Back to Journals » Patient Preference and Adherence » Volume 16
Patient Preferences in Shared Decision Making During Healthcare and Associated Factors Among Adult Admitted Patients at Public Hospitals of West Shoa Oromia, Ethiopia
Authors Gurmu Y
Received 29 May 2022
Accepted for publication 21 July 2022
Published 26 July 2022 Volume 2022:16 Pages 1781—1786
DOI https://doi.org/10.2147/PPA.S376600
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Yonas Gurmu
Department of Nursing, College of Medicine & Health Sciences, Ambo University, Ambo, Ethiopia
Correspondence: Yonas Gurmu, Department of Nursing, College of Medicine & Health Sciences, Ambo University, P. O. Box: 19, Ambo, Ethiopia, Email [email protected]
Background: Patient preferences mean the choices of individuals to make decisions about health and medical treatment by using their own experiences, beliefs, and values. The aim of this study was to assess patient preferences in shared decision making during healthcare and associated factors among adult admitted patients at public hospitals of West Shoa Oromia, Ethiopia.
Methods: A cross-sectional study was carried out among adult admitted patients at public hospitals of West Shoa Oromia, Ethiopia. An interviewer-administered with the Control Preference Scale questionnaire instrument tool was used to assess patient preferences in shared decision making. All statistical analysis was performed using SPSS for windows program version 21.
Results: A total of 403 respondents participated. Out of the total respondents, 168 (41.7%) were females. Overall, 64.8% (n=261) of the respondents prefer a collaborative role in shared decision making. Age (AOR 4.11, 95% CI 2.21– 7.64), marital status (AOR 0.37, 95% CI 0.20– 0.68), and education level (AOR 2.45, 95% CI 1.13– 4.87) are significant in patient preference in shared decision making.
Conclusion and Recommendation: More than half of respondents 261 (64.8%) prefer shared decision making in a collaborative role with healthcare providers. Age, marital status, and level of education are factors associated with the patient preferences in shared decision making. The Ethiopian ministry of health should work on policy of shared decision making. Healthcare providers have to consider patients in shared decision making.
Keywords: patient, patient preferences, admitted patients
Introduction
Patient preferences mean the choices of individuals to make decisions about health and medical treatment by using their own experiences, beliefs, and values.1 The choices and preferences are not left to the patients; there needs to be a shared decision making process between patients and healthcare providers.2,3 The shared decision making efficacy is limited by the impossibility to clearly define the course of action, and the informed ideal, in which the healthcare providers provide information to the patient who is in charge of making decisions.2,4 The know-how coming from patients and healthcare providers on each part cannot replace the other. So, as to specifics. In shared decision making, despite the fact that the healthcare providers have an expertise in diagnosis, prognosis, and treatment options, patients are experts in their medical history, values, preferences, and areas.5 The majority of patients recognized their healthcare providers that a decision needs to be made and the availability of different options. However, the level of shared in treatment decision making process was low.6
Patients wanted their family to be involved in shared decision making; however, patients’ expectation and healthcare providers’ perception of patients’ role preference have a gap. Therefore, healthcare providers should actively involve patients in shared decision making in their daily clinical practice.7
Nowaday’s patient-centered care approach has importance in patients’ contribution and in the medical decision making process. The increase of patient activity within their own care process comes from elements that can be considered as enablers of shared decision making.8–10
Incorporating and understanding individuals’ preferences for participating in healthcare decisions are the bases in delivering patient-centered care.11,12
Communication is an important asset for shared decision making.13 Patients are asked to engage in informed discussion of the risks, benefits, and alternative interventions and decide between them for the elicited preferences.14,15 The patients benefit from their contribution and the shared decision making process by identifying preferred option through a bidirectional communication process.16–18
In general, patient preferences in shared decision making have clinical significances. Patients who collaborate with their healthcare providers to reach a shared healthcare decision have greater trust in the healthcare providers–patient relationship, collaborate more fully to implement the shared decision, and express greater satisfaction with their health care. Research has shown that patients with chronic diseases, such as hypertension, diabetes mellitus, peptic ulcer disease, and rheumatoid arthritis, enjoy better health outcomes when they ask questions, express opinions, and make their preferences known.1 The aim of this study was to find patient preferences in shared decision making during healthcare and associated factors among adult admitted patients at public hospitals of West Shoa Oromia, Ethiopia.
