Back to Journals » Clinical Interventions in Aging » Volume 17
Patients with Kashin-Beck Disease Obtained Lower Functional Activities but Better Satisfaction Than Patients with Osteoarthritis After Total Knee Arthroplasty: A Retrospective Study
Authors Zhang L, Li H , Bai L, Ji N
Received 1 September 2022
Accepted for publication 9 November 2022
Published 22 November 2022 Volume 2022:17 Pages 1657—1662
DOI https://doi.org/10.2147/CIA.S388401
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Maddalena Illario
Liangzhi Zhang,1 Hui Li,1,2 Lulu Bai,1,2 NaiChun Ji1
1Department of Sports Health Research Center, Xi ‘an Medical University, Xi’an City, People’s Republic of China; 2Department of Knee Surgery, Hong Hui Hospital, Xi’an Jiaotong University, Xi’an City, People’s Republic of China
Correspondence: Hui Li, Department of Sports Health Research Center, Xi ‘an Medical University, Xinwang Road, Xi’an City, 710021, Shaanxi Province, People’s Republic of China, Tel/Fax +86-18092901809, Email [email protected]
Background: Increasingly, patient satisfaction after total knee arthroplasty (TKA) is being recognized as an important measure of health-care quality in osteoarthritis (OA) patients. But satisfaction after TKA has not yet been reported in Kashin-Beck disease (KBD). We aim to examine satisfaction and clinical efficacy of TKA in the treatment of OA and KBD.
Methods: Retrospectively review of 37 KBD patients (45 knees) and 52 OA patients (58 knees) who underwent TKA from January 2015 to January 2017. Data of outcome measures such as Knee Society knee score (KSKS) and function score (KSFS), Western Ontario and McMaster Universities Arthritis Index (WOMAC), and radiographic evaluation were collected preoperatively and during the last follow-up. Satisfaction was compared using the 2011 Knee Society Scoring System.
Results: There were no differences in age, gender, BMI and Follow-up time. KBD patients had significantly worse preoperative range of motion, KSKS, and mechanical lateral distal femoral angle (mLDFA) compared with OA patients (P < 0.05). At the last follow-up, the KSKS, KSFS, WOMAC score, and radiographic parameters of all patients significantly improved (P < 0.05), but the satisfaction was higher in KBD patients than in OA (P < 0.05). Further analysis showed that KSFS, WOMAC total, pain, stiffness, and function scores were significantly worse for KBD (P < 0.05).
Conclusion: Patient satisfaction was greater but clinical outcomes were inferior in KBD than in OA. This study also demonstrated that TKA is an effective surgical procedure for KBD, but how to improve functional outcomes needs to be further studied.
Keywords: Kashin-Beck disease, osteoarthritis, total knee arthroplasty, satisfaction
Introduction
Kashin-Beck disease (KBD) is an endemic, deformable and progressively symmetrical joint disease, which is often affected in the knee. The severe knee pain and functional limitations can seriously affecting the quality of life in patients with late-stage KBD.1,2 Total knee arthroplasty (TKA) is an effective surgical procedure which relieving pain, re-aligning the lower limb, increasing the range of motion, and improving the function and quality of daily life for late-stage KBD and osteoarthritis (OA).3,4 With aging, the number of TKA procedures performed continues to increase year on year.5 However, overall assessments of previous TKA focus on successful and comparable physician-assessed objective clinical outcomes and longevity.6
Increasingly, patient satisfaction is increasingly being accepted as an essential part of postoperative outcome assessments. Satisfaction with TKA likely extends beyond physician-assessed objective clinical outcomes, but rather relates to other factors, such as expectations.7,8 Among patients undergoing TKA, patient dissatisfaction rates of 10–20% have been consistently reported.9,10 Many factors, to date, such as age, persistent pain, functional limitation, lower preoperative quality of life and expectations, and postoperative complications are possible reasons for patient dissatisfaction after TKA.11 However, most studies were derived from OA patients, and the KBD patient satisfaction after TKA remains to be investigated. Therefore, it remains unclear whether satisfaction and clinical outcome of TKA performed in KBD and OA patients is the same or not. Due to the pathogenesis difference between KBD and OA in many aspects, there may be differences in postoperative satisfaction and clinical outcomes in TKA.
