Back to Journals » Patient Preference and Adherence » Volume 17
Perception and Attitude of Lebanese IBD Patients During the COVID-19 Pandemic
Authors Mikhael E, Khalife Y, Yaghi C , Khoury B, Khazaka S, Khoueiry C, Safar K, Sayegh RB, Honein K, Slim R
Received 30 May 2023
Accepted for publication 5 August 2023
Published 15 August 2023 Volume 2023:17 Pages 1967—1975
DOI https://doi.org/10.2147/PPA.S423520
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Elio Mikhael, Yaacoub Khalife, Cesar Yaghi, Bernard Khoury, Stephanie Khazaka, Christèle Khoueiry, Karl Safar, Raymond B Sayegh, Khalil Honein, Rita Slim
Department of Gastro-Enterology and Hepatology, Saint-Joseph University, Beirut, Lebanon
Correspondence: Rita Slim, Department of Gastro-Enterology and Hepatology, Saint-Joseph University, Beirut, Lebanon, Email [email protected]
Objective: The emergence of the COVID pandemic affected daily living and healthcare access of IBD patients, due to delays of elective procedures and in-hospital treatments. Our aim is to determine the repercussions of the pandemic on the daily habits of IBD patients and on their compliance to follow-up and treatment.
Methods: This was a cross-sectional observational study. A questionnaire was administered in between 2020 and 2022 to IBD patients in a tertiary center in Lebanon. The outcomes measured were patient perceptions regarding COVID and how it affected their treatment.
Results: A total of 201 answers were included in the analysis with male predominance. Two-thirds had Crohn’s disease. Near 80% were afraid of being infected by COVID-19 and 87.6% were afraid of physical contact. 91.5% reduced their daily habits and 96.0% have used personal protective equipment. 47.3% of the patients report that there are factors that reduced their worries, the most common factor being contacting their physician (61.0%). The main source of information was the treating physician (37.8%). A quarter of patients think that their condition predisposed to COVID-19 infection and about two-thirds believe that immunosuppressive therapy did so. The same amount reported concern regarding visiting the hospital. 27.4% preferred telemedicine and 44.8% preferred over-The-phone consultation to an in-person visit. Three-quarters were in favor of vaccination. 59.6% delayed their in-center treatment, which was associated with a reduction in daily life activities. 13.9% wanted to discontinue their treatment, which was associated with smoking, cardiovascular, and rheumatological comorbidities, but only 4% did so.
Conclusion: The pandemic had significant repercussions on the everyday life of IBD patients, with some preferring to consult via telemedicine and others considering stopping their treatment.
Keywords: inflammatory bowel disease, COVID-19, patient–provider relationship, patient adherence
Plain Language Summary
What is already known on this topic – IBD patients perceive themselves as being more at risk of being affected by COVID-19, and they may subsequently stop or delay their treatment.
What this study adds – This study confirms the aforementioned findings in a Lebanese population and establishes a profile of patients that are more at risk of stopping or delaying their treatment. This includes smokers and patients with known cardiovascular risk factors.
How this study might affect research, practice, or policy – IBD patients should be counselled on the importance of seeking out proper information from their physician or recognized societies and on the importance of taking their treatment. Particular attention should be made on smokers and patients with cardiovascular risk factors or rheumatological comorbidities.
