Back to Journals » HIV/AIDS - Research and Palliative Care » Volume 14
Perceived HIV Stigma and Associated Factors Among Adult ART Patients in Wolaita Zone, Southern Ethiopia
Authors Alemu A , Meskele M , Darebo TD, Beyene Handiso T , Abebe A , Paulos K
Received 28 April 2022
Accepted for publication 30 October 2022
Published 7 November 2022 Volume 2022:14 Pages 487—501
DOI https://doi.org/10.2147/HIV.S372738
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Olubunmi Akindele Ogunrin
Aklilu Alemu,1 Mengistu Meskele,1 Tadele Dana Darebo,1 Tilahun Beyene Handiso,1 Amene Abebe,1 Kebreab Paulos2
1School of Public Health, Wolaita Sodo University, Wolaita Sodo, Ethiopia; 2School of Midwifery, Wolaita Sodo University, Wolaita Sodo, Ethiopia
Correspondence: Kebreab Paulos, Email [email protected]
Objective: This study aimed to assess perceived HIV stigma and associated factors among adult ART patients in Wolaita Zone, Southern Ethiopia.
Methods: A facility-based cross-sectional study was conducted among 638 participants selected using a multistage sampling technique from July 10 to September 2020. A 12-item short version of the HIV stigma scale was used to measure HIV-related stigma. Data were collected by the interview method using a pre-tested questionnaire. Binary and multivariable logistic regression analyses were performed to identify the factors associated with the outcome variable. The strength and direction of the association were measured using the adjusted odds ratio (AOR) with a 95% confidence interval (CI). Statistical significance was declared at P-value < 0.05.
Results: In this study, 57.8% (95% CI = 54.1%-61.9%) of people under HIV care perceived high stigma and 450 (70.5%) disclosed their HIV status. Widowed marital status (AOR = 2.984; 95% CI = 1.728– 5.155), primary education (AOR = 3.36; 95% CI = 2.072– 5.42), undisclosed HIV status (AOR = 1.657; 95% CI = 1.121– 2.451), poor social support (AOR: 2.05; 95% CI = 1.195– 3.433), and being member of an HIV support group (AOR: 0.396; 95% CI = 0.249– 0.630) were significantly associated with perceived stigma.
Conclusion: The perceived stigma is high among adult ART patients in the study setting. Widowed marital status, primary education, undisclosed HIV status, membership to the social support network NEP+ and poor social support were predictors of perceived HIV stigma. Thus, ART patients should be given more psychosocial support to minimize their perceived public HIV-related stigma.
Keywords: adult, ART, HIV, patients, people living with HIV, perceived stigma
Introduction
In many parts of the world, Human Immunodeficiency Virus (HIV) or Acquired Immuno Deficiency Syndrome (AIDS) is commonly considered a consequence of immoral risky sexual behaviors in the back of society thought including Ethiopia. Due to this reason, people living with HIV (PLHIV) face HIV-related stigma in addition to medical problems.1,2 Even though HIV/AIDS is managed in a habitual and convenient condition, PLHIV are facing serious challenges related to HIV-related stigma and discrimination.3
People living with HIV fear stigma and dismissal from their families, friends, and society, and losing their social reputation.4 Moreover, the perceived separation that social dismissal brings can lead to loss of self-esteem, depression, and indeed attempt or act of suicide.5 In a global assessment of HIV-related stigma and discrimination from 36 countries included, in 25 of them, greater than 50% of people aged 15–49 years hold discriminatory beliefs and attitudes toward PLHIV.6
HIV-related Stigma refers to attitudes and beliefs that lead people to reject, avoid, or fear those they perceive as being different.7 Perceived stigma refers to the fear of public stigma and discrimination that prevents people from talking about their experiences and seeking help.8 Perceived stigma among HIV patients might be expressed by a range of perceived mistreatment from society such as the denial of services, expulsion from families, and verbal abuse. People who face and anticipate such mistreatment due to their HIV status are in the continuous feeling of guilt, shame, and loss of self-esteem accompanied by frequent thoughts of harming themselves.9
Based on the data from UNAIDS, one in eight PLHIV face HIV care limitations due to public stigma and discrimination.10 In Ethiopia, studies show that the experience of perceived stigma among PLHIV ranges from 42% to 60%.11–13 Though in the last ten years, in Ethiopia, public HIV- related stigma and discrimination have significantly declined, PLHIV are still suffering from an exaggerated perceived public stigma and discrimination.14,15
Perceived HIV stigma among PLHIV impedes the nutritional and HIV care programs.16 In Ethiopia, PLHIV avoids going to therapeutic feeding centers to receive therapeutic foods such as plumpy nuts and avoids going nearer to health facilities for ART drugs in fear of being exposed to the public.17,18 Moreover, high perceived HIV stigma among PLHIV compromises the retention of patients in HIV care increases the incidence of mental health problems and affects the overall quality of life.19–22 Thus, this affects not only the well-being of the patients but also it affects the overall HIV prevention and control programs.