Methods
Study Design and Participants
A cross sectional study was conducted at four hospitals that are found in West Shoa zone of Oromia regional state. Those hospitals are Ambo University referral hospital, Ambo general hospital, Gedo hospital and Inchini hospital. All adult (18 years or older) admitted patients at medical and surgical wards in selected hospitals were included except those who were seriously ill during data collection. The total sample calculated was 422. The total sample was allocated proportionally to the hospitals depending on the number of admitted patients at medical and surgical wards. Accordingly, 148 patients from Ambo University referral hospital, 127 from Ambo general hospital 84 from Gedo hospital, and 63 from Inchini hospital were selected by systematic sampling technique.
Instruments (Measures) and Data Collection
The questionnaire was translated from English to Afaan Oromo and Amharic languages by a multilingual translator before data collection, and then back translated to English by another multilingual translator after data were collected. The standardized questionnaire was pre-tested, and the internal consistency of the question was evaluated and the Cronbach's alpha value was 0.78. The patient preferences in shared decision making were measured using the Control Preference Scale questionnaire.7 A 5-point Likert scale on shared decision making was used. Scored were recorded as strongly agree with 5, agree with a 4, neutral with a 3, disagree with a 2, and strongly disagree with a 1. The mean score for the 6 items was then calculated for each participant, with a maximum of 5 and a minimum of 1. Collaborative role was considered for which individuals make decisions together with their healthcare providers (mean score ≥4) and passive was considered as preferring to leave decisions to healthcare providers (mean score <4).12 The data were collected by interviewer.
Training was given for the data collectors to warrant that all the data collectors have the same information about the study instrument and have the same interview procedures. The training includes about the purpose of the study, confidentiality, and how to approach and forward questions to patients. The data collectors were BSc healthcare providers. During data collection there has been strict supervision.
Statistical Analysis
The analysis was done using Statistical Package for the Social Sciences (SPSS) statistical software version 21.0. Bivariate and multivariate analyses using logistic regression were computed to assess association between the independent variable (socio-demographic characteristics) and patient preferences (the outcome variable). Independent variables with P<0.2 on bivariate logistic regression were used for multivariate analysis. The statistical level significant is set at alpha of 0.05. The data were described and presented using narrative text, figure, and tables.
Results
Socio‑demographic Characteristics of Respondents
A total of 403 respondents participated. The response rate was 95.5. Out of the total of respondents, 168 (41.7%) were females. About 111 (27.5%) of the respondents were belonging to the age group 20−39 years (Table 1).
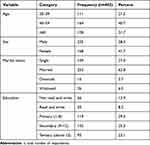 |
Table 1 Socio-Demographic Characteristics of Respondents in Selected Public Hospitals of West Shoa Zone, Oromia, Ethiopia, 2020 |
Patient Preferences of Respondents
More than half of the respondents prefer making a shared decision collaborative role 261 (64.8%) with their healthcare providers, whereas the rest of respondents were passive 142 (35.2%) and they prefer to leave decisions to healthcare providers.
Factors Associated with Patient Preferences
Those variables that had association with patient preferences with p-value less than 0.2 in the simple logistic regression analysis were taken to multiple logistic regression analysis.
The odds of a collaborative role patient is 4.11 times among patients with age >60 years as compared to age 20–39 years (AOR 4.11, 95% CI 2.21–7.64). Those respondents married were 63% less likely to have collaborative role patient preferences in shared decision making than those single (unmarried) (AOR 0.37, 95% CI 0.20–0.68). Those respondents who are above grade 12 were 2.35 times more likely to have collaborative role patient preferences in shared decision making (AOR 2.45, 95% CI 1.13–4.87) compared to those not read and write respondents (Table 2).
 |
Table 2 Factors Associated with Patient Preferences of Respondents in Selected Public Hospitals of West Shoa Zone, Oromia, Ethiopia, 2020 (n=403) |
Discussion
Patient preferences in shared decision making are important in looking for their expression, which the healthcare providers should consider in treating the patients such as fears, imaginations, or unusual beliefs.1 Involving patients in the shared decision making process allows them to their specific needs, values, and preferences,10,19 even though not all patients wish to collaboratively participate in health-related decisions to the same extent.20 About 91% of respondents agree that encouragement from healthcare providers would motivate their participation in shared decision-making.6 Communicationcan be a barrier to share decision-making; some patients from disadvantaged cultural backgrounds are not used to participating in shared decision making.21,22
This study aimed to assess patient preferences in shared decision making and associated factors among adult admitted patients at public hospitals of West Shoa Oromia, Ethiopia. Accordingly, this study identifies that 64.8% of patients prefer to involve collaborative preference in shared decision making. This indicated that the remaining 35.2% prefer passive preference in shared decision making. This study also identify that patient preferences were significantly associated with age, marital status, and education level.
