Back to Journals » International Journal of Women's Health » Volume 15
Perceived Childbirth Self-Efficacy and Its Associated Factors Among Pregnant Women in South-Central Ethiopia
Authors Gemeda Gudeta T , Benti Terefe A , Muhamed AN , Mengistu GT , Abebe Sori S
Received 31 May 2023
Accepted for publication 1 September 2023
Published 12 September 2023 Volume 2023:15 Pages 1431—1442
DOI https://doi.org/10.2147/IJWH.S423784
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Everett Magann
Tolesa Gemeda Gudeta,1 Ayana Benti Terefe,1 Ahmed Nuru Muhamed,1 Girma Teferi Mengistu,1 Seboka Abebe Sori2
1Department of Nursing, College of Medicine and Health Sciences, Wolkite University, Wolkite, Ethiopia; 2Department of Midwifery, College of Medicine and Health Sciences, Wolkite University, Wolkite, Ethiopia
Correspondence: Tolesa Gemeda Gudeta, Department of Nursing, College of Medicine and health Sciences, Wolkite University, P.O. Box 07, Wolkite, Ethiopia, Email [email protected]
Background: Childbirth self-efficacy has been identified as a significant indicator of a positive childbirth experience. It is, however, the most neglected aspect of maternal care, and evidence in this regard was lacking in Ethiopia. Therefore, this study aimed to assess perceived childbirth self-efficacy and its associated factors among pregnant women in the Gurage zone, southern Ethiopia.
Methods: The current study was conducted from April to May 2022 using a facility-based cross-sectional study design. We used a systematic sampling technique and selected a total of 423 women. To collect the data, we utilized an interviewer-administered questionnaire containing a childbirth self-efficacy inventory scale. Multiple linear regression analysis was employed to discover the factors influencing a woman’s self-efficacy during childbirth.
Results: The current study included 423 pregnant women in total. This study revealed that the overall mean score for perceived childbirth self-efficacy was 489.06 (SD = 65.77). Social support (β = 0.214, P< 0.001), psychological well-being (β = 0.254, P< 0.001), education status at the secondary level (β = 0.151, P< 0.001), no fundal pressure (β = 0.11, P = 0.010), and planned pregnancy (β = 0.10, P =0.013) were positively associated with childbirth self-efficacy. Fear of childbirth (β = 0.19, P< 0.001), Primipara women (β = 0.14, P< 0.001), women who had experienced discomfort during vaginal examination (β = 0.10, P = 0.009), and women who experienced the inability to push (β = 0.10, P = 0.013) were negatively associated with childbirth self-efficacy.
Conclusion: The overall mean score for the perceived childbirth self-efficacy was high when compared to the previous studies conducted in Australia. Healthcare professionals should create multifaceted strategies to support childbirth self-efficacy, such as relaxation techniques, prenatal psycho-education to reduce childbirth fear, enhance psychological well-being and encourage social support, particularly partner support during pregnancy and childbirth.
