Back to Journals » Psychology Research and Behavior Management » Volume 16
Perceived Stress Mediating the Association Between Mindfulness and Resilience Among Registered Nurses
Authors Chen SH, Chen PJ, Lee CH, Wu YP, Ahorsu DK , Griffiths MD , Lin CY
Received 11 April 2023
Accepted for publication 12 June 2023
Published 7 August 2023 Volume 2023:16 Pages 3035—3044
DOI https://doi.org/10.2147/PRBM.S412918
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Igor Elman
Shun-Hua Chen,1 Po-Jen Chen,2 Chiu-Hsiang Lee,3,4 Yu-Ping Wu,3,4 Daniel Kwasi Ahorsu,5,6 Mark D Griffiths,7 Chung-Ying Lin8
1School of Nursing, Fooyin University, Kaohsiung, 83102, Taiwan; 2Department of Medical Research, E-Da Hospital, I-Shou University, Kaohsiung, 824005, Taiwan; 3Department of Nursing, Chung Shan Medical University, Taichung, Taiwan; 4Department of Nursing, Chung Shan Medical University Hospital, Taichung, Taiwan; 5Mental Health Research Centre, the Hong Kong Polytechnic University, Hung Hom, Hong Kong; 6Department of Special Education and Counselling, the Education University of Hong Kong, Tai Po, Hong Kong; 7International Gaming Research Unit, Psychology Department, Nottingham Trent University, Nottingham, UK; 8Institute of Allied Health Sciences, College of Medicine, National Cheng Kung University, Tainan, Taiwan
Correspondence: Chiu-Hsiang Lee, Department of Nursing, Chung Shan Medical University, Department of Nursing, Chung Shan Medical University Hospital, 1253F, Jengshin Hall, Taichung, 402, Taiwan, Tel +886-4-24730022 ext. 12216, Email [email protected] Daniel Kwasi Ahorsu, Department of Special Education and Counselling, The Education University of Hong Kong, B4-1/F-13, Tai Po, Hong Kong, Email [email protected]
Purpose: Resilience continues to be an important concept in the nursing profession due to its significant role in personal healthcare, patients’ healthcare, and leadership. The present study examined the mediating role of perceived stress in the association between mindfulness and resilience among registered nurses in order to understand their importance among those in the Taiwanese nursing profession.
Materials and Methods: Between October and November 2021, a total of 816 registered nurses participated in a cross-sectional survey including psychometric measures assessing perceived stress (Chinese Perceived Stress Scale-10), mindfulness (Chinese Mindful Attention Awareness Scale), and resilience (Chinese Questionnaire of Resilience).
Results: Results indicated that perceived stress mediated the association between mindfulness and resilience (standardized coefficient = 0.251, p< 0.001), although there was no significant association between mindfulness and resilience (standardized coefficient = 0.042, p=0.16). This suggests that perceived stress may function as both distress and eustress because mindfulness was not directly associated with resilience but indirectly via perceived stress.
Conclusion: Nurses and their administrators should focus on different ways of coping with stress so that they become more resilient in facing other stressors. Future studies may be conducted to examine the mediating role of perceived stress in the association between other coping strategies and resilience among registered nurses.
Keywords: coping, healthcare, Taiwan, cross-sectional survey, mediation analysis, mindfulness, resilience
Introduction
Resilience is an essential concept among nurses due to its significant role in personal healthcare, patients’ healthcare, and leadership. Resilience involves knowledge, skills, and abilities that enable individuals (including nurses) to recuperate and/or manage challenging situations successfully.1–3 There are varied definitions of resilience, but in general, it encompasses inner energy, strength, selfhood, developed insight concerning responsibilities and roles, faith, self-care and/or enhanced social connections that helps individuals to bounce back and persevere through challenging situations.1–6 How resilience is developed and nurtured is not fully known, although factors such as hope and spirituality, optimism, self-efficacy, sense of humor, control, competence, professional identity, clinical supervision, and experience have been reported to be associated with resilience among nurses.3,5–7 Therefore, resilience involves personal factors (eg, age, gender, experience, spirituality), professional factors (eg, validation, colleague support, mentoring), and environmental factors (eg, culture).6,8–12 Consequently, a nurse who possesses such skills and capabilities may appropriately adapt to challenges in the nursing profession.
