the study group was the right-sided hernia (n = 165). The left-sided hernia accounted for 82 patients and bilateral 29 cases.
During the laparoscopic procedure, the diagnosis was evaluated in the presence of contralateral patent processus vaginalis (CPPV). The diagnosis needed correction in 53 patients. The bilateral inguinal hernia rate increased from 29 to 79 cases. The preoperative diagnosis of left-sided hernia was not confirmed intraoperatively in 25 out of 82 cases. In a total of 7 cases, despite the initial diagnosis of unilateral hernia, the internal opening of the inguinal canal was closed. Two girls (one of whom was operated on due to suspected recurrency after open approach) and five boys (three of whom had a clinical diagnosis of bilateral hernia) represented 2.54% of children operated on for inguinal hernia not confirmed during laparoscopy.
There is a statistically significant difference between preoperative and intraoperative diagnosis in the studied group (p = 0000) (Table 2).
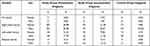 |
Table 2 Preoperative and Intraoperative Diagnosis vs Sex in the Study and Control Group |
Among girls with hernias on the one side, the contralateral internal inguinal ring was open in 28 cases. Diagnosis of bilateral inguinal hernia in females is an indicator for screening for Androgen Insensitivity Syndrome, which can be conducted during laparoscopic exploration. Other significant changes in diagnosis consisted of a decrease by 16 cases in unilateral left-sided inguinal hernia rate in males. A statistically significant difference in diagnosis in both sexes was noted (males and females p = 0000) (Figures 1 and 2).
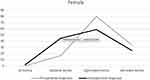 |
Figure 1 Preoperative and intraoperative diagnosis vs sex (female). |
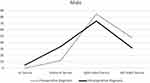 |
Figure 2 Preoperative and intraoperative diagnosis vs sex (male). |
An indirect hernia was diagnosed in the majority of cases. In two patients, a direct inguinal hernia was noted.
In the control group, no change in diagnosis was noted. There was no negative exploration reported, and no direct hernia was observed in the control group. During the follow-up period, a metachronous contralateral inguinal hernia developed postoperatively in 16/274 patients who underwent unilateral hernia repair.
Operating Time
The duration of the procedure was noted and compared to open inguinal hernia repair (clinical control group). The duration of the procedure was calculated from the cleaning of the surgical site to the dressing of postoperative wounds. In the case of a one-sided PIRS procedure, the mean duration was 26 minutes 35 seconds (10 minutes – 55 minutes), a bilateral inguinal hernia – 32 minutes 40 seconds (17 minutes – 60 minutes). The open unilateral inguinal hernia repair duration was 36 minutes and 10 seconds. The mean anesthesia time was measured from the start of intravenous drug administration and putting on an oxygen mask until the patient’s extubation in the operating room. The mean anesthesia time for unilateral hernia treated laparoscopically was 45 minutes 55 seconds, and for bilateral hernia – 51 minutes and 55 seconds. In the control group, the mean anesthesia time was 43 minutes and 15 seconds. The median time of surgery for bilateral and left-sided hernia equals Me = 30. The median time for diagnosis of the right-sided hernia is Me = 25 (Table 3). The operation’s duration is statistically significant depending on the type of hernia diagnosed during the operation (p = 0.000). There was no relation between patient age and duration of the surgery in the study (r=−0.1371) (Table 4).
 |
Table 3 Duration of the Laparoscopic Surgery Analysis |
 |
Table 4 Comparison of the Study and the Control Group |
Contralateral Patency
In this study, there were 53 cases of open deep inguinal rings on the contralateral side (contralateral patent processus vaginalis – CPPV). It counted for 23/82 left-side inguinal hernia with right CPPV and 30/165 right-side hernia with left CPPV. Out of the 25 boys, 11 reported a left-sided CPPV and 14 a right-sided CPPV. In girls, there were 19 cases of left-sided CPPV and 9 cases of the right-sided CPPV. In the control group, no CPPV was noted during the procedure (Table 4).
