Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 16
Pattern, Cause of Childhood Burn injuries and their Management Outcome At Jimma Medical Center, Jimma Zone, Oromia Region, Southwest Ethiopia
Received 10 March 2023
Accepted for publication 8 June 2023
Published 14 June 2023 Volume 2023:16 Pages 1505—1514
DOI https://doi.org/10.2147/CCID.S411693
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jeffrey Weinberg
Zekarias Deribe,1 Diliab Desta2
1Department of Surgery, Faculty of Medical Science, Jimma Medical Center, Jimma, Ethiopia; 2Department of Anatomy, Faculty of Medical Science, Jimma University, Jimma, Ethiopia
Correspondence: Diliab Desta, Email [email protected]
Purpose: Burn injuries are prevalent worldwide, especially in developing countries; and there are significant pediatric burn injuries in Ethiopia. This study was performed to analyze the pattern, cause, and management outcome of burn injuries in Jimma Medical Center.
Methods: A hospital‑based retrospective cross‑sectional study was conducted at Jimma university medical center burn unit. Data were collected through chart review of pediatric patients aged 0 to 14 years who were admitted to the burn unit with a burn injury. A total of 92 hospitalized children were studied from Jan 1, 2020 to Dec 31, 2021 GC. Data were analyzed using SPSS version 25. The statistical significance was determined using odds ratio (OR) with a 95% confidence interval (CI) and the corresponding P-value of less than 0.05.
Results: The majority of the patients were males (52.2%). Scald burn was the most common cause of burn in 57(62.0%). The TBSA of majority of the patients (52.2%) was found to be between 11% and 20%. After adjusting for possible confounders in the multivariate analysis, preexisting illness and time of presentation to care were found to have a statistically significant association with the outcome of burn at discharge (P= 0.007) (P= 0.021) respectively.
Conclusion: The most common cause of burn in our setup was scald burn; upper extremities were also the most affected site. According to our study, the factors associated with the outcome of burn injury were preexisting illness and late presentation to health facilities.
Keywords: childhood burn, outcomes, pediatric, Jimma medical center
Introduction
Background
Burn injuries are among the most important vulnerabilities in children, which can lead to severe functional, social and psychological impairments. In terms of morbidity and disability, burn is a major public health problem throughout the world, especially in low-income countries.1
The term “burn” refers to tissue damage brought on by fire, scald, electricity, sunlight, chemical agents, or nuclear radiation. The most common type of burn is scald burn which can be caused by any hot liquid, including boiling water, hot tap water, coffee or tea, heavier liquids like soup, and even melted butter.2,3
People who have burn wound contractures have limited functional abilities and a lower likelihood of living typical, financially successful lives. According to the WHO, burns caused by fire are the sixth most common cause of mortality for children aged 5 to 14 from low- and middle-income countries.4 The majority of burns occur among children < 14 years of age and children with a low socioeconomic family, and low educational level of the mother are the main demographic factors associated with a high risk of burn injury status.3,5
According to reports, the pattern of burn injuries varies from community to community and is affected by factors such as age, sex, economic level, regional customs, social conditions, and environmental factors.6
According to international statistics, the continent of Africa has the greatest number of pediatric burn admissions and it is also the second most common reason for accidental mortality in African children under the age of five.7 The frequency of burn mortality among children under the age of 14 is nearly four times higher in Africa than among children in the rest of the world. Children who live in poverty are more at risk of burn injuries.8
The total body surface area (TBSA), the depth of the injury, and the location of the injury all affect how severe a burn injury is. A burn’s severity can be determined by estimating its depth and total burned body surface area (TBSA). Additionally, depending on how deeply the skin is damaged, burns are categorized as superficial, partial, and full thickness.9
Children’s burns differ from adults’ burns in a number of ways, including the degree and depth of the burn injury frequently being more severe, the child’s body proportions being different, leading to increased evaporative heat loss, and the child’s fluid requirements generally being higher.10
Children’s dermis is thinner than adults’, hence the consequence of burn will be more severe from any given thermal insult.11
Some of the factors influencing the outcome of burn injuries in children in the pediatric age group in north Ethiopia include fluid resuscitation and the nutritional state of the burn patient. Patients who received inadequate fluid resuscitation within 24 hours had 2.8 times higher risk of being discharged with a complication than those who received adequate fluid resuscitation within 24 hours, and those who were malnourished at admission were 75% less likely to experience complications when they were discharged.12
Sustained research on the epidemiology of burns in many developed and high-income countries such as the United States has made a great contribution to primary and secondary prevention of different kinds of burns . However, many developing or low- and middle-income countries including Ethiopia mostly focus on communicable diseases and burn injuries are given little attention and its epidemiological pattern is not well-studied. For this reason, we were interested in researching this problem using a retrospective design to study pattern, cause, and management outcome in Jimma Medical Center. As there has been no previous study conducted on pediatric burns in JMC, this study will be important and provide data on the prevalence, cause, and effect on society and drive the implementation of more effective burn prevention and management programs throughout the region and country.