Nurses and Stress
Nurses face various kinds of stress in their profession which can limit the quality of service they provide.9,13 Stressors observed in the nursing profession can be service-related (eg, managing difficult patients, death and/or inadequate emotional preparation), and/or work-related (eg, nurturing growth and professional development, communication gaps, role conflict, unfavorable policies and regulation, and/or poor interpersonal relationships).5,6 Without appropriate adaptive coping strategies, these stressors may lead to serious biopsychosocial challenges such as fatigue, musculoskeletal disorders, burnout, depression, lack of concentration, and unhappiness which may affect the quality of service delivery and turnover among nursing staff.14–16 This is consistent with the diathesis-stress model which asserts that stress has the ability to trigger predisposed illnesses,17 especially without adequately effective coping strategies.18,19
Stress among nurses, whether perceived or real, needs to be taken seriously because it is capable of triggering other illnesses if not well managed.20–23 Consequently, stress has been associated with physical and mental illnesses.22,24,25 Fear of contracting COVID-19 and other COVID-19-related issues appears to have been one of the leading causes of stress among healthcare professionals including nurses.14,26–28 Therefore, nurses need effective ways of coping with stress so as to deliver quality service to their patients.
Coping Strategies Among Nurses
Coping strategies remain one of the best ways of mitigating the effects of stress and are defined as an individual’s cognitive and behavioral skills needed to manage and adjust the internal and external demands of challenging and/or stressful situations.17,29 Coping strategies and resilience are closely related because resilience enables or energizes individuals to manage challenges, and helps maintain positivity and stable equilibrium while coping strategies involve the various means that are used to manage these challenges.3,29 Therefore, a nurse with higher levels of resilience is likely to have better adaptive and efficient coping strategies that may be used to deal with challenging and stressful situations.1,3,6,30 There are several types of coping strategies31–33 but the present study focused on mindfulness because it uses a unique approach (ie, awareness and non-judgmental acceptance of an individual’s moment-to-moment experience) in tackling stress.34–36 Therefore, the use of mindfulness by nurses may positively enhance their emotions, reduce their stress, and consequently improve their well-being and resilience.3,37–40
Theoretical Framework
The diathesis-stress model and the transactional model of stress and coping are used as the theoretical frameworks underlying the present study. The diathesis-stress model asserts that stress, especially distress, has the ability to trigger underlying illnesses.17 Therefore, if a nurse is predisposed to any kind of illness/health condition (eg, depression and hypertension), stress may trigger this illness/condition, especially without the use of appropriate adaptive coping strategies. The transactional model of stress and coping asserts that an individual’s ability to cope and adjust to problems/challenges is a result of interactions (transactions) between the individual and their environment.18,19 Therefore, nurses who think they do not have enough experience or ability to deal with work challenges/problems may face more stress than those who think otherwise.
Problem Statement
The aforementioned literature has examined the association between coping strategies, stress, and resilience among different populations.3,8–12,14–16,22,24,25,29,30,37–40 However, associations can be affected by other intervening variables which may weaken or strengthen these associations. Consequently, the present study examined the mediating role of perceived stress in the association between mindfulness and resilience among registered nurses.
Study Purpose and Research Questions
The aim of the present study was to examine the mediating role of perceived stress in the association between mindfulness and resilience among registered nurses. More specifically, the study examined (i) the association between perceived stress, mindfulness, and resilience among registered nurses, and (ii) the mediating role of perceived stress in the association between mindfulness and resilience among registered nurses. Therefore, the study had two major research questions: (i) Are there significant associations between perceived stress, mindfulness, and resilience among registered nurses? and (ii) Can perceived stress mediate the association between mindfulness and resilience among registered nurses?
Materials and Methods
Study Design, Participants, and Recruitment Procedure
Utilizing a cross-sectional survey study design, registered nurses were invited to participate in the study from October to November 2021, a period in which there was a minor COVID-19 outbreak in Taiwan.41,42 All the registered nurses were working in a hospital located in Taichung, a central city in Taiwan, during the survey period. Apart from being a registered nurse, the eligibility criteria included (i) being an adult aged at least 20 years and (ii) providing written informed consent clearly showing the willingness to participate in the study. The only exclusion criterion was if the nurse did not have to work shifts because shift-work can be an important factor affecting nurses’ psychosocial health.
The authors visited each unit to distribute the survey with study information. The participants were therefore fully aware of the study’s purpose and their participant rights. The surveys were then left in each unit for the registered nurses who were interested in participating. Participants could complete the survey in their own time and then post them back to the first author using pre-paid envelopes. Participants were assured that their data would be anonymous and confidential. The research team distributed 830 surveys and received 816 without any missing information (response rate: 98.3%). Some of the data from the study have been published previously.12 The study was approved by the Institutional Review Board of the Chung Shan Medical University Hospital (approval number CS2-21048). Also, the study was conducted in accordance with the guidelines outlined in the Declaration of Helsinki including obtaining written informed consent, protection of privacy and confidentiality of personal information.