Recurrence Rate and Metachronous Contralateral Hernia
Recurrence was observed in 10 patients after the laparoscopic surgery, which accounts for 4.04% (10/247) of the total number of surgeries and 3.15% (10/317) of PIRS procedures. Five of them underwent inguinal hernia repair using the PIRS method, two with the open method, and the remaining 3 awaits the surgery due to the lack of the parental consent.
The control group’s recurrence rate was observed in five cases (1.82%), and 16 children (5.84%) required additional procedure due to the metachronous contralateral inguinal hernia.
Additional Findings
Out of 14 children operated for incarcerated hernia, an unreduced hernia was identified in 10 cases (5%). During the laparoscopic procedure, it was possible to reduce incarcerated organs and assess the organs of the abdominal and pelvic cavity. In the laparoscopic group, there were two girls with the strangulated ovary, and one boy reported with testicular ischemia due to strangulated greater omentum. In the control group, there were 20 children operated due to the incarcerated hernia. All patients had intestinal viability assessed. None of the incarcerated gonads required removal, and subsequent postoperative ultrasonographic examinations reported proper blood flows and no signs of gonadal atrophy. In the laparoscopic group, all abdomen cavities were assessed, which was not possible in the control group.
All-female patients with bilateral herniae (45 girls) had the presence of the uterus and uterine appendages assessed. In the study group, there was a case of a patient diagnosed with CAIS during the laparoscopic inguinal hernia repair procedure. This case was also described in our original series.9
In 6 cases, intestinal pathology was observed. In 5 children, there was intestinal malrotation, and one had Meckel diverticulum noted. Those children were subjected to intense postoperative control, and their parents/legal guardians were instructed about the possible consequences of the detected anomalies.
The laparoscopic method had an additional advantage. For children with an umbilical hernia, the reconstruction of the umbilicus was performed. In ten cases, the umbilical hernia was diagnosed preoperatively. Additionally, in 10 children, a widened umbilical ring was detected and classified for the reconstruction.
Follow Up
The average post-operative follow-up was 70.6 months (5.9 years) for the study group. The average follow-up for the control group was 67.7 months (5.6 years).
The recurrence incidence after the PIRS procedure is 2.4 times higher than after open repair, although this is not statistically significant (OR = 2376; 95% CI: 0.800–7.058; p = 0.119).
The CPPV is diagnosed four times more often during laparoscopy, and there is a statistical significance (OR = 0.3935, 95% CL: 2185–7084; p = 0.000).
Discussion
Risk of Developing MCH
Clinically diagnosed inguinal hernia can be scheduled for open surgery or using minimally invasive techniques. Laparoscopy gives a clear view of the structures inside the abdominal and pelvic cavity,10 while open inguinal hernia repair allows the exploration of the affected site. Data suggest that it is possible to explore the opposite side through the deep inguinal ring during open repair of groin hernia.11 Although it is a complicated procedure, it is frequently impossible due to a full bladder and abdominal organs. Without the CO2 insufflation into the abdominal cavity, the procedure is rather impractical due to the angle of the camera. In our control group, 5% of patients required additional surgery due to the development of metachronous contralateral hernia.
The incidence of metachronous contralateral inguinal hernias was presented by Wenk et al12 who described and analyzed six studies, including 1669 children. The overall incidence was 6%. It was noted that the risk of metachronous contralateral inguinal hernia development is significantly greater in children with an initial left-sided hernia (8.5% vs 3.3%) and children with open contralateral processes vaginalis (13.8% vs 3%). Further risk factors include female gender (8.2% vs 4.1%) and young age <1 year (6.9% vs 4.5%).12 In the study conducted by Thomas et al13 in 16.4% (n = 35) of children contralateral metachronous hernia was found. The right-sided hernias appeared more frequently (57.1%).