Introduction
The severe acute respiratory syndrome coronavirus 2 (SARS-Cov-2) was first described in 2019, in China.1 It was followed by a worldwide spread of the disease, which led the World Health Organization to call it a pandemic in March 2020.1 Hospital resources and personnel were shifted to fight the pandemic and elective procedures were deferred.2
Patients with inflammatory bowel disease (IBD) faced many challenges during the pandemic. First, stress is suggested to be correlated with Crohn’s disease activity.3 With high levels of stress and anxiety being noted during the pandemic,4 disease flares could be suspected in IBD patients. Second, immunosuppressive agents are used to treat IBD, which raises concern among patients for being more easily infected and at risk of more severe disease.5 This led international organizations to issue recommendations on the management of IBD patients during the pandemic.6–8 Third, some of these patients require frequent outpatient or hospital visits for injections or undergoing imaging or endoscopy, which were affected by the pandemic.9
The first case of SARS-Cov-2 in Lebanon was reported in February 2020.10 IBD patients in Lebanon also had to endure a severe economic crisis.10 Consequently, this affected their ability to buy medication, to visit their physician, or to buy into a health insurance policy. In addition, medication shortages have not spared IBD patients, with many having to skip doses.11
Several studies have evaluated their perceptions regarding the outbreak in different countries.5,12–20 In this paper, we aim to evaluate IBD patients' perceptions and behaviors regarding the SARS-Cov-2 pandemic for the first time in Lebanon.
Materials and Methods
This is a cross-sectional observational study conducted in Lebanon. This study was conducted after the approval of the ethics committee of the Saint-Joseph University of Beirut (code CEHDF1753) and was in accordance with the Declaration of Helsinki.
Patient Selection
Patient recruitment was done between 2020 and 2022 in a single institution in Lebanon from the database of IBD patients of a single institution in Lebanon. Inclusion criteria for this study comprised all adults with a confirmed IBD diagnosis without active or previous COVID-19 infection, and who agreed to fill questionnaire. Patients were contacted either by telephone or by face-to-face during their outpatient or inpatient visit and consent was obtained. Previous medical history and IBD related medical history were obtained from electronic medical records.
Questionnaire
The questionnaire in this study (Supplementary Material 1) was built mainly with a focus on patient behavior, attitude, and perception, in accordance with a questionnaire previously used in the EFCCA study, which was translated into different languages.5 Questions were added regarding the behavior and activity of the IBD, delay of in-patient treatment, the used source of information by the patient during the pandemic, and patient opinion towards telemedicine and the COVID-19 vaccine. It was divided into five domains: socio-demographic data and medical history of patients, fear of COVID-19, use of protection equipment, lifestyle modifications, and IBD-related information, compliance to treatment and follow-up. It was available in three languages (Arabic, French, and English). It was translated by an expert and required no prior validation before administration. The questionnaire was administered either by telephone or face-to-face by a trained investigator.
Statistical Analysis
All data were collected and coded for statistical analysis using the SPSS v25.0. Comparison between the different items was studied using the chi-square test and the Fisher t-test with a p-value considered significant when it was ≤0.05. A multivariate analysis was performed using a binary logistic regression, with a p-value considered significant when it was ≤0.05.
Results
A total of 226 patients were contacted, 19 of which were infected by COVID-19 and hence excluded, and 6 patients refused to answer the questionnaire. The analysis included 201 patients.
Sociodemographic Data and Disease Characteristics
The average age of the studied population is 43 years old (± 16 years) out of which 110 are male (54.7%). Most responders are married (n = 125, 62.2%), employed (n = 130, 64.7%) and have a university degree (n = 130, 64.7%). More than half of the population are smokers.
In this population, 132 responders (65.5%) had Crohn’s disease and 69 (34.5%) had ulcerative colitis. In patients with Crohn’s disease, 83 (62.9%) had moderate-to-severe disease compared to 31 (44.9%) ulcerative colitis patients. The most common treatments used were biologics (n = 111, 55.2%). Table 1 represents patient and disease characteristics of the responders.
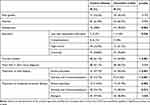 |
Table 1 Characteristics of the Studied Population |
In this population, 116 patients (57.7%) had other comorbidities: cardiovascular risk factors were the most common with 60 patients, followed by cardiac disease (18 patients), rheumatologic disease (9 patients), kidney disease, hepatic disease, and malignancy (6 patients) and finally pulmonary conditions (2 patients).