Measures
Background Information
The participants’ characteristics were collected using a background information sheet. Here, questions were asked concerning the participants’ age (in years), sex (male or female), working experience (in months), level of education (eg, bachelor’s degree, or master/doctoral degree), working department (ie, internal medicine, intensive care unit, gynaecology and paediatrics, surgery and operation room, or other), marital status (ie, single, currently married, or divorced), and the number of children (0, 1, or 2 or above).
Mindfulness
The participants’ mindfulness was assessed using the Chinese translation of the Mindful Attention Awareness Scale (CMAAS).43 The CMAAS is a short 15-item scale with all of its items rated on a six-point Likert scale. A summed score using the CMAAS items is generated with higher scores indicating higher levels of mindfulness.44–48 In the present study sample, the internal consistency of the CMAAS was excellent (ω = 0.93).
Perceived Stress
The participants’ perceived stress was assessed using the Chinese version of Perceived Stress Scale-10 (PSS-10).49 The PSS-10 is a 10-item version of the original 14-item Perceived Stress Scale and all items are rated using a five-point Likert scale. After recoding the negatively worded items (ie, Items 4, 5, 7, and 8), a summed score using the PSS-10 items is generated with higher scores indicating higher levels of perceived stress.50–52 In the present study sample, the internal consistency of the PSS-10 was very good (ω = 0.89).
Resilience
The participants’ resilience was assessed using the Chinese version of the Questionnaire of Resilience (QR).53 The QR is a short 10-item scale and all items in the QR are rated using a five-point Likert scale. A summed score using the QR items is generated with higher scores indicating higher levels of resilience.53 In the present study sample, the internal consistency of the QR was excellent (ω = 0.93).
Data Analysis
Frequencies and percentages were used to analyse participants’ demographic characteristics. Then, the proposed mediation model was tested using structural equation modelling (SEM) with the diagonally weighted least-squares estimator. In the proposed mediation model, three latent constructs were estimated using the study measures: resilience (ie, the dependent variable) using the QR, perceived stress (ie, the mediator) using the PSS-10, and mindfulness (ie, the independent variable) using the CMAAS. Sobel’s54 test was used to examine the significance of mediated effect of perceived stress in the association between mindfulness and resilience. The following fit statistics were used to evaluate if the mediated model was acceptable: a Tucker-Lewis index (TLI) >0.9, a comparative fit index (CFI) >0.9, a standardized root mean square residual (SRMR) <0.08, and a root mean square error of approximation (RMSEA) <0.08.55,56 All the statistical analyses were performed using R software, with the SEM conducted using the lavaan package.57
Results
Among the 816 participants (777 females [95.2%]), most were young adults (388 aged between 20 and 29 years [47.5%]; 195 aged between 30 and 39 years [23.9%]). Over half of the participants (56.7%) had working experience of five years or more (n = 463) and over half of the participants (65.3%) were single (n=533). The majority of the participants (82.2%) had a bachelor’s degree (n=672) and almost three-quarters (71.8%) did not have any children (n=586). The departments where the participants worked are listed in Table 1.
 |
Table 1 Characteristics of the Present Sample (N = 816) |
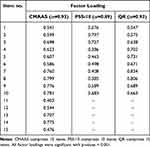
The factor loadings of the items in the three measures (ie, PSS-10, CMAAS, and QR) were moderate to strong. More specifically, factor loadings ranged between 0.403 and 0.799 for CMASS; between 0.385 and 0.797 for PSS-10; and between 0.638 and 0.834 for QR (Table 2). The factor-loading information supplemented the psychometric evidence of the three measures used in the present study. Therefore, the results of the SEM were further investigated. Utilizing SEM, the model fit was satisfactory: CFI = 0.950, TLI = 0.947, RMSEA = 0.061, and SRMR = 0.075. Moreover, significantly direct negative associations were observed between perceived stress and mindfulness (standardized coefficient = −0.665; p<0.001); and between resilience and perceived stress (standardized coefficient = −0.378; p<0.001). A significantly mediated association was observed for perceived stress in the association of mindfulness to resilience (standardized coefficient = 0.251; p<0.001). However, the direct association between mindfulness and resilience was not significant (standardized coefficient = 0.042; p=0.16) (Figure 1).