Another interesting retrospective study was presented by Chin et al regarding second inguinal hernia repairs. It was estimated that the incidence of contralateral metachronous hernia was 9.62%, and the ipsilateral recurrent hernia was 1.23%.14 The incidence of a metachronous contralateral pediatric inguinal hernia is 6.4% in both genders.15
Incidence of CPPV
The incidence of CPPV according to the literature ranges from 4% to 40%.2–27 In study group 19% of children had CPPV treated. Esposito et al, in his study, noted that 41% (n = 533) of patients undergoing unilateral laparoscopic inguinal hernia repair had CPPV.27 Erginel et al presented a study on 205 inguinal hernia repairs in 148 girls. It was noted that preoperative diagnosis consisted of 51.3% right-sided hernia, 27.7% left-sided and 20.9% bilateral hernia. However, in 26 girls, the CPPV was visualised during the laparoscopic procedure and repaired with the PIRS method. In total 38.5% (n = 57) girls had bilateral hernias.19
Incidence of Negative Exploration
Laparoscopy also allows to detect patients with false-positive inguinal hernia and to often avoid an unnecessary extensive exploration of the inguinal canal in this group of patients.28 Other authors have analyzed the problem of the possible occurrence of metachronous inguinal hernia. Despite a true negative evaluation by laparoscopy, there was a 0.8% chance of developing a metachronous contralateral inguinal hernia. Watanabe et al reported that of the 992 patients with negative CPPV at initial operation, eight children (7 boys and one girl) had metachronous contralateral inguinal hernia after the first operation. This phenomenon is male-oriented and may be acquired by indirect inguinal hernia without preceding open contralateral processus vaginalis.16
Risk of Development of Symptomatic Hernia from PPV
The question for further analysis is whether a patent processus vaginalis or clinically silent contralateral hernia may develop into a symptomatic hernia. Some anatomical abnormalities of the inguinal canal may not manifest themselves during the childhood period. Frequently, children aged 10–14 years are brought for hernia repair with active symptoms for several weeks or months.17,24
It seems that laparoscopic closure of open internal inguinal ring brings the benefits of avoiding future surgery. During the laparoscopic procedure, the type of hernia may be defined, as direct, indirect (oblique), and double hernia. Esposito et al reported that 97.9% of patients had an oblique external hernia, 1.6% (n = 21) of cases had a direct hernia, and a double hernia on the same side (hernia en pantalon) was noted in 0.5% (n = 6).27 Schier F. analyzed 542 children and found that the majority were congenital oblique hernias (93%), followed by direct hernias – 10 cases (2.3%), femoral – 4 cases (1%), hernia en pantalon – 3 cases, and the combination of femoral hernia and oblique inguinal hernia in one child.23
Risk of Recurrence
Another aspect discussed in terms of inguinal hernia repair is the risk of recurrence.29–31 The recurrence incidence, stressed by numerous authors, is only slightly higher after the laparoscopic treatment than after the traditional, open surgery.10,18,23,29,32 However, there are authors who, over a long period of observation, did not report any recurrence of hernia after the laparoscopic surgery.22,25 It should also be emphasized that the laparoscopic method, such as the PIRS technique, requires much less intervention in the inguinal canal than the traditional method. Frequently, it is easier to treat hernia laparoscopically in the case of hernia recurrence after the open surgery. At the same time, in the case of open surgery of the recurrent hernia previously treated laparoscopically, there is virtually a “pristine” operating field with no disturbances of anatomical structures due to adhesions. Such situations were observed in our study. One girl was successfully operated on laparoscopically after two traditional surgeries of left-sided inguinal hernia (primary surgery and recurrence). At the same time, there were patients with recurrent hernia treated with the PIRS method who, in the case of recurrence, did not give their consent for laparoscopic surgery and were operated with an open technique. In such cases, surgeons in their operating reports stress the fact that the operating field was as unchanged as if the patient was operated on for the first time. The number of recurrences after surgery and the need to re-do surgery does not balance the need to operate the patients after the metachronous occurrence of inguinal hernia in children operated traditionally.29
Assessment of Incarcerated Organs
