Back to Journals » Clinical Ophthalmology » Volume 17
Pediatric Eye Care Treatment Rates and Community Compliance to a Spectacle Provision Program in an Underserved School District in San Diego, CA
Authors Rohn MCH, O'Sullivan F, Brown SI, Hernandez E, Borooah S, Molina I
Received 17 February 2023
Accepted for publication 30 May 2023
Published 19 June 2023 Volume 2023:17 Pages 1729—1737
DOI https://doi.org/10.2147/OPTH.S409075
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Matthew CH Rohn,1 Flynn O’Sullivan,2 Stuart I Brown,2 Eric Hernandez,2 Shyamanga Borooah,2 Iliana Molina2
1Sidney Kimmel Medical College, Thomas Jefferson University, Philadelphia, PA, USA; 2Department of Ophthalmology, Shiley Eye Institute, School of Medicine, University of California-San Diego, La Jolla, CA, USA
Correspondence: Iliana Molina, Shiley Eye Institute, 9415 Campus Point Dr, La Jolla, CA, 92093-0946, USA, Tel +1 858 822 2585, Fax +1 858 822 1754, Email [email protected]
Significance: The need for early identification and treatment of young children’s refractive error needs has become a public health concern. The UCSD Eyemobile for Children (EyeMobile) provides vision screenings and comprehensive eye exams on the Eyemobile among a population of underserved, predominantly Hispanic preschool and elementary school children. The program also provides spectacles for children who fail eye exams due to refractive error.
Methods: We performed a retrospective cross-sectional analysis of all children screened from 2011 to 2017 by the Eyemobile across 10 San Diego elementary schools. We examined demographics, distance and near visual acuity, autorefraction, stereopsis, and color vision. To measure compliance to our spectacle program, we checked if children who were prescribed spectacles were wearing them, as instructed, at the following year’s screening. Differences between compliance measures with respect to school, age, ethnicity, and gender were determined using chi-square analysis, while all other measures were fit to a binary logistic regression to determine statistically significant factors.
Results: A total of 12,176 elementary school children were screened between 2011 and 2017. Of these children, 5269 (43.3%) were referred for a comprehensive eye examination. Across six years, 3163 (60.0%) of the children referred completed their eye examinations. There was a significant increase (p < 0.001) in exam completion in the successive years. Exam completion was significantly higher in ten-year-olds (p = 0.0278) and in 3 of the 10 schools (p < 0.0001, p = 0.0027, and p = 0.0309). A total of 1089 (8.9% of screened) children were prescribed spectacles. Of the 409 children that were recorded with the compliance method, 342 (83.6%) were found to be fully compliant and wearing their spectacles as prescribed.
Conclusion: The Eyemobile program demonstrated high levels of compliance for both eye examination completion and prescribed spectacle wear in underserved populations in the San Diego region, compared to similar national programs.
Keywords: refractive error, children, free spectacles, Eyemobile, compliance
A Letter to the Editor has been published for this article.
Introduction
Refractive error (RE) is the leading cause of all vision impairment worldwide.1,2 In many cases, this refractive error goes uncorrected and is among the leading causes of reversible blindness. In the United States, it is estimated that half the population has clinically significant refractive error,3 the majority of whom (80.9–85.8%) have been shown to achieve significantly better visual acuity following spectacle correction.3 Although the prevalence of refractive error is lower in children,4,5 the lifelong impact of untreated refractive error in this age group is more significant due to the risk of amblyopia6 refractive error, leading to irreversible deficits in visuocognitive and visuomotor measures,7 which in turn have a profound effect on a child’s overall development, and in particular educational and psychosocial development. Studies of refractive error in children have shown a higher proportion of error in low and middle-income countries.8 The social and economic consequences of refractive error in children consist of limiting educational and employment opportunities.9 As a result, early diagnosis, prompt and facilitated access to care, tailored management and good compliance with prescribed refractive correction are all essential factors to achieve successful visual outcome in children with uncorrected refractive error.