The results of this study are similar to Ambigapathy et al; shared decision making (collaborative) was preferred by 51.9% of patients, followed by passive (26.3%) and active (21.8%) roles in decision making.7 In another study by Mah et al, 51.4% of respondents preferred a collaborative role with their healthcare providers, 44.8% preferred a passive role while only 1.9% preferred an active role. Most patients preferred a collaborative role (57.5%), followed by a semi passive (21.2%), a partly autonomous (16.2%), an autonomous (2.8%) and a fully passive (2.3%) role when making medical decisions.23
In this study, those married women were 63% less likely to have collaborative patient preferences in shared decision making. This may be because marital status need a joint decision either with husband or wife. This can be evidenced by the study done Chang et al,24 joint decision making by a married or cohabitating couple, one of the most prevalent social relationships globally. This may reflect growing equality and partnership between men and women when viewed against historical and traditional norms of men having decision making authority.24
Regarding which factors are associated with patient preferences in a shared decision making process, our findings are in line with other studies, which found age, education to be significantly associated with the desire to participate in health decisions.6,22,23 However, we found no significant differences between different sex, unlike other studies.23,25,26 Having a high response rate and usage of a standardized questionnaire are the strengths of this study. It also used baseline information for future studies of that area. The study has limitation concerning social desirability bias and cross-sectional study design.
Conclusion and Recommendation
More than half of respondents (64.8%) prefer making shared decisions collaboratively with their healthcare providers. Age, marital status, and level of education are factors associated with the patient preferences in shared decision making. The Ethiopian ministry of health should work on a policy of shared decision making. Healthcare providers have to consider patients in shared decision making. Future work that is expected from researchers is an interventional study and identifying the pathway by which cultural backgrounds and diagnosis may affect the degree of patient preference in shared decision making.
Data Sharing Statement
Data will be available from the corresponding author on reasonable request.
Ethical Considerations
The research was reviewed and approved by an Institutional Review Board of Ambo University. The authorities found in the study area were given permission to conduct research. The study was conducted according to the Declaration of Helsinki. Participants of this research were provided written informed consents. Patients’ privacy and confidentiality were maintained at all durations.
Acknowledgments
The author would like to thank Ambo University, College of Medicine and Health Science for providing me the opportunity to conduct this research. In addition, I would like to thank the West shoa zone health department and all hospitals providing me the necessary information. Finally, I would like to thank supervisors, data collectors and all study participants.
Funding
The research was funded by Ambo University.
Disclosure
The author declares no conflicts of interest for this work.
References
1. Albert RJ. Clinical Ethics: A Practical Approach to Ethical Decisions in Clinical Medicine. McGraw-Hill Education; 2021.
2. Gorini A, Pravettoni G. An overview on cognitive aspects implicated in medical decisions. Eur J Intern Med. 2011;22(6):547–553. doi:10.1016/j.ejim.2011.06.008
3. Renzi C, Riva S, Masiero M, Pravettoni G. The choice dilemma in chronic hematological conditions: why choosing is not only a medical issue? A psycho-cognitive perspective. Crit Rev Oncol Hematol. 2016;99:134–140. doi:10.1016/j.critrevonc.2015.12.010
4. Lucchiari C, Masiero M, Pravettoni G, Vago G, Wears RL. End-of life decision-making: a descriptive study on the decisional attitudes of Italian physicians. Life Span Disabil. 2010;13(1):71–86.