Perceived HIV-related stigma aggravates the undisclosing of actual or likely HIV status, and it increases the chance of risky sexual behavior.23 For instance, a study conducted in Ethiopia shows that one in six PLHIV who have high perceived HIV-related stigma reported that their negotiation skills regarding safe sex practice were poor and it has prevented them from seeking sexual and reproductive health services.24
Achieving the Sustainable Development Goal (SDG) of creating an AIDS-free era and ensuring healthy lives for all by 2030 requires reducing the incidence of HIV/AIDS.25 Perceived HIV stigma affects HIV prevention and control programs by increasing risky sexual practices, affecting the nutritional and healthcare programs, limiting the accessibility of healthcare services, and increasing the isolation of patients from health and social services. However, in Ethiopia, perceived HIV-related stigma is not fully known. Therefore, this study aimed to assess the magnitude of perceived HIV stigma and its associated factors among adult ART patients in Wolaita Zone, Southern Ethiopia.
Materials and Methods
Description of the Study Setting
This study was conducted in Wolaita Zone, Southern Ethiopia. Wolaita Zone is one of sixteen zones in the Southern Region of Ethiopia. According to the Wolaita Zone base plan of 2019, from the total population of 2, 067,163 living in the Zone, 1,054,233 were females while the remaining were males. The Zone has a total area of 4512 square kilometers and is administratively divided into 16 districts and 6 town administrations. In Wolaita Zone there are 10 hospitals; two private and eight public, 427 primary healthcare units (77 health centers and 350 health posts), and several pharmacies and drug vendors. Of the total health facilities, 18 were currently providing ART service in the Zone.
Study Design, Period, and Population
A facility-based cross-sectional study design was conducted among 638 adult ART patients from July 10 to September 2020. The source population was all people who are receiving ART medication and aged 15 years. Adult ART patients in the selected facility and aged 15 years and above were considered as the study population. Patients with less than 6 months duration of HIV care, severely ill and unable to respond to questions, and mentally impaired were excluded from the study. A simple cognitive mental impairment test tool was used to screen patients for cognitive status.26 Patients whose screening test results for cognitive impairment score equal to or greater than seven scores were omitted from the study. However, these patients were referred for further mental health status assessment and treatment.
Measurements and Operational Definition
Perceived Stigma
Was assessed using a reliable HIV stigma scale which was used in the other previous studies.13,27–29 The short 12 item stigma scale was used to collect the data.30 The scale consisted of 12 items rated on 4-point Likert scores (strongly disagree to disagree) and the score ranging from 12 to 48 scores with an average score of 30. Then, its reliability was assessed in the study area context and cronbach’s alpha was 0.758. In this study, an average value of 30 was used as a cut-off point to determine the level of HIV stigma by benchmarking previous studies.31–35 Hence, study participants who had a stigma score of equal or greater than the variable mean score of 30 from 12 stigma assessment questions were classified as having “high perceived HIV stigma” while a score less than a variable mean score of 30 was considered as “low perceived HIV stigma”.
Adherence
Was defined as patients’ self-reported behavior of taking ARV medications without missing at least a single ARV dose 30 days before the study. Poor adherence if missed≥ 6 pills (<84%) of 30 doses at the time of the study and good Adherence (95%), if missed ≤2 doses of 30 doses or fair adherence (85–94%), if missed 3–5 doses of 30 ARV doses.36,37
Viral Load Suppression (VLS)
Was assessed using the patient chart review, and the client’s last 6-month serum viral load results were considered at the time of the data collection. A client is having a high viral load if he/she had a serum viral load of >1000 copies/mL before the survey and a non-detectable viral load if below 1000 copies/mL.37
Social Support
In this study, HIV patients were asked to rate the support they receive from their community members using Oslo Social Support Scale (OSSS-3).38 The scale was three items with scores ranging from three to fourteen scores. Its internal consistency in our test was 0.711, which was better than the internal consistency of (0.640) on the developer’s scales. HIV patients are said to have poor social support if they had a score of 3–8 out of three questions, moderate social support was those scored 9–11 scores out of three questions. Otherwise, strong social support if scored 12–14 scores out of the three questions.
Sample Size Determination
The Sample size was estimated by using Epi info statistical software version seven. We used the proportion of perceived HIV stigma as 29.1% (p=29%) from the previous study,39 95% CI, the margin of error between the estimated and actual population proportion of HIV stigma at 5%, and obtained a sample size of 316. However, we have 18 ART-providing clusters for this group of patients. To account for this intra-cluster variation of the health facilities, we used a design effect of two the sample size become 632. Adding the 10% non-response the final sample size was estimated to be 695.