Keywords: childbirth, self-efficacy, pregnant women, support during pregnancy, fear of childbirth
Introduction
Childbirth is a potentially threatening life event due to the possibility of pain and the risk of injury or even death for both mother and child.1 This stressful life event of childbirth, which has no chance of recovery put pregnant women under fear of childbirth.2,3 Confidence in labour and birth, also known as childbirth self-efficacy, has been identified as an important marker of women’s coping abilities during labour.4 Self-efficacy refers to an individual’s confidence or belief in his/her own abilities to meet, overcome or control tasks successfully.5,6 Perceived childbirth self-efficacy (PCBSE), according to Bandura’s self-efficacy theory, relates to women’s perceptions of their cognitive readiness to manage labor and delivery.1,7 Efficacy expectancy and outcome expectancy make up self-efficacy. The term “outcome expectancy” describes the belief that completing a job will result in a particular outcome. On the other hand, efficiency expectancy is the person’s conviction that one carries out that behavior successfully in a specific situation.8
According to the existing global literature, the main modifiable risk factor influencing women’s coping, delivery experiences, and perinatal outcomes is perceived childbirth self-efficacy.1,9,10 Perceived childbirth self-efficacy affects the delivery mode.7,11 Confident women feel more in control during labor, have greater confidence in their abilities, and apply new skills to learn and cope with birth. Additionally, women who are confident experience contraction pain less adversely and less analgesic use which raises their satisfaction with both labor and delivery and leads to better perinatal outcomes.10,12 Contrarily, women with low PCBSE have higher rates of anxiety, depression, and perinatal morbidity risk factors, including more Post-traumatic stress disorder (PTSD) symptoms, loss of control during delivery, and anxiety.1,4,7,10 Generally, higher perceived childbirth self-efficacy is often associated with improved perinatal outcomes.10
Perceived childbirth self-efficacy (PCBSE) is affected by different factors. According to Lowe, PCBSE is affected by: (1) Performance accomplishments; (2) Vicarious experiences; (3) Verbal persuasion; and (4) Emotional arousal.8 Empirical evidence suggests that perceived childbirth self-efficacy is influenced by sociodemographic and obstetric factors such as maternal age, educational level, gestational weeks, whether one has had a previous cesarean section, parity, ethnicity, employment status, and whether one has had a previous miscarriage and pregnancy intention, fear of childbirth, and psychological well-being.4,6,13,14 Studies conducted by Drummond et al and Schwartz et al in Australia, revealed that the sum of mean scores were 443 and 402, respectively.4,9
However, there is a gap in the literature regarding negative performance accomplishments (difficulties in giving birth successfully) and the impact of social support (verbal persuasion), according to Lowe.1 Additionally, self-efficacy is a psychological category that can be associated with many sociocultural factors. The lack of studies examining perceived childbirth self-efficacy among pregnant women in Ethiopia presents another gap in the existing literature since the results of international studies may not be representative for Ethiopia. Therefore, this study aimed to assess perceived childbirth self-efficacy and its associated factors among pregnant women in the Gurage zone, southern Ethiopia.
Methods and Materials
Study Area and Period
The Gurage zone is one of the administrative zones found in the SNNPR of Ethiopia, and it has 13 woredas and two town administrations. The capital city of the Zone is Wolkite town, and Wolkite town is located 153 km southwest of Addis Ababa, the capital city of Ethiopia. Based on the 2007 census of the Central Statistical Agency of Ethiopia (CSA),15 the estimated population of Gurage Zone is 1,280,483. The zone has seventy-two health centers and seven hospitals. The study was conducted from April to May 2022.
Study Design and Population
A facility-based cross-sectional study was conducted in government hospitals in Gurage Zone from April to May 2022. All pregnant women attending Antenatal Care (ANC) services in all public hospitals constituted the source population, and all systematically selected pregnant women attending ANC services during the study period were the study population.
Eligibility Criteria
We included all pregnant women who were attending ANC services in all public hospitals in Gurage Zone and excluded those women who were unable to communicate with the interviewer or who were seriously ill.
Sample Size Determination and Sampling Procedure
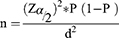
We calculated sample sizes using the formula for a single population proportion considering a confidence interval of 95% (Z = 1.96), a margin of error of 5% (d = 0.05), and a population proportion of 50% (P = 0.5) since there is no research on childbirth self-efficacy or factors related to childbirth self-efficacy in Ethiopia.
The final sample size was then 423 after the addition of a 10% non-response rate.
Since all government hospitals in the Gurage zone (Wolkite University Specialized Hospital, Attat Primary Hospital, Butajira General Hospital, Bui Primary Hospital, Agena Primary Hospital, Gunchire Primary Hospital, and Mahalamba Primary Hospital) included in this study, we proportionally allocated the final sample size to the seven hospitals based on the number of pregnant women who attended the ANC at each hospital two months before the actual data collection period. We employed a systematic sampling technique to select the study subjects in each hospital, and the sampling interval at each hospital was 2 (K=N/n: N was the source population at each hospital, and n was the sample size allocated for each hospital. We used a lottery method to select the first study subject to be interviewed in each hospital on the first day of data collection. After reviewing the eligibility criteria, we interviewed every other lady from each hospital.
Data Collection Tools and Procedure
In the present study, we used a pretested and structured questionnaire for data collection. The questionnaire consists of sociodemographic and obstetric factors, a childbirth attitudes questionnaire, social support questionnaire, World Health Organization Health Index (Five) questionnaire, Edinburgh Postnatal Depression Scale, and a Childbirth Self-Efficacy Inventory Scale.
