Back to Journals » Patient Preference and Adherence » Volume 17
Patient Preferences for Adjuvant Treatment in Muscle-Invasive Urothelial Carcinoma: A Multi-Country Discrete Choice Experiment
Authors King-Concialdi K , Beusterien K, Senglaub SS , Will O , Jaffe DH , Patel MY, Harrison MR
Received 14 April 2023
Accepted for publication 9 August 2023
Published 8 September 2023 Volume 2023:17 Pages 2237—2248
DOI https://doi.org/10.2147/PPA.S411751
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jongwha Chang
Kristen King-Concialdi,1 Kathleen Beusterien,1 Steven S Senglaub,1 Oliver Will,1 Dena H Jaffe,1 Miraj Y Patel,2 Michael R Harrison3
1Real-World Evidence, Cerner Enviza, an Oracle Company, North Kansas City, MO, USA; 2Health Economics and Outcomes Research, Bristol Myers Squibb, Princeton, NJ, USA; 3Duke Cancer Institute Center for Prostate and Urologic Cancers, Department of Medicine, Division of Medical Oncology, Duke University Medical Center, Durham, NC, USA
Correspondence: Steven S Senglaub, Real-World Evidence, Cerner Enviza, an Oracle Company, 2800 Rock Creek Parkway, North Kansas City, MO, 64117, USA, Tel +1 816 201 1198, Email [email protected]
Purpose: The evolving treatment landscape in muscle-invasive urothelial carcinoma creates challenges for clinicians and patients in selecting the most appropriate therapy. Here, we aimed to understand adjuvant treatment preferences among patients with muscle-invasive urothelial carcinoma who underwent radical resection, including tradeoffs between efficacy outcomes and toxicity risks.
Patients and Methods: An observational, cross-sectional study utilizing a discrete choice experiment was conducted across the United States, United Kingdom, Canada, France, and Germany via a web-based survey. Patients ≥ 18 years of age who self-reported as having been diagnosed with muscle-invasive urothelial carcinoma were included. Patients indicated their preferences between hypothetical treatment profiles varying in eight attributes relating to efficacy, regimen, and side effects. Preference weights were estimated using hierarchical Bayesian logistic regression; relative attribute importance estimates were calculated.
Results: Overall, 207 patients were included (age ≥ 56 years, 65.7%; male, 54.1%). Patients chose adjuvant treatment 91.2% of the time vs no treatment. Prolonging overall survival from 25 to 78 months was most important, followed by reducing serious side effect risks. Increasing disease-free survival from 12 to 24 months was more important than decreasing risks of fatigue from 54% to 15% and nausea from 53% to 7%. Treatment with the shortest dosing regimen was more important for patients who received neoadjuvant chemotherapy vs patients who did not receive neoadjuvant chemotherapy; prolonging overall survival was more important than reducing the risk of a serious side effect in non-US patients; the opposite was found in the United States.
Conclusion: Patients with muscle-invasive urothelial carcinoma who underwent radical resection preferred adjuvant treatment over no treatment regardless of side effects. Patients prioritized overall survival improvements followed by a reduced side effect profile.
Keywords: bladder cancer, discrete choice experiment, muscle-invasive urothelial carcinoma, patient treatment preferences
Introduction
Urothelial carcinoma (UC) accounts for approximately 90% of bladder cancers, with about 30% diagnosed as muscle-invasive localized tumors.1,2 Bladder cancer is the 10th most commonly diagnosed cancer worldwide, and its occurrence is about threefold higher in Europe and North America than in other regions.3,4
The American Urological Association and the European Association of Urology (EAU) recommend cisplatin-based neoadjuvant chemotherapy (NAC) followed by radical cystectomy as the mainstay treatment of muscle-invasive bladder cancer (MIBC).5,6 However, not all patients with MIBC are cisplatin-eligible, and there are associated toxicities.5,7 Although the EAU guidelines recommend adjuvant cisplatin-based chemotherapy in high-risk MIBC patients not given NAC, these trials were underpowered to adequately assess efficacy.6 The use of immunotherapy is evolving in the treatment of UC.8–11
Nivolumab, a programmed death-1 inhibitor, demonstrated significant improvement in disease-free survival as an adjuvant treatment for muscle-invasive urothelial carcinoma (MIUC) with/without cisplatin-based NAC in the CheckMate 274 trial.12,13 Nivolumab was approved by the US Food and Drug Administration and the European Medicines Agency as adjuvant treatment in patients with UC who are at high risk of recurrence after surgery.14,15 The EAU guidelines recommend discussing adjuvant immunotherapy with nivolumab after radical cystectomy in selected patients who are ineligible for or declined adjuvant cisplatin-based chemotherapy.6
The evolving treatment landscape and necessity for multi-disciplinary consultation in MIUC may create challenges for clinicians and patients in deciding the most appropriate course of therapy. In the decision-making process, patients need to weigh the benefits and risks of available treatment options that differ in treatment characteristics such as efficacy, potential side effects, dosing regimen, and mode of administration. An understanding of patients’ preferences and willingness to accept tradeoffs between various treatment attributes and outcomes is critical when selecting treatment options. Although the discrete choice experiment (DCE) explores patients’ preferences for cancer therapy in the management of different types of cancers,16–19 there exists a paucity of such research in MIUC for adjuvant treatments.
