Back to Journals » Vascular Health and Risk Management » Volume 16
Pattern of Cardiac Diseases and Co-Existing Morbidities Among Newly Registered Cardiac Patients in an Adult Cardiac Referral Clinic of Hawassa University Comprehensive Specialized Hospital, Southern-Ethiopia
Authors Tesfaye S , Shifeta M, Hirigo AT
Received 7 June 2020
Accepted for publication 23 August 2020
Published 23 September 2020 Volume 2020:16 Pages 379—387
DOI https://doi.org/10.2147/VHRM.S266582
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Magnus Bäck
Sisay Tesfaye,1 Mekdes Shifeta,2 Agete Tadewos Hirigo3
1Hawassa University, College of Medicine and Health Science, Faculty of Medicine, Department of Internal Medicine, Hawassa, Ethiopia; 2Hawassa University, College of Medicine and Health Science, Faculty of Medicine, Department of Paediatrics, Hawassa, Ethiopia; 3Hawassa University, College of Medicine and Health Science, Faculty of Medicine, School of Medical Laboratory Sciences, Hawassa, Ethiopia
Correspondence: Sisay Tesfaye
Hawassa University, College of Medicine and Health Science, Faculty of Medicine, Department of Internal Medicine, P.O. Box 1560, Hawassa, Ethiopia
Tel +251-913-938640
Email [email protected]
Background: Currently, cardiovascular diseases (CVDs) are rising in the world and require great concern because the consequences are not only morbidity and mortality, but also a high economic burden. However, the pattern of CVDs in Ethiopia is not well known. Therefore, this study aimed to describe CVD and co-existing morbidities among newly registered cardiac patients in Hawassa University Comprehensive Specialized Hospital.
Methods: A retrospective cross-sectional study was conducted from January 1 to December 31, 2016 among newly registered cardiac patients in an adult cardiac referral clinic. Records and cardiac referral clinic logbooks were used to collect relevant information using structured checklists.
Results: Of the total 310 records of cardiac patients, 236 were explored and included in the study, while the records of 74 patients were absent in the cards room when tracing and/or incomplete to assess cardiac pattern. Rheumatic heart disease (RHD) was the leading cardiac problem and diagnosed in 70 (29.7%) cases followed by non-ischemic cardiomyopathy (55, 23.3%), ischemic heart disease (41, 17.4%), hypertensive heart disease (29, 12.3%), and cor pulmonale (14, 5.9%). The mean age of RHD patients was 28.7 (± 13.1) years. Eighty-two (35%) females and 23 (19.8%) males had RHD, while 69 (29.2%) females and 23 (19.8%) males had non-ischemic cardiomyopathy. The overall rate of mitral stenosis, mitral regurgitation, and aortic regurgitation among patients with RHD were 39 (55.7%), 48 (68.6%), and 26 (37.1%), respectively. Moreover, the overall coexisted morbidity was 81 (34.3%), with a high rate of hypertension alone at 44 (18.6%) followed by hypertension with diabetes at 11 (4.7%).
Conclusion: This study indicated that more than one-third of cardiac patients had at least one of the co-existing morbidities like hypertension, diabetes mellitus, asthma and other diseases. Therefore, careful diagnosis and management of cardiac patients plays an important role to minimize comorbidity-linked complications. Moreover, population-based studies are recommended for better representing and generalization.