Sampling Procedure
In this study, a multi-stage sampling technique with proportional allocation to the size of each health facility was done. Currently, there are seven hospitals and 69 health centers in the Wolaita Zone of which 18 health facilities were identified as providing ART service. The health facilities were stratified into hospitals and health centers. Hospitals were further stratified into referral and primary hospitals. Nine health facilities (five-health centers, one referral hospital, and three primary hospitals) were randomly selected from each stratum of the health facilities.
The total sample size was then proportionally allocated to the average monthly patient flow using the last 6-months before the study. Accordingly, the total monthly patient flow for the nine ART health facilities was 3280. Using the total sample size of 695, the sampling interval was calculated to be 3280/695= five. The lottery method was used to determine the first participant from the first one to five on the patient logbook and the 3rd participant was randomly selected. After including the third (3rd) participant, the second would be the eighth (3+5=8), the third would be (8+5=13), and we continued this way until fulfilling the allocated sample size from all health facilities.
Data Quality Control and Data Collection
The quality of data assured of the maximum attainable level by using a standardized adapted questionnaire. To ensure the quality of data, we used 5% (35 participants) of the total sample size to pre-test data collection tools. Data collectors were trained for two days on the purpose and procedure of data collection by principal investigators. All data collectors availed of the field guideline that was prepared in their local language to maintain the procedure consisting of all ART clinics. The four supervisors and investigators coordinated data collection. Cronbach's alpha was calculated for the stigma scale to ensure reliability. Besides, data collectors, supervisors, and the principal investigator checked the questionnaire for completeness and consistency after each day of data collection.
Data were collected through face-to-face interviews in a separate room after participants complete their ART services. The data collection tool consisted of two parts: first, background information and HIV-related question, and the second part consisted of adopted HIV stigma scale questions. The trilingual person translated the tool from English to Amharic then to “Wolaitatto dona” and back to English to confirm its consistency (Supplementary Files Section 2). Six ART-providing health professionals and six case managers were involved in the data collection process. All of the ART-providing health professionals were bachelor’s degree holders and from the six case managers, two were bachelor of nursing holders, one was a diploma in public health nursing and the remaining three were secondary education completed with a minimum of two years of psychosocial support work experience with PLHIV.
Data Management and Analysis
Before data entry in Epi Data version 3.1, the data were checked for completeness and consistency. Then, the data were exported into SPSS version 21 for data analysis was done. Descriptive statistics including proportions, distribution, and measures of central tendency were computed. Stigma responses were summed for the total stigma score. In the regression model, the stigma scores equal to or greater than the variable mean score of 30 were coded as “1” for high stigma, and stigma scores less than the variable mean score of 30 were coded as “0” for low stigma.
Variables with a p-value less than 0.25 in the bivariate logistic regression analysis were considered candidates for multivariable logistic regression analysis. The Hosmer–Lemeshow goodness-of-fit test was checked and the model was a good fit (P-value=0.263). Variables with a p-value<0.05 in multivariable logistic regression were considered statistically significant. The multi-co linearity test was conducted using a VIF cut-off <5 and was in the acceptable range. Both crude and adjusted odds ratios with a 95% CI were reported.
Results
Socio-Demographic and Psychosocial Characteristics of Adult ART Patients in Wolaita Zone, Southern Ethiopia
A total of 638 participants were included in this study with a response rate of 92%. Fifty-five participants terminated the interview before completing the full questions and two refused to participate in the study. More than half, 353 (55.3%) of the participants were females and 295 (46.2%) belong to the age group of 30–39 years. The mean age of participants was 35±8.3 years. The majority, 365 (57.2%) of the participants were Wolaita in ethnicity, and 285 (44.7%) were married. Among the study participants, 257 (40.3%) completed primary education and 266 (42.3%) were merchants in occupation. Regarding income, 427 (66.9%) were earning a monthly income of more than one thousand Ethiopian birrs and 537 (84.2%) were urban residents (Table 1).