In this study, we retrospectively reviewed a prospectively maintained database case-matched cohort to examine satisfaction and clinical efficacy of TKA in the treatment of OA and KBD.
Materials and Methods
Patients
This was an IRB-approved retrospective study by Xi’an Honghui Hospital, and written informed consent was obtained. The eligibility criteria were as follows: (a) diagnosed KBD or OA, according to the clinical criteria,12,13 (b) patients who had late-stage KBD or OA and severe knee pain, (c) had a Kellgren–Lawrence radiographic classification of more than III in knee,14 and (d) follow-up time more than 2 years. The exclusion criteria were as follows: (a) had any abnormal vital signs affecting the joint, (b) patients with other knee diseases, such as rheumatoid arthritis, post trauma of knee, and metabolic bone disorders, and (c) patients with other joints involvement in the lower extremity, such as hip and ankle.
Surgical Technique
All TKAs were performed by the same senior surgeon. After admission, patient education, and pre-operative evaluations were performed. Under general anaesthesia, a standard midline incision and medial parapatellar approach were routinely adopted, and intra-articular osteophytes and soft tissues were subsequently removed. The distal femoral and proximal tibial plateau resections were, respectively, made using an intramedullary alignment and extramedullary guide system. Intraoperatively, we obtained a relatively accurate mechanical axis and osteotomy plane of the lower extremity using double calibration of the tibial anterior crest and tendon. Soft-tissue balance was adjusted to achieve optimum knee kinematics. The implant used was a cemented postero-stabilized total knee prosthesis (United Orthopedic, Taipei, Taiwan). After prosthesis installation, the wound was sutured in the flexed position without drainage.
Post-Operative Rehabilitation Protocol
Oral NSAIDs were routinely administered for postoperative pain relief. All patients underwent pressure dressing and cryotherapy for 24 hours. The CPM machine was used after two days postoperatively. Guided active functional exercises were gradually increased. Post-operative radiography was performed before discharge and at the final follow-up. After discharge, patients continued to undergo rehabilitation programs to progressively re-establish muscle strength and balance. All postoperative rehabilitations were administered by the same physiotherapist.
Outcome Assessment
The demographic characteristics, such as age, gender, BMI, follow-up time, and the patient-reported outcome measures, such as the Knee Society knee score (KSKS) and function score (KSFS), and Western Ontario and McMaster Universities osteoarthritis index (WOMAC) were collected and assessed by an independent observer at preoperation and final follow-up. Satisfaction scores of the 2011 Knee Society Scoring System were compared at the final follow-up. The satisfaction sub-scale consisted of five items scored from 0 to 5 points, with a maximum score of 40 points. We adopted criteria of Van Onsem to define a total score >20 as satisfactory.15
Radiological Evaluation
All radiological parameters were measured on standing full-leg radiographs before and at the final follow-up. The hip-knee-ankle (HKA), mechanical lateral distal femoral angle (mLDFA), and mechanical medial proximal tibial angle (mMPTA) were assessed by an experienced observer.
Statistical Analysis
The data were analysed using SPSS (version 22.0; SPSS, Inc., Chicago, IL, USA). The distributions of variables were tested with the Kolmogorov–Smirnov test. Normally distributed continuous data were expressed as means ± standard deviations, and assessed using a t-test. Categorised data were expressed as rates, and the Pearson’s χ2 test was used. Statistical significance was set at P < 0.05.
Results
Baseline Characteristics
A total of 37 KBD patients (45 knees) and 52 OA patients (58 knees) treated with TKA were enrolled from January 2015 to January 2017. All patients were followed more than 2 years. The average follow-up time for KBD was 44.18±7.58 months and for OA was 42.84±6.59 months. Preoperatively, there were no differences in age, gender, BMI and follow-up time (P > 0.05) (Table 1).
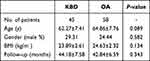 |
Table 1 Demographic Characteristics of Patients |
Clinical Evaluation
The KSKS, KSFS, and WOMAC score were significantly improved in all patients at the last follow-up (P < 0.05). At baseline, KBD had significantly worse preoperative range of motion (ROM) and KSKS (P < 0.05), but at the final follow-up, the ROM and KSKS were equivalent for both groups (P > 0.05) (Table 2).
