Back to Journals » Clinical Epidemiology » Volume 12
Patterns of Multimorbidity and Differences in Healthcare Utilization and Complexity Among Acutely Hospitalized Medical Patients (≥65 Years) – A Latent Class Approach
Authors Juul-Larsen HG, Christensen LD , Bandholm T, Andersen O, Kallemose T , Jørgensen LM , Petersen J
Received 9 August 2019
Accepted for publication 12 November 2019
Published 28 February 2020 Volume 2020:12 Pages 245—259
DOI https://doi.org/10.2147/CLEP.S226586
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Irene Petersen
Helle Gybel Juul-Larsen, 1–3 Line Due Christensen, 1, 4 Thomas Bandholm, 1–3, 5 Ove Andersen, 1, 2, 6 Thomas Kallemose, 1 Lillian Mørch Jørgensen, 1, 6 Janne Petersen 1, 7, 8
1Clinical Research Centre, Copenhagen University Hospital Hvidovre, Hvidovre, Denmark; 2Department of Clinical Medicine, University of Copenhagen, Copenhagen, Denmark; 3Department of Physical and Occupational Therapy, Physical Medicine & Rehabilitation Research - Copenhagen (PMR-C), Copenhagen University Hospital Hvidovre, Hvidovre, Denmark; 4Research Unit for General Practice, Aarhus, Denmark; 5Department of Orthopedic Surgery, Copenhagen University Hospital Hvidovre, Hvidovre, Denmark; 6Emergency Department, Copenhagen University Hospital Hvidovre, Hvidovre, Denmark; 7Centre for Clinical Research and Prevention, Copenhagen University Hospital Bispebjerg and Frederiksberg, Copenhagen, Denmark; 8Section of Biostatistics, Department of Public Health, University of Copenhagen, Copenhagen, Denmark
Correspondence: Helle Gybel Juul-Larsen
Clinical Research Centre, Section 056, Copenhagen University, Amager and Hvidovre Hospitals, Kettegård Allé 30, Hvidovre DK-2650, Denmark
Tel +45 38626077
Email [email protected]
Purpose: The majority of acutely admitted older medical patients are multimorbid, receive multiple drugs, and experience a complex treatment regime. To be able to optimize treatment and care, we need more knowledge of the association between different patterns of multimorbidity and healthcare utilization and the complexity thereof. The purpose was therefore to investigate patterns of multimorbidity in a Danish national cohort of acutely hospitalized medical patients aged 65 and older and to determine the association between these multimorbid patterns with the healthcare utilization and complexity.
Patients and Methods: Longitudinal cohort study of 129,900 (53% women) patients. Latent class analysis (LCA) was used to develop patterns of multimorbidity based on 22 chronic conditions ascertained from Danish national registers. A latent class regression was used to test for differences in healthcare utilization and healthcare complexity among the patterns measured in the year leading up to the index admission.
Results: LCA identified eight distinct multimorbid patterns. Patients belonging to multimorbid patterns including the major chronic conditions; diabetes and chronic obstructive pulmonary disease was associated with higher odds of healthcare utilization and complexity than the reference pattern (“Minimal chronic conditions”). The pattern with the highest number of chronic conditions did not show the highest healthcare utilization nor complexity.
Conclusion: Our study showed that chronic conditions cluster together and that these patterns differ in healthcare utilization and complexity. Patterns of multimorbidity have the potential to be used in epidemiological studies of healthcare planning but should be confirmed in other population-based studies.
Keywords: chronic conditions, multimorbidity, older medical patients, acute hospitalization, latent class analysis
Introduction
Through the last decades, clinical guidelines and Disease Management Programs have been developed for single chronic conditions1,2 and hospital treatment has become increasingly specialized. The treatment of single chronic diseases has thereby been significantly improved. However, as the prevalence of multimorbidity is rising this development poses great challenges for the health professionals who must navigate in the complexity of multiple care pathways when treating patients with co- and multimorbidity3 (the presence of more than one chronic condition in a single individual4,5). Consequently, patients with multimorbidity face increasingly complicated medical lifestyle with fragmented appointments, investigations, polypharmacy, and medical regimes.6 Also, patients with multimorbidity are experiencing difficulties with access to information,7,8 lack of coherence or coordination in treatments8,9 and managing and adhering to treatment recommendation.8,10
Acute medical illness in older adults is associated with several adverse outcomes11–15 and the majority of the acutely hospitalized older medical patients are multimorbid.16 The number of chronic conditions are highly associated with hospitalizations, including acute admissions, and patients with multimorbidity have a higher healthcare utilization in both primary and secondary settings.17 However, a deeper understanding of multimorbidity that goes beyond counting the numbers of chronic conditions is needed.18 Several approaches have been used to capture the complexity of multimorbidity.19,20 Grouping multimorbidity into different combinations or patterns of chronic conditions may be a helpful tool to investigate healthcare outcomes. A handful of studies have investigated multimorbidity patterns and their relationship with healthcare outcomes.21–24 Olaya et al (2017) found two multimorbid patterns – the cardiovascular/mental/arthritis and the metabolic/stroke – that were significantly associated with more use of health services.21 Another study found four multimorbid patterns: Heart impairment, Metabolic-ischemic, Cardio-respiratory, and Cancer were associated with hospitalization.23 However, these studies have only investigated healthcare utilization without taking the logistical complexity of visiting different physicians into account. To optimize healthcare resources to accommodate the need of both the patients and the healthcare system, we need to identify the healthcare utilization as well as the logistical complexity of the treatment in relation to different patterns of multimorbidity.
The aim of this study was to investigate patterns of multimorbidity in a cohort of acutely hospitalized medical patients aged 65 and older and to investigate the healthcare utilization and the healthcare complexity among patients within these patterns the last year prior to admission. Furthermore, to study differences in the prognosis after admission among different patterns of multimorbidity.