It has been reported that ethnic minority groups and individuals in underserved communities are less likely to have access to or accept treatment for refractive error.1,10 Therefore, children in these groups represent one of the most vulnerable populations with respect to uncorrected refractive error.9,11,12 Studies measuring the degree of compliance for refractive error treatment among children in multiethnic, underserved communities, have reported unsatisfactory levels of compliance, ranging from 13% to 58%, with a follow-up period of 5 weeks to 18 months.13–16
The University of California San Diego (UCSD) Eyemobile program (Eyemobile) is a school-based spectacle provision program that started providing services in 2000 and is exclusively funded through grants and donations. The program performs vision screenings, comprehensive dilated eye exams, and specialist eye care, when necessary, for underserved children in San Diego County, CA. Underserved students were those who attended school and resided in a priority zip code. Priority zip codes refer to those in which a certain percentage of the population earned income less than 200% of the federal poverty level.
Eyemobile currently serves 245 school sites throughout San Diego County, with a predominantly Latino population. In 2011, a grant was received from Price Charities to bring services to elementary school children in a particularly underserved community, the Hoover Cluster of the San Diego Unified School District. This community, in the City Heights area, represents one of San Diego County’s most vulnerable communities and is made up of 34% foreign-born immigrants, only 55% of whom have some degree of health insurance.17 The Hoover Cluster consists of 10 schools, representing a population that has 97% students of color and where students are twice as likely to drop out of high school as their peers, district-wide.17 Fifty-seven percent of children in this area live in poverty with a family income of less than 150% of the poverty line.18
In the present study, we aimed to investigate the factors leading to eye care compliance in children attending schools located in the Hoover Cluster of the San Diego Unified School District in San Diego, CA, USA. We investigated the compliance of children with spectacles prescribed by asking caregivers to monitor their use. We also analyzed the effectiveness of the Eyemobile in addressing important barriers to treating refractive error in children in underserved areas by focusing on access to care.
Methods
Screening
This study was approved by the UCSD Human Research Protection Program institutional review board (#121689) and adhered to the tenets of the Declaration of Helsinki. Data from children within the 10 elementary schools of the Hoover Cluster of the San Diego Unified School District were analyzed. Screening and spectacle provision for preschoolers at these schools began in 2000. In 2011, screenings were added for kindergarten, 3rd and 5th grades. Children screened in Pre-K were referred with guidelines established by Donahue et al.19 For older children, the criteria utilized was set by the American Association for Pediatric Ophthalmology and Strabismus.20 Screening was conducted in the classrooms of these schools by trained, experienced screeners under ambient lighting using a retinal autorefractor (RAR; Retinomax K-plus 3, Lombart Instrument). This handheld autorefractor device is more efficient and accurate than its counterparts and is able to determine astigmatism more effectively than a visual acuity chart. Children who failed the screening criteria (Table 1) and were not already under the care of an eye specialist were referred for a comprehensive optometric examination conducted by an Eyemobile optometrist.
 |
Table 1 Referral Criteria |
Post-Screening Comprehensive Exam
All parents of children who failed screening were given information about their child’s vision and the reasons for screen failure, as well as general information regarding their child’s eye care. Parents were provided with an informed consent form for a no cost eye exam conducted by the optometrists on board the Eyemobile. Eyemobile staff coordinated with school staff and scheduled a day the Eyemobile could return to the school and set up appointments. Parents who signed the consent form were asked to come to the school location and attend the eye exam. Children with parents who were not able to attend were often accompanied by a school nurse or designated caregiver. The examination included visual acuity, pupil reactivity, ocular motility and cover testing, eye preference test, Titmus stereopsis, anterior segment evaluation via slit lamp, cycloplegic refraction, and fundus examination. Cycloplegia was achieved using one drop of phenylephrine (2.5%) and one drop of tropicamide (1%).21 Cycloplegic refraction was carried out 30 minutes after administration of drops.
When prescribed, spectacles were provided to the children and families free of charge. Parents of children who received spectacles were called approximately 4–6 weeks after the prescription was received to inquire about possible problems and urge spectacle wear. All parents of the children who received spectacles were advised to follow up with eye care professionals after one year. Children suspected of having amblyopia were referred to specialists for medical care. If a child did not have insurance, they were referred to a pediatric ophthalmologist at the Ratner Children’s Eye Center at Shiley Eye Institute.