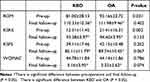 |
Table 2 Preoperative and Postoperative Variables for ROM, KSKS, KSFS, and WOMAC |
At the final follow-up, the satisfaction score of KBD patients was noticeably better than that in OA patients (P < 0.05). However, further analysis showed that the KSFS, and WOMAC total, WOMAC pain, WOMAC stiffness, and WOMAC function scores were significantly worse in KBD patients than in OA patients (P < 0.05) (Table 3).
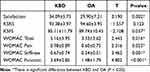 |
Table 3 Postoperative Variables for Satisfaction and Function |
Radiographic Assessment
Postoperative radiography revealed that lower limb alignment was significantly improved, and prosthesis components were well-fixed. At preoperation, except for the mLDFA (KBD, 92.16 ± 2.60; OA, 90.85 ± 2.12; P < 0.05), there were no statistically significant differences between the two groups. At the final follow-up, HKA, mLDFA, and mMPTA significantly improved (P < 0.05), with no difference between the two groups (Table 4).
 |
Table 4 Radiographic Outcomes |
Discussion
Recent researches indicated that KBD patients could achieve excellent clinical outcomes after TKA and no longer lag behind OA at the follow-up, despite having different pathogenesis in many aspects.16 Patient satisfaction is increasingly gaining significance as a quality metric in today’s healthcare environment, and the rates of OA patient after TKA have ranged from 80% to 93%.8,17 However, it is still unclear whether the satisfaction of TKA performed in KBD patients and OA patients is the same or not. In this study, we retrospectively evaluated the efficacy and satisfaction of TKA in the treatment of OA and KBD, and revealed that KBD patients achieve better satisfaction but lower functional activities as compared to OA patients after TKA. In this study, we found that the satisfaction score of patients in the KBD group was significantly higher than that in the OA group. Patient satisfaction with TKA likely extends beyond physician-assessed objective clinical outcomes, but rather relates to other factors such as age, persistent pain, functional limitation, lower pre-operative quality of life and preoperative expectations.18 To the best of our knowledge, only a few studies have investigated the clinical efficacy of KBD after TKA and compared with OA. Liu. et al16 reported that despite worse pre-operative function in KBD, the clinical efficacy was quite similar to OA at the final follow-up. Jin. et al19 and Ling. et al20 indicated that the pain and function were significantly improved in KBD, but the clinical efficacy was still poor compared with OA. However, it is still unclear whether satisfaction with TKA performed in KBD and OA patients is the same or not. In our study, KBD patients achieve greater satisfaction than that in the OA patients. Marked alleviation of pain and clinical efficacy after KBD TKA might be contributed to the satisfaction. Poor pre-operative status in KBD is closely associated with worse pain and function, because it has a long course of disease. KBD more commonly occurred in childhood and progressively aggravated, and might be involved multiple joint damage.21 In addition, previous studies have revealed that knee pain in OA patients probably involved central sensitization.22 In contrast, nociceptive pain in KBD patients possibly involved synovial inflammation, and the prevalence of central sensitization of pain was low, which may be related to greater satisfaction than that in the OA patients.
At the final follow-up, the KSFS and WOMAC total, pain, stiffness, and function scores were significantly worse in KBD patients than in OA patients. There are severe reasons may contribute to the outcome of KBD after TKA. First, KBD is a deformable and systematic disease that mainly involves multiple joints, such as the shoulder, elbow, wrist, hip, knee, ankle, and interphalangeal joints. Although the knee is the most commonly affected, with an incidence of approximately 93%,1,23 TKA alone cannot solve all joint problems in patients. In contrast, OA has been defined as a “wear and tear” disease, which is characterized by the degradation of articular cartilage and involved in partly joints.24 Second, with the development of the disease from childhood, KBD patients often suffer from severe muscle atrophy, and their poor muscle volume and strength may lead to poor postoperative results.19 Finally, post-operative rehabilitation exercise is an important factor for achieving a good curative effect.25 Unfortunately, KBD patients are mostly from remote mountainous areas, economically backward, with low level of education, and poor medical care, which may not achieve good effect of rehabilitation function exercise, resulting in poor postoperative function and activity ability.
