Back to Journals » Advances in Medical Education and Practice » Volume 13
Perceptions of Lecturers, Administrators, and Students About the Workplace as Learning Environment for Undergraduate Medical Students at a National Referral and Teaching Hospital in Uganda
Authors Kagawa MN , Kiguli S, Steinberg H , Jama MP
Received 4 January 2022
Accepted for publication 19 May 2022
Published 26 May 2022 Volume 2022:13 Pages 555—566
DOI https://doi.org/10.2147/AMEP.S357003
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Md Anwarul Azim Majumder
Mike Nantamu Kagawa,1 Sarah Kiguli,2 Hannes Steinberg,3 Mpho Priscilla Jama4
1Department of Obstetrics & Gynaecology, Makerere University, Kampala, Uganda; 2Department of Paediatrics & Child health, Makerere University, Kampala, Uganda; 3Department of Family Medicine, University of the Free State, Bloemfontein, Republic of South Africa; 4Division Student Learning and Development, Office of the Dean, Faculty of Health Sciences, University of the Free State, Bloemfontein, Republic of South Africa
Correspondence: Mike Nantamu Kagawa, Department of Obstetrics & Gynaecology, Makerere University, Kampala, Uganda, Tel +256772449613, Email [email protected]
Purpose: The workplace is an important element of the learning ecosystem for medical students during their competence development. It offers engagement opportunities that enable students to participate in clinical activities as part of learning in their preparation for future clinical practice. The purpose of this study was to explore the perceptions and experiences of lecturers, administrators, and students of Makerere University College of Health Sciences about the workplace, at Mulago National Referral and Teaching Hospital, as a learning environment for the undergraduate medical students with the ultimate aim of identifying opportunities and challenges to learner competence development in the learning environment for purposes of improvement.
Methods: The study design was cross-sectional descriptive with a qualitative approach using key informant interviews for the lecturers and administrators and focus group discussions for the students. The framework method was used to perform thematic data analysis.
Results: The workplace was perceived to be well endowed with adequate patient numbers, a suitable case mix and unrestricted access to patients which enhanced competence development. The challenges reported included inadequate resources, such as infrastructure, equipment and supplies and overcrowding, which compromised competence development. The resource challenge appeared insurmountable in the context of two autonomous institutions with divergent planning priorities in terms of teaching, research, and patient care.
Conclusion: There were mixed perceptions about the learning environment at the hospital with both enabling and challenging factors on the backdrop of two autonomous institutions with divergent planning priorities in terms of teaching, research, and patient care. In order to improve the workplace as a learning environment, it is imperative that the two institutions find common ground in terms of clinical care, students’ teaching and provision of supplies that are essential not only for patient care but competence development of the learners who are the clinicians of tomorrow.
Keywords: workplace learning, learning ecosystem, competence development, medical education
Introduction
Learning at the workplace is a significant contributor to competence development in preparation for clinical practice.1–3 Competences such as clinical skills, communication and interpersonal skills achieved during learning at the workplace have a significant impact on patient care.4 Clinical medicine is a practical discipline where practice is learnt by practising.5
For effective competence development, the workplace as a learning environment should offer engagement opportunities for students to participate in activities at the workplace according to the highest level allowed by their experience and abilities.6 Additionally, there should be protected time, designated, or protected space and an enthusiastic group of lecturers and students. Assessment, which is known to drive learning, should be an integral part of training where teachers are available to observe the students demonstrate competence while working with real patients in the clinical setting.7,8 The learning environment should be conducive for patients by ensuring that preparation and identification of opportunities for learning at the workplace by both lecturers and students is balanced with acknowledgement of patients’ rights to privacy, confidentiality, and dignity.9,10 Health-care provision has changed over time in terms of health system expectations and clinical practice requirements as well as patient demographics such as patient numbers, expectations and level of education.11,12 A mismatch between graduate competencies and population health requirement has been reported in literature which could be an indictment on the slow pace of change in medical training in response to the changes in health-care delivery.13 Perceptions of stakeholders such as lecturers, administrators, and students about the workplace as a learning environment may therefore provide some insight into the challenges faced in health professions training and whether medical training is moving in tandem with the times.11
At the time of the study, undergraduate medical students of Makerere University College of Health Sciences (MakCHS) had placements in their fourth and fifth year at Mulago National Referral and Teaching Hospital (MNRTH). This placement enabled students to gain exposure to situations similar to those they will encounter when they qualify which is important for their transition from a student identity to that of a clinician.14,15
MakCHS, now a constituent college of Makerere University since 2008, was originally founded in 1924 and is the oldest medical school in East Africa. It is now comprised of four schools: Medicine, Health Sciences, Public Health, and Biomedical Sciences. Mulago Hospital, a 1790-bed capacity hospital was founded in 1913 and was designated the National Referral and Teaching hospital in 1962. The hospital has 10 clinical departments where students rotate for their clinical placements namely, Surgery (General Surgery, Orthopaedics, Cardiothoracic Surgery, Neurosurgery), Obstetrics & Gynaecology, Internal Medicine, Paediatrics & Child health, Ophthalmology, Anaesthesia & Critical Care, and Ear Nose & Throat. Psychiatry placements take place at Butabika Hospital, a separate hospital that is about 9km away.