Discussion
The present cross-sectional survey study reported here comprised 816 registered nurses with varied working experience to examine (i) the association between perceived stress, mindfulness, and resilience among registered nurses, and (ii) the mediating role of perceived stress in the association between mindfulness and resilience among registered nurses. The results concerning the associations showed that there were significant negative direct associations between perceived stress and mindfulness, and between resilience and perceived stress but not between mindfulness and resilience.
More specifically, the significant negative association between perceived stress and mindfulness indicated that the higher the level of nurses’ perceived stress, the lower the level of mindfulness and vice versa. Consequently, when nurses have higher levels of stress or face more stressful situations their sense of awareness and non-judgmental acceptance of moment-to-moment experiences decreases. On the other hand, when they have a higher level of mindfulness, their level of perceived stress likely decreases. Therefore, it may be beneficial for nurses to continually practice mindfulness meditation in order to boost their capacity for handling adverse situations. This assertion is similar to other studies which examined the association between mindfulness and perceived stress.58,59 However, there was no significant direct association between mindfulness and resilience in the present study. This suggests that other factors may be responsible for enhancing the resilience of registered nurses in Taiwan apart from mindfulness.
Also, in relation to the significant negative association between perceived stress and resilience, the higher the level of nurses’ perceived stress, the lower the level of their resilience and vice versa. This further indicates that more resilient nurses may perceive fewer situations as stressful (ie, resilience may have a positive impact on events that are deemed stressful by nurses). This finding is similar to previous studies that used different populations.60–62 Based on the findings here, Taiwanese health authorities and other relevant stakeholders should implement programs to improve registered nurses’ resilience and reduce their perceived stress simultaneously. This would likely lead to registered nurses having improved health via this positive feedback loop (ie, improved resilience would help nurses cope with perceived stress and reduced perceived stress would increase nurses’ resilience levels).
The association between mindfulness and resilience was mediated by perceived stress. This is particularly interesting because no significant direct association between mindfulness and resilience was found. This implies that although mindfulness may not have been directly associated with resilience, it has an indirect role via perceived stress. This suggests that perceived stress may function as both distress and eustress. Therefore, more focus may be put on learning different ways of coping with stress among nurses so that they will be more resilient to face other stressors. This chain of activities may ultimately lead to healthy, satisfied, and experienced nurses37–40 as well as quality service delivery.15
Limitations
The present study has some limitations. First, a cross-sectional study design was used which inhibits drawing causal inferences from the findings of this study. Therefore, there is a need for longitudinal study designs or randomised control studies to be conducted to delineate the causal associations between the study variables. Second, the data comprised self-report measures which make the data susceptible to known biases (eg, social desirability bias). Nonetheless, adequate measures were taken to assuage these potential biases (eg, anonymity and confidentiality). Third, closely related to the use of self-report measures or scales is the use of a quantitative research method which has limited ability to examine issues deeply and (in the present study) to know the personal feelings, thinking, and behavior of the nurses who participated. In order to understand the nurses’ personalized views on perceived stress, resilience, and mindfulness/coping strategies, qualitative research methods or mixed-method research is needed. One of the newest qualitative research methods, photovoice (either offline or online), has been reported to provide effective and rich data by reaching a wide range of participants.63–65 Therefore, the online photovoice could be used to explore registered nurses’ work experiences, perceived stress, coping strategies, and resilience.
Implications
The present study’s findings have several implications. First, nurses and/or nursing management need to be aware that stress has the ability to trigger predisposed illnesses. Therefore, they must invest adequate resources to lessen the severity of stress and to implement different coping strategies at both an organizational and personal level. Based on the present study’s findings, mindfulness appears to be efficient in mitigating the stress of nurses and so it can be integrated into the coping strategies used by nurses. Given that the effect of stress was negatively associated with resilience, nurses should have regular seminars, meetings, and peer-education sessions, so they could learn from each other in successfully dealing with work-related stress. Second, clinicians can use these findings to help educate and treat nurses (as well as healthcare workers more generally) with stress-related issues to improve their resilience, health, and wellbeing more generally. Third, given the small number of variables examined in the present study, researchers may further explore other variables that mediate the association between mindfulness and resilience. Also, there may be a need for a more personalized view of the association between these variables using mixed-methods or qualitative research. This would help deepen the understanding of these associations from personalized viewpoints.