Materials and Methods
Study Design
We conducted a longitudinal study based on data from national registries in a cohort of acutely hospitalized patients aged 65 and older. We studied patterns of multimorbidity based on the Chronic Condition Measurement Guide25 using latent class analysis. Healthcare utilization and healthcare complexity were based on data from national health registers in the year leading up to the index admission in 2011. Time to death and time to readmission was studied in a period of 5 years after discharge. The study is reported according to the STROBE checklist, using the extension for cross-sectional studies.26
Setting
The public Danish healthcare system, predominantly financed through general taxes, provides universal, free and equal access for all 5.6 million citizens. It is divided into two sectors: the primary sector; covering general practitioners, dentists, physiotherapists, etc., and the specialized sector; covering mainly public hospitals and a few private hospitals. The Danish citizens are registered each time they are in contact with the national healthcare system. Therefore, Denmark has comprehensive health records.27 At birth, all Danish citizens are given a unique personal identification number, the central personal register number (CPR-number).28 Because of the CPR-number, linkage at the individual level between nationwide registries is feasible.
Study Population
The study population contains all Danish citizens aged 65 years or older acutely admitted to a somatic department in a hospital in Denmark due to a medical illness in a period from 1st of January 2011 until 31st of December 2011.
Data Collection
The analyses are based on data from seven national registers: The Danish National Patient Register, which contains data on all Danish patients’ contacts with hospitals, both somatic and psychiatric, in Denmark. The Danish National Patient Register was established in 1977 and is considered to be very comprehensive internationally;29 The Danish Civil Registration System, which contains individual information on the CPR-number, name, sex, date and place of birth, and citizenship. The Danish Civil Registration System was established in 1968 and has a high validity;28 The Danish Register of Causes of Death, which contains data on all deaths in Denmark from 1875;30 The Danish National Prescription Register, which contains information on dispensed prescriptions since 1994, not including over-the-counter drugs;31 The Danish National Health Service Register for Primary Care, which contains data on health services from general practitioners, practicing medical specialists, physiotherapists, dentists, psychologists, chiropractors, and chiropodists since 1990;32 The Population’s Education Register, which contains information on ongoing and completed education, including length, level and institution33 and the Register for Migration from 1973, which contains the date of both immigration and emigration.34
Outcomes
Measures of Multimorbidity
To assess multimorbidity in the study population, we used the Chronic Condition Measurement Guide to define chronic conditions based on ICD10- and ATC-codes.25 Data on ICD10- and ATC-codes was extracted with 10 years of history as previous work suggest this to be an optimal follow-up time as 5 years is too short and 15 years do not add any more information when using administrative data.25,35 The Chronic Condition Measurement Guide is a guide of 83 chronic conditions based on registry data derived from persons aged 65 years and older. The 83 chronic conditions were compiled according to their pathophysiology by a specialist in internal medicine (OA), which constituted 38 chronic conditions in the list, e.g. the ICD-10 and ATC-codes for cardiac valve disorders; heart failure; chronic ischemic heart disease; acute myocardial infarction; pulmonary heart disease; cardiac arrhythmias; and heart disease, unspecified were compiled under the chronic condition: Heart disease (Additional file Table S1). To avoid too few observations, the analyses included 22 chronic conditions covering 95% of the chronic conditions in the cohort (Additional file Table S2).
Healthcare Utilization
Healthcare utilization was assessed 1 year prior to the index admission and was described as: No. of admissions, defined as both planned and acute. No. of acute admissions, defined as acute admission at a somatic department in a hospital. No. of outpatient clinic visits, defined as visits at a hospital or clinic in the secondary sector. Cumulated length of stay (CUMLOS), defined as the time between admission and discharge and cumulated for all somatic admissions within the period. No. of general practitioner (GP) visits, defined as face-to-face consultations. No. of visits at a specialist in private practice, defined as a visit at a specialist in the primary sector.
Healthcare Complexity
Healthcare complexity was assessed 1 year prior to the index admission and was described as: No. of different specialists in private practice, defined as visits at different specialists within different specialties in the primary sector. No. of different specialists in outpatient clinic, defined as visits at different specialists at a hospital or clinic in the secondary sector. No. of different causes of admission based on chapters in the ICD10. A total number for complexity was derived from adding no. of different specialists in private practice, no. of different specialists in outpatient clinic, and no. of different causes of admission.
Descriptive Data
Sociodemographic data were obtained regarding age, sex, marital status, and education level. Multimorbidity was defined as the presence of more than one chronic condition in a single individual.36 No. of chronic diagnoses was defined as number of diagnosis in the Chronic Condition Measurement Guide using 10 years of history from the index admission. Drug use at ATC level 4 was assessed based on from data on all redeemed prescriptions at pharmacy, including older people living in institutions obtained from the Danish National Prescription Register. Only medications for systemic use were included in the study: inhalators, medications with topical or ocular administration, and dietary supplements were excluded. To gain knowledge on the most recent drug use, data was extracted with 1 year of history prior to the index admission.
Ethical Considerations
The Danish national registries are protected by the Danish Act on Processing of Personal Data and can only be assessed following application and subsequent approval. This study has been approved by the Data Protection Agency (Project nr. 704775 at Statistics Denmark). No approval from the Danish Research Ethics Committees for the Capital Region was needed, since only national registers were used.