Perception Regarding the SARS-Cov-2 Outbreak
In the second part of the questionnaire, patients answered questions regarding their perception of the COVID-19 outbreak. The answers are summarized in Table 2.
 |
Table 2 Perception Regarding the COVID-19 Outbreak |
In total, 49 patients (24.4%) think that their condition predisposes to COVID-19 infection and 129 patients (64.2%) believe that immunosuppressive therapy predisposes to this infection. In addition, 53 (26.4%) patients and 37 (18.4%) patients responded with “I don’t know” respectively, for each question. The same amount reported concern regarding visiting the hospital (n = 129, 64.2%). Fifty-five patients (27.4%) preferred telemedicine and 90 patients (44.8%) preferred over-The-phone consultation to an in-person visit to their doctor’s office.
During this period, 112 patients (55.7%) contacted their physician of which 93 (83%) contacted their gastroenterologist. Of those, 112 patients, 105 (93.6%) received recommendations and information, and they were all satisfied except for one patient. However, 47 patients (42.0%) reported that they needed more information. Finally, 152 (75.6%) of the responders were in favor of vaccination.
Treatment Delay, Desire of Treatment Discontinuation and Treatment Discontinuation
Patients were asked whether they delayed their in-center treatment, if they desired to stop their treatment, or if they discontinued their treatment on their own. A univariate analysis (Supplementary Material 2) was performed regarding risk factors of these attitudes, followed by a multivariate analysis (Table 3).
 |
Table 3 Univariate and Multivariate Analysis of Delay of in-Center Treatment and Desire to Stop Treatment |
Among the 110 patients requiring intravenous injections, 65 patients (59.6%) delayed their in-hospital treatment because of COVID-19. Fear of having contact with other people is associated with a higher risk of desire to delay in-center IBD treatment in a univariate analysis. In addition, the reduction of daily habits was associated with in-center IBD treatment delay in a multivariate and in a univariate analysis, whereas the use of gloves and the use of disinfectants were associated with fewer delays.
In this population, 28 (13.9%) wanted to discontinue their treatment. In both univariate and multivariate analysis, cardiovascular risk factors and rheumatological comorbidities were associated with a higher desire to stop the treatment. Smoking is associated with a higher desire to stop the treatment in a multivariate analysis of the whole population, but not in a univariate analysis. In a univariate analysis of patients with mild disease, having a degree lower than a high school degree and the presence of malignancies is associated with a higher desire to stop the medications. A univariate analysis of patients with moderate-to-severe disease seeking reassurance through a psychologist and being unemployed is associated with a higher desire to stop medications.
A total of 8 patients (4.0%) stopped their treatment with their own initiative because of worry (3 patients were on immunomodulators, 3 patients were on anti-TNF agents and 1 patient was taking amino salicylates). While rheumatological comorbidities were associated with treatment discontinuation in a univariate analysis, no factors reached statistical significance in a multivariate analysis.
Discussion
In this study, we evaluated 201 IBD patients’ perceptions and actions with regard to the SARS-Cov-2 outbreak. Most patients’ everyday life have been impacted due to the pandemic. First, as D’Amico et al have already reported, most responders were afraid of getting infected, infecting other people, or having a physical contact with another person.5 In addition, almost 90% of patients went less frequently to public spaces, the majority was worried about traveling, and more than 80% reduced their travels.5 When compared to our population, the numbers are similar except for the fear of traveling. One could argue that the rate of patients that reduced their travels could be overestimated in our population given the probable presence of a severe financial crisis.21 Furthermore, one could also argue that the rate of reduction of daily habits can be overestimated given that the purchasing power of the average Lebanese has taken a hit.21
When comparing our population to the general Lebanese population, adherence to personal protective equipment (PPE) is higher in IBD patients (96% IBD patients wore masks regularly vs 79.3%).22 Multiple studies have reported on the use of PPE in IBD populations. High rates of adherence to PPE are seen across most studies.5,13,17,23 This is in line with the increased worry of IBD patients with regard to being infected or having a physical contact with others. These numbers should be taken with caution since these studies were done in different times, and recommendations for the use of PPE varied throughout the pandemic. Finally, almost three-quarters of our responders were in favor of vaccination, in line with other IBD populations.24,25 This is slightly superior to the Lebanese general population, where only 63% were in favor.26
In our study, the importance of the relation between the patient and his physician is highlighted in two ways: the physician as a relieving factor and as a source of information. Unlike European populations, in Lebanon contacting physicians was the most common relieving factor, whereas it was the fifth most common in the EFCCA study.5 This may be due to the relative easiness to contact the physician in Lebanon. Most patients possess the private phone number of their physician and can either contact them directly or via text messaging. In addition, friends and families were the second most common relieving factor in Lebanon, with half of the responders mentioning them, whereas only 34% of the EFCCA study responders did so.5 Lebanese are known for their proximity to their respective families and the moral support they provide.