Conclusion
The present cross-sectional study demonstrated that perceived stress mediated the association between mindfulness and resilience among registered nurses, although there was no significant association between mindfulness and resilience. This indicates that mindfulness may only be indirectly associated with resilience via perceived stress. This also suggests that perceived stress may function as both distress and eustress. Therefore, more focus should be put on ways of coping with stress among nurses so that they will be more resilient to face other stressors. The present investigation is unique because it is the only known study to have ever examined the mediating role of perceived stress in the association between mindfulness and resilience among registered nurses. Therefore, further studies are needed to understand the mediating role of perceived stress in the association between other coping strategies and resilience among registered nurses.
Ethics Approval Statement
This study was approved by the Institutional Review Board of the Chung Shan Medical University Hospital (approval number CS2-21048). Also, the study was conducted in accordance with the guidelines outlined in the Declaration of Helsinki including obtaining written informed consent, protection of privacy and confidentiality of personal information.
Acknowledgments
We gratefully acknowledge the Chung Shan Medical University Hospital for financial support [grant number CSH-2021-A-009]. Special thanks to the administration of this hospital for allowing us to conduct this study in the nursing department. In addition, we would like to thank all those who participated.
Funding
This research was funded by the Chung Shan Medical University Hospital, Taiwan (grant number CSH-2021-A-019).
Disclosure
The authors declare that they have no competing interests.
References
1. Foster K, Roche M, Giandinoto J-A, Furness T. Workplace stressors, psychological well-being, resilience, and caring behaviours of mental health nurses: a descriptive correlational study. Int J Ment Health Nurs. 2020;29(1):56–68. doi:10.1111/inm.12610
2. Hart PL, Brannan JD, De Chesnay M. Resilience in nurses: an integrative review. J Nurs Manag. 2014;22(6):720–734. doi:10.1111/j.1365-2834.2012.01485.x
3. Wei H, Roberts P, Strickler J, Corbett RW. Nurse leaders’ strategies to foster nurse resilience. J Nurs Manag. 2019;27(4):681–687. doi:10.1111/jonm.12736
4. Edward K-L. The phenomenon of resilience in crisis care mental health clinicians. Int J Ment Health Nurs. 2005;14(2):142–148. doi:10.1111/j.1440-0979.2005.00371.x
5. Robertson HD, Elliott AM, Burton C, et al. Resilience of primary healthcare professionals: a systematic review. Br J Gen Pract. 2016;66(647):e423–e433. doi:10.3399/bjgp16X685261
6. Yılmaz EB. Resilience as a strategy for struggling against challenges related to the nursing profession. Chin Nurs Res. 2017;4(1):9–13. doi:10.1016/j.cnre.2017.03.004
7. Jackson D, Firtko A, Edenborough M. Personal resilience as a strategy for surviving and thriving in the face of workplace adversity: a literature review. J Adv Nurs. 2007;60(1):1–9. doi:10.1111/j.1365-2648.2007.04412.x
8. McCann CM, Beddoe E, McCormick K, et al. Resilience in the health professions: a review of recent literature. Int J Wellbeing. 2013;3(1):60–81. doi:10.5502/ijw.v3i1.4
9. Babapour A-R, Gahassab-Mozaffari N, Fathnezhad-Kazemi A. Nurses’ job stress and its impact on quality of life and caring behaviors: a cross-sectional study. BMC Nurs. 2022;21(1):75. doi:10.1186/s12912-022-00852-y
10. Sonika S, Kumar R. Resilience, psychological well-being, and coping strategies in medical students. Indian J Psy Nsg. 2019;16:92–97. doi: 10.4103/IOPN.IOPN_22_19.
11. Kumar R, Beniwal K, Bahurupi Y. Pandemic fatigue in nursing undergraduates: role of individual resilience and coping styles in health promotion. Front Psychol. 2022;13:940544. doi:10.3389/fpsyg.2022.940544
12. Wu YP, Ahorsu DK, Chen JS, Lee CH, Lin CY, Griffiths MD. The role of demographic factors, mindfulness and perceived stress in resilience among nurses: a cross sectional study. J Nurs Manag. 2022;30(7):3093–3101. doi:10.1111/jonm.13715
13. Sarafis P, Rousaki E, Tsounis A, et al. The impact of occupational stress on nurses’ caring behaviors and their health related quality of life. BMC Nurs. 2016;15:56. doi:10.1186/s12912-016-0178-y
14. Ahorsu DK, Lin C-Y, Marznaki ZH, Pakpour H. The association between fear of COVID-19 and mental health: the mediating roles of burnout and job stress among emergency nursing staff. Nurs Open. 2022;9(2):1147–1154. doi:10.1002/nop2.1154
15. Manomenidis G, Panagopoulou E, Montgomery A. Job burnout reduces hand hygiene compliance among nursing staff. J Patient Saf. 2019;15(4):e70–e73. doi:10.1097/PTS.0000000000000435
16. Manomenidis G, Panagopoulou E, Montgomery A. Resilience in nursing: the role of internal and external factors. J Nurs Manag. 2019;27(1):172–178. doi:10.1111/jonm.12662
17. Ingram RE, Luxton DD. Vulnerability-stress models. In: Hankin BL, Abela JRZ, editors. Development of Psychopathology: A Vulnerability-Stress Perspective. Sage; 2005:32–46.