In clinical practice, radiography is an important objective index for diagnosing and evaluating bone and joint diseases and surgical results.26 We found that post-operative radiographs of KBD patients were similar to those in OA patients. Currently, despite the debate of the relationship between neutral mechanical alignment and clinical outcomes is continuing, the neutral mechanical lower limb alignment remains the gold standard and target for TKA.27 Thus, for KBD patients, we intraoperatively obtained a relatively accurate mechanical axis and osteotomy plane of the lower extremity using double calibration of the tibial anterior crest and tendon. This study had several limitations. We performed a retrospective database review of a prospectively maintained database case-matched cohort, with a relatively long follow-up time. In addition, our cases were obtained from a single center, and are small in number. Although there are many patients with KBD in China, most are located in low-income remote areas. Due to the sample size, and without adjusting for potential confounders and mediating factors conclusions from the study should be further supported by multi-center research on large data in the future. Finally, this study demonstrates that TKA can significantly improve the symptoms and function of patients with KBD, but how to improve postoperative mobility and stiffness needs to be further studied.
Conclusions
Patient satisfaction was greater but clinical outcomes were inferior in KBD than in OA. As the poor functional activity was evident in KBD patients, to improve functional outcome should be further studied for KBD TKA.
Abbreviations
KBD, Kashin-Beck disease; OA, osteoarthritis; TKA, Total knee arthroplasty; KSKS, Knee Society knee score; KSFS, Knee Society function score; WOMAC, Western Ontario and McMaster Universities Arthritis Index score; HKA, hip-knee-ankle; mLDFA, mechanical lateral distal femoral angle; mMPTA, mechanical medial proximal tibial angle; ROM, range of motion.
Ethics Approval and Informed Consent
This study was reviewed and approved by the ethics committee of Xi’an Honghui Hospital. All methods of this study were carried out in accordance with the relevant guidelines. The authors confirm that all human data comply with the requirements of the ethics committee of Xi’an Honghui Hospital.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Li Y, Zhou Z, Shen B, et al. Clinical features of Kashin-Beck disease in adults younger than 50 years of age during a low incidence period: severe elbow and knee lesions. Clin Rheumatol. 2013;32(3):317–324. doi:10.1007/s10067-012-2115-0
2. Hinsenkamp M. Kashin-Beck disease. Int Orthop. 2001;25(3):133. doi:10.1007/s002640000177
3. Price AJ, Alvand A, Troelsen A, et al. Knee replacement. Lancet. 2018;392(10158):1672–1682. doi:10.1016/s0140-6736(18)32344-4
4. Wu Y, Zeng Y, Bao X, et al. Comparison of mini-subvastus approach versus medial parapatellar approach in primary total knee arthroplasty. Int J Surg. 2018;57:15–21. doi:10.1016/j.ijsu.2018.07.007
5. Sloan M, Premkumar A, Sheth NP Projected volume of primary total joint arthroplasty in the U.S., 2014 to 2030. J Bone Joint Surg Am 2018;100(17):1455–1460.
6. Ismail MS, Shokri AA, Sharifudin MA, Rahman SA. Pre-operative physiotherapy and short term functional outcome of primary total knee arthroplasty.
7. Hirata A, Ogura T, Hayashi N, et al. Concordance of patient-reported joint symptoms, physician-examined arthritic signs, and ultrasound-detected synovitis in rheumatoid arthritis. Arthritis Care Res. 2017;69(6):801–806. doi:10.1002/acr.23006
8. Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KDJ. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res. 2010;468(1):57–63. doi:10.1007/s11999-009-1119-9
9. Robertsson O, Dunbar M, Pehrsson T, Knutson K, Lidgren L. Patient satisfaction after knee arthroplasty: a report on 27,372 knees operated on between 1981 and 1995 in Sweden. Acta Orthop Scand. 2000;71(3):262–267. doi:10.1080/000164700317411852
10. Wylde V, Learmonth I, Potter A, Bettinson K, Lingard E. Patient-reported outcomes after fixed- versus mobile-bearing total knee replacement: a multi-centre randomised controlled trial using the Kinemax total knee replacement. J Bone Joint Surg Br. 2008;90(9):1172–1179. doi:10.1302/0301-620x.90b9.21031
11. Choi YJ, Ra HJ. Patient satisfaction after total knee arthroplasty. Knee Surg Relat Res. 2016;28(1):1–15. doi:10.5792/ksrr.2016.28.1.1
12. Xiong G. Diagnostic, clinical and radiological characteristics of Kashin-Beck disease in Shaanxi Province, PR China. Int Orthop. 2001;25(3):147–150. doi:10.1007/s002640100248
13. Singh JA, O’Byrne M, Harmsen S, Lewallen D. Predictors of moderate-severe functional limitation after primary Total Knee Arthroplasty (TKA): 4701 TKAs at 2-years and 2935 TKAs at 5-years. Osteoarthritis Cartilage. 2010;18(4):515–521. doi:10.1016/j.joca.2009.12.001