Compliance Analysis
The overall compliance data was drawn from the children examined between 2011 and 2017. We analyzed the percentage of children who failed screening, were referred for an optometric examination, and completed the optometric examination. This was used as a measure of school/parental compliance, and differences with respect to school year, individual school, age, gender, and ethnicity were examined.
We first investigated the number of children who had received their first spectacle prescription from the Eyemobile and were screened again between 2011 and 2017. If a child wore their spectacles as prescribed at their next school screening (between 1 and 5 years after the initial exam), they were considered compliant, and otherwise they were deemed a compliance failure. Except in cases where the child had sought private care, the spectacles were the same prescription, style, and frame as was prescribed by the Eyemobile. This measure was modeled on several previously published studies that analyzed the effectiveness of similar interventions prescribing spectacles to children.13–16 The number of years of spectacle wear compliance was also recorded. Children who had received their initial prescription from the Eyemobile and had received follow-up care from a private provider were also considered compliant and recorded.
Differences between the above compliance measures with respect to school, age, ethnicity, and gender were determined using chi-square analysis, while all other measures were fit to a binary logistic regression. All statistical tests were performed using Python version 3.9.5.
Results
In total, 12,176 children were screened between 2011 and 2017. Of these children, 5269 (43.3%) failed screening and were referred for an examination of the Eyemobile. The demographic data of the referred children are summarized in Table 2. Overall, 3163 children (60.0% of those referred, 26.0% of total screened) were examined on the Eyemobile. Of those examined on the Eyemobile, 1089 (34.4% of those examined, 8.9% of total screened) received spectacles.
 |
Table 2 Demographic Data |
There was an increase in the proportion of children who attended examinations after being referred (exam completion rate) across successive years. In the first year (2011–2012), the percentage was 36% (642). From 2014 onwards, the exam completion rate remained above 70%, ending at 77.3% (627) in the 2016–2017 year.
The only statistically significant differences in exam completion rate based on age were that 9-year-olds were less likely to complete an exam after being referred and 10-year-olds were more likely (p = 0.0485 and p = 0.0278, respectively). The exam completion rates, based on age and average, are shown in Figure 1. The reason the completion rate of 4-year-olds was not statistically significant is that only 28 4-year-olds were used in the sample—more data would be needed about younger children to measure how their exam completion rates compare with older children.
 |
Figure 1 Exam completion rate based on age after referral. Statistically significant rates are shown in darker blue and the average rate across all ages is shown with a red line. |
Three of the ten schools demonstrated a significantly higher overall percentage of referred children who completed an exam (72.08%, 72.16%, and 68.51%; p < 0.0001, p = 0.0027, and p = 0.0309, respectively) compared to the mean across all ten schools. The exam completion rates for all the schools are shown in Figure 2.
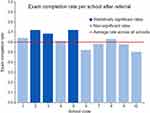 |
Figure 2 Exam completion rate based on school after referral. Statistically significant rates are shown in darker blue and the average rate across all schools is shown with a red line. |
We found no significant differences in age, gender, or ethnicity in which patients had a higher exam completion rate. We did not perform an economic analysis.
Of the children screened between 2011 and 2017 who received spectacles from the Eyemobile, 409 (37.6%) were measured for compliance at their school’s next screening. Of the 409 children, 342 (83.6%) were found to be compliant with wearing their prescribed spectacles. The number of years of compliance for those who wore their spectacles as prescribed is shown in Table 3. Children’s gender did not have a statistically significant effect on spectacle wear.
 |
Table 3 Spectacle Wear at Follow Up |
The sex of children, years of spectacle wear, school, successive school years, diagnosis of hyperopia vs myopia, presence of astigmatism, and age did not have a statistically significant effect on spectacle wear (Table 4). It should be noted that 395 children were in the 5th grade at the time of prescription, so were not screened the following year and thus could not be included in this method of measuring compliance.
 |
Table 4 Logistic Regression Model of Predictors of Spectacles Wear |
Overall, 118 (28.9%) of the children who were seen at a follow-up exam eventually pursued eye care from an outside private eye care provider in their community. More years of spectacle wear resulted in a significantly greater number of children pursuing private eye care (p < 0.001). Older children were more likely to pursue private eye care (p < 0.001). Additionally, children attending three of the ten schools were significantly more likely (p = 0.016, p = 0.038, and p = 0.042) to pursue private eye care. No statistically significant effects were observed with respect to sex, ethnicity, and diagnosis of hyperopia, myopia, or astigmatism.