Outcome Measurement
We measured the study’s primary outcome, PCBSE using the Childbirth Self-Efficacy Inventory (CBSEI). CBSEI has a 62-item scale requiring responses on a 10-point Likert scale, and it is a four-dimensional instrument. Its sum score ranges from 62 to 620, with higher scores indicating higher levels of childbirth self-efficacy.8 The Cronbach’s alpha for the CBSEI in this study is 0.95, and the CBSEI has been validated for use in Australian perinatal populations, with reported reliability coefficients of more than 0.909 for all four subscales.
Covariate Measurements
We used the Childbirth Attitudes Questionnaire (CAQ) to assess childbirth-related fears.1 The CAQ consists of 16 items and uses a four-point Likert response scale, and the CAQ sum scores range from 16 to 64, with higher scores reflecting higher levels of fear of childbirth. The reliability and validity of the CAQ were good in the previous study, which was about 0.92.16 In the present study, Cronbach’s alpha is 0.86.
The research team developed the Childbirth Problems Questionnaire that encompasses the most prevalent problems associated with childbirth after reviewing available literature.10,17 This questionnaire contains 12 items that measure the concerns or difficulties of mothers during labor and delivery. Each question in the questionnaire was answered with a “yes” or “no” answer.
The World Health Organization (Five) Well-Being Index (WHO-5) was used to assess psychological well-being.18 The WHO-5 consists of five items related to general well-being, well-being, and vitality, and it is a reliable and validated tool that has demonstrated good psychometric properties in pregnant women.19 Each item is rated on a six-point Likert scale, and the possible raw score ranges from 0 to 25, and the higher score expresses a better state of well-being. The reliability and validity of the WHO-5 were good in the previous study, which was about 0.89.16 In this study, Cronbach’s alpha is 0.75.
The 10-item Edinburgh Postnatal Depression Scale (EPDS) was employed to screen for possible antenatal and postnatal depression in the current study.20,21 Each question has four response options, and women choose one. Each item is scored from zero to three and summed to produce a total score. Possible total scores range from 0 to 30, with higher scores indicating more negative mood and risk of prenatal depression. An EPDS score >12 during the prenatal or postnatal period has been recommended as a possible indicator of depression but not a diagnosis of depression.22 This tool is valid and reliable in Ethiopia. Its Cronbach’s alpha is 0.88 in this study.
The Multidimensional Scale of Perceived Social Support (MSPSS) from family, friends, and significant others was used to assess perceived social support.23 The scale consists of 12 items rated on a seven-point Likert scale ranging from one (strongly disagree) to seven (strongly agree). The overall total score of the MSPSS ranges from twelve to eighty-four, with higher scores considered higher social support.24 In the present study, Cronbach’s alpha for the overall scale of the MSPSS is 0.85.
In the current study, the content validity of the questionnaires was checked by experts with several backgrounds (An assistant professor of maternity and reproductive health nursing, an epidemiologist, and a gynecologist). Seven Diploma and two MSC maternity health nurses who have experience in data collection and are fluent in English and local languages (Amharic and Guragigna) were recruited as data collectors and supervisors, respectively.
Data Quality Management
The following steps were taken to ensure the quality of the study: the questionnaire was developed in English, translated into Amharic, and then translated back to English by another person blind to the original questions to check the consistency. The questionnaire was adapted from a standardized data collection instrument and pretested on 21 (5%) of the sampled pregnant women following ANC at Wolkite Health Center. The reliability of the data collection instrument was assessed, the duration of data collection was calculated, and several changes were implemented, such as logical ordering and rewriting of difficult-to-understand components. Both data collectors and supervisors received two days of training (one-day theory and one day practical) on the purpose of the study, data collection methods and tools, how to approach respondents, and how to maintain confidentiality. At the end of each data collection day, the principal investigator and supervisors checked the questionnaires for completeness and consistency.