In addition, the treating physician was the main source of information in our population and in the general Lebanese population.22 This has not been the case in other studies. In fact, social media platforms, television, and public health organization were cited as the main source of information.12,13,18,23 This is also a consequence of the ease of access to treating physicians in Lebanon, with specialized care being readily available. Furthermore, these numbers highlight the trust that patients have in their gastroenterologist and the importance of that relationship, as it is the main source of relief and information. Patient–physician relationship in IBD has been studied in the past.27,28 Karimi et al reported that there are still a lack of studies that evaluate the impact of a positive or negative patient–physician relationship on outcomes in IBD.28 Nevertheless, trust in the provider appears to be an important issue for IBD patients.27 This seems to be the case in Lebanese IBD patients to a greater degree.
Unfortunately, there is a downside to this tight patient–physician relationship in Lebanon. During the past few years, there has been an exodus of Lebanese physicians due to the deteriorating economy.29 As a result, IBD patients are losing a pillar upon which they used to rely for psychological relief and medical information. Amid this crisis, a new solution must be sought. Interestingly, while patient associations represent nearly half of the relieving factors in European IBD populations,5 only one patient mentioned them in our study. That is because patients ignore the presence of such associations in Lebanon (I Battle Disease). Patient associations are important as they can increase patient knowledge and improve quality of life.30 This is an area that needs to improve as they can help patients during these times to provide a safe zone in which trust can be built and easily accessible information.
In terms of perception, our population seems to think less that IBD predisposes to COVID-19 infection (24.4% vs 30–87% found in the literature).5,13,14,17,20,31 On the other hand, our population tends to think more that their immunosuppressive therapy predisposes to this infection (64.2% vs 25–48% in the literature).5,12,13,20,23,31 In our survey, 13.9% of patients wanted to stop their medication but only 4% did so by their own initiative. Similar rates have been reported with less than 10% of self-discontinuation rate.12,13,18,32 In our population, 64.2% patients reported concern regarding hospital visits and 59.6% patients requiring in-hospital injections delayed their doses. Identical findings were reported in Europe.12,31,32 In other regions, almost 60% of patient hospital visits were affected.14,17 Despite the context of medication shortages in Lebanon, treatment stoppage or delay due to non-availability was not evaluated in our study.33 This was the reason why most patients missed their doses in India.13
In the setting of pandemic and subsequent lockdowns, telemedicine has emerged as a possible solution to ensure that patients receive the care they need despite the restrictions imposed.34 In our study, 27.4% of patients preferred telemedicine and 44.8% preferred over-the-phone consultation over in-person visits. Variable rates of telemedicine usage by IBD patients have been reported in the literature,15,17,20 but the perception is viewed as largely favorable.31,34 Telemedicine in Lebanon is only picking up with the majority of Lebanese physicians using it during the pandemic.35 However, only 9% of physicians used specialized applications for telemedicine, while the majority used regular phone calls, messengers, or emails.35 Therefore, efforts must be made to develop such platforms in Lebanon.