Statistics
We used latent class models to classify persons into patterns of multimorbidity according to their distribution of chronic conditions. The objective of latent class analysis (LCA) is to classify individuals from an apparently heterogeneous population into more homogenous subgroups (latent classes) based on a number of observed indicators, in this case, the 22 chronic conditions.37 The analysis consisted of development of a model to form the disease patterns. To be able to validate results from class development we randomly divided our population in three datasets of 43,300 patients. We determined the optimal number of classes included in the categorical latent variable model by sequentially fitting models from one to more latent classes without any grouping variables or covariates. We then compared the Bayesian information criterion (BIC) across the models (lower values are better).38 Additionally, we plotted the conditional probabilities for each class and compared the results from the three datasets to validate the model. Together with the BIC and the plots, we used clinical evaluations of the usefulness and face validity to determine the optimal number of classes. After determining the optimal number of classes, we tested for differential item functioning with respect to sex. If differential item functioning with one of the items were statistically significant, they were included in the final model. We initially started the analyses with one model including both women and men with differential item functioning with respect to sex. The 13-class model yielded the lowest BIC. We were, however, not able to identify a model with differential item functioning. Therefore, we determined to stratify our analyses according to sex. The stratified classes were labeled based on which conditions exhibited excess prevalence (i.e., prevalence in class exceeds prevalence in full cohort). We used the entropy-based pseudo-R2 measure to describe the degree of classification uncertainty when assigning individuals into the multimorbid patterns. This measure indicates how precise one can predict class membership based on the observed variables (chronic conditions). The closer these values are to 1 the better the predictions. Due to the large number of parameters estimated in the LCA we used 40,000 random starts and 350 full iterations per set to avoid local maxima of the likelihood function. To estimate the association between healthcare utilization and patterns of multimorbidity we used the two-step estimation of models and external variables.39 After selecting on the best model, we fixed the parameter estimates from the measurement part of the latent class model using the average of the parameters estimates from the three datasets. We then fitted a latent class regression model with the covariates and tested differences among the multimorbid patterns. To investigate differences in time to death between the multimorbid patterns, we used a proportional hazards model with the parameter estimates fixed. To investigate differences in time to readmission between the multimorbid patterns, we used a proportional hazards model with death as a competing risk. In Mplus version 8 (Muthén & Muthén, Los Angeles, CA) it is not possible to model competing event; therefore, we used modal assignment in which all patients were assigned to a specific multimorbid pattern based on the multimorbid pattern with the highest posterior probability. Level of significance was set at 0.05. Descriptive analyses were done using the SAS 9.4 software package for Windows (SAS Institute, Cary, NC, USA), plots were created in R 3.2.3 (R Foundation for Statistical Computing, Vienna, Austria) and Latent Class Models were fitted using Mplus version 8 (Muthén & Muthén, Los Angeles, CA).
Results
In total, 129,900 persons aged 65 or more were acutely hospitalized due to a medical illness from 1st of January 2011 until 31st of December 2011 of which 53% were women (Table 1).
 |
Table 1 Characteristics of the Population (n=129,900) |
Model Selection
The BIC and entropy are shown in Table 2. For both sexes, the models with 7, 8, 9, and 10 classes were chosen to be investigated more thoroughly. For women, looking at model fit, the BIC was lowest in the model with 10 classes for two datasets and in the model with 9 classes for one dataset. For men, the BIC was lowest in the model with 9 classes for two datasets and for the model with 10 classes for one dataset. When comparing the posterior probabilities of the chronic conditions within each multimorbid pattern among the three different datasets for the model with 9 classes for both sexes, we were not able to identify consistent results. However, in the 8-class model the results were similar across datasets. Based on the BIC-values, the plots of the three data sets and the clinical evaluations of the usefulness, the 8-class model was chosen for both men and women. The 8-class model showed a median entropy of 0.62 (range 0.55 to 0.63) for women and 0.64 (range 0.61 to 0.65) for men, corresponding to a moderate classification quality.39
 |
Table 2 Bayesian Information Criterion (BIC) for Latent Models with 7–11 Classes |
Tables 3 and 4 show prevalence and the estimated conditional probability of having a chronic condition in each of the identified chronic condition patterns. The patterns were labelled based on the prevalence of the included chronic conditions. We found six multimorbid patterns that showed minimal differences between women and men: “Minimal chronic conditions”; “Cardiovascular disorders”; “Neurological and vascular disorders”; “Degenerative and pulmonary disorders”; “Metabolic and cardiovascular disorders”; and “Neuropsychiatric and functional disorders”. Overall, the largest pattern was labelled “Minimal chronic conditions” (23% (women) and 25% (men)) and this pattern was characterized by low probabilities compared to the marginal probabilities on all chronic conditions except for cancer (expected number of chronic conditions 2.2 for women and 2.2 for men). In addition, for women, all patients with no or one chronic condition belonged to the “Minimal chronic conditions” pattern. For men, 96% of the patients with no or one chronic condition belonged to the “Minimal chronic conditions” pattern. The second largest pattern was labelled “Cardiovascular disorders” (expected number of chronic conditions 3.7 for women and 3.8 for men. The patterns characterized by the highest expected number of chronic conditions were labeled “Neuropsychiatric and functional disorders” (expected number of chronic conditions 7.4 for women and 7.1 for men). The remaining patterns were labelled “Metabolic and cardiovascular disorders” (expected number of chronic conditions 6.1 for women and 6.3 for men), “Degenerative and pulmonary disorders” (expected number of chronic conditions 4.9 for women and 5.2 for men), and “Neurological and vascular disorders” (expected number of chronic conditions 4.0 for women and 3.9 for men). For men, 2% of the patients with no or one chronic condition belonged to the “Neurological and vascular disorders” pattern. We found two patterns for both men and women that could not be identified at the opposite sex. For women, the first pattern was labelled “Degenerative and mental disorders” (expected number of chronic conditions 5.0) and the second pattern was labelled “Complex multimorbidity” (expected number of chronic conditions 6.6). For men, the first pattern was labelled “Mental disorders” (expected number of chronic conditions 5.1). The second pattern was labelled “Dementia and Parkinson’s Disease” for men (expected number of chronic conditions 4.0). In total, 2% of the patients with no or one chronic condition belonged to the “Dementia and Parkinson’s Disease” pattern.