5. Moss AH. Ethical issues in chronic kidney disease. In: Chronic Renal Disease. Academic Press; 2015:882–889.
6. Mah HC, Muthupalaniappen L, Chong WW. Perceived involvement and preferences in shared decision-making among patients with hypertension. Fam Pract. 2016;33(3):296–301. doi:10.1093/fampra/cmw012
7. Ambigapathy R, Chia YC, Ng CJ. Patient involvement in decision-making: a cross-sectional study in a Malaysian primary care clinic. BMJ open. 2016;6(1):e010063. doi:10.1136/bmjopen-2015-010063
8. Bailo L, Guiddi P, Vergani L, Marton G, Pravettoni G. The patient perspective: investigating patient empowerment enablers and barriers within the oncological care process. Ecancermedicalscience. 2019;13:912. doi:10.3332/ecancer.2019.912
9. Vergani L, Marton G, Pizzoli SF, Monzani D, Mazzocco K, Pravettoni G. Training cognitive functions using mobile apps in breast cancer patients: systematic review. JMIR mHealth uHealth. 2019;7(3):e10855. doi:10.2196/10855
10. Barry MJ, Edgman-Levitan S. Shared decision making — the pinnacle of patient-centered care. N Engl J Med. 2012;366(9):780–781. doi:10.1056/NEJMp1109283
11. Chang DH, Wang YH, Hsieh CY, Chang CW, Chang KC, Chen YS. Incorporating patient preferences into a decision-making model of hand trauma reconstruction. Int J Environ Res Public Health. 2021;18(21):11081. doi:10.3390/ijerph182111081
12. Chi WC, Wolff J, Greer R, Dy S. Multimorbidity and decision-making preferences among older adults. Ann Family Med. 2017;15(6):546–551. doi:10.1370/afm.2106
13. Russo S, Jongerius C, Faccio F, et al. Understanding patients’ preferences: a systematic review of psychological instruments used in patients’ preference and decision studies. Value Health. 2019;22(4):491–501. doi:10.1016/j.jval.2018.12.007
14. Medical Device Innovation Consortium. Medical device innovation consortium (MDIC) patient centered benefit-risk project report: a framework for incorporating information on patient preferences regarding benefit and risk into regulatory assessments of new medical technology. Med Dev Innov Consortium. 2015;4:e34.
15. Ryan M, Scott DA, Reeves C, et al. Eliciting public preferences for healthcare: a systematic review of techniques. Health Technol Assess. 2001;5(5):1–86. doi:10.3310/hta5050
16. Charles CA, Gafni A, Whelan T. Decision-making in the physician-patient encounter: revisiting the shared treatment decision-making model. Soc Sci Med. 1999;49:651–661. doi:10.1016/S0277-9536(99)00145-8
17. Neuman HB, Charlson ME, Temple LK. Is there a role for decision aids in cancer-related decisions? Crit Rev Oncol Hematol. 2007;62(3):240–250. doi:10.1016/j.critrevonc.2006.12.006
18. Fischhoff B. Decision research strategies. Health Psychol. 2005;24(4S):S9. doi:10.1037/0278-6133.24.4.S9
19. Whitney SN, McGuire AL, McCullough LB. A typology of shared decision making, informed consent, and simple consent. Ann Intern Med. 2004;140(1):54–59. doi:10.7326/0003-4819-140-1-200401060-00012
20. Gregório M, Teixeira A, Henriques T, et al. What role do patients prefer in medical decision-making?: a population-based nationwide cross-sectional study. BMJ open. 2021;11(10):e048488. doi:10.1136/bmjopen-2020-048488
21. Espanha R, Ávila P. Health literacy survey Portugal: a contribution for the knowledge on health and communications. Procedia Comput Sci. 2016;100:1033–1041. doi:10.1016/j.procs.2016.09.277
22. Goggins KM, Wallston KA, Nwosu S, Schildcrout JS, Castel L, Kripalani S; for the Vanderbilt Inpatient Cohort Study (VICS). Health literacy, numeracy, and other characteristics associated with hospitalized patients’ preferences for involvement in decision making. J Health Commun. 2014;19(sup2):29–43. doi:10.1080/10810730.2014.938841
23. Michaelis S, Kriston L, Härter M, Watzke B, Schulz H, Melchior H. Predicting the preferences for involvement in medical decision making among patients with mental disorders. PLoS One. 2017;12(8):e0182203. doi:10.1371/journal.pone.0182203
24. Osamor PE, Grady C. Autonomy and couples’ joint decision-making in healthcare. BMC Med Ethics. 2018;19(1):1–8. doi:10.1186/s12910-017-0241-6
25. Levinson W, Kao A, Kuby A, Thisted RA. Not all patients want to participate in decision making: a national study of public preferences. J Gen Intern Med. 2005;20(6):531–535. doi:10.1111/j.1525-1497.2005.04101.x
26. Say R, Murtagh M, Thomson R. Patients’ preference for involvement in medical decision making: a narrative review. Patient Educ Couns. 2006;60(2):102–114. doi:10.1016/j.pec.2005.02.003
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