MakCHS & MNRTH have parallel and autonomous administrative structures and hierarchy of staff involved in clinical patient care and teaching of undergraduate medical students (Figure 1).
 |
Figure 1 Hierarchy of clinical staff at Makerere University College of Health Sciences and Mulago National Referral and Teaching Hospital. |
The purpose of this study was to explore the perceptions of lecturers, administrators, and students about the workplace at MNRTH as a learning environment for undergraduate medical students of MakCHS with the ultimate aim of identifying opportunities and challenges in the learning environment for purposes of improvement to address the reported mismatch between graduate competences and population health needs.
Materials and Methods
Design and Setting
The study design was cross-sectional descriptive with a qualitative approach. Data collection was done using Key Informant Interviews and Focus Group Discussions.
Makerere University College of Health Sciences (MAKCHS) is a constituent college of Makerere University, a national public university located in Kampala, the capital city of Uganda. The college runs a five-year undergraduate medical training program leading to the award of a Bachelor of Medicine and Bachelor of Surgery (MBChB) degree of Makerere University. At the time of the study, the undergraduate medical curriculum was implemented in three phases; an introductory phase that exposed medical students to the normal structure (anatomy) and function (physiology) of the human body. This was followed by the second phase that comprised of learning about human disease and treatment in the form of microbiology, pathology and pharmacology, and finally the phase of clinical experience at the workplace. As the student progressed towards the final year, there was significant reduction in classroom-based teaching with emphasis shifting more towards workplace learning. While there were opportunities for clinical exposure right from the first year of medical school, these were mainly for orientation to the clinical workplace with no formal students–patient interaction for the first three years. During the fourth and fifth year, undergraduate medical students were allocated clinical placements at the workplace to the 10 departments at MNRTH.
Characteristics of Participants
The participants for the Key Informant Interviews were administrators and lecturers from MakCHS & MNRTH. Administrators from MakCHS were the College Principal, Deputy Principal, College Registrar, and School Deans and Registrars. Administrators from MNRTH were the Hospital Executive Director, Deputy Executive Director and the Principal Hospital Administrator. We purposed to include MakCHS and MNRTH administrators who had served in their positions for a minimum of three years. The participants in the focus group discussions were undergraduate medical students (MBChB) of MakCHS in their fourth and fifth year on clinical placement at the workplace.
The choice of various stakeholders as participants and varied methods of data collection was for purposes of triangulation to improve understanding, validate each other, verify viewpoints, and provide corroboration, hence contributing to confirmability.16,17
Inclusions and Exclusion Criteria
All administrators, heads of departments and lecturers at MakCHS and MNRTH, from the level of assistant lecturer to professor, and specialist doctors from the level of Medical Officer Special Grade (MOSG) also referred to as registrar to senior consultants involved in teaching undergraduates, were eligible to participate (Figure 1). Altogether, there were 187 specialist doctors, inclusive of the 10 heads of department.
Administrators from the other Schools in the College with no clinical placements for undergraduate medical student were excluded, ie, School of Public Health, School of Health Sciences, and School of Biomedical Sciences. Lecturers not involved in clinical teaching of undergraduate medical students at the workplace such as those in the laboratories and public health were excluded.
There were 258 undergraduate medical students: 130 in fourth year and 128 in fifth year who were eligible to participate. Out of these, 170 students completed the Dundee Ready Education Environment Measure (DREEM) questionnaire that was part of a quantitative preliminary study conducted to evaluate the students’ perceptions of the learning environment at MNRTH. The participants for the present study were drawn from respondents in the preliminary study, which gave them an opportunity to expound more about the responses they provided to the DREEM questionnaire. Undergraduate medical students in their fourth and fifth years of study who were not rotating in MNRH, ie, those rotating in Butabika Psychiatry hospital at the time of the study were excluded.
Data Collection Methods
Data from the administrators and lecturers were collected using Key Informant Interviews (KII) and from students using Focus Group Discussions (FGD). The data collection tools were developed by reviewing literature and from information collected in a preliminary study conducted to evaluate the students’ perceptions of the learning environment at MNRTH, using the Dundee Ready Education Environment Measure (DREEM).18
For the KII, an interview guide was designed with a list of topics and issues to be covered during each session. The guide contained questions on the lecturers’ and administrators’ perceptions of the workplace as a learning environment, its strengths and weaknesses, the curriculum requirements, their expectations of the students, and their perceived role and challenges in facilitating student learning. Each KII lasted approximately 45 minutes.