Materials and Methods
Study Area and Study Period
The study was conducted in JUMC, Jimma zone, Oromia Region, South west Ethiopia. Jimma town is located about 346 km South west of the capital city, Addis Ababa.
According to information obtained from Jimma town municipality, there is a population of 174,778 of which 87,879 are males and 86,999 are females and 31,000 were children under 5, distributed among 17 kebele. The data were collected between Jan 1, 2020 to Dec 31, 2021 GC.
Study Design
Hospital-based retrospective cross-sectional study design was used.
Study Population
All selected pediatric patients who were admitted to the burn unit of JMC due to a burn injury from Jan 1, 2020 to Dec 2021 GC who received medical/surgical care. Patients’ medical records with illegible handwriting and incomplete data were excluded.
Sample Size
The sample size was calculated by using single population proportion formula by considering the following assumptions: p = 6.4%; prevalence of pediatric burn injury among traumatic injuries in Yekatit 12 Hospital Addis Ababa Ethiopia.13
Where; n = the minimum sample size required, d = Margin of error = 5%, Zα/2 = Standard normal value at (1- α) =1.96.
Total Number of Pediatric Burn Patients per Year: 50 Patients
Sampling Technique
Systematic random sampling with every other patient’s card was selected until the minimum sample size was reached.
Data Collection Instrument and Quality Assurance
Using the medical record number of the patient, all cards of pediatric burn patients were collected from the card office by workers in the office. For this purpose, the card number in the registration book of admission in surgical wards was used. After selecting the cards, the structured format was filled-in by Clinical II students after training on how to extract the necessary information from the cards depending on each variable. The principal investigator provided ongoing supervision each day during the data collection to ensure the quality of data by checking for completeness and consistency.
Data Processing and Analysis
Using SPSS version 25, the acquired data were verified, cleaned up, and analyzed. Based on the scales of the variables, descriptive statistics were conducted and presented using frequency, percentages. To find factors linked to patient outcome during discharge, bivariate and multivariable logistic regression was used. The statistical significance was determined using odds ratio (OR) with a 95% confidence interval (CI) and the corresponding P-value of less than 0.05.
Ethical Consideration
Ethical clearance was obtained from Jimma University Institutional Review Board (IRB). The study was conducted in accordance with the Declaration of Helsinki. The ethics committee waived the requirement for patient’s informed consent to study their medical records because retrospective data were used. The confidentiality of the study participants was taken into consideration prior to the actual data collection by avoiding the names and any other forms of personal identification.
Operational Definition Terms
First degree burn: burn that involves epidermis only.
Second degree burn: burn that involves dermis and epidermis.
Third degree burn: burn that involves muscle and subcutaneous tissue dermis and epidermis.
Length of hospital stay: days including day of admission and day of discharge.
Pediatric age: age from birth to 14 years.
Superficial: involves epidermis and upper dermis.
Deep: involves lower dermis, subcutaneous tissue, deep connective tissue.
Mixed: involves both superficial and deep.
Result
A total of 92 children were included in the study. Out of these, 52.2% (n=48) were males and 47.8% (n=44) were females. Figure 1 shows the age and gender distribution of the children. High number of females were counted in the age group 1–4 but the number of boys were higher in the rest of the age groups.
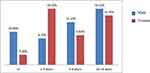 |
Figure 1 Distribution of burns by age and sex. |
Scald burn was the most common cause of burn: 57(62.0%) of the patients followed by flame which accounted for 24(26.1%) (Figure 2). Most of the scald burn injuries were more common in the age group 1–4 years (84.6%) and from all types of burn scald burn accounted for 60.4% in male and 63.6% in female children (Figure 3).
 |
Figure 2 Distribution of the cause of burn by age. |
 |
Figure 3 Distribution of the cause of burn by sex. |
The TBSA of the majority of patients (52.2%) was found to be between 11% and 20% followed by TBSA <10% which accounted for 26(28.3%) (Figure 4). Majority of burns (29.3%) were single site which involved the upper extremity followed by multiple site injury (27.2%), while burn injury on the face was less common (4.3%) (Figure 5).