Keywords: cardiac diseases, comorbidity, pattern, referral clinic, Hawassa
Introduction
Currently, cardiovascular diseases (CVD) are rising in the world and are a cause for great concern because the consequences are not only a high morbidity and mortality rate but also high economic burden.1 CVD is a principal cause of mortality in the world and about 80% of the deaths occurring in low- and middle-income countries including Sub-Saharan Africa (SSA).2 According to the 2015 World Health Organization (WHO) report, 1.2 million people died in Africa due to CVD,3 and this might be doubled by 2030 with the presence of obesity, hypertension (HTN), and high-risk behaviors like smoking and alcoholism.4 Over 82% of the CVD patients’ deaths are caused by ischemic or coronary heart disease (IHD), stroke (both hemorrhagic and ischemic), hypertensive heart disease (HHD) or congestive heart failure (CHF), peripheral arterial disease, and cardiomyopathy.5 Rheumatic heart disease (RHD) is the utmost common cause of acquired heart disease in children and young adults in the world.6 Besides, acute rheumatic fever (ARF) and RHD are diseases that are mostly linked with poverty, particularly in poor sanitation, overcrowded life situations, with malnutrition and limited access to healthcare.6 The 2015 Global Burden of Diseases (GBD) report indicated 33.4 million people globally were affected by RHD, of them 319,400 had died and almost all of them were from low–middle income countries.6
Different studies reported that patients with cardiovascular diseases might be affected by 43–90% with other cardiovascular or non-cardiovascular comorbid problems including diabetes and chronic kidney disease.7–9 These comorbid conditions could lead to poorer functional status, lower quality-of-life, and even increased morbidity and mortality rates.10,11 CVDs are rising globally and may result in a high economic burden besides its morbidity and mortality mainly in low- to middle-income countries. However, existing comorbidity and patterns of cardiac disease are not well studied in the current study setting. Therefore, this study aimed to describe CVD and co-existing morbidities among newly registered cardiac patients in the adult cardiac referral clinic of Hawassa University Comprehensive Specialized Hospital (HUCSH).
Methods
Study Setting and Study Population
The study was conducted at HUCSH, Hawassa city, Southern-Ethiopia. This teaching hospital was established in 2005 and serves as a training center for health professionals, and providing public healthcare services. In addition, the hospital gives both inpatient and outpatient healthcare services for more than 20 million population in the region, andcurrently, it has more than 400 admission beds. The hospital provides payment free services for delivery of pregnant women, HIV testing, and antiretroviral therapy, TB diagnosis, and treatment. The hospital also provides payment free care services particularly for those who provide an official evidence letter concerning their economic status to be free of care service pay, while others get the care service with a charge of pocket money. Regarding cardiac diagnostic imaging: electrocardiography, echocardiography, CT scan, and chest X-rays are available in the hospital. Besides, there are laboratory tests like lipid profile, cardiac biomarkers (troponin, CK-MB), and other baseline tests are available in the hospital. This retrospective cross-sectional study was conducted from January 1 to December 31, 2016 among 310 newly registered cardiac patients at the adult referral clinic. The cardiac clinic is one of the referral follow-up clinics and it provides services for all cardiac referral cases from different parts of the region, nearby regions, and also from different departments (both inpatients and outpatients) of the same hospital. Patients with cardiac problems aged ≥15 years are referred to the adult cardiac referral clinic and the managed by medical residents, internists, and cardiologists every Thursday. All patients who had cardiac problems aged ≥15 years old and newly registered in the cardiac referral clinic were eligible for the study.
Data Collection and Assessments
Socio-demographic, clinical and echocardiographic data of the study subjects were collected from medical records of all patients with cardiac problems who were referred to the adult cardiac referral clinic of HUCSH using structured checklists. The cardiac referral clinic registration book also was assessed for identifying new cases and to explore the study-related data.
Inclusion and Exclusion Criteria
All cardiac patients with age greater than or equal to 15 years old who were newly registered in the adult cardiac referral clinic from January 1 to December 31, 2016 were included in the study. However, newly registered cardiac patients whose record was incomplete for the assessment of cardiac pattern and those patients whose medical records absent in the cards room when tracing were excluded from the study.
Definition of Terms and Diagnosis
- Adult cardiac clinic: is a unit of the internal medicine department where patients with the cardiac problem and aged ≥15 years are diagnosed for cardiac diseases and followed-up for therapeutic management.
- Acute coronary syndrome is myocardial necrosis in a clinical setting consistent with acute myocardial ischemia (with evidence of cardiac biomarkers, electrocardiogram, and echocardiogram findings).