For the students, a focus group discussion guide was formulated from items that received the lowest scores on the DREEM questionnaire and additional questions were formulated as each focus group discussion progressed. The FGD guide included questions on matters such as preparations prior to clinical placement, learner expectations and if they were met, positive and negative learning experiences in the workplace, learning opportunities and challenges and use of spare moments in the workplace. Each FGD was comprised of 8–10 medical students and lasted from 45 minutes to 1 hour. The guides had open-ended questions and were pre-tested for clarity and to estimate the time required for administration.
The administrators and lecturers were selected purposively so as to get results that were information-rich by virtue of their knowledge and experience.19,20 A requirement for participation in the Key Informant Interviews was an experience in the position of at least three years for the administrators. This was guided by the knowledge that, in every culture, some individuals know much more than the average person, and it therefore becomes imperative to talk to those with more experience rather than randomly selecting individuals to participate.20 To minimise bias from the researchers, the students to participate in the focus group discussions were selected purposively by their leaders. The students were grouped according to year of study so that they could feel comfortable with each other as they provided insights into their perceptions of the workplace at MNRTH as a learning environment. It also motivated them to engage freely in the discussion and generate data based on synergy of group interaction.
The KII with the administrators and lecturers were conducted in their offices. The FGDs were conducted in one of the offices on campus to ensure both visual and auditory privacy. To ensure credibility of the findings, participation was voluntary, and participants were free to withdraw from the study at any time.21 The students were assured of confidentiality and encouraged to discuss freely as their identities were anonymised during the FGDs by referring to each other by letters (and not their names) that they were assigned at the beginning of each discussion. For the students to remain fully engaged in the discussion and minimise social desirability bias, the interviews were conducted by a research assistant who was not part of faculty.21 Permission was sought from all participants to record the interviews using an audio recorder and there were no objections. All the audio recordings and transcripts were stored as password-protected files on a password-protected computer. All participants provided informed consent, including permission for publication of anonymized responses.
Data Analysis
The framework method was used to perform thematic data analysis using ATLAS.ti software.22,23 Using an inductive approach, codes were developed from five transcripts as an initial step in the data analysis process. This was done by the author and one research assistant working separately. The two then met to discuss the codes and develop a codebook which was used to code the rest of the transcripts collaboratively and in real time. Quotes that were not fitting within the codebook were classified as “others” and used to generate additional codes. The codes formed the themes and subthemes used to describe the perceptions of the administrators, lecturers, and students about the workplace at MNRTH as a learning environment.
Results
Altogether, 36 students participated in focus group discussions. Groups of 8–10 students in their fourth and fifth year were constituted for the focused discussions and four FGDs were conducted: two from each of the fourth- and fifth-year classes (Table 1).
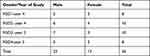 |
Table 1 Focus Group Discussion Participant Demographics |
Altogether, eight administrators, 10 heads of department and six clinicians from the different clinical departments participated in the study. The target for administrators and lecturers was 30 participants. Saturation was, however, attained at 24 participants, when interviews elicited no additional new information and recruitment for further interviews was discontinued.
There were mixed perceptions from the participants about the workplace at MNRTH as a learning environment with some describing it as enabling while others noted that there were many challenges at the workplace that needed to be addressed for effective learning. The themes that emerged included clinical cases, challenges at work, and planning priorities, as shown in Table 2.
 |
Table 2 Themes and Subthemes from the Data Collected |
Clinical Cases
Clinical cases (patients) at the workplace are a critical resource in the learning process which is comparable to none when learners participate in managing patients with their teachers in a real clinical context.24 During encounters with patients, students are exposed to real-life experiences that are similar to situations they are likely to encounter when they qualify, thus preparing them for clinical practice.
Patient Numbers and Case Mix
A large number of clinical cases (patients with a variety of pathologies - case-mix) at the workplace provide authentic learning opportunities for students to support clinical competence development. The workplace at MNRTH was perceived to be well endowed with adequate patient numbers and a suitable case mix.
It is a national referral hospital, and this provides a wide range of patients, cases nearly in all disciplines are referred from all the regions of the country so, clinically, that is very good, because the students end up getting exposed to nearly all the cases. Administrator, MakCHS.
About the working environment here, am very positive about it, there is opportunity to learn, because in Mulago, which is a national referral hospital, we get all kinds of patients and conditions, so there is a very big opportunity to learn. Student FGD, 4th year.
Access to Patients
There was no undue restriction of access to patients by the students at the workplace and this ensured that students could observe their clinical lecturers in action as they cared for the patients. Students also got opportunities to participate in patient care to the extent that their experience could allow.
The patients do not mind the students, they actually like the students because they are very close to them and they think that they can be their means to the ultimate ((the best care)), so they do not have a problem. Administrator, MNRTH.