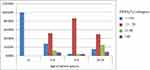 |
Figure 4 Distribution of pediatric burn by TBSA%. |
 |
Figure 5 Distribution of pediatric burn site of injury by the age of patients. |
Forty-two (45.7%) burn patients presented early (before 24 hours), 12 (13%) presented after 72 hrs. Most of the patients (41.3%) stayed in hospital for 15–30 days and patient stays of longer than 60 days were less common (10.9%). Based on the classification of the degree of burn of patients, 69 (75%) had second degree burn. Conservative treatment only with analgesics, antibiotics, tetanus toxoid, topical antimicrobial agents, antiseptics and wound dressing was performed in 39 (42.4%) patients. Surgical treatment was performed in 53 (57.6%) patients; of these, 33 (35.9%) patients underwent wound debridement, 16 (17.4%) underwent skin grafting, 4 (4.3%) underwent amputation. Most of the burns (78.3%) healed, from those who survived some healed with physical disability and 20 (21.7%) patients died at discharge (Table 1).
 |
Table 1 Distribution of the Pediatric Burn Patients, Length of Hospital Stay, Timing of Care, Degree of Burn, Burn Depth, Treatment Modalities, and Patient Outcome at Discharge |
In the bivariate analysis, age, degree of burn, TBSA, LOHS, preexisting illness, time of presentation for care, distance traveled, inhalational injury, burn depth, degree of severity of burn injury, management done, were found to be statistically significant regarding burn outcome at discharge. After adjusting for the possible confounders in the multivariate analysis, only preexisting illness and time of presentation for care were found to have a statistically significant association with outcome of burn at discharge (P= 0.007) (P= 0.021) respectively. Patients who had preexisting illness had an 8.729 times higher chance of death than patients without preexisting illness (AOR = 8.729; 95% CI (1.794–42.460)) and the odds of dying from burn was 9.63 times more likely in patients who got management care after 72 hrs when compared to those who got management care before 24 hrs (AOR = 9.635; 95% CI (1.403–66.180)) (Table 2).
 |
Table 2 Bivariate and Multivariable Logistic Regression Model |
Discussion
Burn injuries are a major burden that primarily affects the world’s poor. Around 95% of burn injuries caused by fires take place in low- and middle-income nations. However, childhood burn injuries are becoming less common in Western nations as a result of safety measures and preventive programs.4,14
Our findings showed that the male to female ratio was 1.09:1 which is in agreement with other studies.3,10,15–18 The hyperactive nature of male babies in comparison to female babies may be one explanation for the study’s predominance of male participants.
According to our findings, scald (62.0%) was the main cause of burn injuries. This is similar to some studies done in Iran, Tanzania, USA.3,10,17,19 This is due to the fact that children may not be able to accurately identify danger, they may have less environmental control, and they may not be able to leave a burn situation that poses a threat to their lives.
Majority of patients in this study had burns with an extent of 11–20% of TBSA, burn injuries that covered >40% of TBSA were seen in 6.5% of the individuals, this finding is comparable with a study conducted in Jimma medical center in which burn extent in 55.67% of the patients was between 10–20% TBSA.20
According to the current study, extremities are the most commonly burned anatomical sites, particularly upper extremities, whereas burn injuries on the face were the least common. This is aligned with the study done in Peshawar in which upper extremities burns accounted for 29.7%, but lower extremity burns made-up 34.4.16 These may be due to sample size variation. Even though there is variation in percentage, most of the studies reported extremities are common anatomical site which is more affected.12,17,19,21 This can be because extremities are affected due to manipulation of different objects and the falling of boiled liquids affect lower extremities.
Compared to other reports, the mortality rate in this study was similar to a study done in India,22 but quite higher compared to other reports from Iran, Tanzania, India.3,10,23,24 This is because children who received outpatient treatment for mild burn injuries were left out of the study. In addition, because our facility serves as a referral center, a lot of patients from other hospitals who are in the latter stages of septicemia are admitted there and it may be because of different sample size.