With the SARS-Cov-2 outbreak perhaps in the rear-view mirror, this is the moment to review our attitude towards the pandemic and to learn from our mistakes. One important aspect that needs to be addressed is the knowledge gap in our IBD patients. For instance, despite evidence that has shown that IBD medications are safe to take during the pandemic except for corticosteroids,6,7 some patients stopped or delayed their treatment. We established a profile of patients that are more likely to delay or stop their treatment. For instance, patients who have reduced their visits to public spaces are more likely to delay their in-center treatment, which is consistent with fear of contact with other persons. In addition, current smokers and patients with cardiovascular risk factors are more frequently associated with a desire to stop medication. This may be due to that they are associated with worse COVID-19 outcomes.36 Similarly, patients with rheumatologic comorbidities are also associated with a desire to stop treatment, which is in line with available reports of adherence to treatment in patients with rheumatic disease during the pandemic.37
We must ensure that our patients receive the right information, and we must specifically target patients with the profiles mentioned above. Patients should be able to easily access reliable information from reliable sources. If patient associations are frequented elsewhere in the world, in Lebanon it is still an unknown entity. Thus, patients should be encouraged to reach out to patient associations in Lebanon to learn about their condition in a general setting or during a pandemic. The knowledge gap does not concern the patients only. Further research is needed to determine which patients are more at risk of getting infected, which treatments need to be stopped, and how to manage IBD flares or complications in the setting of a pandemic. Finally, telemedicine is a very interesting aspect of healthcare that needs to be improved as it could be an important asset.
To our knowledge, this is the first study to evaluate the impact of COVID-19 on IBD patients in Lebanon. This study has many limits. First, there were no open-ended questions. This could have been a better tool to evaluate patient perception. Second, there are no validated questionnaires for IBD patients in COVID-19. We chose this questionnaire because our purpose was to evaluate patient behavior, attitudes, and perception during the pandemic. Disease activity was not evaluated in this study. Finally, the generalizability of our results is limited because this study was done in a single center in Lebanon.
Conclusion
The SARS-Cov-2 pandemic was a brutal one, and it had severe damages both in terms of death toll and financial implications. To prevent such huge losses in the future we must use what we have learned during this pandemic and improve the things we started developing. Patient and physician knowledge needs to be improved and telemedicine must be fine-tuned.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
No funding was necessary for this study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. World Health Organization. WHO director-general’s opening remarks at the media briefing on COVID-19. Available from: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-The-media-briefing-on-covid-19---11-march-2020.
2. Centers for Medicare and Medicaid Services. Non-emergent, elective medical services, and treatment recommendations; 2020. Available from: https://www.cms.gov/files/document/cms-non-emergent-elective-medical-recommendations.pdf.
3. Schoultz M, Beattie M, Gorely T, Leung J. Assessment of causal link between psychological factors and symptom exacerbation in inflammatory bowel disease: a systematic review utilising Bradford Hill criteria and meta-analysis of prospective cohort studies. Syst Rev. 2020;9(1):169. doi:10.1186/s13643-020-01426-2