14. Kellgren JH, Lawrence JS. Radiological assessment of osteoarthritis. Ann Rheum Dis. 1957;16:499–502.
15. Van Onsem S, Van Der Straeten C, Arnout N, Deprez P, Van Damme G, Victor J. A new prediction model for patient satisfaction after total knee arthroplasty. J Arthroplasty. 2016;31(12):2660–7.e1. doi:10.1016/j.arth.2016.06.004
16. Liu HM, Wang YF, Wu JM, et al. A comparative study of clinical effect of total knee arthroplasty in the treatment of primary osteoarthritis and osteoarthritis of Kashin-Beck disease. Int Orthop. 2020;44(9):1719–1726. doi:10.1007/s00264-020-04542-9
17. Dunbar M, Richardson G, Robertsson O. I can’t get no satisfaction after my total knee replacement: rhymes and reasons. Bone Joint J. 2013;95-B95-B:148–152. doi:10.1302/0301-620x.95b11.32767
18. Nishitani K, Furu M, Nakamura S, et al. No differences in patient-reported outcomes between medial pivot insert and symmetrical insert in total knee arthroplasty: a randomized analysis. Knee. 2018;25(6):1254–1261. doi:10.1016/j.knee.2018.08.005
19. Jin Z, Yang Y, Xu C, et al. Outcomes of total knee arthroplasty in the adult Kashin-Beck disease with severe osteoarthritis. Int Orthop. 2019;43(2):323–331. doi:10.1007/s00264-018-4029-1
20. Ling M, Wu X, Chang Y, et al. Staged total knee arthroplasty for bilateral complex knee deformities from Kashin-Beck disease and skeletal dysplasia. Knee. 2017;24(3):692–698. doi:10.1016/j.knee.2016.11.011
21. Huang Q, Zhou Z, Ma J, et al. The arthropathic and functional impairment features of adult Kashin-Beck disease patients in Aba Tibetan area in China. Osteoarthritis Cartilage. 2015;23(4):601–606. doi:10.1016/j.joca.2015.01.005
22. Lluch E, Torres R, Nijs J, Van Oosterwijck J. Evidence for central sensitization in patients with osteoarthritis pain: a systematic literature review. Eur J Pain. 2014;18(10):1367–1375. doi:10.1002/j.1532-2149.2014.499.x
23. Mathieu F, Begaux F, Suetens C, De Maertelaer V, Hinsenkamp M. Anthropometry and clinical features of Kashin-Beck disease in central Tibet. Int Orthop. 2001;25(3):138–141. doi:10.1007/s002640000192
24. Cunningham N, Kashikar-Zuck S. Nonpharmacological treatment of pain in rheumatic diseases and other musculoskeletal pain conditions. Curr Rheumatol Rep. 2013;15(2):306. doi:10.1007/s11926-012-0306-y
25. Brennan GP, Fritz JM, Houck LT, Hunter SJ. Outpatient rehabilitation care process factors and clinical outcomes among patients discharged home following unilateral total knee arthroplasty. J Arthroplasty. 2015;30(5):885–890. doi:10.1016/j.arth.2014.12.013
26. Moreland JR, Bassett LW, Hanker GJ. Radiographic analysis of the axial alignment of the lower extremity. J Bone Joint Surg Am. 1987;69(5):745–749. doi:10.2106/00004623-198769050-00016
27. Slevin O, Amsler F, Hirschmann M. No correlation between coronal alignment of total knee arthroplasty and clinical outcomes: a prospective clinical study using 3D-CT. Knee Surg Sports Traumatol Arthrosc. 2017;25(12):3892–3900. doi:10.1007/s00167-016-4400-y
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