Majority of the patients in this study were managed conservatively. Surgical treatment like wound debridement (35.9%) and skin grafting (17.4%) was performed, similar to a study reported in Tanzania,10 but surgical treatment was commonest treatment used India.25 This discrepancy may be due to the setup of the hospital in which only patients who need plastic surgery were referred to this unit in India.
In the bivariate analysis, age, degree of burn, TBSA, LOHS, preexisting illness, time of presentation to care, distance traveled, inhalational injury, burn depth, degree of severity of burn injury, management done, were found to have a statistically significant association with burn outcome at discharge, this is consistent with study conducted in Ethiopia, Ayder Referral Hospital12 and in Kuwait.26
In the multivariate analysis, preexisting illness and time of presentation to care were found to behave a statistically significant association with outcome of burn at discharge (P= 0.007) (P= 0.021) respectively, this is consistent with a study conducted in patients who have preexisting illness who had an 8.729 times higher chance of dying than patients without preexisting illness, which is in line with research done in Ethiopia, South Gondar zone government hospitals.24 This is in line with the scientific rationale that patients with burn injuries who exhibit poor clinical outcomes are likely suffering from severe fluid loss, anemia, infection, increased catabolism, and/or decreased intake, all of which might ultimately cause the victim to eventually die.27 Unlike this study, in a study from Tanzania,10 preexisting illness had no significant correlation with death associated with childhood burn. The discrepancy might be due to focusing on/giving attention to only the presented illness (burn) of the patient in our setup because of the absence of multi-disciplinary care within the burn unit.
The odds of dying from a burn injury were 9.63 times higher in patients who received care after 72 hrs when compared to those who received care before 24 hrs. Similarly, a study conducted in Tanzania10 showed that delayed presentation after burn injury raises the risk of death. On the contrary, in other studies in Ethiopia12,24 late presentation after burn injury was not statistically significant. This discrepancy might be because of categorization of late presentation and early presentation of burn injury in our study and in the mentioned studies.
Conclusion
In our setup, burn injuries are a significant cause of child morbidity and mortality. The most common cause of burn in our setup was scald burn followed by flame injuries and the most commonly affected sites of burn injury were upper extremities. According to the current findings, burn-affected TBSA of patients was between 11% and 20%. The factors associated with the outcome of burn injury according to our study were preexisting illness and late presentation to health facilities. Our recommendation, based on the finding, is that there has to be awareness creation and education of the community on the prevention and pre-hospital handling of burn patients. In most circumstances, excellent results can be achieved for burn patients with appropriate and prompt treatment.
Limitation of the Study
Since this study was retrospective, it was not possible to include other features that could only be evaluated by observation or history taking. Due to the time and financial feasibility, the sample size was relatively small and it was from a single institution. In addition, children who were not admitted to the pediatric burn unit were not included in the study. Therefore, generalizing of the findings to the population and other health facilities will be difficult.
Acknowledgments
Firstly, we would like to express our deepest gratitude to the Jimma University for ethical approval. Our gratitude and appreciation are extended to the data collectors, supervisors, Jimma Medical center for their cooperation during data collection.
Disclosure
Authors declare that they have no conflicts of interest in this work.
References
1. Peck M, Molnar J, Swart D. A global plan for burn prevention and care. Bull World Health Organ. 2009;87(10):802–803. doi:10.2471/blt.08.059733
2. Srivastava P, Durgaprasad S. Burn wound healing property of Cocos nucifera: an appraisal. Indian J Pharmacol. 2008;40(4):144. doi:10.4103/0253-7613.43159
3. Torabian S, Saba M. Epidemiology of paediatric burn injuries in Hamadan, Iran. Burns. 2009;35(8):1147–1151. doi:10.1016/j.burns.2009.06.194
4. World health Organization. A WHO Plan for Burn Prevention and Care. World health Organization; 2008.
5. Duke J, Wood F, Semmens J, et al. A study of burn hospitalizations for children younger than 5 years of age: 1983–2008. Pediatrics. 2011;127(4):e971–e977. doi:10.1542/peds.2010-3136
6. Al-Shehri M. The pattern of paediatric burn injuries in Southwestern, Saudi Arabia. West Afr J Med. 2004;23(4):294–299. doi:10.4314/wajm.v23i4.28144
7. Forjuoh SN. Burns in low-and middle-income countries: a review of available literature on descriptive epidemiology, risk factors, treatment, and prevention. Burns. 2006;32(5):529–537. doi:10.1016/j.burns.2006.04.002
8. World Health Organization. Injuries, Violence Prevention Department, World Health Organization, World Health Organization. Department of Injuries, Violence Prevention. The Injury Chart Book: A Graphical Overview of the Global Burden of Injuries. World Health Organization; 2002.