For Mulago, as a teaching hospital, the patients are there with all sorts of diseases, so we get the exposure, which is a bonus, and they want you to attend to them so you can never say you don’t have a patient. They are always there; they are always wanting someone to listen to them. Student FGD, 5th year.
Challenges at the Workplace
Learning at the workplace is frequently undermined by challenges such as inadequate infrastructure, equipment and supplies, time pressure due to competing demands, large numbers of students and patients, and concerns about patient safety.
Infrastructure, Equipment, and Supplies
While patient numbers and case mix provided opportunities for learning to students, equipment and supplies such as gloves, aprons, oxygen, anaesthetic drugs, etc. were inadequate, and this affected learning, as students missed opportunities for practice.
The general impression is that the learning environment is excellent in terms of availability of patients, but it provides so many challenges which can sometimes be frustrating for both the teachers and the students. If a student is to learn how to perform a procedure by assisting in surgery, they are relegated to just watching because of unavailability of, for example sterile gowns. Lecturer, Surgery.
But as much as there are many patients, the resources are limited, you find that sometimes like in labour suite on some nights, we were just spectators and did not participate in delivering babies because there were not enough gloves and aprons. Student FGD, 5th year.
Learning at the workplace was also compromised by the large number of students and inadequate infrastructure in terms of space and other facilities.
Teaching sessions on the ward can be overwhelming, because of the large number of students that we have to interface with. You know about six junior clerks, about six senior clerks, then about six postgraduate students, visiting students from wherever, so you end up being one lecturer who literally needs a microphone on the ward. Lecturer, Paediatrics and Child health.
The ward is actually a good platform for our learning because we learn with patients but there has been an increase in numbers of students over time and yet the space is the same. So, it gets to a point where you find maybe 30 students have come to learn and they all cannot fit around that small bed, and here we are considering only medical students but there are all sorts of people; nurses, SHOs, international students, eh. Student FGD, 5th year.
Limited access to Information and Communication Technology (ICT) can hamper the lecturers’ and students’ ability to search recent literature as part of evidence-based care for patients which can also compromise the quality of the learning experience.
Students and staff should be able to access to facilities such as internet wherever they are because even in theater you may want to refer or make some consultations, they can even take a picture and share with someone, so there is greater need to actually have wireless everywhere. So, internet should not be our limiting factor but currently it is. Lecturer, Obstetrics & Gynaecology.
Other facilities required for training include online libraries, computers, internet, etc., but there is a time when there was no wireless internet for so long. I mean in this day and age for PBL students? I couldn’t believe it. I mean, where do you expect the teachers and learners to get internet access from. Lecturer, Paediatrics & Child health.
Resource challenges notwithstanding, the alternative perception was that occasional shortages of equipment and supplies at the workplace and learning environment may present as a reality check for students.
This learning environment is in the context of the country, we have resource challenges, we have human resource challenges, we have budgetary challenges. So generally, it is in that context, things can be better, but we are in a resource-limited country. Lecturer, General Surgery.
The positive side about it is that it makes students more resilient and creative. Because they have trained in a difficult environment, it makes them more thoughtful and consider the resources much more carefully, compared to those who train from an environment where resources are just flowing and never stop to think about the need to conserve or to utilize resources carefully. Administrator, MakCHS.
Lecturer Availability for Bedside Teaching
Clinical lecturers provide engagement opportunities for students during bedside teaching. The practice of bedside teaching, however, appeared to be on the decline.
The bedside teaching, evening ward rounds, where people were taught in emergency wards, those ones are no longer taking place very well. They are not, because most of the lecturers are now engaged in private practice in order to survive, they are engaged in research, and they do not have time for the students. Administrator, MNRTH.
We have minimum contact time with the consultants, yet we need them to facilitate us. You find that in a week during ward rounds, you meet them once or twice and sometimes they don’t show up at all, or when they show up, the atmosphere is very tense then it’s hard to ask them questions. Student FGD, 5th year.
Planning Priorities
Resources for Patient Care and Student Learning
The resource challenge appeared even more pronounced in the context of two autonomous institutions MNRTH and MakCHS responsible for ensuring that work and learning takes place. While the two institutions share common goals, namely teaching, research and patient care, their planning priorities may differ.
In planning for the resources that go into teaching at the Hospital, the University has always been clear or, at least, MakCHS has always been clear that we cannot plan for resources used in a different facility. Mulago is a teaching hospital, it is known as a teaching hospital, so the hospital should plan with the idea of the teaching component in mind. Administrator, MakCHS.
The Hospital budgets for itself and does not budget for the students, so the undergraduates and other students are a priority of the University. Unfortunately, the University that is supposed to be budgeting and giving those resources for teaching does not appear to budget. Administrator, MNRTH.