To better understand the factors that may have played a part in poor compliance, 102 parents of children in the final year of data collection (2016–2017) were called via telephone 4–6 weeks after spectacle prescription was received. Of the 54 parents (52.94%) who were successfully contacted, 50 (92.6%) reported their children “wearing spectacles and liked them”. Two (3.7%) of these children reported their spectacles lost or broken, two (3.7%) reported not wearing them without reason. Forty-eight (47.1%) of the families called could not be reached by phone.
Discussion
The results of this study demonstrated that the Eyemobile had a high level of successful examination completion for those referred for refractive error in the ten schools investigated. This program was similar to other programs in the country. In a retrospective 12-year study in deprived areas of Cleveland, Ohio, 5355 children (8.39%) qualified for free spectacles.22 UCSD’s Shiley Eyemobile gave free spectacles to 8.94% of the children who were originally screened. This figure is on par with the Cleveland study and shows that the Eyemobile program is as effective at providing free spectacles as its counterparts. Since 2011, the program showed increasing levels of examination completion, reaching levels higher than have been previously reported in other similar programs.14,15,22 The rate of exam completion began at 27.8% for the first year and gradually increased to more than three quarters in the last three years.
We believe that the increasing examination completion may be the result of the combined effect of the longevity of our program (6 years versus up to 18 months in similar programs), the mentioned educational initiatives to both the parents and school staff, as well as the increasing approval and trust this program has had in the families of the community. It is vital to clarify that the effect of the longevity of the UCSD Eyemobile program was not studied, but that it would be a topic of future interest when comparing other schools within our program. Anecdotally, this trust grew over the duration of our study, leading to more active involvement of nurses and teachers in our program and producing better outcomes. In the first year of the program, both teachers and nurses complained of class disruption during screening or examination appointments. However, this changed in the second year and beyond, as teachers and nurses began to participate willingly. This participation included calling families to urge them to attend exams and personally deliver the prescribed spectacles to parents after school pickup. Consequently, we believe that the program would not be successful without traction from various stakeholders, including teachers, nurses, and parents.
For example, the positive effect of nurse involvement was supported by the increased levels of exam completion observed at the schools that employed consistent nursing care. While the other schools relied on a rotating group of nurses who, as a consequence of their rotation, had less or no contact with our program, the nurses at these two schools (full-time and part-time) were more constant and set time aside to personally call parents to remind parents/caregivers to attend examinations with their children. This impact of full-time nurses on exam completion rates is supported by the literature, specifically Rodriguez et al which observed a 96% follow-up rate in schools with full-time nurses and a 67% rate in schools with a rotating nurse staff.23 Differences between children played no significant role in the completion rates. Children attending these same schools were also more likely to pursue private eye care, perhaps indicating that the parents were influenced by the nurses at these schools. Socio-economic analysis was not performed on the families of children attending these schools.
The levels of compliance observed in grades 3 to 6 were higher than similar studies, but the levels of pre-K compliance were lower when compared to a similar program for only pre-K at the University of California Los Angeles (UCLA) using the same model that reported an exam completion rate of 65%.14 This again is likely due to the time to establish the program in the schools. Furthermore, it would be interesting to return to the same schools and review the pre-K compliance rates to see if they have now increased.