- Cor pulmonale was defined as an alteration in the structure and function of the right ventricle (RV) of the heart caused by a primary disorder of the respiratory system and triggered by the onset of pulmonary hypertension. The diagnosis was made using two-dimensional echocardiography.
- Pattern of cardiac disease: it is concerned with addressing the frequency and distribution of cardiac disease including its causes in a defined human population.
- Diagnosis of rheumatic heart disease (RHD) was made in the presence of typical echocardiographic rheumatic changes that are consistent with the WHO and World Heart Federation’s guidelines.
- Non-ischemic dilated cardiomyopathy was diagnosed in the presence of dilated left ventricle or biventricular dilation with systolic dysfunction that is not caused by ischemic or valvular heart disease.
- The diagnosis of ischemic heart disease was made using echocardiography (according to the American Society of Echocardiography) to look for regional wall motion abnormalities.
Ethical Considerations
The Institutional Review Board (IRB) of the College of Medicine and Health Sciences of Hawassa University ethically approved the study (Ref No: IRB/069/09). Then permission was obtained from the Academic and Clinical Director office to explore data from patients’ records. This study conformed with the principles established in the Declaration of Helsinki and its following revisions. The ethics committee waived the need for informed consent because the research could not be possible to conduct without the waiver, had vital social value and posed no more than insignificant risks to the study subjects. However, privacy of the study subjects’ personal information was kept utmost.
Statistical Analysis
Data were coded and entered into a statistical package for social science (SPSS) version 20 for statistical analysis. The results were presented as frequency and percentage for categorical variables, and means and standard deviation for continuous quantitative variables.
Results
Socio-Demographic and Cardiac Characteristics of the Study Subjects
Out of the 310 cases with a cardiac problem, the records of 64 (20.6%) patients were absent in the cards room when traced and 10 (3.2%) were incomplete for the assessment of cardiac pattern. The overall 236 complete records of cardiac patients were included in the study. One hundred and twenty (50.8%) were females and the rest 116 (49.2%) were males with mean and standard deviation (SD) age of 43.1±14.6 years old. In relation to age group, 11.4% were 15–19 years, 17.8% were 20–29 years, 13.6% were 40–49 years, 12.7% were 50–59 years, 18.2% were 50–59 years, 17.8% were 60–69 years, and 8.5% were greater than or equal to 70 years.
Patterns of Cardiac Diseases
The leading five cardiac disease etiologies identified were RHD, non-ischemic cardiomyopathy, IHD, HHD, and cor pulmonale. Of the total 236 cardiac patients, 70 (29.7%) were diagnosed as RHD cases, of these 61/236 (25.8%) were diagnosed as RHD alone, and 9/236 (3.8%) were diagnosed as RHD with infective endocarditis (IE). Fifty-five (23.3%) had non-ischemic cardiomyopathy, 41 (17.4%) had IHD, 29 (12.3%) had HHD, and 14 (5.9%) had cor pulmonale. Eighty-two (35%) females and 23 (19.8%) males had RHD, while 69 (29.2%) females and 23 (19.8%) males had non-ischemic cardiomyopathy (Table 1).
 |
Table 1 Pattern of Cardiac Disease and Age of Patients During Registry at the Cardiac Clinic |
From a total of 70 patients with RHD, 65.7% were aged 18–29 years; 27.6% (8/29) of HHD cases were aged ≥70 years; 25.45% (14/55) of non-ischemic cardiomyopathy cases were aged 50–59 years and 42.8% (6/14) of cor pulmonale cases were aged 50–59 years. Besides 39% (16/41) of IHD and 70% (7/10) of degenerative valvular heart disease (DVHD) cases were aged 60–69 years; 44.4% (4/9) of RHD+IE and 33.3% (3/9) of congenital heart diseases, arrhythmia and myocarditis were aged 15–19 years (Table 2).