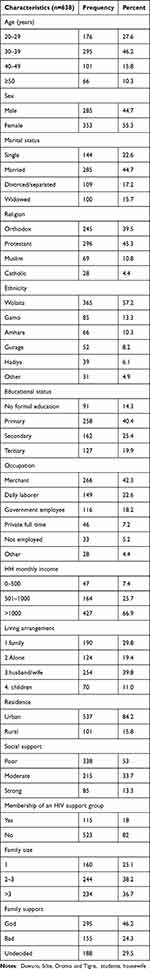 |
Table 1 Socio-Demographic and Psychosocial Characteristics of Adult People Living with HIV (n=638) in Wolaita Zone, July 10-September 2020 |
Individual and HIV-Related Characteristics of Adult ART Patients in Wolaita Zone, Southern Ethiopia
The majority of ART patients, 176 (27.6%) were tested for HIV due to suspect of HIV/AIDS by health providers during their first-time diagnosis, 430 (67.4%) were tested by their free will, 142 (22.3%) were forced to be tested, and 578 (90.6%) were received both pre- and post-test counseling. Three hundred ninety-eight (62.4%) were diagnosed with HIV more than a year ago.
Regarding the disclosure of HIV status, 450 (70.5%) participants disclosed their HIV status either to their spouses or to family or close friends. The majority of undisclosed HIV status was due to fear of losing their family 97 (15.2%). Sixty (9.4%) of the participants reported that their HIV status was disclosed against their will and 23 (3.6%) blamed family members or caregivers, and 13 (2%) blamed health service providers for their involuntary HIV status disclosure.
As to the clinical characteristics of participants, 471 (73.8%) were treated for >3 years, and 541 (84.8%), 65 (10.2%), and 32 (5%) had good, fair, and poor adherence to ARV medications respectively. On the other hand, 502 (78.7%) of participants had viral suppression of less than 1000 copies/mL and 119 (18.7%) had comorbidity in the last three months. Regarding the WHO stage of the disease, 11 (1.9%) had stage 3/4 HIV/AIDS and 57 (8.9%) were admitted to the hospital in the last 6 months for HIV-related treatment. Moreover, 127 (19.9%) rated their current health status as bad (Table 2).
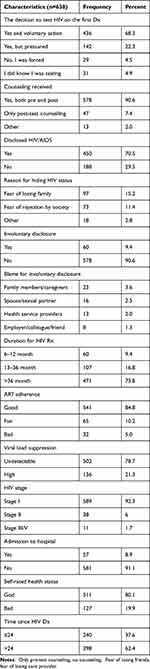 |
Table 2 Individual and HIV-Related Characteristics of Adult People Living with HIV (n=638) in the Wolaita Zone, July 10-September 2020 |
Perceived HIV-Related Stigma and the Social Support of Adult ART Patients in Wolaita Zone, Southern Ethiopia
Of the total study participants, 369 (57.8%), (95% CI=54.1–61.9) reported high HIV-related stigma while the remaining reported low. Regarding the response to individual items toward perceived stigma, most of the study participants agree that they had the concern to disclose their HIV/AIDS status to others (Table 3).
 |
Table 3 Stigma Responses Towards Individual Items by Adult People Living with HIV (n=638) in Wolaita Zone, July 10-September 2020 |
Out of the total study participants, only 115 (18%) were a member of an HIV/AIDS support group (NEP+) while 155 (24.3%) of participants reported that they were facing bad family support. Concerning the family size of the participants, 234 (36.5%) were living with more than 3 people and 254 (39.8%) were living with their spouse. Three hundred thirty-eight (53%) participants reported that the social support from their community is poor (Figure 1).
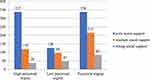 |
Figure 1 Level of social support by perceived stigma. |
Factors Associated with Perceived HIV Stigma Among Adult ART Patients in Wolaita Zone, Southern Ethiopia
In bivariate logistic regression analysis at p-value <0.25 age, residence, marital status, educational status, the decision to test HIV, membership in NEP+, ART adherence, viral load suppression, and social support were found to be statistically significantly associated with perceived HIV-related stigma and candidate variables for subsequent multivariable regression analysis.
In the final model (multivariable logistic regression analysis), marital status, educational status, HIV disclosure, poor social support, and being a member of NEP+ were found to be independently associated with perceived HIV stigma. Perceived HIV stigma was approximately 3 times higher among widowed HIV patients than among married HIV patients (AOR=2.984; 95% CI=1.728–5.155). HIV patients who attained primary education were more than three times more likely to experience perceived HIV/AIDS stigma when compared to those who attended tertiary education (AOR=3.36; 95% CI=2.072–5.42). HIV patients who did not disclose their status were nearly two times more likely to experience perceived HIV stigma than those who disclosed their HIV status (AOR=1.657; 95% CI=1.121–2.451). Perceived HIV stigma was two times higher among patients who get poor social support than those who get good social support (AOR: 2.05; 95% CI=1.195–3.433). On the other hand, those patients who owned a membership in NEP+ were 60% less likely to experience perceived stigma as compared with a non-member (AOR=0.396; 95% CI=0.249–0.63) (Table 4).
 |
Table 4 Factors Associated with Perceived HIV Stigma Among Adult People Living with HIV in HIV (n=638) in Wolaita Zone, July 10-September 2020 |
Discussion
This study attempted to determine perceived HIV stigma and associated factors among adult ART patients in Wolaita Zone, Southern Ethiopia. The study found that the overall perceived HIV stigma among adult ART patients was found to be 57.8%, (95% CI=54.1–61.9) in the study area.