The overall rate of spectacle-wear in this study (83.6%) was also higher than that of comparable studies (13–58%), representing further evidence of the success of the Eyemobile.10,24,25 Additionally, it was observed that the number of years between spectacle prescription and follow-up did not have a significant effect on spectacle wear, suggesting that compliant children continued to wear their spectacles over extended periods of time. However, unlike the rates of exam completion, levels of spectacle wear were consistent throughout the study. We speculate that this may be related to an obvious improvement in vision and the impact on both children and their families, causing families and children alike to be more motivated towards consistent spectacle wear. In addition, to receive spectacles, children and their parents must complete the various steps of our program, including screening day procedures, appointment scheduling, consent form preparation, and educational information on exam completion. Therefore, it is possible that children and families who completed these necessary stages were both more available and more aware of the value of vision care for their children.
Although this study has identified possible relevant contributors to compliance with treatment for refractive error, it has some limitations with respect to follow-up. Our program screened children in the fifth grade and, consequently, these children could not be screened for follow-up in future screenings, as elementary schools are K-5th only. In addition, low-income families from the community were often transient and moved to other locations, thus children from these families were also lost to follow-up. Future studies should include income, poverty, social problems, and staff and parental factor differences.
The Eyemobile program has overcome important barriers to the treatment of refractive errors in underserved children in its target area. By going directly to these communities and offering free examinations and spectacle prescriptions, Eyemobile has eliminated both financial impediments and problems with access to care, which in turn has resulted in progressively improving compliance. Based on our results, we believe that the continued relationship with the community (schools, nurses, children, and parents) resulting from the Eyemobile model is an essential contributor to improved compliance. While this study highlighted the success of Eyemobile in improving access to and adherence to treatment, there remain several areas with room for improvement. Although an exam completion rate of about 77% in the last three years of the study represents the highest among similar interventions, to our knowledge, this means that there is a sizable minority of children not receiving necessary care. Increased exam completion may be achieved by improving parents’ access and examining the factors leading to better attendance of exams, which were noted in two of the schools in the Hoover Cluster. Parents and school staff represent an essential component of the success of the Eyemobile as they are responsible for arranging exam appointments, completing consent forms, and encouraging spectacle wear and are thus key to establishing and maintaining children’s eye care. Future studies addressing the involvement of parents and school personnel (teachers and nurses) as well as general attitudes (including children) could offer further success in improving compliance in this population. In future studies, more factors could also be brought in to assess spectacle wear compliance, such as the model of frame.
Hoover Cluster schools represent children from an underserved community who traditionally exhibit poor access to and adherence to care. However, our results indicate a positive change in behavior in both categories. This study supports the use of mobile eye services, such as the Eyemobile model, in schools in underserved communities to facilitate the identification and treatment of refractive errors and other eye diseases.
Disclosure
The authors report no conflicts of interest in this work.
References
1. World Health Organization. World Report on Vision. Geneva: World Health Organization; 2019.
2. Flaxman SR, Bourne RRA, Resnikoff S, et al. Global causes of blindness and distance vision impairment 1990–2020: a systematic review and meta-analysis. Lancet Glob Health. 2017;5(12):e1221–e1234. doi:10.1016/S2214-109X(17)30393-5