18. Folkman S. The Oxford Handbook of Stress, Health, and Coping. Oxford University Press; 2011.
19. Lazarus RS, Folkman SC. Stress, Appraisal, and Coping. New York: Springer; 1984.
20. Ahorsu DK, Adjaottor ES, Yeboah FA, Opoku Y. Mental health challenges in academia: comparison between students of the various educational levels in Ghana. J Ment Health. 2021;30(3):292–299. doi:10.1080/09638237.2020.1739253
21. Jordan TR, Khubchandani J, Wiblishauser M. The impact of perceived stress and coping adequacy on the health of nurses: a pilot investigation. Nurs Res Pract. 2016;2016:5843256. doi:10.1155/2016/5843256
22. Lindegård A, Larsman P, Hadzibajramovic E, Ahlborg G. The influence of perceived stress and musculoskeletal pain on work performance and work ability in Swedish health care workers. Int Arch Occup Environ Health. 2014;87(4):373–379. doi:10.1007/s00420-013-0875-8
23. Monroe SM, Simons AD. Diathesis-stress theories in the context of life stress research: implications for the depressive disorders. Psychol Bull. 1991;110(3):406–425. doi:10.1037/0033-2909.110.3.406
24. Kane PP. Stress causing psychosomatic illness among nurses. Indian J Occup Environ Med. 2009;13(1):28–32. doi:10.4103/0019-5278.50721
25. Shen Y, Zhan Y, Zheng H, Liu H, Wan Y, Zhou W. Anxiety and its association with perceived stress and insomnia among nurses fighting against COVID-19 in Wuhan: a cross-sectional survey. J Clin Nurs. 2021;30(17–18):2654–2664. doi:10.1111/jocn.15678
26. Çınar D, Kılıç Akça N, Zorba Bahçeli P, Bağ Y. Perceived stress and affecting factors related to COVID-19 pandemic of emergency nurses in Turkey. J Nurs Manag. 2021;29(7):1916–1923. doi:10.1111/jonm.13329
27. Lee S-Y, Chiang K-J, Tsai Y-J, et al. Perceived stress and coping behavior of nurses caring for critical patients with COVID-19 outbreak in Taiwan: a mixed-methods study. Int J Environ Res Public Health. 2022;19(7):4258. doi:10.3390/ijerph19074258
28. M-Y L, Ahorsu DK, Kukreti S, et al. The prevalence of post-traumatic stress disorder symptoms, sleep problems, and psychological distress among COVID-19 frontline healthcare workers in Taiwan. Front Psychiatry. 2021;12:705657. doi:10.3389/fpsyt.2021.705657
29. Sampogna G, Del Vecchio V, Giallonardo V, et al. What is the role of resilience and coping strategies on the mental health of the general population during the COVID-19 pandemic? Results from the Italian Multicentric COMET Study. Brain Sci. 2021;11(9):1231. doi:10.3390/brainsci11091231
30. McDonald G, Jackson D, Wilkes L, Vickers MH. A work-based educational intervention to support the development of personal resilience in nurses and midwives. Nurse Educ Today. 2012;32(4):378–384. doi:10.1016/j.nedt.2011.04.012
31. Eslami Akbar R, Elahi N, Mohammadi E, Fallahi Khoshknab M. What strategies do the nurses apply to cope with job stress?: a qualitative study. Glob J Health Sci. 2015;8(6):55–64. doi:10.5539/gjhs.v8n6p55
32. Gholamzadeh S, Sharif F, Rad FD. Sources of occupational stress and coping strategies among nurses who work in admission and emergency departments of hospitals related to Shiraz University of Medical Sciences. Iran J Nurs Midwifery Res. 2011;16(1):41–46.