In Ethiopia, Turi et al (2021), Adane et al (2020) and Chekole (2020) found a lower perceived HIV stigma of 42%, 49%, and 43%, respectively, than the current study.31,32,40 This dissimilarity could be explained by the difference in the study setting, sample size, tool, and participant variation.
The finding is consistent with the study reported by other researchers; Nigeria (59.9%), Cameron 62.6% and Ethiopia reported 61.1%.41–43 The current study found a lower perceived HIV stigma than three other studies from South Africa, Nigeria, and Iran where the studies reported perceived HIV stigma of 66.5%, 77.2%, and 67.9%, respectively.35,44,45 The difference can also be due to the variation in socioeconomic status, culture, sample size, and stigma measurement tool.
The odds of experiencing perceived HIV stigma was three times higher for widowed HIV patients than married HIV patients. This finding was similar to the study findings from Ethiopia,32 and South Africa45 and inconsistent with the findings from India46 and Iran.33 The possible reason for the inconsistency might be attributed to the study setting, socio-cultural variation, and the time lapse between the studies.
Those HIV patients who did not disclose their status were almost two times more likely to experience perceived HIV stigma than those who disclose their status. This result was reported similarly to the other two studies in Ethiopia.31,39
This study also indicated that those who attended the primary educational level were four times more likely to experience perceived HIV stigma than those who attended the tertiary educational level. A lower level of education was similarly associated with higher HIV-related stigma in several previous studies.32,41,43,47 However, the present study result seems to be inconsistent with the study reports of India and China where the studies reported a higher level of education (above secondary educational level) has a positive association with HIV-related stigma.34,48 The difference might be explained in terms of socio-cultural, lifestyle, and accessibility of education.
The statistical association between educational level and HIV-related stigma was not reported in the other two studies from India and South Africa.33,45 The possible explanation for the difference might be that socio-cultural and sample size differences.
The odds of perceived HIV stigma was more than 2 times higher among patients who poorly get social support than those who get good social support. Those who owned a membership of a NEP+ are less likely to develop perceived HIV stigma than non-members. This result was reported similarly in another study from South Africa.45 However, the finding is contrary to the study finding from India.49 This discrepancy might be due to the study population, sample size, and the study setting.
According to this study’s findings, high-perceived stigma by PLHIV was reported in the study area contrary to the decline in the actual stigma and discrimination due to national and international HIV-related stigma elimination efforts. A high perception of stigma may halt the effort to HIV prevention and control through risky sexual practice, unsafe sex, undisclosed HIV status, and imposing high care-seeking limitations.
Policymakers, governmental and non-governmental organizations, and other stakeholders who are working on HIV prevention and control should simultaneously focus on HIV patients’ perceived stigma and actual. Wolaita Zone and other policymakers should design and implement improving the accessibility of education for HIV patients. Enhancement of social support schemes and membership in HIV patients support network (NEP+) should be improved. Furthermore, further large-scale studies using mixed methods and implementation science principles are recommended.
Strength of the Study
The present study provides additional evidence concerning HIV-related stigma among PLHIV in southern Ethiopia from the patients’ perspective in which little is known. The study also included the special population group of PLHIV and created an opportunity for the participants to share their perceptions regarding HIV-related stigma. The study findings’ validity was also ensured by the use of a large stratified random sample and using the standard measurements and data collection tool.
Limitations of the Study
This study does not consider people with HIV who are not enrolled in HIV care. Hence, the findings are generalized to only those in HIV care. During the translation and adoption of the data collection tool, there might be an introduction of deviation from the original developer’s version. Lastly, the subjectivity of some of the questions may pave the way for social desirability bias.
Conclusion
According to this study, the perceived HIV stigma was high among adult ART patients in this study area when compared to the fact that the declining actual HIV-related stigma and discrimination in Ethiopia. Perceived HIV stigma was significantly higher among widowed, those who attended only primary education, and those who did not disclose their HIV status. However, perceived HIV stigma was significantly lower among those who owned membership to the HIV support group NEP+ and those getting higher social support. Targeted counseling and encouragement of PLHIV to disclose their HIV status, encouraging patients to be included in the HIV support group NEP+, and strengthening the social support system for PLHIV are recommended.
Abbreviations
ART, anti-retroviral therapy; HIV/AIDS, human immunodeficiency virus/acquired immunodeficiency syndrome; NEP+, Network of Networks of HIV positives in Ethiopia; PLHIV, people living with HIV.