Healthcare Utilization
For women, the “Complex multimorbidity” pattern showed the highest healthcare utilization regarding no. of; GP visits, visits at a specialist in private practice, hospitalizations, acute hospitalizations, and visits in outpatient clinics (adjusted for age) compared to the “Minimal chronic conditions” pattern (Figure 1). For men, the “Degenerative and pulmonary disorders” showed the highest healthcare utilization regarding no. of; GP visits, visits at a specialist in private practice, hospitalizations, and acute hospitalizations (adjusted for age) compared to the “Minimal chronic conditions” pattern (Figure 2). The “Neurological and vascular disorders” pattern showed general lower odds of healthcare utilization (adjusted for age) compared to the “Minimal chronic conditions” pattern for both sexes (Figures 1 and 2). In general, the highest healthcare utilization was at the GP with mean visits ranging from 8 visits (“Minimal chronic conditions”) to 14 visits (“Complex multimorbidity”) for women and from 8 visits (“Neurological and vascular disorders”) to 14 visits (“Degenerative and pulmonary disorders”) for men (Additional file Table S3 and S4). Acute admissions in the year leading up to the index admission ranged from 0.7 (“Minimal chronic conditions” and “Neurological and vascular disorders”) to 1.6 (“Neuropsychiatric disorders”) for women and from 0.6 (“Neurological and vascular disorders”) to 1.5 (“Mental disorders” and “Neuropsychiatric disorders”) for men (Additional file Table S3 and S4).
 |
Figure 1 Age-adjusted odds ratios for differences in healthcare utilization the last year before an acute hospitalization between patients in the eight multimorbid patterns for women. |
 |
Figure 2 Age-adjusted odds ratios for differences in healthcare utilization the last year before an acute hospitalization between patients in the eight multimorbid patterns for men. |
Healthcare Complexity
For women, the patterns “Metabolic and cardiovascular disorders”, “Degenerative and pulmonary disorders”, and “Complex multimorbidity” showed the highest complexity (adjusted for age) regarding number of different specialists in the primary sector, and in outpatient clinics compared to the “Minimal chronic conditions” pattern (Figure 3). The patterns “Degenerative and mental disorders”, “Neuropsychiatric and functional disorders”, and “Complex multimorbidity” showed the highest number of different diagnoses at admission (adjusted for age) compared to the “Minimal chronic conditions” pattern (Figure 3). For men, the patterns “Metabolic and cardiovascular disorders”, and “Degenerative and pulmonary disorders” showed the highest complexity (adjusted for age) regarding number of different specialists in the primary sector, and in outpatient clinics compared to the “Minimal chronic conditions” pattern (Figure 3). The patterns “Metabolic and cardiovascular disorders”, “Mental disorders”, “Degenerative and pulmonary disorders” and “Neuropsychiatric and functional disorders” showed the highest number of different diagnoses at admission (adjusted for age) compared to the “Minimal chronic conditions” pattern (Figure 3). Out of the top 10% most complex female patients (4913), 20% were in the pattern “Degenerative and pulmonary disorders”; 19% were in “Cardiovascular disorders”; and 17 were in “Complex multimorbidity”. Out of the top 10% of most complex male patients (4810), 25% were in the pattern “Metabolic and cardiovascular disorders”; 24% were in “Cardiovascular disorders”; and 15% were in “Degenerative and pulmonary disorders”.
 |
Figure 3 Age-adjusted odds ratios for differences in healthcare complexity the last year before an acute hospitalization between patients in the eight multimorbid patterns. |
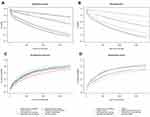
Time to Death and Readmission After an Acute Hospitalization
In total, 5134 (7.5%) women and 5159 (8.4%) men died during their index hospitalization. The differences in time to readmission and time to death for the different patterns of multimorbidity stratified by sex are depicted in Figure 4. For women, the patterns “Complex multimorbidity”; “Neuropsychiatric and functional disorders”; and “Degenerative and mental disorders” showed the highest mortality within 5 years of discharge among the eight multimorbid patterns (adjusted for age). For men, the patterns “Metabolic and cardiovascular disorders”; “Degenerative and pulmonary disorders”; and “Neuropsychiatric and functional disorders” showed the highest mortality among the eight multimorbid patterns (adjusted for age). Among those who survived their admission, 47,775 (75%) women and 42,669 (76%) men were readmitted within 5 years of discharge. For women, the patterns “Complex multimorbidity”; “Neuropsychiatric and functional disorders”; “Metabolic and cardiovascular disorders”; and “Degenerative and mental disorders” showed the highest cumulative incidence of being readmitted (adjusted for age). For men, the patterns “Mental disorders”; “Neuropsychiatric and functional disorders”; “Metabolic and cardiovascular disorders”; and “Degenerative and pulmonary disorders” showed the highest cumulative incidence of being readmitted (adjusted for age).
Discussion
In a national population of acutely hospitalized older medical patients, we identified eight patterns of multimorbidity based on the presence or absence of 22 chronic conditions in both women and men. Interestingly, our results also show that multimorbid patterns differ in their healthcare utilization and complexity. Notably, the pattern characterized by the highest number of chronic conditions as well as the highest number of expected chronic conditions did not show the highest healthcare utilization or complexity. Although the multimorbid patterns characterized by high numbers of chronic conditions as well as the high numbers of expected chronic conditions did show high levels of healthcare utilization or complexity as well as high risks of readmission and mortality after an acute admission.
The identified patterns of multimorbidity described clinically recognizable patterns of multimorbidity among acutely hospitalized older medical patients. For example, the “Metabolic and cardiovascular disorders” pattern describes the well-established association between diabetes and cardiovascular disorders40 and the “Degenerative and pulmonary disorders” pattern describes the well-established association between osteoporosis and chronic obstructive pulmonary disease (COPD).41 We did not find a pattern that we could classify as “healthy” as other studies have.21,42–45 However, the population in our study was defined as acutely hospitalized older medical patients and therefore likely represents a more vulnerable group. The majority of our sample (23% for women and 25% for men) was classified into the “Minimal chronic conditions” pattern for both sexes and also had the lowest expected number of chronic conditions (2 for women and 2 for men). The pattern had a slightly higher conditional probability of cancer than the marginal probability. The reason for this low expected number of chronic conditions for a pattern with an elevated conditional probability for a serious chronic disease such as cancer might be caused by the definition of the chronic conditions being based on a 10-year prevalence. It is, therefore, possible for a person to have been diagnosed with cancer 7 years ago and being cured for this cancer since then and not otherwise have a chronic condition.