This multi-country study aimed to describe adjuvant treatment preferences among patients with MIUC who underwent radical resection, including patient willingness to make tradeoffs between efficacy outcomes and toxicity risks. Additionally, the study aimed to assess the treatment history and demographic factors that could potentially explain differences in treatment preference.
Patients and Methods
Study Design
An observational, cross-sectional, web-based survey was conducted in the United States, United Kingdom, Canada, France, and Germany with data collection from May to September 2021. A DCE design assessed preferences for attributes associated with MIUC treatments, including immunotherapies and chemotherapies. This study was conducted according to International Society for Pharmacoeconomics and Outcomes Research (ISPOR) guidelines.20 Patients were recruited through survey panel databases, cancer advocacy groups, physician referrals, and social media outreach. The study received ethics approval or exemption status, depending on the country (US, exemption via Pearl IRB; UK, exemption via the Health Research Authority; Canada, approval via Veritas IRB; 2016 Veritas Inc.; and France and Germany, approval via Cerner Enviza independent review board, and was in compliance with the principles of the Declaration of Helsinki. All patients provided electronic informed consent, and patients who completed the full survey received fair market value compensation for their time.
Eligibility Criteria
The study included adults (≥18 years) who were self-reported residents of the surveyed country, self-reported a medical diagnosis of MIUC (defined as bladder, ureter, or renal pelvis cancer), and underwent radical cystectomy or nephroureterectomy within 12 months before study participation. Patients with UC recurrence or distant metastasis after surgery were excluded.
Measures
Demographic and Health Characteristics
Demographics including age, sex, and race/ethnicity (US and Canada only), and health characteristics such as overall health rating, comorbidities, and the Charlson Comorbidity Index (CCI) were reported. Data on patients’ medical history, pre- and post-surgery discussions regarding adjuvant therapy, and use of neoadjuvant/adjuvant treatments were also collected.
Discrete Choice Experiment
DCE was employed to assess adjuvant treatment preferences for MIUC. In a series of 13 DCE choice tasks, patients were asked to choose the preferred option from two hypothetical treatment profiles or a “no treatment” option (Supplementary Table 1). The DCE included attributes and levels associated with programmed death-1 inhibitors and chemotherapy options for MIUC. Attributes were identified through literature reviews, input by patient advocates and medical experts, and in-depth interviews with 12 patients and 4 physicians.
The draft survey questionnaire was pretested through cognitive interviews with 13 patients across all five study countries. Each treatment profile included eight treatment attributes with two to four levels each (Table 1): disease-free survival; overall survival (OS); risk of nausea; risk of diarrhea; risk of hypothyroidism; risk of fatigue; risk of a serious side effect that requires hospitalization; and dosing regimen. The minimum and maximum levels for the attributes were based on data from clinical trials. The risk levels for the side effect attributes were based on the risks reported for all grades; the risk level for the serious side effect attribute was based on risks reported for grade 3 or higher. Before the DCE, patients completed an introductory section that familiarized them with the attributes. Patients were asked to rate the various attribute levels on a 5-point Likert scale (1=very bad to 5=very good).
 |
Table 1 Attributes and Levels for DCE Choice Tasks |
A formula for determining minimum sample sizes for aggregate-level full-profile DCE modeling is nta/c >500, where n=number of respondents, t=number of choice tasks (each with two profiles/alternatives), a=number of alternatives (profiles) per task, and c=largest number of levels for any one attribute. With a sample size of 290, eight attributes, a maximum of four levels, and 13 choice tasks, the formula result is 2827; a score >500 indicates a sufficient sample size to obtain relatively precise utility estimates.
Statistical Analyses
Descriptive statistics (means and standard deviations for continuous variables, and frequency and percentage for categorical variables) were reported for all study variables. A hierarchical Bayesian logistic regression model was used to estimate preference weights for each attribute level.21 Such preference weights can be used to assess the magnitude of the tradeoffs that patients are willing to make among the attribute levels.
Relative importance estimates were calculated for each attribute to demonstrate how much difference each attribute could make in the total utility of a product; these reflect the importance of each attribute relative to others in the study. Relative importance estimates were calculated at the patient level by dividing the range of each attribute (utility of most favorable minus least favorable levels) by the sum of ranges of all attributes and multiplying by 100.
Subgroup analyses compared preference weights and attribute relative importance (using chi-square tests or ANOVAs) by country (US vs non-US patients), treatment regimen (patients who received NAC [NAC group] vs patients who did not receive NAC [non-NAC group]), and age group (18–55, 56–65, and ≥66 years).