4. Pfefferbaum B, North CS. Mental health and the covid-19 pandemic. N Engl J Med. 2020;383(6):510–512. doi:10.1056/NEJMp2008017
5. D’Amico F, Rahier JF, Leone S, Peyrin-Biroulet L, Danese S. Views of patients with inflammatory bowel disease on the COVID-19 pandemic: a global survey. Lancet Gastroenterol Hepatol. 2020;5(7):631–632. doi:10.1016/S2468-1253(20)30151-5
6. Rubin DT, Feuerstein JD, Wang AY, Cohen RD. AGA clinical practice update on management of inflammatory bowel disease during the COVID-19 pandemic: expert commentary. Gastroenterology. 2020;159(1):350–357. doi:10.1053/j.gastro.2020.04.012
7. Rubin DT, Abreu MT, Rai V, Siegel CA. International organization for the study of inflammatory bowel disease. management of patients with Crohn’s disease and ulcerative colitis during the coronavirus disease-2019 Pandemic: results of an international meeting. Gastroenterology. 2020;159(1):6–13.e6. doi:10.1053/j.gastro.2020.04.002
8. Kennedy NA, Jones GR, Lamb CA, et al. British Society of Gastroenterology guidance for management of inflammatory bowel disease during the COVID-19 pandemic. Gut. 2020;69(6):984–990. doi:10.1136/gutjnl-2020-321244
9. Ng SC, Mak JWY, Hitz L, Chowers Y, Bernstein CN, Silverberg MS. COVID-19 pandemic: which IBD patients need to be scoped—who gets scoped now, who can wait, and how to resume to normal. J Crohns Colitis. 2020;14(Supplement_3):S791–S797. doi:10.1093/ecco-jcc/jjaa128
10. Bizri AR, Khachfe HH, Fares MY, Musharrafieh U. COVID-19 pandemic: an insult over injury for Lebanon. J Community Health. 2021;46(3):487–493. doi:10.1007/s10900-020-00884-y
11. Ahsan S. Lebanese health care racked by medicine shortages. Lancet. 2021;398(10300):568. doi:10.1016/S0140-6736(21)01852-3
12. Grunert PC, Reuken PA, Stallhofer J, Teich N, Stallmach A. Inflammatory bowel disease in the COVID-19 pandemic: the patients’ perspective. J Crohns Colitis. 2020;14(12):1702–1708. doi:10.1093/ecco-jcc/jjaa126
13. Kale A, Shinde L, Sundaram S, et al. COVID‐19 pandemic and inflammatory bowel disease from patients’ perspective: a survey from COVID epicenter in India. JGH Open. 2022;6(2):126–131. doi:10.1002/jgh3.12686
14. Askar SR, Sakr MA, Alaty WHA, Sherief AF, Rashad H, Eltabbakh M. Egypt’s second wave of coronavirus disease of 2019 pandemic and its impact on patients with inflammatory bowel disease. JGH Open. 2021;5(6):664–668. doi:10.1002/jgh3.12551
15. Koletzko L, Klucker E, Le Thi TG, et al. Following pediatric and adult IBD patients through the COVID-19 pandemic: changes in psychosocial burden and perception of infection risk and harm over time. J Clin Med. 2021;10(18):4124. doi:10.3390/jcm10184124
16. Trindade IA, Ferreira NB. COVID-19 pandemic’s effects on disease and psychological outcomes of people with inflammatory bowel disease in Portugal: a preliminary research. Inflamm Bowel Dis. 2021;27(8):1224–1229. doi:10.1093/ibd/izaa261
17. Lee YJ, Kim KO, Kim MC, et al. Perceptions and behaviors of patients with inflammatory bowel disease during the COVID-19 Crisis. Gut Liver. 2022;16(1):81–91. doi:10.5009/gnl210064
18. Mir N, Cheesbrough J, Troth T, et al. COVID-19-related health anxieties and impact of specific interventions in patients with inflammatory bowel disease in the UK. Frontline Gastroenterol. 2021;12(3):200–206. doi:10.1136/flgastro-2020-101633
19. Álvarez FP, Belvis Jiménez M, Maldonado Pérez B, et al. Views of patients with inflammatory bowel disease during the COVID-19 pandemic: ACCU survey results. Rev Esp Enfermedades Dig. 2020. doi:10.17235/reed.2020.7472/2020
20. Hrabar D, Cacic P, Biscanin A, et al. IBD patients’ perception of severe acute respiratory syndrome coronavirus 2 pandemic and satisfaction with provided healthcare: a cross-sectional study. Turk J Gastroenterol. 2022;33(3):190–195. doi:10.5152/tjg.2022.21050
21. World Bank Group.Lebanon economic monitor, fall 2021: the great Denial. World Bank Group; 2021. Available from: https://www.worldbank.org/en/country/lebanon/publication/lebanon-economic-monitor-fall-2021-The-great-denial.