Only a handful of studies have investigated multimorbid patterns among older people using LCA and have in general found fewer multimorbid patterns than in the present study.19,21,42,44–47 This might be caused by differences in population; study sample; and/or items. Despite these differences, there are however some similarities in the multimorbid patterns. The multimorbid patterns: “Metabolic and cardiovascular disorders”; “Cardiovascular disorders”; “Minimal chronic conditions”; “Neuropsychiatric and functional disorders”; and for women “Complex multimorbidity” were also found in other studies.19,21,42,44–46 We found six patterns that showed only minimal differences between sexes, and two patterns showed substantial differences in disease patterns and was therefore labelled differently for women and men. The “Complex multimorbidity” pattern was only found for women. This finding may be caused by the fact that women visit the doctor more often than men48 and henceforth are diagnosed with more chronic conditions than men, but also by an association between age and number of chronic conditions as women generally live longer than men.49 We found a pattern of “Dementia and Parkinson’s Disease” for men. The prevalence of Parkinson’s Disease is slightly larger for men than for women50 although in this study the prevalence was similar for women and men. For women, the patients with Parkinson’s Disease did not fall into one main pattern but were distributed across patterns. The pattern with the highest conditional probability of Parkinson’s Disease did for women also coincide with dementia (“Degenerative and mental disorders”).
We found that the pattern with the highest number of chronic conditions as well as the highest number of expected chronic conditions (the “Neuropsychiatric and functional disorders” pattern) only showed a high healthcare utilization in relation to a high number of acute admission, which might be caused by patients from this pattern not being part of one of the disease management programs with many control visits, such as the COPD or the Diabetes program.51,52 This finding confirms that the need for a deeper understanding of multimorbidity than just looking at the count of chronic diseases when investigating the effect of multimorbidity on different outcomes. Among the remaining patterns, we did, however, see a tendency towards a higher healthcare utilization as the number of chronic conditions rose. We found a relatively low healthcare utilization among the patterns “Cardiovascular disorders” and “Neurological and vascular disorders” for both women and men. These two patterns share pathophysiology but are also, together with the “Minimal chronic conditions” pattern, the multimorbid patterns with the lowest expected number of chronic conditions. Also, we found a relatively high healthcare utilization and a high expected number of chronic conditions among the patterns “Complex multimorbidity” for women and “Metabolic and cardiovascular disorders” and “Degenerative and pulmonary disorders” for men. This finding is in line with other findings of an association between an increasing number of chronic conditions and a high healthcare utilization.17,53–57
The “Degenerative and mental disorders” pattern for women and the “Mental disorders” pattern for men, both containing the highest conditional probabilities of mental disorders due to alcohol and depression, showed a high healthcare utilization in the secondary sector with many acute hospitalizations compared to the “Minimal chronic conditions” pattern. Together with the high readmission rate as well as the high mortality rate, especially for women, this study highlights the need for increasing the treatment of patients with alcohol-related problems.
Treatment at different primary care physicians and specialists, reflecting the burden of treatment has previously been associated with multimorbidity.53,55 Both women and men belonging to the patterns “Metabolic and cardiovascular disorders” and “Degenerative and pulmonary disorders” showed a relatively high healthcare complexity. In Denmark, the responsibility of the management and treatment of COPD and diabetes is currently being transferred from the specialists in the hospital to the GP´s in the primary sector to treat the patients more closely to their home, but also to reduce the treatment burden for the patients. However, studies of the GPs´ experience with treating patients with multimorbidity, show that the GPs´ experience many barriers.3,58,59 These include structural barriers of short time consultations, which makes it difficult to treat the whole patient and not just one problem.3,59 This can be easily dealt with by agreeing on longer consultations and payment hereof. But there are also barriers related to the medical treatment.3,58,59 In Denmark, GPs manage over 80% of all prescribed drugs,60 however many physicians have difficulties with deprescribing drugs not prescribed by themselves and hence, contribute to an accumulation of prescribed drugs and a complex medical regime for the patient.61 In this study, the number of redeemed prescriptions ranged from 4 (“Minimal chronic conditions” and “Neurological and vascular disorders”) to 17 (“Complex multimorbidity”) for women and from 3 (“Neurological and vascular disorders”) to 15 (“Degenerative and pulmonary disorders”) for men. To gain a successful reorganization of the healthcare system, i.e. relocating tasks from the specialists in the hospital to GP, re-prioritization of resources, education, and a closer collaboration between municipalities, GPs and the hospital service are required.9,62
In the time after the acute admission, the patterns “Complex multimorbidity”; “Neuropsychiatric and functional disorders”; and “Degenerative and mental disorders” for women showed the highest mortality as well as high cumulative incidence of being readmitted compared to the “Minimal chronic conditions” pattern. For men, the patterns “Metabolic and cardiovascular disorders”; “Degenerative and pulmonary disorders”; and “Neuropsychiatric and functional disorders” showed the highest mortality as well as high risk of being readmitted compared to the “Minimal chronic conditions” pattern. What these multimorbid patterns have in common is a high expected number of chronic conditions, polypharmacy, as well as a high number of acute admissions leading up to the index admission. In addition, both the number of chronic conditions and acute admissions predict mortality among older people.11,63,64 Furthermore, Klausen et al (2017) have shown that among acutely hospitalized older medical patients the number of admission laboratory results outside the reference interval, representing different organ systems, was strongly associated with mortality.65
Strengths and Limitations
The main strengths of this study include the large national unselected population, no risk of recall bias because of the use of detailed and complete register data, and the large spectrum of chronic conditions included. Furthermore, we included data that have been collected prospectively and objectively which increases the validity of the disease classification. There are several limitations in this study. Firstly, it can be difficult to directly compare our findings with the previous studies, as the results are influenced by a number of factors, including the number and type of chronic conditions included, the demographic and underlying risk factors of the population and the way in which data has been obtained. Despite this complexity, however, we have allowed ourselves to compare these results with results found in other western countries. Secondly, we have not included data on the time of diagnosis. Further studies with time included in the analysis could provide more knowledge for use in determining prevention strategies. Thirdly, diagnosis codes from the primary sector would have increased the validity of the disease classification, but in Denmark, no register of ICD-10 codes in the primary sector exists. However, by including chronic conditions based on drug prescribing information we include patients with chronic conditions only seen in the primary sector, which lower the risk of misclassification. In addition, some ICD-10 codes are not systematically used such as ICD-10 codes for obesity, which can lead to an underestimation and affect the conditional prevalence. However, we do believe that the high conditional prevalence for obesity in the “metabolic and cardiovascular” pattern would be consistent. We used 10 years of history for all the chronic conditions, though it is possible that some chronic conditions diagnosed 10 years ago and not replicated since is not of importance any longer and can lead to risk of misclassification. Fourthly, despite the large sample size and the high number of items in the latent class model, there is still some degree of uncertainty associated with latent class classification as inclusion of other diseases could have led to other classes. However, as ICD-10 codes are grouped across related ICD-10 codes, we are convinced that this issue is of minor importance. Also, by dividing the data into three data sets and performing the LCA separately on all three, we ensured that the results are reproducible. Furthermore, the labeling of the patterns was based on which conditions exhibited excess prevalence. Different ways of labeling could have been used, e.g. based on combinations of chronic conditions within each pattern, which might have resulted in other labels. Therefore, the labels of the patterns should be interpreted with caution. We determined to label the first pattern “minimal chronic conditions” despite the slightly higher conditional probability of cancer, because 1) the majority of patients with no or only one chronic condition belonged to this pattern; 2) the conditional probability of cancer was similar to the conditional probability of cancer in other patterns; and 3) there is a risk of misclassification of cancer as a patient could have been treated for that cancer, and therefore not have a chronic condition at the index admission.