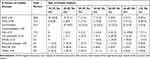 |
Table 2 Pattern of Cardiac Diseases Distribution with the Age of Cardiac Patients |
Echocardiographic (ECHO) Reports of Cardiac Patients
Overall, 70/236 (29.7%) cardiac patients had RHD and their ECHO diagnosis revealed the mitral valve abnormality was the most encountered problem in the rheumatic group and found in all RHD cases. While 26/70 (37.1%) of the patients had aortic valve involved cardiac problem. The ECHO finding indicated the overall 39/70 (55.7%) RHD patients had mitral stenosis (MS), 48/70 (68.6%) had isolated mitral regurgitation (MR), and 26/70 (37.1%) had aortic regurgitation (AR). However, 16/70 (22.8%) had combined MR and MS. Twelve patients (17.1%) had combined MR+MS+AR, 11/70 (4.7%) had combined MR and AR, and 8/70 (11.4%) had isolated MS. Moreover, six (8.6%) males and five (7.1%) females had MR+AR. The mean age of patients during enrollment was 28.6 (±9.6) years for MS; 26.6 (±12.5) years for MS+MR, 29.1 (±15.4) years for MR, 26.3 (±5.7) years for AR+MS, 30 (±13.1) years for MR+AR, and 26.9 (±10.9) years for AR+MS+MR (Figure 1).
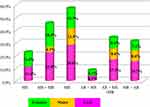 |
Figure 1 Echocardiographic report of RHD patients for the valve(s) involvement. |
Non-ischemic cardiomyopathy was the second commonest cardiac disease and occurred in 55/236 (23.3%) cases. Among them, 49 (89.1%) had dilated cardiomyopathy, four (7.3%) had restricted cardiomyopathy, and two (3.6%) had peripartum cardiomyopathy.
Out of the total cardiac cases, 41/236 (17.4%) had IHD. Among these 41 IHD cases, 27 (65.9%) had acute coronary syndrome (ACS), 12 (29.3%) had ischemic cardiomyopathy, and two (4.9%) had stable angina. Of the total 27 ACS cases, 18 were males and nine were females. Around 8/41 (19.5%) males and 4/41 (9.7%) females had ischemic cardiomyopathy. The mean age and rate of patients with the pericardial disease were 34.9 (±4.3) years and 8/236 (3.4%), in all cases tuberculosis was considered with support of epidemiology and clinical presentation of the patients.
Among 5/236 (2.1%) cases of coronary heart disease (CHD), two of them had patent ductus arteriosus (PDA), one patient had tetralogy of Fallot, one patient had an atrial septal defect (ASD), and one patient had a ventricular septal defect (VSD).
Of 32/236 (13.6%) arrhythmic cases, three of them had isolated arrhythmia without structural lesions on the ECHO study. More than half (68.7%), 4/32 (12.5%), 3/32 (9.4%), and 3/32 (9.4%) of arrhythmic cases had atrial fibrillation (AF), followed by other supraventricular tachycardia (SVT), bradyarrhythmia and ventricular tachycardia, respectively.
The Pattern of Existing Comorbidities Among Cardiac Patients
The overall prevalence of coexisting morbidities among cardiac patients was 81/236 (34.3%). From the total 236 cardiac patients, 44/236 (18.6%) of them had HTN alone, 4.7% had HTN with diabetes mellitus (DM), and 1.27% had HTN with asthma (Table 3).
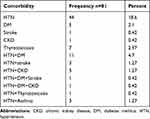 |
Table 3 Pattern of Co-Existed Morbidities Among Cardiac Patients in the Cardiac Referral Clinic |
Of the total 41 IHD cases, 22/41 (53.6%) had comorbid diseases. Among these, 14/41 (34.1%) had HTN alone, 2/41 (4.9%) had DM, and 6/41 (14.6%) of them had HTN and DM. Out of the total 32 arrhythmic patients, 12/32 (37.5%) had a chronic co-morbid illness and, of these, 7/32 (21.9%) had HTN and 3/32 (9.4%) had thyrotoxicosis with AF.