Another advantage in children operated on due to inguinal hernia, especially after its incarceration and discharge, is the assessment of ovaries, testes, intestines, and other structures present in the hernia sac. During surgery, ovaries were found in 3 patients, tuba uterine in 2 patients, and in one patient, the omentum was sliding into hernia sacs.19 Esposito et al found an incarcerated hernia in 27 cases (2%).27 In another study, the same author observed 46 children with incarcerated inguinal hernias (7.6% of all procedures due to the presence of inguinal hernia). Twenty-one of 46 children were reduced preoperatively and then operated laparoscopically, 25/46 were irreducible, and they operated directly in laparoscopy. In the first group, the operation time was 23 minutes, and the second group was 30 minutes. There was one recurrence of hernia in both groups, while the scientific literature shows the recurrence incidence in such a situation at 15–20%.33 Houben et al reported a 1.6% (n = 34) incidence of irreducible inguinal hernia after reduction attempts by the attending surgeon. The majority (70%) were seen on the right side. The laparoscopic method was used in 24 patients. The content of incarcerated hernia consisted of intestines (21 cases), omentum (4 patients). Three girls had incarcerated ovaries. Following incarceration, four children required a resection of the necrotic intestine, one ovary was removed, and one boy was operated on due to testicular atrophy (6 months after the first surgery).34
Additional Findings
Another advantage of the laparoscopic treatment of inguinal hernia is the possibility to detect other defects in the pelvis and abdomen. It also allows the inspection of female reproductive organs, such as ovaries, fallopian tubes, and uterus.28,35 In our material, we observed the complete androgen insensitivity syndrome (CAIS),36 where male gonads moved to inguinal canals on both sides in phenotypically 4-year-old girl.21,23 In laparoscopy, it is possible to observe the disorders in the bowel movement, determine the presence of the Meckel’s diverticulum (a similar case was discussed by Quail et al)37 and to assess the position of the appendix. Another aspect of laparoscopic surgery is the reconstruction of the navel after removing the port – this avoids treatment of the umbilical hernia. An integral part of any laparoscopy is the closure of an opening after the removal of an umbilical trocar. Laparoscopic surgery damages the nerves around the inguinal canal to a lesser extent than the open surgery. The PIRS procedure was found to be safe and easily applicable and caused no damage to the ilioinguinal nerve.38
The patient should be appropriately prepared for each laparoscopic procedure, and their urinary bladder should be emptied. Payiziwula et al reported in early postoperative time a sliding hernia not recognized during laparoscopic inguinal hernia repair (bladder herniating into the right inguinal region, consistent with an extraperitoneal invisible, undetectable hernia).35
The treatment of sliding hernia was discussed by Ishii et al, who in the years 2006–2015, operated 482 girls, 14 of whom had invisible inguinal hernia diagnosed preoperatively.39
Feasibility of the PIRS Method
The simplicity of the PIRS method allows it to be used during other surgical procedures done laparoscopically. In our material, there were two cases of inguinal hernia repair performed during laparoscopy for non-complicated appendicitis. Erginel et al made similar observations. There were two cases of inguinal hernia repair during appendectomy and one during laparoscopic splenectomy.19 The same study discusses an obvious benefit of using laparoscopy for other reasons – we can evaluate the degree of the inguinal canal repair after the previous treatment of inguinal hernia performed both openly and laparoscopically. Closed internal inguinal rings were observed in a second-look laparoscopy in 2 patients as a suspected recurrent hernia after PIRS procedures.19 Similar observations were made in our previous material.9,11 Another advantage of laparoscopic methods over the traditional ones is shorter operative and anesthesia time and faster recovery time.19,40 Most authors stress the aesthetic aspect of the laparoscopic method, with minimal or invisible scars after the surgery.20,21,23 Thanks to its simplicity and the possibility to repair other anomalies, laparoscopy has an advantage over traditional methods and should become a method of choice for an experienced surgeon in the treatment of inguinal hernia in children, especially in girls.7,8,13,19–21,25–27,39
Conclusions
The laparoscopic approach to inguinal hernia repair is feasible as it is associated with a significantly shorter duration of surgery and anesthesia. It allows making a proper diagnosis with detection and closure of CPPV. Laparoscopy also brings the possibility of inspection of abdominal and pelvic organs and assessment after incarceration.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Research Committee of Jan Kochanowski University Research Ethics Board, nr 12/2016.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. The parent or legal guardian of each child provided informed consent.