Data Processing and Analysis Approach
The data entry and analysis processes used Epi Data version 3.1 and SPSS version 26. In the current study, the Kolmogorov–Smirnov test was used to check the distribution of data for all continuous variables. Based on the characteristics of the independent variables, we used different analyzes to identify potentially significant factors. Accordingly, a one-sided sample independent t-test was employed to compare PCBSE between two groups, and an analysis of variance was used to compare PCBSE among three or more groups. To examine the relationship between PCBSE and non-normally distributed continuous variables, Spearman correlation coefficients were used. Multiple linear stepwise models were used to perform multivariate analyzes and identify factors associated with PCBSE. P values below 0.05 were considered statistically significant. The reliability of each scale used in the study was calculated.
Ethical Consideration
The Wolkite University College of Medicine and Health Sciences Ethics Review Committee approved this study under IRB approval number RCSUILC/018/2022. Both the Declaration of Helsinki and the rules of the College of Medicine and Health Sciences of Wolkite University were followed during the study. We obtained written informed consent from all participants involved in the study.
Results
Sociodemographic Characteristics of the Participants
Altogether, four hundred twenty-three pregnant women participated in the current study. The result of the Kolmogorov–Smirnov test demonstrated that the distribution of data regarding maternal age is not normal (Z = −2.5, P 0.05). In the present study, the median age of the study participant was 27 years (IQR = 24~31). Regarding the marital status of the study subjects, almost all participants (95.7%) were married. Concerning educational and pregnancy status, sixty-two percent (62.6%) of the participants had completed secondary education or higher, and more than a quarter of the pregnancies were unplanned (Table 1).
 |
Table 1 Socio-demographic and Obstetric Characteristics of Pregnant Women in Gurage Zone, Ethiopia, 2022 (N = 423) |
Description of PCBSE of the Pregnant Woman in Gurage Zone
Table 2 displays the study participants’ PCBSE results. The distribution of PCBSE scores appears to be normal, according to the result of the Kolmogorov–Smirnov test (Z = 1.02, P> 0.05). The mean score for each item was 8.03 (SD = 1.06) at the time of the survey, and the participants’ average perceived childbirth self-efficacy score was 489.06 (SD = 65.77).
 |
Table 2 Descriptive Statistics for Perceived Childbirth Self-Efficacy Scale Score of Pregnant Women in Gurage Zone, Ethiopia, 2022 (N = 423) |
Explanatory Variables Related to PCBSE
Table 3 displays the associations between demographic, obstetric, and PCBSE data. The results found that the mother’s age (P = 0.001), occupational status of the mother (P = 0.007), mother’s parity (P=0.032), previous cesarean section (P = 0.04), and pregnancy status (P<0.001) had a significant association with PCBSE.
 |
Table 3 Univariate Relationships Between Demographic, Obstetric Characteristics, and PCBSE Score Among Pregnant Women in Gurage Zone, Ethiopia, 2022 (N = 423) |
Childbirth Problems
The descriptive statistics for birthing problems and their univariate relationships with perceived childbirth self-efficacy are shown in Table 4. The results of this study depicted that 24.6% of the participants experienced the inability to cope with labor, birth pains, and fundal pressure. In the current study, 14.9% of mothers reported feeling embarrassed when a male caregiver conducted a vaginal examination. One in four study participants (25.3%) reported poor communication with the care provider, and 36.6% reported spousal/partner support during labor and delivery. The univariate analysis shows that four of these childbirth problems had a significant association with CBSE. Specifically, these problems included augmentation/Induction of Labour (P = 0.01), inability to cope with labor and birth pains (P = 0.033), fundal pressure (P = 0.002), and experience discomfort during vaginal examination (P<0.001) (Table 4).
 |
Table 4 Univariate Analysis of Childbirth-Related Problems Against PCBSE Score Among Pregnant Women in Gurage Zone, Ethiopia, 2022 (N = 423) |
Other Covariates
We employed median and interquartile ranges to analyze data for fear of childbirth, mental health, Edinburgh postnatal depression, and social support because the results of the Kolmogorov–Smirnov test (P < 0.05) indicated non-normality of the data for these variables. Social support scores averaged 52 at the time of the study, indicating that participants typically thought they had a moderate level of social support. The median EDPS score was 7, which was below the threshold for prenatal depression. Different factors were shown to be significantly correlated with the perceived childbirth self-efficacy by the research. In particular, maternal social support (P< 0.001) and mental health (P<0.001) had significant positive correlations with PCBSE. At the same time, the results show fear of childbirth (P< 0.001) had a significant negative relationship with PCBSE (Table 5).