Conclusion
This study identified eight distinct patterns of multimorbidity among both women and men using LCA in a nationally representative sample of acutely hospitalized older medical patients. The multimorbid patterns have the potential to be used in further epidemiological studies on healthcare utilization and complexity as well as treatment and prevention strategies but should be confirmed in other population-based studies. The eight multimorbid patterns differed in their healthcare utilization and complexity. Besides the fact that multimorbid patterns with high numbers of chronic conditions showed a high mortality and readmission risk in the time after an acute hospitalization, we found that the pattern with the highest number of chronic conditions was not the pattern with the highest healthcare utilization or complexity, which highlights the need for not just investigating multimorbidity by simply counting the number of chronic conditions. High levels of healthcare utilization and/or complexity were found among the multimorbid patterns characterized by high probabilities of the major chronic diseases as chronic obstructive pulmonary disease and/or diabetes, both belonging to clinical guidelines with many control visits.
Acknowledgments
This study was performed in collaboration with the Optimized Senior Patient Program at Copenhagen University Hospital in Hvidovre.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Hughes LD, McMurdo MET, Guthrie B. Guidelines for people not for diseases: the challenges of applying UK clinical guidelines to people with multimorbidity. Age Ageing. 2013;42(1):62–69. doi:10.1093/ageing/afs100
2. Boyd CM, Darer J, Boult C, Fried LP, Boult L, Wu AW. Clinical practice guidelines and quality of care for older patients with multiple comorbid diseases: implications for pay for performance. JAMA. 2005;294(6):716–724. doi:10.1001/jama.294.6.716
3. Søndergaard E, Willadsen TG, Guassora AD, et al. Problems and challenges in relation to the treatment of patients with multimorbidity: general practitioners’ views and attitudes. Scand J Prim Health Care. 2015;33(2):121–126. doi:10.3109/02813432.2015.1041828
4. van den AM, Buntinx F, Knottnerus JA. Comorbidity or multimorbidity. Eur J General Pract. 1996;2(2):65–70. doi:10.3109/13814789609162146
5. Nicholson K, Makovski TT, Griffith LE, Raina P, Stranges S, van den Akker M. Multimorbidity and comorbidity revisited: refining the concepts for international health research. J Clin Epidemiol. 2018. doi:10.1016/j.jclinepi.2018.09.008
6. Moffat K, Mercer SW. Challenges of managing people with multimorbidity in today’s healthcare systems. BMC Fam Pract. 2015;16(1):129. doi:10.1186/s12875-015-0344-4
7. Millar E, Stanley J, Gurney J, et al. Effect of multimorbidity on health service utilisation and health care experiences. J Prim Health Care. 2018;10(1):44–53. doi:10.1071/HC17074
8. McGilton KS, Vellani S, Yeung L, et al. Identifying and understanding the health and social care needs of older adults with multiple chronic conditions and their caregivers: a scoping review. BMC Geriatr. 2018;18. doi:10.1186/s12877-018-0925-x
9. Schiøtz ML, Høst D, Frølich A. Involving patients with multimorbidity in service planning: perspectives on continuity and care coordination. J Comorb. 2016;6(2):95–102. doi:10.15256/joc.2016.6.81
10. Rosbach M, Andersen JS. Patient-experienced burden of treatment in patients with multimorbidity - A systematic review of qualitative data. PLoS One. 2017;12(6):e0179916. doi:10.1371/journal.pone.0179916
11. Boyd CM, Landefeld CS, Counsell SR, et al. Recovery of activities of daily living in older adults after hospitalization for acute medical illness. J Am Geriatr Soc. 2008;56(12):2171–2179. doi:10.1111/j.1532-5415.2008.02023.x
12. Gill TM, Allore HG, Gahbauer EA, Murphy TE. Change in disability after hospitalization or restricted activity in older persons. JAMA. 2010;304(17):1919–1928. doi:10.1001/jama.2010.1568
13. Juul-Larsen HG, Petersen J, Sivertsen DM, Andersen O. Prevalence and overlap of Disease Management Program diseases in older hospitalized patients. Eur J Ageing. 2017;14(3):283–293. doi:10.1007/s10433-017-0412-9
14. de Gelder J, Lucke JA, Heim N, et al. Predicting mortality in acutely hospitalized older patients: a retrospective cohort study. Intern Emerg Med. 2016;11:587–594. doi:10.1007/s11739-015-1381-7