Funding
This work was supported under the program of the Minister of Science and Higher Education under the name Regional Initiative of Excellence in 2019–2022 project number: 024/RID/2018/19, financing amount: 11.999.000.00 PLN.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Miltenburg DM, Nuchtern JG, Jaksic T, Kozinetiz C, Brandt ML. Laparoscopic evaluation of the pediatric inguinal hernia—a meta-analysis. J Pediatr Surg. 1998;33:874–879. doi:10.1016/S0022-3468(98)90664-9
2. Kantor N, Travis N, Wayne C, Nasr A. Laparoscopic versus open inguinal hernia repair in children: which is the true gold-standard? A systematic review and meta-analysis. Pediatr Surg Int. 2019;35(9):1013–1026. doi:10.1007/s00383-019-04521-1
3. Nakashima M, Ide K, Kawakami K. Laparoscopic versus open repair for inguinal hernia in children: a retrospective cohort study. Surg Today. 2019;49(12):1044–1050. doi:10.1007/s00595-019-01847-0
4. Dreuning K, Maat S, Twisk J, van Heurn E, Derikx J. Laparoscopic versus open pediatric inguinal hernia repair: state-of-the-art comparison and future perspectives from a meta-analysis. Surg Endosc. 2019;33(10):3177–3191. doi:10.1007/s00464-019-06960-2
5. Fujiogi M, Michihata N, Matsui H, Fushimi K, Yasunaga H, Fujishiro J. Outcomes following laparoscopic versus open surgery for pediatric inguinal hernia repair: analysis using a national inpatient database in Japan. J Pediatr Surg. 2019;54(3):577–580. doi:10.1016/j.jpedsurg.2018.03.015
6. Al-Taher RN, Khrais IA, Alma’aitah S, et al. Is the open approach superior to the laparoscopic hernia repair in children? A retrospective comparative study. Ann Med Surg. 2021;71:102889. doi:10.1016/j.amsu.2021.102889
7. Patkowski D, Chrzan R, Jaworski W, Apoznański W, Czernik J. Percutaneous internal ring suturing for inguinal hernia repair in children under three months of age. Adv Clin Exp Med. 2006;15:851–856.
8. Patkowski D, Czernik J, Chrzan R, Jaworski W, Apoznański W. Percutaneous internal ring suturing: a simple minimally invasive technique for inguinal hernia repair in children. J Laparoendosc Adv Surg Tech. 2006;16:513–517. doi:10.1089/lap.2006.16.513
9. Wolak P. Laparoscopy in inguinal hernia and complete androgen insensitivity syndrome in children whether and when to remove the gonads because of cancer? Medical Studies/Studia Medyczne. 2015;31:277–280.