Data Sharing Statement
All data generated or analyzed during this study are included in this published article and its Supplementary Information Files.
Ethical Consideration
The current study was conducted following the declaration of Helsinki for studies involving human participants. The study protocol was approved by Wolaita Sodo University, College of Health and Medical Science, Institutional Health Research Ethics Review Committee. Official letters of cooperation were written to all hospitals, health centers, and concerned administrative bodies sequentially. Information on the study was explained to the participants, including the procedures, potential risks, and benefits of the study. Informed voluntary written consent was obtained from all respondents before the study (Supplementary Files Section 1).
Acknowledgment
We would like to thank Wolaita Sodo University and the Wolaita Zone health department administrative bodies for their moral and technical support. Next, we would like to acknowledge, Wolaita Sodo’s teaching and referral hospital management, Zonal Hospital administration, data collectors, supervisors, study participants, and all who contributed directly or indirectly to the success of this study.
Author Contributions
All authors equally contributed to this work beginning from the conception, study design, execution, acquisition of data, analysis, and interpretation. Authors of this work took part in the drafting, revising, and/or critically reviewing of the article and finally agreed on the journal to which the article was submitted. All authors are also reviewed and agreed on all versions of the article before submission, during revision, and the final version is accepted for publication and agreed to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests.
References
1. Haghdoost A, Karamouzian M. Zero New HIV Infections, Zero Discrimination, and Zero AIDS-Related Deaths: feasible Goals or Ambitious Visions on the Occasion of the World AIDS Day? Int J Prev Med. 2012;3(12):819–823. doi:10.4103/2008-7802.104850
2. Nachega JB, Morroni C, Zuniga JM, et al. HIV-related stigma, isolation, discrimination, and serostatus disclosure: a global survey of 2035 HIV-infected adults. J Int Assoc Physicians AIDS Care. 2012;11(3):172–178. doi:10.1177/1545109712436723
3. Chambers LA, Rueda S, Baker DN, et al. Stigma, HIV and health: a qualitative synthesis. BMC Public Health. 2015;15(1):848. doi:10.1186/s12889-015-2197-0
4. Kontomanolis EN, Michalopoulos S, Gkasdaris G, Fasoulakis Z. The social stigma of HIV-AIDS: society’s role. HIV/AIDS. 2017;9:111–118. doi:10.2147/HIV.S129992
5. The well project. Stigma and Discrimination Against Women Living with HIV submitted on Nov 2, 2021.2021; Available from: file:///C:/Users/WSU/Downloads/The%20Well%20Project%20-%20Stigma%20and%20Discrimination%20Against%20Women%20Living%20with%20HIV%20-%202022-03-22.pdf.
6. UNAID. HIV and stigma and discrimination: human rights fact sheet series. 2021; Available from: https://www.unaids.org/sites/default/files/media_asset/07-hiv-human-rights-factsheet-stigma-discrmination_en.pdf.
7. Gray AJ. Stigma in psychiatry. J R Soc Med. 2002;95(2):72–76. doi:10.1177/014107680209500205
8. Mohite VR, Mohite RV, George J. Correlates of perceived stigma and depression among the women with HIV/AIDS infection. Bangladesh J Med Sci. 2015;14(2):151–158. doi:10.3329/bjms.v14i2.21864
9. Burnham KE, Cruess DG, Kalichman MO, Grebler T, Cherry C, Kalichman SC. Trauma symptoms, internalized stigma, social support, and sexual risk behavior among HIV-positive gay and bisexual MSM who have sought sex partners online. AIDS Care. 2016;28(3):347–353. doi:10.1080/09540121.2015.1096894
10. UNAIDS. Make Some Noise for Zero Discrimination on 1 March 2017; 2017. Available from: https://www.unaids.org/en/resources/presscentre/pressreleaseandstatementarchive/2017/february/20170301_zero-discrimination-day.
11. Nikus Fido N, Aman M, Brihnu Z. HIV stigma and associated factors among antiretroviral treatment clients in Jimma town, Southwest Ethiopia. HIV/AIDS. 2016;8:183–193. doi:10.2147/HIV.S114177
12. Turi E, Simegnew D, Fekadu G, et al. High Perceived Stigma Among People Living with HIV/AIDS in a Resource Limited Setting in Western Ethiopia: the Effect of Depression and Low Social Support. HIV/AIDS. 2021;13:389–397. doi:10.2147/HIV.S295110
13. Adane B, Yalew M, Damtie Y, Kefale B. Perceived Stigma and Associated Factors Among People Living with HIV Attending ART Clinics in Public Health Facilities of Dessie City, Ethiopia. HIV/AIDS. 2020;12:551–557. doi:10.2147/HIV.S274019
14. Salih MH, Tessema GA, Cherkos EA, Ferede AJ, Zelalem Anlay D. Stigma towards people living on HIV/AIDS and associated factors among nurses’ working in Amhara region referral hospitals, Northwest Ethiopia: a cross-sectional study. Adv Nursing. 2017;2017. doi:10.1155/2017/6792735
15. Gebremedhin M, Gebrehawerya T, Tesfaye G, Gebretsadik G, Kebede L. Stigma and Discrimination towards HIV Positive People among In-School Adolescents. J HIV AIDS. 2017;3:3.