33. Tesfaye TD. Coping strategies among nurses in south-west Ethiopia: descriptive, institution-based cross-sectional study. BMC Res Notes. 2018;11(1):421. doi:10.1186/s13104-018-3557-5
34. Hayes AM, Feldman G. Clarifying the construct of mindfulness in the context of emotion regulation and the process of change in therapy. Clin Psychol Sci Pract. 2004;11(3):255–262. doi:10.1093/clipsy.bph080
35. Kabat-Zinn J. Full Catastrophe Living, Revised Edition: How to Cope with Stress, Pain and Illness Using Mindfulness Meditation. Hachette; 2013.
36. Keng S-L, Smoski MJ, Robins CJ. Effects of mindfulness on psychological health: a review of empirical studies. Clin Psychol Rev. 2011;31(6):1041–1056. doi:10.1016/j.cpr.2011.04.006
37. Galante J, Stochl J, Dufour G, Vainre M, Wagner AP, Jones PB. Effectiveness of providing university students with a mindfulness-based intervention to increase resilience to stress: 1-year follow-up of a pragmatic randomised controlled trial. J Epidemiol Community Health. 2021;75(2):151–160. doi:10.1136/jech-2020-214390
38. Lin L, He G, Yan J, Gu C, Xie J. The effects of a modified mindfulness-based stress reduction program for nurses: a randomized controlled trial. Workplace Health Saf. 2018;67(3):111–122. doi:10.1177/2165079918801633
39. Ramasubramanian S. Mindfulness, stress coping and everyday resilience among emerging youth in a university setting: a mixed methods approach. Int J Adolesc Youth. 2017;22(3):308–321. doi:10.1080/02673843.2016.1175361
40. Slatyer S, Craigie M, Rees C, Davis S, Dolan T, Hegney D. Nurse Experience of participation in a mindfulness-based self-care and resiliency intervention. Mindfulness. 2018;9(2):610–617. doi:10.1007/s12671-017-0802-2
41. Kuo Y-J, Chen Y-P, Wang H-W, et al. Community outbreak moderates the association between COVID-19-related behaviors and COVID-19 fear among older people: a one-year longitudinal study in Taiwan. Front Med. 2021;8:756985. doi:10.3389/fmed.2021.756985
42. Lin C-Y, Fan C-W, Ahorsu DK, Lin YC, Weng H-C, Griffiths MD. Associations between vaccination and quality of life among Taiwan general population: a comparison between COVID-19 vaccines and flu vaccines. Hum Vaccin Immunother. 2022;2079344. doi:10.1080/21645515.2022.2079344
43. Chang J-H, Lin Y-C, Huang C-L. Psychometric Properties of the Chinese Translation of Mindful Attention Awareness Scale (CMAAS). Psychol Test. 2011;58:235–260. doi:10.7108/PT.201104.0090
44. Brown KW, Ryan RM. The benefits of being present: mindfulness and its role in psychological well-being. J Pers Soc Psychol. 2003;84(4):822–848. doi:10.1037/0022-3514.84.4.822
45. Hansen E, Lundh LG, Homman A, Wångby‐Lundh M. Measuring mindfulness: pilot studies with the Swedish versions of the Mindful Attention Awareness Scale and The Kentucky Inventory of Mindfulness Skills. Cogn Behav Ther. 2009;38(1):2–15. doi:10.1080/16506070802383230
46. Jermann F, Billieux J, Larøi F, et al. Mindful Attention Awareness Scale (MAAS): psychometric properties of the French translation and exploration of its relations with emotion regulation strategies. Psychol Assess. 2009;21(4):506–514. doi:10.1037/a0017032
47. Michalak J, Heidenreich T, Ströhle G, Nachtigall C. Die deutsche version der Mindful Attention and Awareness Scale (MAAS): psychometrische befunde zu einem achtsamkeitsfragebogen. [German version of the Mindful Attention an Awareness Scale (MAAS)—Psychometric features of a mindfulness questionnaire.]. Z Klin Psychol Psychother. 2008;37(3):200–208. doi:10.1026/1616-3443.37.3.200
48. Poorebrahim A, Lin C-Y, Imani V, et al. Using Mindful Attention Awareness Scale on male prisoners: confirmatory factor analysis and Rasch models. PLoS One. 2021;16(7):e0254333–e0254333. doi:10.1371/journal.pone.0254333