Discussion
Nowadays CVD is a big challenge for the world and needs great attention to manage all aspects of its burden, particularly in developing world countries including Ethiopia. However, the pattern of cardiac disease and co-existing morbidities were not well explored in Ethiopia including the study site. Therefore, this study aimed to describe CVD and co-existing morbidities among patients in an adult cardiac referral clinic.
The Pattern of Cardiac Diseases
In this study, the overall prevalence of RHD was 29.7% and it was the most encountered etiology of cardiac diseases. The finding was nearly comparable with the study conducted in Southwest Ethiopia, which was 32.8%.12 However, the higher rate was reported from Bangalore, South India,13 which was 60.2%, and Southwest Nigeria,14 which was 67.7%. In addition, a lower rate of RHD was reported from several studies like North Ethiopia,15 Southwest Cameroon,16 and Rural Pakistan,17 in which the rates were 11.8%, 6.7%, and 5.7%, respectively. The economic status of the population across countries, access to healthcare, the presence of RHD in the parents, and genetic disparities could also be plausible reasons for the variations across the studies. In support, ARF and RHD diseases are mostly linked with poverty, particularly in poor sanitation, overcrowded living conditions, malnutrition, and limited access to healthcare.6 Moreover, rarely ARF/RHD relative to the frequency of childhood group A streptococci (GAS) infection raises the likelihood of genetic predisposition.18,19
In this study, the second leading cardiac disease etiology was non-ischemic cardiomyopathy (23%). This finding was almost comparable with the rate reported from Southwest Ethiopia,12 which was 20.2%. However, an inconsistent rate of cardiomyopathy was reported in different studies, like 9.54% in Southwest Nigeria,14 9.3% in North Ethiopia,15 17.6% in Southwest Cameroon,16 1.9% in Addis Ababa, Ethiopia,20 and 11.4% in Northwest Cameroon.21 The variation might be due to the difference in the sample size of the study and variations in the incident definitions. Besides, this study highlights a need for further investigation that related to specific risks and etiologies to explain the reason why it becomes more prevalent.
Studies from Southwest Ethiopia,12 Madrid, Spain,22 and 19 European centers23 revealed that RHD was significantly higher in females when compared to males. Similarly, the current study indicated a high rate of RHD among females (35%) when compared to males (16.4%). In addition, in this study overall 55.7% of RHD patients had MS. This finding was comparable with a study conducted in Gondar, North Ethiopia, which indicated 55.8% MS among RHD patients.15 However, a higher rate of MS was identified from RHD in Southwest Ethiopia12 and Bangalore, South India13 in which the rates were 86.0% and 97.4%, respectively. A study report from North Ethiopia15 revealed that the rate of MR, AR, and MS+MR from RHD patients was 59.8%, 33.3%, and 17.6%, respectively. However, the current study indicated 68.6%, 28.6%, and 22.8% of patients with RHD had MR, AR, and MS+MR, respectively.
In this study, the rate of MS was higher among females when compared to males. Likewise, the studies conducted in South India13 and California24 indicated MS was higher among females when compared with males. Besides one study indicated three times more increased occurence of MS in females than males, and females accounted for 70.0% of all cases.25 These reflect our patients might have encountered a delay in medical attention and mitral valvotomy. Further, lack of early detection of the disease at the primary level, poor management of throat infections, and poor rheumatic fever prophylaxis can also increase the problems.26
This study identified that IHD was the third leading cardiac disease etiology (17.4%). This was higher than the studies conducted in Southwest Ethiopia,12 Nigeria,14 North Ethiopia,15 Southwest Cameroon,16 Addis Ababa, Ethiopia,20 and Northwest Cameroon,21 in which the rates were 12%, 1.59%, 6.5%, 9.6%, 6.2%, and 7%, respectively. The variation might be attributed to differences in the study approach, time of the study, and the number of populations included between the studies. In addition, the increased prevalence of conventional risk factors and lifestyle of the community might be a reason.