These divergent perceptions seemed to suggest that a middle ground was unattainable based on this analogy from one key informant:
Therefore, it is like two neighbours co-existing, and when I come to your home, I eat what I find and when you come to my home, you eat what you find, but that does not mean that your home budgets for my coming and even plans for me. You should plan for yourself as I also plan for myself, but in case I visit you, we can share and so that is exactly the problem. Administrator, MNRTH.
Nevertheless, there were voices of moderation too, which proposed that the two institutions should exploit each other’s strengths for mutual benefit.
The college can say, we can provide counsellors and the patients can be counselled because they really need the counselling. You get what I mean, and you know it helps that we are pooling resources. Administrator, MNRTH.
The equipment sometimes is not there, if you know that the training of medical students requires a particular equipment and Mulago cannot put it there, is it possible for Makerere to provide that equipment, such that Makerere and Mulago work out a custody agreement? Administrator, MakCHS.
Discussion
The workplace at MakCHS was perceived to be well endowed with adequate patient numbers and a wide case mix as well as unrestricted access to patients which allowed students to get adequate exposure to most common clinical situations and gave them more opportunities to observe a variety of pathologies, and to learn from their workplace experiences.25 Students observed their lecturers during patient encounters, listened to them verbalising their thoughts, a process known as “thinking aloud” which enabled the students to learn beyond what was being formally taught and enhanced their clinical reasoning process.26,27 During the patient encounter at the bedside, the lecturer should play the dual role of diagnosing the patient based on the clinical findings presented by the student, as well as diagnosing the student’s competence level based on expressed knowledge, observed interpersonal and communication skills, physical examinations and clinical decision-making skills exhibited.28 These skills acquired during learning at the workplace can then easily be applied in clinical practice in future by the graduates when they eventually qualify.24 “Active structured participation by students in day-to-day clinical activities is the key to learning in context”.3 For successful competence development, students should be afforded opportunities, as willing participants to work with patients as they learn. This approach provides for the gradual integration of students as they immerse themselves into the medical ecosystem and its culture, language, and values in an authentic fashion as they transition from the student identity to that of a practicing clinician.15
The physical infrastructure, equipment and supplies at the workplace can have a profound impact on the quality of care provided to patients as well as the quality of learning experienced by students at the workplace.29,30 The administrators, lecturers and learners perceived the workplace as having inadequate infrastructure, equipment and supplies to facilitate learning. Infrastructure, equipment and supplies are very important resources as they form part of the ecology of medical education.31 An environment fraught with shortages can be quite uncomfortable and pose a big challenge to clinical teaching.32
In a study to evaluate trainer perception about the workplace as a learning environment in Ethiopia, lack of infrastructure and equipment was found to be one of the emergent themes.2,33 Often, because of frequent shortages, lecturers become creative and devise alternatives, which can be good in the short term, but when this becomes routine practice, it compromises quality and sometimes promotes the hidden curriculum.34 The occasional shortages of equipment and supplies during learning at the workplace could, however, be considered a reality check because students who have encountered such adverse environments during training become more resilient and creative with positive adaptations to their context and become doctors fit for purpose.35 After all, such situations may be similar to what they will encounter when they qualify.
In contemporary medicine, successful learning at the workplace requires additional resources, such as online libraries and facilities for ICT. This was perceived as inadequate at the workplace. The ability to consult while learning and offering health care at the workplace enhances the students’ learning experience. It adds value to the quality of education while on the move and provides an excellent opportunity to keep up-to-date with the ever-increasing evidence base, thus improving the quality of care provided to patients through correct drug dosage calculations and information sharing.36–40
While the workplace at MNRTH was considered to have enough clinical lecturers, the overall perception was that there were missed opportunities for learning because lecturers were not fully available at the clinical areas to facilitate bedside teaching. This was attributed to competing demands for their time, such as private practice for economic survival and research, thus making it difficult to avail themselves for bedside teaching. Unfortunately, this situation created negative role models for the learners, which can impact on their behaviour when they qualify. The reported decline in the use of the bedside for learning important clinical skills for medical students has been reported elsewhere.32,41 Based on the one-minute preceptorship model, learning at the workplace should be such that every patient encounter is a learning opportunity.3 This can only be possible when the lecturers are available, competent, and willing to teach, with adequate protected time and space, as well as students with the right experience, backgrounds and interest.6
The workplace that was explored, comprised of two major stakeholders; MNRTH and MakCHS, whose situation presented both opportunities and threats to the learning environment.42 The two institutions have autonomous organisational and management structures, although they share common goals of teaching, research and patient care. In such a relationship, an imbalance may exist between the influence and interests of the different stakeholders.43 While it is in the interest of MakCHS to have the workplace offer the best learning experience possible to the medical students, MakCHS may have little influence over the way priorities are set by MNRTH, in terms of procurement of equipment and supplies for patient care and by extension, student learning. This was compounded by varied expectations from the stakeholders where each viewed the other as not doing enough to facilitate teaching and learning at the workplace. This was highlighted by the diametrically opposing views from the Key Informants about who was responsible for procurement of resources for students learning at the workplace. The antagonism may have little to do with roles and responsibilities for teaching and learning but more with resource mobilisation, allocation and utilisation.44 The different supervising ministries: Ministry of Health for MNRTH and Ministry of Education for MakCHS may complicate the situation due to insufficient coordination in terms of budgets, priorities and expected outcomes as is the case in most African countries.30 In order for institutions with such an intricate relationship to flourish, the different stakeholders need to engage constructively through constant communication so as to collectively drive the community’s agenda with more synergism than antagonism as they share their successes and challenges with each other in a quest for constant renewal and survival.30,45,46
A supportive learning environment should have protected spaces, so that the lecturer and the students can discuss the theoretical concepts underlying the patient’s condition in more detail. This is best done away from the patient’s bedside so as to discuss freely, those clinical aspects that do not require patient’s presence and to raise sensitive issues related to a patient’s illnesses such as differential diagnoses (handling the “what if” questions), treatment options and prognosis.32 Patients who participate in the teaching sessions need to be assured of privacy and confidentiality and this can only become reality when the workplace is equipped with facilities such as patient screens to ensure privacy and ward side-rooms for student debriefing. The workplace at MNRTH had large numbers of patients and students leading to situations of profound overcrowding which compromised patient privacy and confidentiality. There was also a shortage of designated protected spaces for teaching and learning.