3. Vitale S, Cotch MF, Sperduto RD. Prevalence of visual impairment in the United States. JAMA. 2006;295(18):2158–2163. doi:10.1001/jama.295.18.2158
4. Hashemi H, Fotouhi A, Yekta A, Pakzad R, Ostadimoghaddam H, Khabazkhoob M. Global and regional estimates of prevalence of refractive errors: systematic review and meta-analysis. J Curr Ophthalmol. 2017;30(1):3–22. doi:10.1016/j.joco.2017.08.009
5. Jobke S, Kasten E, Vorwerk C. The prevalence rates of refractive errors among children, adolescents, and adults in Germany. Clin Ophthalmol. 2008;2(3):601–607. doi:10.2147/OPTH.S2836
6. Stewart CE, Moseley MJ, Fielder AR, Stephens DA. Refractive adaptation in amblyopia: quantification of effect and implications for practice. Br J Ophthalmol. 2004;88:1552–1556. doi:10.1136/bjo.2004.044214
7. Atkinson J, Nardini M, Anker S, Braddick O, Hughes C, Rae S. Refractive errors in infancy predict reduced performance on the movement assessment battery for children at 3 1/2 and 5 1/2 years. Dev Med Child Neurol. 2005;47(4):243–251. doi:10.1017/S0012162205000472
8. Naidoo KS, Jaggernath J. Uncorrected refractive errors. Indian J Ophthalmol. 2012;60(5):432–437. doi:10.4103/0301-4738.100543
9. Qiu M, Wang SY, Singh K, Lin SC. Racial disparities in uncorrected and undercorrected refractive error in the United States. Invest Ophthalmol Vis Sci. 2014;55(10):6996–7005. doi:10.1167/iovs.13-12662
10. Gogate P, Mukhopadhyaya D, Mahadik A, et al. Spectacle compliance amongst rural secondary school children in Pune district, India. Indian J Ophthalmol. 2013;61(1):8–12. doi:10.4103/0301-4738.99996
11. Norouzirad R, Hashemi H, Yekta A, et al. The prevalence of refractive errors in 6- to 15-year-old school children in Dezful. Iran J Curr Ophthalmol. 2015;27:51–55. doi:10.1016/j.joco.2015.09.008
12. Varma R, Wang MY, Ying-Lai M, et al. The prevalence and risk indicators of uncorrected refractive error and unmet refractive need in Latinos: the Los Angeles Latino Eye Study. Invest Ophthalmol Vis Sci. 2008;49:5264–5273. doi:10.1167/iovs.08-1814
13. Horwood AM. Compliance with first time spectacle wear in children under eight years of age. Eye. 1998;12:173–178. doi:10.1038/eye.1998.43
14. Mehravaran S, Duarte PB, Brown SI, et al. The UCLA preschool vision program, 2012–2013. J AAPOS. 2016;20:63–67. doi:10.1016/j.jaapos.2015.10.018
15. Preslan MW, Novak A. Baltimore vision screening project. Phase 2. Ophthalmology. 1998;105:150–153. doi:10.1016/S0161-6420(98)91813-9
16. Von-bischhoffshausen FB, Munoz B, Riquelme A, et al. Spectacle-wear compliance in school children in Concepción, Chile. Ophthalmic Epidemiol. 2014;21:362–369. doi:10.3109/09286586.2014.975823
17. Marcelli E, Pastor M. Unauthorized and uninsured: City Heights and San Diego County; 2015.
18. Burks M. San Diego’s richest poor neighborhood, two decades later; 2014. Available from: https://www.voiceofsandiego.org/topics/news/san-diegos-richest-poor-neighborhood-two-decades-later/.
19. Donahue SP, Arthur B, Neely DE, et al. Guidelines for automated preschool vision screening: a 10-year, evidence-based update. J AAPOS. 2013;17:4–8. doi:10.1016/j.jaapos.2012.09.012
20. Miller JM, Harvey EM. Spectacle prescribing recommendations of AAPOS members. J Pediatr Ophthalmol Strabismus. 1998;35:51–52. doi:10.3928/0191-3913-19980101-17
21. Caputo AR, Lingua RW. The problem of cycloplegia in the pediatric age group: a combination formula for refraction. J Pediatr Ophthalmol Strabismus. 1980;17:119–128. doi:10.3928/0191-3913-19800301-14
22. Griffith JF, Wilson R, Cimino HC, Patthoff M, Martin DF, Traboulsi EI. The use of a mobile van for school vision screening: results of 63,841 evaluations. Am J Ophthalmol. 2016;163:108–114.e1. doi:10.1016/j.ajo.2015.11.026
23. Rodriguez E, Srivastava A, Landau M. Increasing screening follow-up for vulnerable children: a partnership with school nurses. Int J Environ Res Public Health. 2018;15(8):1572. doi:10.3390/ijerph15081572
24. Castanon Holguin AM, Congdon N, Patel N, et al. Factors associated with spectacle-wear compliance in school-aged Mexican children. Invest Ophthalmol Vis Sci. 2006;47:925–928. doi:10.1167/iovs.05-0895
25. Messer DH, Mitchell GL, Twelker JD, et al. Spectacle wear in children given spectacles through a school-based program. Optom Vis Sci. 2012;89:19–26. doi:10.1097/OPX.0b013e3182357f8c
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