9. Pham TN, Cancio LC, Gibran NS. American Burn Association practice guidelines burn shock resuscitation. J Burn Care Res. 2008;29(1):257–266.
10. Chalya PL, Mabula JB, Dass RM, et al. Pattern of childhood burn injuries and their management outcome at Bugando Medical Centre in Northwestern Tanzania. BMC Res Notes. 2011;4:1–10.
11. Lowell G, Quinlan K, Gottlieb L. Preventing unintentional scald burns: moving beyond tap water. Pediatrics. 2008;122(4):799–804. doi:10.1542/peds.2007-2979
12. Alemayehu S, Afera B, Kidanu K, Belete T. Management outcome of burn injury and associated factors among hospitalized children at Ayder Referral Hospital, Tigray, Ethiopia. Int J Pediatr. 2020;2020. doi:10.1155/2020/9136256
13. Tadele A. Magnitude, clinical presentation, and outcome of pediatric burn injuries at Yekatit 12 hospital, Addis Ababa, Ethiopia. Addis Ababa University; 2014.
14. Atiyeh BS, Costagliola M, Hayek S. Burn prevention mechanisms and outcomes: pitfalls, failures and successes. Burns. 2009;35(2):181–193.
15. Rahmani F, Ebrahimi Bakhtavar H, Zamani A, Abdollahi F, Rahmani F. Demographic features of pediatric patients with burn injuries referred to the emergency department of Sina hospital in Tabriz, Iran, in 2014. J Clin Med Res. 2017;5(1):4–8.
16. Aslam M, Niazi MZ, Khan I. Epidemiology of paediatric burns at Lady Reading hospital Peshawar. Pak J Surg. 2017;33(1):87–91.
17. Alharthy N, Al Mutairi M, AlQueflie S, et al. Pattern of burns identified in the pediatrics emergency department at King Abdul-Aziz Medical City: Riyadh. J Nat Sci Biol Med. 2016;7(1):16. doi:10.4103/0976-9668.175019
18. Kazemzadeh J, Vaghardoost R, Dahmardehei M, et al. Retrospective epidemiological study of burn injuries in 1717 pediatric patients: 10 years analysis of hospital data in Iran. Iran J Public Health. 2018;47(4):584.
19. Lee CJ, Mahendraraj K, Houng A, et al. Pediatric burns: a single institution retrospective review of incidence, etiology, and outcomes in 2273 burn patients (1995–2013). J Burn Care Res. 2016;37(6):e579–e585.
20. Mulugeta T, Alemayehu H, Gerema U. Clinical profiles and the outcomes of burn patients admitted to the burn unit of Jimma Medical Center. Clin Cosmet Investig Dermatol. 2021;14:859–866. doi:10.2147/CCID.S322486
21. Ahmad M. Pakistani experience of childhood burns in a private setup. Ann Burns Fire Disasters. 2010;23(1):25.
22. Mukerji G, Chamania S, Patidar G, Gupta S. Epidemiology of paediatric burns in Indore, India. Burns. 2001;27(1):33–38. doi:10.1016/s0305-4179(00)00058-9
23. Maghsoudi H, Samnia N. Etiology and outcome of pediatric burns in Tabriz, Iran. Burns. 2005;31(6):721–725. doi:10.1016/j.burns.2005.02.003
24. Tiruneh CM, Belachew A, Mulatu S, et al. Magnitude of mortality and its associated factors among Burn victim children admitted to South Gondar zone government hospitals, Ethiopia, from 2015 to 2019. Ital J Pediatr. 2022;48(1):1–8.
25. Kumar P, Chirayil PT, Chittoria R. Ten years epidemiological study of paediatric burns in Manipal, India. Burns. 2000;26(3):261–264. doi:10.1016/s0305-4179(99)00109-6
26. Sharma PN, Bang RL, Al-Fadhli AN, Sharma P, Bang S, Ghoneim I. Paediatric burns in Kuwait: incidence, causes and mortality. Burns. 2006;32(1):104–111.
27. Behrman RE, Vaughan VC
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.