49. Chiu Y-H, FJ-H L. Application and research development of Cohen’s perceived stress scale within and beyond sports context. Quarterly Chine Phys Educ. 2013;27(3):221–230. doi:10.6223/qcpe.2702.201309.1006
50. Bastianon CD, Klein EM, Tibubos AN, Brähler E, Beutel ME, Petrowski K. Perceived Stress Scale (PSS-10) psychometric properties in migrants and native Germans. BMC Psychiatry. 2020;20(1):450. doi:10.1186/s12888-020-02851-2
51. Liu X, Zhao Y, Li J, Dai J, Wang X, Wang S. Factor structure of the 10-item Perceived Stress Scale and measurement invariance across genders among Chinese adolescents. Front Psychol. 2020;11:537. doi:10.3389/fpsyg.2020.00537
52. Sun Y, Gao L, Kan Y, Shi BX. The Perceived Stress Scale-10 (PSS-10) is reliable and has construct validity in Chinese patients with systemic lupus erythematosus. Lupus. 2019;28(2):149–155. doi:10.1177/0961203318815595
53. Hsiao W-C, Lee -C-C, Yang H-Y, Yao S-J. Development of a questionnaire of resilience and a survey of the status of resilience of medical worker–example from a regional hospital in southern Taiwan. J Healthc Manag. 2019;20(4):325–341. doi:10.6174/JHM.201912_20(4).325
54. Sobel ME. Asymptotic confidence intervals for indirect effects in structural equation models. Sociol Methodol. 1982;13:290–312. doi:10.2307/270723
55. Lin C-Y, Broström A, Griffiths MD, Pakpour AH. Psychometric evaluation of the Persian eHealth Literacy Scale (eHEALS) among elder Iranians with heart failure. Eval Health Prof. 2020;43(4):222–229. doi:10.1177/0163278719827997
56. Nejati B, Fan C-W, Boone WJ, Griffiths MD, Lin C-Y, Pakpour AH. Validating the Persian Intuitive Eating Scale-2 among breast cancer survivors who are overweight/obese. Eval Health Prof. 2021;44(4):385–394. doi:10.1177/0163278720965688
57. Rosseel Y. Lavaan: an R package for structural equation modeling and more. Version 0.5–12 (BETA). J Stat Softw. 2012;48(2):1–36. doi:10.18637/jss.v048.i02
58. Bartlett L, Buscot M-J, Bindoff A, Chambers R, Hassed C. Mindfulness is associated with lower stress and higher work engagement in a large sample of MOOC participants. Front Psychol. 2021;12:724126. doi:10.3389/fpsyg.2021.724126
59. Vonderlin R, Biermann M, Bohus M, Lyssenko L. Mindfulness-based programs in the workplace: a meta-analysis of randomized controlled trials. Mindfulness. 2020;11(7):1579–1598. doi:10.1007/s12671-020-01328-3
60. García-León MÁ, Pérez-Mármol JM, Gonzalez-Pérez R, García-Ríos M, Peralta-Ramírez MI. Relationship between resilience and stress: perceived stress, stressful life events, HPA axis response during a stressful task and hair cortisol. Physiol Behav. 2019;202:87–93. doi:10.1016/j.physbeh.2019.02.001
61. Lara-Cabrera ML, Betancort M, Muñoz-Rubilar CA, Rodríguez Novo N, De Las Cuevas C. The mediating role of resilience in the relationship between perceived stress and mental health. Int J Environ Res Public Health. 2021;18(18):9762. doi:10.3390/ijerph18189762
62. Sarrionandia A, Ramos-Díaz E, Fernández-Lasarte O. Resilience as a mediator of emotional intelligence and perceived stress: a cross-country study. Front Psychol. 2018;9:2653. doi:10.3389/fpsyg.2018.02653
63. Armiya’u AY, Yildirim M, Muhammad A, Tanhan A, Young JS. Mental health facilitators and barriers during Covid-19 in Nigeria. J Asian Afr Stud. 2022. doi:10.1177/00219096221111354
64. Doyumğaç İ, Tanhan A, Kıymaz MS. Understanding the most important facilitators and barriers for online education during COVID-19 through online photovoice methodology. Int J High Educ. 2021;10(1):166–190. doi:10.5430/ijhe.v10n1p166
65. Tanhan A, Strack RW. Online photovoice to explore and advocate for Muslim biopsychosocial spiritual wellbeing and issues: ecological systems theory and ally development. Curr Psychol. 2020;39(6):2010–2025. doi:10.1007/s12144-020-00692-6
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.