10. Esposito C, St. Peter SD, Escolino M, Juang D, Settimi A, Holcomb GW. Laparoscopic versus open inguinal hernia repair in pediatric patients: a systematic review. J Laparoendosc Adv Surg Tech. 2014;24:811–818. doi:10.1089/lap.2014.0194
11. Sajid MS, Ladwa N, Colucci G, Miles WFA, Baig MK, Sains P. Diagnostic laparoscopy through deep inguinal ring: a literature-based review on the forgotten approach to visualize the abdominal cavity during emergency and elective groin hernia repair. Surg Laparosc Endosc Percutan Tech. 2013;23(3):251–254. doi:10.1097/SLE.0b013e31828dacc5
12. Wenk K, Sick B, Sasse T, Moehrlen U, Meuli M, Vuille-dit-Bille RN. Incidence of metachronous contralateral inguinal hernias in children following unilateral repair — a meta-analysis of prospective studies. J Pediatr Surg. 2015;50:2147–2154. doi:10.1016/j.jpedsurg.2015.08.056
13. Thomas DT, Göcmen KB, Tulgar S, Boga I. Percutaneous internal ring suturing is a safe and effective method for the minimal invasive treatment of pediatric inguinal hernia: experience with 250 cases. J Pediatr Surg. 2016;51:1330–1335. doi:10.1016/j.jpedsurg.2015.11.024
14. Chin TW, Pan ML, Lee HC, Tsai HL, Liu CS. Second hernia repairs in children—a nationwide study. J Pediatr Surg. 2015;50:2056–2059. doi:10.1016/j.jpedsurg.2015.08.024
15. Nataraja R, Mahomed A. Metachronous contralateral pediatric inguinal hernia. Open Access Surgery. 2010;3:87–90.
16. Watanabe T, Yoshida F, Ohno M, et al. Morphology-based investigation of metachronous inguinal hernia after negative laparoscopic evaluation – is it acquired indirect inguinal hernia? J Pediatr Surg. 2016;51:1548–1551. doi:10.1016/j.jpedsurg.2016.03.008
17. Miyake H, Fukumoto K, Yamoto M, et al. Risk factors for recurrence and contralateral inguinal hernia after laparoscopic percutaneous extraperitoneal closure for pediatric inguinal hernia. J Pediatr Surg. 2017;52(2):317–321. doi:10.1016/j.jpedsurg.2016.11.029
18. Lee SR, Choi SB. The efficacy of laparoscopic intracorporeal linear suture technique as a strategy for reducing recurrences in pediatric inguinal hernia. Hernia. 2017;21:425–433. doi:10.1007/s10029-016-1546-y
19. Erginel B, Akin M, Yildiz A, Karadag CA, Sever N, Dokucu AI. Percutaneous internal ring suturing as a first choice laparoscopic inguinal hernia repair method in girls: a single-center study in 148 patients. Pediatr Surg Int. 2016;32:697–700. doi:10.1007/s00383-016-3903-4
20. Shalaby R, Ismail M, Shehata S, et al. Shalaby technique for efficient single incision laparoscopic pediatric inguinal hernia repair. J Pediatr Surg. 2015;50:1995–2000.
21. Wolak PK, Patkowski D. Laparoscopic inguinal hernia repair in children using the percutaneous internal ring suturing technique - own experience. Wideochir Inne Tech Maloinwazyjne. 2014;9:53–58. doi:10.5114/wiitm.2014.40389
22. Watanabe T, Nakano M, Endo M. An investigation on the mechanism of contralateral manifestations after unilateral herniorrhaphy in children based on laparoscopic evaluation. J Pediatr Surg. 2008;43:1543–1547. doi:10.1016/j.jpedsurg.2007.11.010
23. Schier F. Laparoscopic inguinal hernia repair—a prospective personal series of 542 children. J Pediatr Surg. 2006;41:1081–1084. doi:10.1016/j.jpedsurg.2006.02.028
24. Yang C, Zhang H, Pu J, Mei H, Zheng L, Tong Q. Laparoscopic vs open herniorrhaphy in the management of pediatric inguinal hernia: a systematic review and meta-analysis. J Pediatr Surg. 2011(46):1824–1834.