22. Domiati S, Itani M, Itani G. Knowledge, attitude, and practice of the Lebanese community toward COVID-19. Front Med. 2020;7:542. doi:10.3389/fmed.2020.00542
23. Spagnuolo R, Larussa T, Iannelli C, et al. COVID-19 and inflammatory bowel disease: patient knowledge and perceptions in a single center survey. Med Kaunas Lith. 2020;56(8):E407. doi:10.3390/medicina56080407
24. Nishida Y, Hosomi S, Kobayashi Y, et al. Acceptance of COVID-19 vaccines among patients with inflammatory bowel disease in Japan. Healthc Basel Switz. 2021;10(1):6. doi:10.3390/healthcare10010006
25. Viola A, Muscianisi M, Voti RL, Costantino G, Alibrandi A, Fries W. Predictors of Covid-19 vaccination acceptance in IBD patients: a prospective study. Eur J Gastroenterol Hepatol. 2021;33(1S):e1042–e1045. doi:10.1097/MEG.0000000000002320
26. Hanna P, Issa A, Noujeim Z, Hleyhel M, Saleh N. Assessment of COVID-19 vaccines acceptance in the Lebanese population: a national cross-sectional study. J Pharm Policy Pract. 2022;15(1):5. doi:10.1186/s40545-021-00403-x
27. Katta M, Shao C, Herbey I, et al. IBD and the patient-provider relationship: does trust impact telemedicine utilization? Inflamm Bowel Dis. 2022;28(Supplement_1):S83–S83. doi:10.1093/ibd/izac015.133
28. Karimi N, Kanazaki R, Lukin A, Moore AR, Williams AJ, Connor S. Clinical communication in inflammatory bowel disease: a systematic review of the study of clinician–patient dialogue to inform research and practice. BMJ Open. 2021;11(8):e051053. doi:10.1136/bmjopen-2021-051053
29. Shallal A, Lahoud C, Zervos M, Matar M. Lebanon is losing its front line. J Glob Health. 2021;11:03052. doi:10.7189/jogh.11.03052
30. Swarup N, Nayak S, Lee J, et al. Forming a support group for people affected by inflammatory bowel disease. Patient Prefer Adherence. 2017;11:277–281. doi:10.2147/PPA.S123073
31. Zingone F, Siniscalchi M, Savarino EV, et al. Perception of the COVID-19 pandemic among patients with inflammatory bowel disease in the time of telemedicine: cross-sectional questionnaire study. J Med Internet Res. 2020;22(11):e19574. doi:10.2196/19574
32. Iborra I, Puig M, Marín L, et al. Treatment adherence and clinical outcomes of patients with inflammatory bowel disease on biological agents during the SARS-CoV-2 pandemic. Dig Dis Sci. 2021;66(12):4191–4196. doi:10.1007/s10620-020-06807-0
33. Devi S. Economic crisis hits Lebanese health care. Lancet Lond Engl. 2020;395(10224):548. doi:10.1016/S0140-6736(20)30407-4
34. Taxonera C, Alba C, Olivares D, Martin M, Ventero A, Cañas M. Innovation in IBD care during the COVID-19 pandemic: results of a cross-sectional survey on patient-reported experience measures. Inflamm Bowel Dis. 2021;27(6):864–869. doi:10.1093/ibd/izaa223
35. Shaarani I, Ghanem A, Jounblat M, Jounblat H, Mansour R, Taleb R. Utilization of telemedicine by the Lebanese physicians during time of pandemic. Telemed J E-Health off J Am Telemed Assoc. 2022;28(2):219–226. doi:10.1089/tmj.2021.0090
36. Harrison SL, Buckley BJR, Rivera-Caravaca JM, Zhang J, Lip GYH. Cardiovascular risk factors, cardiovascular disease, and COVID-19: an umbrella review of systematic reviews. Eur Heart J Qual Care Clin Outcomes. 2021;7(4):330–339. doi:10.1093/ehjqcco/qcab029
37. Fouad AM, Elotla SF, Elkaraly NE, Mohamed AE. Impact of COVID-19 pandemic on patients with rheumatic and musculoskeletal diseases: disruptions in care and self-reported outcomes. J Patient Exp. 2022;9:23743735221102680. doi:10.1177/23743735221102678
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