 |
Table 5 Correlations for Some Independent Variables Not Normally Distributed Against PCBSE Score Among Pregnant Women in Gurage Zone, Ethiopia, 2022 (N = 423) |
Factors Associated with PCBSE Among Pregnant Women in Gurage Zone
Stepwise multiple linear regressions show that nine variables explain 36.8% of the variation in pregnant women’s self-efficacy for giving birth in the Gurage zone. Social support (β = 0.214, P< 0.001), psychological well-being (β = 0.254, P< 0.001), education status ≥ Secondary level (β = 0.151, P< 0.001), no fundal pressure (β = 0.11, P = 0.010), and planned pregnancy (β = 0.10, P =0.013) were positively associated with PCBSE. In contrast, fear of childbirth (β = −0.19, P< 0.001), Primipara women (β = −0.14, P< 0.001), women who had experienced discomfort during vaginal examination (β = −0.10, P = 0.009), and women who experienced the inability to push (β = −0.10, P = 0.013) were negatively associated with PCBSE (Table 6).
 |
Table 6 Multivariable Linear Regression Results Showing Factors Associated with PCBSE Among Pregnant Women in Gurage Zone, Ethiopia, 2022 (N = 423) |
Discussion
This study examined perceived childbirth self-efficacy (PCBSE) and its associated factors among pregnant mothers in the Gurage zone. To the best of our knowledge, this study is the first to assess PCBSE and factors affecting it in the Gurage zone, even though earlier research has examined topics in developed countries but not in Africa and specifically in Ethiopia. Therefore, the result of the current study may assist healthcare professionals in identifying pregnant women who have poor PCBSE and may be at risk for adverse perinatal outcomes. It may also provide potential areas for improvement for researchers and practitioners looking to improve PCBSE among expectant mothers in the Gurage zone.
Participants in this study received an average PCBSE score of 489.06, with an average item score of 8.03. This result is higher when compared to the research conducted by Drummond et al and Schwartz et al in Australia, where the sum of mean scores were 443 and 402, respectively.4,9 The result of the current study is also higher than the study conducted by Kathleen et al25 and Shaw et al,26 in which the sum mean score was 228.94 and 421.38.25,26 This discrepancy may result from sociocultural and data collection methods used in Australian research that used a self-administered technique. Additionally, this discrepancy is explained by the relatively large number of multipara women in this study compared with the Australian study,9 and primipara is a risk factor for lower PCBSE in this study and prior investigations, and the studies by Kathleen et al25 and Shaw et al,26 were exclusively performed on purposefully selected Primipara women. However, the findings of this study were consistent with the study by Lowe when the first testing of the CBSEI measure was done.8
The study’s other empirical finding was that, in comparison to multiparous women, nulliparous women exhibited lower self-efficacy in childbirth. This result is congruent with the investigation of Schwartz et al,4 Soh et al,16 and Tilden et al10 in which multiparous women demonstrated a higher childbirth self-efficacy score than nulliparous women. Additionally, this conclusion is consistent with Bandura’s self-efficacy theory, which states that the firsthand experience of childbirth in the past would be a powerful source of knowledge that could influence mothers’ perceptions of their own efficacy beliefs.5 This finding thus emphasizes the significance of parity-specific childbirth self-efficacy interventions that aim to increase pregnant women’s PCBSE.