This study revealed that the proportion of IHD was a little bit higher in males (23.3%) when compared to females (16.7%). This is in line with the studies reported from Northwest Cameroon21 and another study.27 In 2013, the estimated prevalence of IHD was 6.1%, 6.4%, 5.3%, and 3.7% in Caucasian, African, Latino, and Asian populations aged ≥18 years old, respectively.28 In support, IHD is the first ranked and the most common cause of deaths in patients affected by the disease.28
In this study, HHD was the fourth cardiac disease etiology and the rate was 12.3%. The finding was in line with the study conducted in Jimma, which was 12%.29 Conversely, HHD was the second commonest type of heart disease in Southwest Ethiopia,12 it was the first most common heart disease among the study conducted in Northwest Cameroon,21 the rates of which were 24% and 41.1%, respectively. In support, HTN increased from 594 million in 1975 to 1.13 billion in 2015, with a high increase in low- and middle-income countries,30 and is strongly associated with heart diseases like CHD, heart failure, AF, aortic valvular disease, left ventricular hypertrophy, and abdominal aortic aneurysms.31
In the current study, the fifth cardiac disease etiology was cor-pulmonale, which was 5.9%. However, studies reported a variable rate of cor pulmonale: 0.27% in Nigeria,14 2.2% in Gondar, North Ethiopia,15 and 8.8% in Southwest Cameroon.16 Abdominal obesity is an essential risk factor for developing cor pulmonale, an individual’s lifestyle might be a possible reason for the variations, and this is supported by the study reports.32
Co-Existed Morbidities
This study indicated that HTN was a predominant (18.6%) comorbid problem among cardiac patients followed by HTN+DM (4.7%), thyrotoxicosis (2.97%), and DM (2.1%). This might put them to more health complications. Therefore, prevention, screening, early diagnosis, and treatment of comorbid conditions in cardiac patients will improve the health outcomes and quality-of-life for cardiac patients.33
Limitations
First, the study was retrospective by its nature and based on only secondary data and exploring all necessary information including risk factors and clinical conditions are difficult because the study only focused on documented information from patients’ records. Second, this study was an institution based records review; some charts could not be found, and others were not complete. Third, the study was conducted on a single healthcare institute, on only 236 cases, and it might not represent the pattern of the cardiac disease of the general population as a whole. Fourth, the study included patients with more symptomatic cardiac problems, since it was at a referral clinic, and this may cause bias in the assessment of cardiac pattern and coexisted morbidities. Fifth, the study was ethically approved in 2017 and the study conducted subsequently, however a different finding might be observed if records of patients from 2017–2019 were included in the study. Regardless of the described limitations, this descriptive study ultimately adds input for other prospective studies that can be conducted in cardiac diseases.
Conclusion
The study identified that RHD, non-ischemic cardiomyopathy, IHD, HHD, and cor pulmonale were the topmost five cardiac diseases in descending order of frequency. Patients with RHD had a high rate of MR, MS, and AR, and the age of these patients was below 30 years. Besides, HTN, DM, and HTN with DM were the top-three existing comorbid diseases in cardiac patients. Therefore, physicians/clinicians who were working in the cardiac clinic should strongly adhere to the national guidelines for accurate diagnosis and management of cases to limit the severity and complications of the disease as well as to improve their health outcomes. Further, this study is single institution-based and cannot reflect the overall prevalence of comorbidity and pattern of cardiac diseases of the general population. Therefore, population-based studies are recommended for better representing and generalization.
Abbreviations
AR, aortic regurgitation; CKD, chronic kidney disease; DM, diabetes mellitus; DVHD, degenerative valvular heart disease; IE, infective endocarditis; IHD, ischemic heart disease; HHD, hypertensive heart disease; HTN, hypertension; RHD, rheumatic heart disease; MR, mitral regurgitation; MS, mitral stenosis.