Study Limitations
The participants in key informant interviews and focus group discussions passionately shared their experiences and perceptions about the workplace and a lot of information was generated. However, not all the responses could be shared as quotes in the results, although representative quotes were used, as far as possible.
The principal investigator being part of faculty at the study site may have created some degree of expected-response bias, especially among the student participants but this was mitigated by the anonymity created by the use of letters and number for referring to the participants, and collection of data for the FGDs by a research assistant who was not part of faculty.
Conclusion
The key stakeholders expressed mixed perceptions about the learning environment at MakCHS with both enabling and challenging factors that needed to be addressed in order for an optimal learning experience. The large patient numbers, wide case-mix and unrestricted access to patients afforded students the opportunity to observe their lecturers in action while they attended to the variety of cases. The students also had opportunities to practise taking care of the patients with increasing responsibility according to their level of experience under supervision.
The challenges of shortage of equipment and supplies, infrastructural inadequacies and an ever-increasing number of students hampered the available students practice opportunities at the workplace. This was compounded by the ambiguity of the organisational setup at the workplace, regarding the roles and responsibilities of the university and the hospital in planning for the resources required for undergraduate teaching and learning. Each entity perceived the other as not doing enough to facilitate the workplace as a learning environment.
The chronic inadequacies could impact negatively on the students’ choice of career when they graduate, as they may see no satisfaction in clinical medicine under the prevailing conditions.
Data Sharing Statement
All data regarding this manuscript are available from the corresponding author.
Ethical Approval, Consent to Participate and Publication
Before commencing with data collection, permission was obtained from the ethical committees of MakCHS (REC REF No. 2015-125), MNRTH (MREC 868), the Uganda National Council for Science and Technology (SS 3935), and the University of the Free State (ECUFS NR 174/2015). Permission was sought to record the interviews using an audio recorder and there were no objections from the study participants. Participation in the study was voluntary and participants were free to withdraw from the study at any time. Anonymity and confidentiality of the study participants and data sets was ensured by using numbers and letters to refer to the participants in the focus group discussions and the key-informant interviews, while the audio recordings and transcripts were assigned letters and numbers for electronic storage. Audio recordings and transcripts were stored as password-protected files on a password-protected laptop belonging to the principal investigator. All participants provided informed consent, including permission for publication of anonymized responses.
Consent for Publication
All authors consent to be a part of this publication by taking full responsibility and accountability for the contents of the article. All the work, figures and tables in this publication were prepared by the authors and where other work is used, it has been appropriately cited.
Acknowledgment
I would like to acknowledge the lecturers, administrators and students who agreed to participate in the study, and the research assistants who assisted with data collection. I would also like to acknowledge NURTURE Project of Makerere University College of Health Sciences for the funding support during the course of this work, from conceptualisation, data collection, analysis and manuscript writing; Nurture Fellowship Grant Number D43TW010132 supported by Office Of The Director National Institutes Of Health (OD), National Institute Of Dental & Craniofacial Research (NIDCR), National Institute Of Neurological Disorders And Stroke (NINDS), National Heart, Lung, And Blood Institute (NHLBI), Fogarty International Center (FIC), National Institute On Minority Health And Health Disparities (NIMHD).