The results of the current study additionally indicate that social support from significant others and PCBSE in pregnant Ethiopian women are strongly positively correlated. Although few studies have examined the impact of social support on birthing self-efficacy globally in the past, this finding aligns with the study of Schwartz et al,4 which stated when compared to first-time mothers, multiparous women reported lower self-efficacy levels for birthing when partner support was unavailable. This supports the research of Copstick and Lowe, which confirms that verbal persuasion from family members, especially close relatives and especially the birth partner, further influences the birth process.8,27 Also, women who have partner support throughout labor tend to seek fewer medications and have more positive thoughts about birth than women who try to manage alone because friends are their closest and most important social network.28
The empirical findings of this study also reveal that women with high levels of pregnancy fear had low self-efficacy. This finding is consistent with previous studies13,29 in which fearful women had lower perceived childbirth self-efficacy results than their counterparts. The possible explanation for this might be according to Bandura’s self-efficacy theory; emotional arousal is one of the sources of perceived self-efficacy,5 and significantly lower self-efficacy is associated with perceived high childbirth fear.30,31 Thus, it has been discovered that reducing women’s childbirth fear through midwifery psycho-education considerably increases their confidence during delivery.32
The empirical findings of this study also reveal that, compared to women who had positive birthing experiences, those who had negative ones had much lower PCBSE scores. Lower PCBSE was strongly associated with three childbirth problem characteristics, including discomfort during the vaginal examination, inability to push, and fundal pressure in the current study. Although there have been few studies that have specifically examined the role of negative childbirth experiences in PCBSE, these results are consistent with a study conducted by Slade et al33 found that women who had positive prior experiences were more likely to report having positive childbirth experience and to have higher self-efficacy for the impending birth; on the other hand, women who had negative prior experiences and felt they handled childbirth poorly were more likely to have lower self-efficacy for the impending birth.33 Self-efficacy increases when past experiences are positive, but self-efficacy tends to fall when past experiences are negative.5
The current study showed that women with good psychological well-being are more likely to have higher levels of childbirth self-efficacy. This result is consistent with previous research,16,34 which showed higher CBSE in women with good psychological health. According to self-efficacy theory, positive emotions can increase confidence and improve childbirth self-efficacy, which could be one explanation for this finding. Women’s self-efficacy in birthing increased when they felt confident in their abilities to achieve desired goals through their actions, which was associated with positive moods.5 Another explanation is that women with high psychological well-being were shown to have positive interpersonal relationships and human functions, making them more likely to experience social support from their spouses, family, and friends.6
Finally, a high school education or higher was linked in this study to increased PCBSE. This finding is consistent with that of Larsen et al35 and Slade et al,36 who found that PCBSE increased with increasing educational status. The possible justification for this finding might be the financial stability and privilege that comes with having a higher education could theoretically boost a woman’s confidence in her ability to give birth. Also, planned pregnancy status contributes to higher PCSE in this study. This finding contradicts the study conducted in China in which pregnancy status was not determinant of CBSE.16 These contradictory conclusions may be due to differences in the sociocultural characteristics of the participants. Further research is needed to understand the relationship between pregnancy status and perceived childbirth self-efficacy.
Strength and Limitations
The use of reliable instruments to measure perceived childbirth self-efficacy is the study’s strength. There are some drawbacks to this study. Role modeling effects, which Lowe identifies as a component of vicarious experience, were not included in this study and should be investigated further. Given that childbirth self-efficacy may alter throughout pregnancy and that this study used a cross-sectional methodology (evaluation of PCBSE was collected at a single moment in time), a longitudinal study is necessary to investigate causal relationships in the future. To identify mothers who are at high risk of low PCBSE at various stages of the antepartum period and to create effective interventions to improve PCBSE in Ethiopia, additional research is required to examine the full range of determinants of perceived childbirth self-efficacy and their temporal and causal associations to perceived childbirth self-efficacy.
Conclusion
The overall mean scores of perceived childbirth self-efficacy in the current were higher compared to the previous studies conducted in Australia. Our study discovered a strong connection between social support, psychological health, education level, childbirth problems, pregnancy status, childbirth fear, parity, and perceived childbirth self-efficacy. Healthcare professionals and researchers should develop comprehensive strategies to improve perceived childbirth self-efficacy, such as relaxation strategies and psycho-education throughout pregnancy, to reduce fears about childbirth and improve psychological health. Comprehensive prenatal social support and parity-based childbirth self-efficacy therapies are needed to increase perinatal self-efficacy. The findings of our study also imply that to improve perceived childbirth self-efficacy, healthcare providers should assist women in resolving common birthing problems such as discomfort during vaginal examination and difficulty pushing.