Data Sharing Statement
The dataset of this article is available on reasonable request from the corresponding author with the permission of the clinical and academic director of Hawassa University’s comprehensive specialized hospital clinical.
Acknowledgments
We want to acknowledge the nurses who were working in the cardiac referral clinic of Hawassa University comprehensive specialized hospital.
Author Contributions
All authors made substantial contributions to the conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Raji Y, Mabayoje O, Bello T. Familial clustering of risk factors for cardiovascular disease among first-degree relatives of patients with chronic kidney disease in a sub-Saharan African population. Cardiovasc J Afr. 2015;26:11–14. doi:10.5830/CVJA-2015-041
2. World Health Organization Noncommunicable Diseases. Available from: http://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases.
3. WHO. Global Health Estimates 2015: Death by Cause, Age, Sex, by Country and by Region, 2000–2015. Geneva: World Health Organization; 2016.
4. Kariuki JK, Stuart-Shor EM, Leveille SG, Hayman LL. Methodological challenges in estimating trends and burden of cardiovascular disease in sub-Saharan Africa. Cardiol Res Pract. 2015;2015:921021. doi:10.1155/2015/921021
5. WEF (World Economic Forum). The global economic burden of non-communicable diseases. A report by the World Economic Forum and the Harvard School of Public Health. September, 2011. Available from: http://www3.weforum.org/docs/WEF_Harvard_HE_ Global EconomicBurdenNonCommunicableDiseases_2011.pdf.
6. Global Burden of Diseases (GBD). Mortality and causes of death collaborators. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1459–1544.
7. Schmidt M, Jacobsen JB, Johnsen SP, Boøtker HE, Soørensen HT. Eighteen-year trends in stroke mortality and the prognostic influence of comorbidity. Neurology. 2014;82:340–350. doi:10.1212/WNL.0000000000000062
8. McManus DD, Nguyen HL, Saczynski JS, Tisminetzky M, Bourell P, Goldberg RJ. Multiple cardiovascular comorbidities and acute myocardial infarction: temporal trends (1990–2007) and impact on death rates at 30 days and 1 year. Clin Epidemiol. 2012;4:115–123. doi:10.2147/CLEP.S30883
9. Chen HY, Saczynski JS, McManus DD, et al. The impact of cardiac and noncardiac comorbidities on the short-term outcomes of patients hospitalized with acute myocardial infarction: a population-based perspective. Clin Epidemiol. 2013;5:439–448. doi:10.2147/CLEP.S49485
10. Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross sectional study. Lancet. 2012;380(9836):37–43. doi:10.1016/S0140-6736(12)60240-2
11. Vos R, van den Akker M, Boesten J, Robertson C, Metsemakers J. Trajectories of multimorbidity: exploring patterns of multimorbidity in patients with more than ten chronic health problems in life course. BMC Fam Pract. 2015;16:2. doi:10.1186/s12875-014-0213-6
12. Habte B, Alemseged F, Tesfaye D. The pattern of cardiac diseases at the cardiac clinic of Jimma University specialised hospital, south West Ethiopia. Ethiop J Health Sci. 2010;20:2.