15. Bodilsen AC, Klausen HH, Petersen J, et al. Prediction of mobility limitations after hospitalization in older medical patients by simple measures of physical performance obtained at admission to the emergency department. PLoS One. 2016;11(5):e0154350. doi:10.1371/journal.pone.0154350
16. Juul-Larsen HG, Andersen O, Bandholm T, et al. Differences in function and recovery profiles between patterns of multimorbidity among older medical patients the first year after an acute admission – an exploratory latent class analysis [Submitted]. Archiv Gerontol Geriatr. 2020;86:103956. doi:10.1016/j.archger.2019.103956
17. Palladino R, Tayu Lee J, Ashworth M, Triassi M, Millett C. Associations between multimorbidity, healthcare utilisation and health status: evidence from 16 European countries. Age Ageing. 2016;45(3):431–435. doi:10.1093/ageing/afw044
18. Marengoni A, Vetrano DL, Onder G. Target population for clinical trials on multimorbidity: is disease count enough? J Am Med Dir Assoc. 2019;20(2):113–114. doi:10.1016/j.jamda.2018.10.012
19. Islam MM, Valderas JM, Yen L, Dawda P, Jowsey T, McRae IS. Multimorbidity and comorbidity of chronic diseases among the senior australians: prevalence and patterns. PLoS One. 2014;9(1):e83783. doi:10.1371/journal.pone.0083783
20. Ng SK, Tawiah R, Sawyer M, Scuffham P. Patterns of multimorbid health conditions: a systematic review of analytical methods and comparison analysis. Int J Epidemiol. 2018;47(5):1687–1704. doi:10.1093/ije/dyy134
21. Olaya B, Moneta MV, Caballero FF, et al. Latent class analysis of multimorbidity patterns and associated outcomes in Spanish older adults: a prospective cohort study. BMC Geriatr. 2017;17. doi:10.1186/s12877-017-0586-1
22. Dong H-J, Wressle E, Marcusson J. Multimorbidity patterns of and use of health services by Swedish 85-year-olds: an exploratory study. BMC Geriatr. 2013;13:120. doi:10.1186/1471-2318-13-120
23. Buja A, Rivera M, De Battisti E, et al. Multimorbidity and hospital admissions in high-need, high-cost elderly patients. J Aging Health. 2018:898264318817091. doi:10.1177/0898264318817091
24. Collerton J, Jagger C, Yadegarfar ME, et al. Deconstructing complex multimorbidity in the very old: findings from the newcastle 85+ study. Biomed Res Int. 2016;2016:8745670. doi:10.1155/2016/8745670
25. Juul-Larsen HG, Christensen LD, Andersen O, Bandholm T, Kaae S, Petersen J. Development of the “chronic condition measurement guide”: a new tool to measure chronic conditions in older people based on ICD-10 and ATC-codes. Eur Geriatr Med. 2019;10:431–444. doi:10.1007/s41999-019-00188-y
26. von Elm E, Altman DG, Egger M, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 2007;335(7624):806–808. doi:10.1136/bmj.39335.541782.AD
27. Thygesen LC, Daasnes C, Thaulow I, Brønnum-Hansen H. Introduction to Danish (nationwide) registers on health and social issues: structure, access, legislation, and archiving. Scand J Public Health. 2011;39(7_suppl):12–16. doi:10.1177/1403494811399956
28. Pedersen CB. The Danish civil registration system. Scand J Public Health. 2011;39(7 Suppl):22–25. doi:10.1177/1403494810387965
29. Lynge E, Sandegaard JL, Rebolj M. The Danish national patient register. Scand J Public Health. 2011;39(7 Suppl):30–33. doi:10.1177/1403494811401482
30. Helweg-Larsen K. The Danish register of causes of death. Scand J Public Health. 2011;39(7 Suppl):26–29. doi:10.1177/1403494811399958
31. Kildemoes HW, Sørensen HT, Hallas J. The Danish national prescription registry. Scand J Public Health. 2011;39(7 Suppl):38–41. doi:10.1177/1403494810394717
32. Andersen JS, Olivarius NDF, Krasnik A. The Danish national health service register. Scand J Public Health. 2011;39(7 Suppl):34–37. doi:10.1177/1403494810394718
33. Jensen VM, Rasmussen AW. Danish education registers. Scand J Public Health. 2011;39(7Suppl):91–94. doi:10.1177/1403494810394715
34. Norredam M, Kastrup M, Helweg-Larsen K. Register-based studies on migration, ethnicity, and health. Scand J Public Health. 2011;39(7 Suppl):201–205. doi:10.1177/1403494810396561
35. Schram MT, Frijters D, van de Lisdonk EH, et al. Setting and registry characteristics affect the prevalence and nature of multimorbidity in the elderly. J Clin Epidemiol. 2008;61(11):1104–1112. doi:10.1016/j.jclinepi.2007.11.021
36. Fortin M, Bravo G, Hudon C, Vanasse A, Lapointe L. Prevalence of multimorbidity among adults seen in family practice. Ann Fam Med. 2005;3(3):223–228. doi:10.1370/afm.272