25. Shalaby R, Ismail M, Samaha A, et al. Laparoscopic inguinal hernia repair; experience with 874 children. J Pediatr Surg. 2014;49:460–464. doi:10.1016/j.jpedsurg.2013.10.019
26. Karadağ C, Erginel B, Sever N, Akın M, Yıldız A, Dokucu A. Laparoscopic hernia repair in children: which method is the best? J Exp Clin Med. 2016;33:11–13.
27. Esposito C, Escolino M, Cortese G, et al. Twenty-year experience with laparoscopic inguinal hernia repair in infants and children: considerations and results on 1833 hernia repairs. Surg Endosc. 2017;31:1461–1468. doi:10.1007/s00464-016-5139-8
28. Ramaraj A, Fisher JC. Pseudorecurrence following female laparoscopic inguinal hernia repair in children. J Pediatr Surg Case Rep. 2016;12:21–23. doi:10.1016/j.epsc.2016.06.009
29. Shalaby R, Ismail M, Gouda S, et al. Laparoscopic management of recurrent inguinal hernia in childhood. J Pediatr Surg. 2015;50:1903–1908.
30. Novotny NM, Puentes MC, Leopold R, Ortega M, Godoy-Lenz J. The burnia: laparoscopic sutureless inguinal hernia repair in girls. J Laparoendosc Adv Surg Tech. 2017;27:430–433. doi:10.1089/lap.2016.0234
31. Boo YJ, Han HJ, Ji WB, Lee JS. Laparoscopic hernia sac transection and intracorporeal ligation show very low recurrence rate in pediatric inguinal hernia. J Laparoendosc Adv Surg Tech. 2012;22:720–723. doi:10.1089/lap.2012.0040
32. Gibbons AT, Hanke RE, Casar Berazaluce AM, et al. Recurrence after laparoscopic high ligation in adolescents: a multicenter international retrospective study of ten hospitals. J Pediatr Surg. 2021;56(1):126–129. doi:10.1016/j.jpedsurg.2020.09.026
33. Esposito C, Turial S, Alicchio F, et al. Laparoscopic repair of incarcerated inguinal hernia. A safe and effective procedure to adopt in children. Hernia. 2013;17:235–239. doi:10.1007/s10029-012-0948-8
34. Houben CH, Chan KWE, Mou JWC, Tam YH, Lee KH. Irreducible inguinal hernia in children: how serious is it? J Pediatr Surg. 2015;50:1174–1176. doi:10.1016/j.jpedsurg.2014.10.018
35. Payiziwula J, Zhao P-J, Aierken A, et al. Laparoscopy versus open incarcerated inguinal hernia repair in octogenarians: single-center experience with world review: single-center experience with world review. Surg Laparosc Endosc Percutan Tech. 2019;29(2):138–140. doi:10.1097/SLE.0000000000000629
36. Hurme T, Lahdes-Vasama T, Makela E, Iber T, Toppari J. Clinical findings in prepubertal girls with inguinal hernia with special reference to the diagnosis of androgen insensitivity syndrome. Scand J Urol Nephrol. 2009;43(1):42–46. doi:10.1080/00365590802299247
37. Quail JF, Ignacio RC. Appendicitis associated with a strangulated Littre’s hernia. J Pediatr Surg Case Rep. 2015;3:41–43. doi:10.1016/j.epsc.2014.11.018
38. Kara Ö, Yıldız A, Toydemir HE, et al. Does percutaneous internal ring suturing contain risk of ilioinguinal nerve entrapment? Pediatr Surg Int. 2015;31:485–491.
39. Ishii T, Yonekura T, Yamauchi K, et al. Laparoscopic repair of sliding inguinal hernia in female children. Pediatr Surg Int. 2016;32(9):895–899. doi:10.1007/s00383-016-3935-9
40. Wolak PK, Strzelecka A, Piotrowska A, et al. The operative time for unilateral inguinal hernia repair in children performed with Percutaneous Internal Ring Suturing (PIRS) or open approach method. J Clin Med. 2021;10(6):1293. doi:10.3390/jcm10061293
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