13. Manjunath CN, Srinivas P, Ravindranath KS, Dhanalakshmi C. Incidence and patterns of valvular heart disease in a tertiary care high-volume cardiac center: a single center experience. Indian Heart J. 2014;66(3):320–326. doi:10.1016/j.ihj.2014.03.010
14. Ajayi EA, Adewuya OA, Ohunakin AA, Olaoye OB. Echocardiographic pattern of heart diseases at a Southwest Nigerian private clinic. Sahel Med J. 2018;21(3):153. doi:10.4103/smj.smj_19_17
15. Tefera YG, Abegaz TM, Abebe TB, Mekuria AB. The changing trend of cardiovascular disease and its clinical characteristics in Ethiopia: hospital-based observational study. Vasc Health Risk Manag. 2017;13:143. doi:10.2147/VHRM.S131259
16. Nkoke C, Makoge C, Dzudie A, et al. A predominance of hypertensive heart disease among patients with cardiac disease in Buea, a semi-urban setting, South West Region of Cameroon. BMC Res Notes. 2017;10(1):684. doi:10.1186/s13104-017-3034-6
17. Rizvi SF, Khan MA, Kundi A, Marsh DR, Samad A, Pasha O. Status of rheumatic heart disease in rural Pakistan. Heart. 2004;90(4):394–399. doi:10.1136/hrt.2003.025981
18. Carapetis JR, Currie BJ, Mathews JD. Cumulative incidence of rheumatic fever in an endemic region: a guide to the susceptibility of the population? Epidemiol Infect. 2000;124:239–244. doi:10.1017/S0950268800003514
19. Guilherme L, Kohler KF, Postol E, Kalil J. Genes, autoimmunity and pathogenesis of rheumatic heart disease. Ann Pediatr Cardiol. 2011;4:13–21. doi:10.4103/0974-2069.79617
20. Abdissa SG, Oli K, Feleke Y, Goshu DY, Begna DM, Tafese A. Spectrum of cardiovascular diseases among Ethiopian patients at Tikur Anbessa Specialized University Teaching Hospital, Addis Ababa. Ethiop Med J. 2014;52(1):9–17.
21. Akono MN, Simo LP, Agbor VN, Njoyo SL, Mbanya D. The spectrum of heart disease among adults at the Bamenda Regional Hospital, Northwest Cameroon: a semi-urban setting. BMC Res Notes. 2019;12(1):76. doi:10.1186/s13104-019-4803-1
22. Martínez-Sellés M, García-Fernández MA, Moreno M, Larios E, García-Robles JA, Pinto Á. Influence of gender on the etiology of mitral regurgitation. Rev Esp Cardiol (Engl Ed). 2006;59(12):1335–1338. doi:10.1016/S1885-5857(07)60091-7
23. Monteagudo Ruiz JM, Galderisi M, Buonauro A, et al. Overview of mitral regurgitation in Europe: results from the European Registry of mitral regurgitation (EuMiClip). Eur Heart J Cardiovasc Imaging. 2018;19(5):503–507. doi:10.1093/ehjci/jey011
24. Movahed MR, Ahmadi-Kashani M, Kasravi B, Saito Y. Increased prevalence of mitral stenosis in women. J Am Soc Echocardiogr. 2006;19(7):911–913. doi:10.1016/j.echo.2006.01.017
25. Women & Valve Disease. Available from: https://my.clevelandclinic.org/health/diseases/17647-women–valve-disease.
26. Ahmad S, Hayat U, Naz H. Frequency of severe mitral stenosis in young female patients having pure mitral stenosis secondary to rheumatic heart disease. J Ayub Med Coll Abbottabad. 2010;22(4):19–22.
27. Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics–2015 update: a report from the American Heart Association. Circulation. 2015;131(4):e29–322. doi:10.1161/CIR.0000000000000152
28. Abubakar I, Tillmann T, Banerjee A. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;385(9963):117–171.
29. Petros G. Patterns of heart disease Jimma Hospital. Bull JIHS. 1996;6(2):85–92.
30. Hypertension. Available from: https://www.who.int/news-room/fact-sheets/detail/hypertension.
31. Kokubo Y, Matsumoto C. Hypertension is a risk factor for several types of heart disease: review of prospective studies. Adv Exp Med Biol. 2017;956:419–426.
32. Vakhlamov DA, Vakhlamov VA. Priority risk factors of developing cor pulmonale in patients with chronic obstructive pulmonary disease according to correlation analysis findings. Современные Технологии В Медицине. 2016;8(4(eng)).
33. Kendir C, van den Akker M, Vos R, Metsemakers J. Cardiovascular disease patients have increased risk for comorbidity: a cross-sectional study in the Netherlands. Eur J Gen Pract. 2018;24(1):45–50. doi:10.1080/13814788.2017.1398318
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