Abbreviations
ANC, Antenatal Care; CSA, Central Statistical Agency of Ethiopia; CAQ, Childbirth Attitudes Questionnaire; CBSE, Childbirth self-efficacy; CBSEI, Childbirth self-efficacy inventory; EPDS, PCBSE, Perceived Childbirth self-efficacy; Edinburgh Postnatal Depression Scale; PTSD, Post-traumatic stress disorder; SNNPR, Southern Nation Nationalities, and Peoples’ Region; WHO, World Health Organization; WHO5, World Health Organization (Five) Well-Being Index.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research did not receive any grant from any funding agencies.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Lowe NK. Self-efficacy for labor and childbirth fears in nulliparous pregnant women. J Psychosom Obstet Gynaecol. 2000;21(4):219–224. doi:10.3109/01674820009085591
2. Kabale WD, Bekele GG, Roga EY, et al. Perceived stress and associated factors among pregnant women in western Ethiopia: community based cross-sectional study, 2021. J Obstet Gynaecol. 2023;7:3.
3. Kohlhepp L, Hollerich G, Vo L, et al. Physiological changes during pregnancy. Der Anaesthesist. 2018;67:383–396. doi:10.1007/s00101-018-0437-2
4. Schwartz L, Toohill J, Creedy DK, et al. Factors associated with childbirth self-efficacy in Australian childbearing women. BMC Pregnancy Childbirth. 2015;15(1):1–9. doi:10.1186/s12884-015-0465-8
5. Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191. doi:10.1037/0033-295X.84.2.191
6. Yuksel A, Bayrakci H. Self-efficacy, psychological well-being and perceived social support levels in pregnant women. Int J Caring Sci. 2019;12(2):1–10.
7. Gourounti K, Kouklaki E, Lykeridou K. Validation of the Childbirth Attitudes Questionnaire in Greek and psychosocial characteristics of pregnant women with fear of childbirth. Women Birth. 2015;28(3):e44–e51. doi:10.1016/j.wombi.2015.02.004
8. Lowe NK. Maternal confidence for labor: development of the childbirth self‐efficacy inventory. Res Nurs Health. 1993;16(2):141–149. doi:10.1002/nur.4770160209
9. Drummond J, Rickwood D. Childbirth confidence: validating the childbirth self‐efficacy inventory (CBSEI) in an Australian sample. J Adv Nurs. 1997;26(3):613–622. doi:10.1046/j.1365-2648.1997.t01-24-00999.x
10. Tilden EL, Caughey AB, Lee CS, et al. The effect of childbirth self-efficacy on perinatal outcomes. J Obstet Gynecol Neonatal Nurs. 2016;45(4):465–480. doi:10.1016/j.jogn.2016.06.003
11. Zhang Z, Gu C, Zhu X, et al. Factors associated with Chinese nulliparous women’s choices of mode of delivery: a longitudinal study. Midwifery. 2018;62:42–48. doi:10.1016/j.midw.2018.03.013
12. Sánchez-Cunqueiro MJ, Comeche MI, Docampo D. On the relation of self-efficacy and coping with the experience of childbirth. J Nurs Educ Pract. 2018;8(6):48. doi:10.5430/jnep.v8n6p48
13. Salomonsson B, Berterö C, Alehagen S. Self‐efficacy in pregnant women with severe fear of childbirth. J Obstet Gynecol Neonatal Nurs. 2013;42(2):191–202. doi:10.1111/1552-6909.12024
14. Chen S-W, Hutchinson AM, Nagle C, et al. Women’s decision-making processes and the influences on their mode of birth following a previous caesarean section in Taiwan: a qualitative study. BMC Pregnancy Childbirth. 2018;18:1–13. doi:10.1186/s12884-018-1661-0
15. CSA. 2007 Population and housing census of Ethiopia: administrative report. Addis Ababa, Ethiopia: Statistical Authority; 2012.
16. Soh YX, Razak NKBA, Cheng LJ, et al. Determinants of childbirth self-efficacy among multi-ethnic pregnant women in Singapore: a structural equation modelling approach. Midwifery. 2020;87:102716. doi:10.1016/j.midw.2020.102716
17. Aktaş S, Aydın R. The analysis of negative birth experiences of mothers: a qualitative study. J Reprod Infant Psychol. 2019;37(2):176–192. doi:10.1080/02646838.2018.1540863
18. World Health Organization. Wellbeing measures in primary health care/the DepCare Project: report on a WHO meeting. Stockholm, Sweden: World Health Organization. Regional Office for Europe; 1998.