Author Contributions
All authors: MNK, SK, HS & MPJ, made a significant contribution to the work reported, that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, and also took part in drafting, revising and critically reviewing the article. They gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Dijkstra IS, Pols J, Remmelts P, Rietzschel EF, Cohen-Schotanus J, Brand PL. How educational innovations and attention to competencies in postgraduate medical education relate to preparedness for practice: the key role of the learning environment. Perspect Med Educ. 2015;4(6):300–307. doi:10.1007/s40037-015-0219-3
2. Kibwana S, Haws R, Kols A, et al. Trainers’ perception of the learning environment and student competency: a qualitative investigation of midwifery and anesthesia training programs in Ethiopia. Nurse Educ Today. 2017;55:5–10. doi:10.1016/j.nedt.2017.04.021
3. Sajjad M, Mahboob U. Improving workplace-based learning for undergraduate medical students. Pak J Med Sci. 2015;31(5):1272–1274. doi:10.12669/pjms.315.7687
4. Salam A, Siraj HH, Mohamad N, Das S, Rabeya Y. Bedside teaching in undergraduate medical education: issues, strategies, and new models for better preparation of new generation doctors. Iran J Med Sci. 2011;36(1):1–6.
5. Dornan T, Muijtjens A, Graham J, Scherpbier A, Boshuizen H. Manchester Clinical Placement Index (MCPI). conditions for medical students’ learning in hospital and community placements. Adv Health Sci Educ. 2012;17(5):703–716. doi:10.1007/s10459-011-9344-x
6. Chen HC, ten Cate O, O’Sullivan P, et al. Students’ goal orientations, perceptions of early clinical experiences and learning outcomes. Med Educ. 2016;50(2):203–213. doi:10.1111/medu.12885
7. Norcini JJ, McKinley DW. Assessment methods in medical education. Teach Teach Educ. 2007;23(3):239–250. doi:10.1016/j.tate.2006.12.021
8. Ramani S, Leinster S. AMEE guide no. 34: teaching in the clinical environment. Med Teach. 2008;30(4):347–364. doi:10.1080/01421590802061613
9. Cohen J, Ezer T. Human rights in patient care: a theoretical and practical framework. Health Hum Rights. 2013;15(2):7–19.
10. Parniyan R, Pishgar Z, Rahmanian S, Zahra S. A comparison between awareness and observance of patients’ rights charter from the perspectives of the personnel, students, and patients in the operating rooms of the University Hospitals of Jahrom. Glob J Health Sci. 2016;8(12):36–44. doi:10.5539/gjhs.v8n12p36
11. Corrigan MJ, Eden J. Leadership by example: IOM report calls for U.S. to become more visible in quality arena. Qual Lett Healthc Lead. 2002;14(12):11–12.
12. Weinberger S. The medical educator in the 21st century: a personal perspective. Trans Am Clin Climatol Assoc. 2009;120:239–248.
13. Frenk J, Chen L, Bhutta ZA, et al. Health professionals for a new century: transforming education to strengthen health systems in an interdependent world. Lancet. 2010;376(9756):1923–1958. doi:10.1016/S0140-6736(10)61854-5
14. Gonzalo JD, Thompson BM, Haidet P, Mann K, Wolpaw DR. A Constructive reframing of student roles and systems learning in medical education using a communities of practice lens. Acad Med. 2017;92(12):1687–1694. doi:10.1097/ACM.0000000000001778
15. Köhl-Hackert N, Krautter M, Andreesen S, et al. Workplace learning: an analysis of students’ expectations of learning on the ward in the Department of Internal Medicine. GMS Z Med Ausbild. 2014;31(4):Doc43. doi:10.3205/zma000935
16. Johnson RB, Onwuegbuzie AJ, Turner LA. Toward a definition of mixed methods research. J Mix Methods Res. 2007;1(2):112–133. doi:10.1177/1558689806298224
17. Moran-Ellis J, Alexander VD, Cronin A, et al. Triangulation and integration: processes, claims and implications. Qual Res. 2006;6(1):45–59. doi:10.1177/1468794106058870
18. Koohpayehzadeh J, Hashemi A, Soltani Arabshahi K, et al. Assessing validity and reliability of Dundee ready educational environment measure (DREEM) in Iran. Med J Islam Repub Iran. 2014;28:60.
19. Palinkas LA, Horwitz SM, Green CA, Wisdom JP, Duan N, Hoagwood K. Purposeful sampling for qualitative data collection and analysis in mixed method implementation research. Adm Policy Ment Health. 2015;42(5):533–544. doi:10.1007/s10488-013-0528-y