16. Zareipour M, Ali Morowatisharifabad M, Movahed E, Hosseinzadeh M, Ameri M. Application of information-motivation-behavioral skills model in adherence to diet and reduction of depression among HIV-positive patients: health promotion strategy 90-90-90. Int J HIV Related Problems. 2021;20(3):187–194.
17. Tesfay F, Javanparast S, Mwanri L, Ziersch A. Stigma and discrimination: barriers to the utilisation of a nutritional program in HIV care services in the Tigray region, Ethiopia. BMC Public Health. 2020;20(1):1–13. doi:10.1186/s12889-020-09040-6
18. Hoffman S, Tymejczyk O, Kulkarni S, et al. Brief Report: stigma and HIV Care Continuum Outcomes Among Ethiopian Adults Initiating ART. J Acquired Immune Deficiency Syndromes. 2017;76(4):382–387. doi:10.1097/QAI.0000000000001530
19. Ekstrand ML, Heylen E, Mazur A, et al. The role of HIV stigma in ART adherence and quality of life among rural women living with HIV in India. AIDS Behav. 2018;22(12):3859–3868. doi:10.1007/s10461-018-2157-7
20. Tesfaw G, Ayano G, Awoke T, et al. Prevalence and correlates of depression and anxiety among patients with HIV on-follow up at Alert Hospital, Addis Ababa, Ethiopia. BMC Psychiatry. 2016;16(1):368. doi:10.1186/s12888-016-1037-9
21. Bitew H, Andargie G, Tadesse A, Belete A, Fekadu W, Mekonen T. Suicidal ideation, attempt, and determining factors among HIV/AIDS patients, Ethiopia. Depress Res Treat. 2016;2016. doi:10.1155/2016/8913160
22. Ameri M, Movahed E, Farokhzadian J. Effect of information, motivation, and behavioral skills model on adherence to medication, diet, and physical activity in HIV/ADIS patients: a health promotion strategy. J Educ Health Promot. 2020;9:317. doi:10.4103/jehp.jehp_188_20
23. Mosisa G, Woldemichael K, Ayalew F. Risky sexual behavior and associated factors among antiretroviral therapy attendees in Nekemte Referral Hospital, Western Ethiopia: a cross-sectional study. HIV/AIDS. 2018;10:125.
24. Dessalegn NG, Hailemichael RG, Shewa-Amare A, et al. HIV Disclosure: HIV-positive status disclosure to sexual partners among individuals receiving HIV care in Addis Ababa, Ethiopia. PLoS One. 2019;14(2):e0211967. doi:10.1371/journal.pone.0211967
25. Grossman CI, Stangl AL. Global action to reduce HIV stigma and discrimination. J Int AIDS Soc. 2013;16:18881. doi:10.7448/IAS.16.3.18881
26. Callahan CM, Unverzagt FW, Hui SL, Perkins AJ, Hendrie HC. Six-item screener to identify cognitive impairment among potential subjects for clinical research. Med Care. 2002;771–781. doi:10.1097/00005650-200209000-00007
27. Subedi B, Timilsina BD, Tamrakar N. Perceived stigma among people living with HIV/AIDS in Pokhara, Nepal. HIV/AIDS. 2019;11:93–103. doi:10.2147/HIV.S181231
28. Chekole YA, Tarekegn D. HIV-related perceived stigma and associated factors among patients with HIV, Dilla, Ethiopia: a cross-sectional study. Ann Med Surgery. 2021;71:102921. doi:10.1016/j.amsu.2021.102921
29. Pourmarzi D, Khoramirad A, Gaeeni M. Perceived Stigma in People Living With HIV in Qom. J Family Reproductive Health. 2017;11(4):202–210.
30. Reinius M, Wettergren L, Wiklander M, Svedhem V, Ekström AM, Eriksson LE. Development of a 12-item short version of the HIV stigma scale. Health Qual Life Outcomes. 2017;15(1):1–9. doi:10.1186/s12955-017-0691-z
31. Adane B, Yalew M, Damtie Y, Kefale B. Perceived Stigma and Associated Factors Among People Living with HIV Attending ART Clinics in Public Health Facilities of Dessie City, Ethiopia. HIV/AIDS. 2020;12:551.