19. Mortazavi F, Mousavi SA, Chaman R, et al. Validation of the world health organization-5 well-being index; assessment of maternal well-being and its associated factors. Turk Psikiyatri Derg. 2015;26(1):48–55.
20. Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression: development of the 10-item Edinburgh postnatal depression scale. Br J Psychiatry. 1987;150(6):782–786. doi:10.1192/bjp.150.6.782
21. Murray D, Cox JL. Screening for depression during pregnancy with the Edinburgh Depression Scale (EDDS). J Reprod Infant Psychol. 1990;8(2):99–107. doi:10.1080/02646839008403615
22. Beyondblue. Clinical practice guidelines for depression and related disorders – anxiety, bipolar disorder and puerperal psychosis – in the perinatal period. A guideline for primary care health professionals. Melbourne: beyondblue: the national depression initiative; 2011.
23. Zimet GD, Powell SS, Farley GK, et al. Psychometric characteristics of the multidimensional scale of perceived social support. J Pers Assess. 1990;55(3–4):610–617.
24. Jalal M, Dolatian M, Mahmoodi Z, et al. The relationship between psychological factors and maternal social support to breastfeeding process. Electron Physician. 2017;9(1):3561. doi:10.19082/3561
25. Beebe KR, Lee KA, Carrieri‐Kohlman V, et al. The effects of childbirth self‐efficacy and anxiety during pregnancy on prehospitalization labor. J Obstet Gynecol Neonatal Nurs. 2007;36(5):410–418. doi:10.1111/j.1552-6909.2007.00170.x
26. Berentson‐Shaw J, Scott KM, Jose PE. Do self‐efficacy beliefs predict the primiparous labour and birth experience? A longitudinal study. J Reprod Infant Psychol. 2009;27(4):357–373. doi:10.1080/02646830903190888
27. Copstick S, Taylor KE, Hayes R, et al. Partner support and the use of coping techniques in labour. J Psychosom Res. 1986;30(4):497–503. doi:10.1016/0022-3999(86)90089-9
28. Broome ME, Koehler C. Childbirth education: a review of effects on the woman and her family. Fam Community Health. 1986;9(1):33–44. doi:10.1097/00003727-198605000-00006
29. Lazolglu M, Apay SE. Does fear of giving birth impact the self-efficacy perceptions of a pregnant woman? East J Med Sci. 2018;2018:70–75.
30. Lowe NK. Maternal confidence in coping with labor a self‐efficacy concept. J Obstet Gynecol Neonatal Nurs. 1991;20(6):457–463. doi:10.1111/j.1552-6909.1991.tb01711.x
31. Salomonsson B, Gullberg MT, Alehagen S, et al. Self-efficacy beliefs and fear of childbirth in nulliparous women. J Psychosom Obstet Gynaecol. 2013;34(3):116–121. doi:10.3109/0167482X.2013.824418
32. Toohill J, Fenwick J, Gamble J, et al. A randomized controlled trial of a psycho‐education intervention by midwives in reducing childbirth fear in pregnant women. Birth. 2014;41(4):384–394. doi:10.1111/birt.12136
33. Slade P, MacPherson SA, Hume A, et al. Expectations, experiences and satisfaction with labour. Br J Clin Psychol. 1993;32(4):469–483. doi:10.1111/j.2044-8260.1993.tb01083.x
34. Taghizdeh Z, Ebadi A, Dehghani M, et al. A time for psycho-spiritual transcendence: the experiences of Iranian women of pain during childbirth. Women Birth. 2017;30(6):491–496. doi:10.1016/j.wombi.2017.04.010
35. Larsen K, O’Hara MW, Brewer KK, et al. A prospective study of self-efficacy expectancies and labour pain. J Reprod Infant Psychol. 2001;19(3):203–214. doi:10.1080/02646830125493
36. Slade P, Escott D, Spiby H, et al. Antenatal predictors and use of coping strategies in labour. Psychol Health. 2000;15(4):555–569. doi:10.1080/08870440008402013
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.