37. Hagenaars JA, ed. Applied Latent Class Analysis. Cambridge: Cambridge University Press; 2009.
38. Nylund KL, Asparouhov T, Muthén BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: a monte carlo simulation study. Struct Equ Modeling. 2007;14(4):535–569. doi:10.1080/10705510701575396
39. Bakk Z, Kuha J. Two-step estimation of models between latent classes and external variables. Psychometrika. 2018;83(4):871–892. doi:10.1007/s11336-017-9592-7
40. Balakumar P, Maung-U K, Jagadeesh G. Prevalence and prevention of cardiovascular disease and diabetes mellitus. Pharmacol Res. 2016;113:600–609. doi:10.1016/j.phrs.2016.09.040
41. Inoue D, Watanabe R, Okazaki R. COPD and osteoporosis: links, risks, and treatment challenges. Int J Chron Obstruct Pulmon Dis. 2016;11:637–648. doi:10.2147/COPD.S79638
42. Whitson HE, Johnson KS, Sloane R, et al. Identifying patterns of multimorbidity in older americans: application of latent class analysis. J Am Geriatr Soc. 2016;64(8):1668–1673. doi:10.1111/jgs.14201
43. Filipčić I, Šimunović Filipčić I, Grošić V, et al. Patterns of chronic physical multimorbidity in psychiatric and general population. J Psychosom Res. 2018;114:72–80. doi:10.1016/j.jpsychores.2018.09.011
44. Nguyen QD, Wu C, Odden MC, Kim DH. Multimorbidity patterns, frailty, and survival in community-dwelling older adults. J Gerontol a Biol Sci Med Sci. 2018. doi:10.1093/gerona/gly205
45. Gonsoulin ME, Durazo-Arvizu RA, Goldstein KM, et al. A health profile of senior-aged women veterans: a latent class analysis of condition clusters. Innov Aging. 2017;1(2). doi:10.1093/geroni/igx024
46. Buja A, Claus M, Perin L, et al. Multimorbidity patterns in high-need, high-cost elderly patients. PLoS One. 2018;13(12):e0208875. doi:10.1371/journal.pone.0208875
47. Gellert P, von Berenberg P, Zahn T, Neuwirth J, Kuhlmey A, Dräger D. Multimorbidity profiles in german centenarians: a latent class analysis of health insurance data. J Aging Health. 2019;31(4):580–594. doi:10.1177/0898264317737894
48. Osika Friberg I, Krantz G, Määttä S, Järbrink K. Sex differences in health care consumption in Sweden: a register-based cross-sectional study. Scand J Public Health. 2016;44(3):264–273. doi:10.1177/1403494815618843
49. Statistics Denmark [statistikbanken.dk/HISB7] In Danish. 2019. Available from: https://www.statistikbanken.dk/statbank5a/default.asp?w=1280.
50. Wong SL, Gilmour H, Ramage-Morin PL. Parkinson’s disease: prevalence, diagnosis and impact. Health Reports. 2014;25(11):7.
51. Capital region, Denmark. [Forløbsprogram for diabetes Type 2]. In Danish. 2009. Available from: https://www.regionh.dk/til-fagfolk/Sundhed/kronisk-sygdom/PublishingImages/Sider/Forloebsprogram-for-type-2-diabetes/Forl%C3%B8bsprogrammet%20for%20type%202-diabetes.pdf.
52. Capital region, Denmark. [Forløbsprogram for KOL]. In Danish. 2009. Available from: https://www.regionh.dk/til-fagfolk/Sundhed/kronisk-sygdom/PublishingImages/Sider/Forloebsprogram-for-KOL/Forloebsprogram_KOL_LR.pdf.
53. Bähler C, Huber CA, Brüngger B, Reich O. Multimorbidity, health care utilization and costs in an elderly community-dwelling population: a claims data based observational study. BMC Health Serv Res. 2015;15:23. doi:10.1186/s12913-015-0698-2
54. Hutchinson AF, Graco M, Rasekaba TM, Parikh S, Berlowitz DJ, Lim WK. Relationship between health-related quality of life, comorbidities and acute health care utilisation, in adults with chronic conditions. Health Qual Life Outcomes. 2015;13:69. doi:10.1186/s12955-015-0260-2
55. van den Bussche H, Schön G, Kolonko T, et al. Patterns of ambulatory medical care utilization in elderly patients with special reference to chronic diseases and multimorbidity–results from a claims data based observational study in Germany. BMC Geriatr. 2011;11:54. doi:10.1186/1471-2318-11-54
56. Glynn LG, Valderas JM, Healy P, et al. The prevalence of multimorbidity in primary care and its effect on health care utilization and cost. Fam Pract. 2011;28(5):516–523. doi:10.1093/fampra/cmr013
57. van Oostrom SH, Picavet HSJ, de Bruin SR, et al. Multimorbidity of chronic diseases and health care utilization in general practice. BMC Fam Pract. 2014;15:61. doi:10.1186/1471-2296-15-61
58. Austad B, Hetlevik I, Mjølstad BP, Helvik A-S. Applying clinical guidelines in general practice: a qualitative study of potential complications. BMC Fam Pract. 2016;17:92. doi:10.1186/s12875-016-0490-3
59. Smith SM, O’Kelly S, O’Dowd T. GPs’ and pharmacists’ experiences of managing multimorbidity: a ‘Pandora’s box.’. Br J Gen Pract. 2010;60(576):e285–e294. doi:10.3399/bjgp10X514756
60. Vass M, Hendriksen C. Polypharmacy and older people–the GP perspective. Z Gerontol Geriatr. 2005;38(Suppl 1):I14–17. doi:10.1007/s00391-005-1104-1
61. Kouladjian L, Gnjidic D, Reeve E, Chen TF, Hilmer SN. Health care practitioners’ perspectives on deprescribing anticholinergic and sedative medications in older adults. Ann Pharmacother. 2016;50(8):625–636. doi:10.1177/1060028016652997
62. Frølich A, Olsen F, Kristensen I. [Hvidbog Om Multisygdom. Dokumentation Af Multisygdom i Det Danske Samfund - Fra Silotænkning Til Sammenhæng.] In Danish. 2017. Available from: http://Multisygdom.Dk/Wp-Content/Uploads/2017/03/Hvidbog-Til-Net_2_rettet1.Pdf.
63. Nunes BP, Flores TR, Mielke GI, Thumé E, Facchini LA. Multimorbidity and mortality in older adults: a systematic review and meta-analysis. Arch Gerontol Geriatr. 2016;67:130–138. doi:10.1016/j.archger.2016.07.008
64. Bradshaw LE, Goldberg SE, Lewis SA, et al. Six-month outcomes following an emergency hospital admission for older adults with co-morbid mental health problems indicate complexity of care needs. Age Ageing. 2013;42(5):582–588. doi:10.1093/ageing/aft074
65. Klausen HH, Petersen J, Bandholm T, et al. Association between routine laboratory tests and long-term mortality among acutely admitted older medical patients: a cohort study. BMC Geriatr. 2017;17:62. doi:10.1186/s12877-017-0434-3
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.