32. Chekole YA. HIV-Related Perceived Stigma and Associated Factors Among Patients with HIV. Dilla, Ethiopia: Cross-Sectional Study; 2020.
33. Pourmarzi D, Khoramirad A, Gaeeni M. Perceived Stigma in People Living With HIV in Qom. J Family Reproductive Health. 2017;11(4):202.
34. Subedi B, Timilsina BD, Tamrakar N. Perceived stigma among people living with HIV/AIDS in Pokhara, Nepal. HIV/AIDS. 2019;11:93.
35. Zarei N, Joulaei H, Fararouei M. Perceived stigma and quality of life among women living with HIV/AIDS. Women’s Health Bulletin. 2017;4(1):1–6.
36. Ketema AK, Weret ZS. Assessment of adherence to highly active antiretroviral therapy and associated factors among people living with HIV at Debrebrihan Referral Hospital and Health Center, Northeast Ethiopia: a cross-sectional study. HIV/AIDS. 2015;7:75.
37. Desta AA, Woldearegay TW, Futwi N, et al. HIV virological non-suppression and factors associated with non-suppression among adolescents and adults on antiretroviral therapy in northern Ethiopia: a retrospective study. BMC Infect Dis. 2020;20(1):1–10. doi:10.1186/s12879-019-4732-6
38. Kocalevent R-D, Berg L, Beutel ME, et al. Social support in the general population: standardization of the Oslo social support scale (OSSS-3). BMC Psychol. 2018;6(1):1–8. doi:10.1186/s40359-018-0249-9
39. Melis T, Fikadu Y, Lemma L. Perceived Stigma and Associated Factors Among HIV Positive Adult Patients Attending Antiretroviral Therapy Clinics at Public Facilities of Butajira Town, Southern Ethiopia, 2020. HIV/AIDS. 2020;12:717.
40. Turi E, Simegnew D, Fekadu G, et al. High Perceived Stigma Among People Living with HIV/AIDS in a Resource Limited Setting in Western Ethiopia: the Effect of Depression and Low Social Support. HIV/AIDS. 2021;13:389.
41. Ajong AB, Njotang PN, Nghoniji NE, et al. Quantification and factors associated with HIV-related stigma among persons living with HIV/AIDS on antiretroviral therapy at the HIV-day care unit of the Bamenda Regional Hospital, North West Region of Cameroon. Global Health. 2018;14(1):56. doi:10.1186/s12992-018-0374-5
42. Chukwuma C, Okeafor U. Perceived Stigma and Highly Active Antiretroviral Treatment Adherence among Persons Living with HIV/AIDS in the University of Port Harcourt Teaching Hospital. Orient J Med. 2017;29:12.;29:12.
43. Fido NN, Aman M, Brihnu Z. HIV stigma and associated factors among antiretroviral treatment clients in Jimma town, Southwest Ethiopia. HIV/AIDS. 2016;8:183.
44. Oke OO, Akinboro AO, Olanrewaju FO, Oke OA, Omololu AS. Assessment of HIV-related stigma and determinants among people living with HIV/AIDS in Abeokuta, Nigeria: a cross-sectional study. SAGE Open Med. 2019;7:2050312119869109. doi:10.1177/2050312119869109
45. Peltzer K, Pengpid S. Prevalence And Associated Factors Of Enacted, Internalized And Anticipated Stigma Among People Living With HIV In South Africa: results Of The First National Survey. HIV/AIDS (Auckland, N.Z.). 2019;11:275–285. doi:10.2147/HIV.S229285
46. Datta S, Bhattacherjee S, SherPa PL, Banik S. Perceived HIV related stigma among patients attending art center of a tertiary care center in rural West Bengal, India. J Clin Diagnostic Res. 2016;10(10):VC09. doi:10.7860/JCDR/2016/21366.8669
47. Li Z, Morano JP, Khoshnood K, Hsieh E, Sheng Y. HIV-related stigma among people living with HIV/AIDS in rural Central China. BMC Health Serv Res. 2018;18(1):453. doi:10.1186/s12913-018-3245-0
48. Lin YC, Dhaliwal JS, Kong AZH, Chan LG, Tan PLL. HIV-related stigma as perceived by HIV-positive individuals in Singapore. Int J HIV Related Problems. 2017;16(3):176–182.
49. Charles B, Jeyaseelan L, Pandian AK, Sam AE, Thenmozhi M, Jayaseelan V. Association between stigma, depression and quality of life of people living with HIV/AIDS (PLHA) in South India–a community based cross sectional study. BMC Public Health. 2012;12(1):463. doi:10.1186/1471-2458-12-463
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