20. Tongco MDC. Purposive sampling as a tool for informant selection. Ethnobot Res Appl. 2007;5:12.
21. Krefting L. Rigor in qualitative research: the assessment of trustworthiness. Am J Occup Ther. 1991;45(3):214–222. doi:10.5014/ajot.45.3.214
22. Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol. 2013;13(1):117. doi:10.1186/1471-2288-13-117
23. Woods M, Paulus T, Atkins DP, Macklin R. Advancing qualitative research Using Qualitative Data Analysis Software (QDAS)? Reviewing potential versus practice in published studies using ATLAS.ti and NVivo, 1994–2013. Soc Sci Comput Rev. 2016;34(5):597–617. doi:10.1177/0894439315596311
24. Nordquist J, Hall J, Caverzagie K, et al. The clinical learning environment. Med Teach. 2019;41(4):366–372. doi:10.1080/0142159X.2019.1566601
25. Duvivier R, Stalmeijer R, Van Dalen J, Van Der Vleuten C, Scherpbier A. Influence of the workplace on learning physical examination skills. BMC Med Educ. 2014;14(1):61. doi:10.1186/1472-6920-14-61
26. Chen HC, Teherani A. Workplace affordances to increase learner engagement in the clinical workplace. Med Educ. 2015;49(12):1184–1186. doi:10.1111/medu.12888
27. Morris C. Facilitating learning in the workplace. Br J Hosp Med. 2010;71(1):48–50. doi:10.12968/hmed.2010.71.1.45974
28. Nilsson MS, Pennbrant S, Pilhammar E, Wenestam C-G. Pedagogical strategies used in clinical medical education: an observational study. BMC Med Educ. 2010;10(1):9. doi:10.1186/1472-6920-10-9
29. Leslie HH, Sun Z, Kruk ME. Association between infrastructure and observed quality of care in 4 healthcare services: a cross-sectional study of 4300 facilities in 8 countries. PLoS Med. 2017;14(12):e1002464. doi:10.1371/journal.pmed.1002464
30. Tsinuel G, Tsedeke A, Matthias S, et al. Establishing medical schools in limited resource settings. Ethiop J Health Sci. 2016;26(3):277–284. doi:10.4314/ejhs.v26i3.10
31. Ringsted C, Hodges B, Scherpbier A. ‘The research compass’: an introduction to research in medical education: AMEE guide no. 56. Med Teach. 2011;33(9):695–709. doi:10.3109/0142159X.2011.595436
32. Gat I, Pessach-Gelblum L, Givati G, et al. Innovative integrative bedside teaching model improves tutors’ self-assessments of teaching skills and attitudes. Med Educ Online. 2016;21(1):30526. doi:10.3402/meo.v21.30526
33. Ranson MK, Chopra M, Atkins S, Dal Poz MR, Bennett S. Priorities for research into human resources for health in low- and middle-income countries. Bull World Health Organ. 2010;88(6):435–443. doi:10.2471/BLT.09.066290
34. Altirkawi K. Teaching professionalism in medicine: what, why and how? Sudan J Paediatr. 2014;14(1):31–38.
35. Matheson C, Robertson HD, Elliott AM, Iversen L, Murchie P. Resilience of primary healthcare professionals working in challenging environments: a focus group study. Br J Gen Pract. 2016;66(648):e507. doi:10.3399/bjgp16X685285
36. Chun M. A study on college students’ use intention of internet learning resources in Chongqing. Asian Soc Sci. 2014;10(3). doi:10.5539/ass.v10n3p70
37. Koehler N, Vujovic O, McMenamin C. Healthcare professionals’ use of mobile phones and the internet in clinical practice. J Mob Technol Med. 2013;2(1). doi:10.7309/jmtm.2.1.2
38. Majid S, Foo S, Luyt B, et al. Adopting evidence-based practice in clinical decision making: nurses’ perceptions, knowledge, and barriers. J Med Libr Assoc. 2011;99(3):229–236. doi:10.3163/1536-5050.99.3.010
39. Rouleau G, Gagnon M-P, Côté J. Impacts of information and communication technologies on nursing care: an overview of systematic reviews (protocol). Syst Rev. 2015;4(1):75. doi:10.1186/s13643-015-0062-y
40. Twiss-Brooks AB, Andrade R
41. Peters M, Ten Cate O. Bedside teaching in medical education: a literature review. Perspect Med Educ. 2014;3(2):76–88. doi:10.1007/s40037-013-0083-y
42. Chapleo C, Simms C. Stakeholder analysis in higher education. Perspect Policy Pract High Educ. 2010;14(1):12–20.
43. Smith LW. Stakeholder Analysis: a Pivotal Practice of Successful Projects.
44. Mubuuke AG, Businge F, Mukule E. The intricate relationship between a medical school and a teaching hospital: a case study in Uganda. Educ Health. 2014;27(3):249–254. doi:10.4103/1357-6283.152183
45. Cruess RL, Cruess SR, Steinert Y. Medicine as a community of practice: implications for medical education. Acad Med. 2018;93(2):185–191. doi:10.1097/ACM.0000000000001826
46. Shehnaz SI, Arifulla M, Sreedharan J, Gomathi KG. What do faculty feel about teaching in this school? Assessment of medical education environment by teachers. Educ Health. 2017;30(1):68–74. doi:10.4103/1357-6283.210500
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