Analyses were conducted using IBM SPSS version 25.0/Sawtooth Software Lighthouse Studio version 9.11.0/SAS version 9.4/R version 4.0.3 or greater versions.
Results
Patients
Of the 544 patients who entered the survey, 42 did not complete the survey and 293 did not meet eligibility criteria. Two patients were removed as the current type of UC could not be determined. In total, 207 patients were included in the final analysis: United States (n=97), Germany (n=60), United Kingdom (n=31), France (n=1), and Canada (n=18). Most patients were ≥56 years old (65.7%) and male (54.1%). Among patients in the United States and Canada, nearly half were White (48.7%). The most common comorbidities were hypertension (29.5%) and hypercholesterolemia (15.9%). The CCI (mean ± standard deviation) was 0.48±0.90, with 71.5% of patients having a CCI of 0 (Table 2).
 |
Table 2 Patients’ Demographic and Health Characteristics (Overall MIUC Population) |
Overall, 66.7% of patients reported no spread or recurrence of UC after surgery. Of the 40.6% of patients who received neoadjuvant treatment, most had received chemotherapy (91.7% [cisplatin, carboplatin]; Supplementary Table 2) compared with other neoadjuvant treatments. As this survey was conducted during the COVID-19 pandemic, 46.4% of patients reported some form of impact to the management and treatment of their UC owing to COVID-19, for example, 12.1% of patients reported that their surgery was delayed.
Attribute-Level Preference Weights
Overall, patients chose adjuvant treatment 91.2% of the time vs no treatment (8.8%) across the DCE choice tasks. With respect to treatment profiles, preference weights increased as attribute levels improved (ie, efficacy improvements and reduction in risk of side effects; Figure 1). Based on the preference weights, example trade-offs that patients were willing to make included that a decrease in cancer-free survival from 18 to 12 months was acceptable for patients in exchange for an increase in OS from 25 to 54 months; patients valued an increase in 12 months of cancer-free survival similarly to an increase in 10.5 months of OS. Patients would require an increase in OS of 33 months to offset an increase in the risk of a serious side effect from 15% to 69%. Additionally, patients would require an increase in OS of 7.2 months to offset an increase in nausea from 7% to 53%.
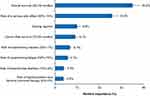
Relative Attribute Importance
Prolonging survival from 25 to 78 months was the most important attribute (relative importance mean ± standard error, 35.0%±1.5%), followed by reducing the risk of a serious side effect from 69% to 15% (25.8%±1.2%). Increasing cancer-free survival from 12 to 24 months was more important than decreasing risk of fatigue from 54% to 15% and nausea from 53% to 7%. Decreases in risks of nausea, fatigue, diarrhea, and hypothyroidism requiring lifelong hormone treatment were the least important attributes (Figure 2).
Subgroup Analyses
Improvements in attributes had a similar rank order in importance among NAC vs non-NAC groups (Figure 3A). Among patients who received vs those who did not receive NAC, prolonging survival from 25 to 78 months was the most important (31.22% vs 37.33%, p=0.054). However, patients who received NAC vs non-NAC placed higher importance on the shortest dosing regimen (two infusions every 3–4 weeks for 4 months; 11.99% vs 8.7%, p=0.026) and reduced risk of nausea (7.7% vs 6.22%, p=0.006).
Prolonging survival from 25 to 78 months was more important for non-US vs US patients (42.6% vs 26.4%, p<0.001) (Figure 3B). Reduction in risk of a serious side effect from 69% to 15% was more important for US vs non-US patients (31.7% vs 20.6%, p<0.001).
No significant differences in preference weights or relative importance among attribute levels were observed among age groups (all p>0.05; data not shown).
Discussion
This study demonstrated that patients with MIUC who underwent radical resection preferred adjuvant treatments over no treatment, regardless of risks of side effects or inconvenience of dosing regimen. Preferences for adjuvant treatment varied based on differences in OS, side effects, and dosing regimen. Overall, patients were willing to accept the risk of side effects in exchange for improved efficacy. All eight attributes evaluated in this study were found to influence treatment choice with the most important attribute for patients being prolonging OS from 25 to 78 months. Such findings can help support healthcare providers in decision-making processes by understanding patients’ preferences in the real world.22
In this study, patients chose an adjuvant treatment 91.2% of the time vs no treatment, suggesting that patients strongly favor intervention even after undergoing surgery. This is similar to a real-world study where most patients with resected melanoma opted for adjuvant therapy.23 We observed that patients with MIUC were willing to accept increased risks of all grades of fatigue, nausea, or diarrhea with adjuvant treatments in exchange for an increase in cancer-free survival from 12 to 24 months. Likewise, in other types of cancers, prolonging OS followed by quality-of-life attributes were most important for patients.18,24,25 Some previous DCE studies on cancer treatment, however, reported greater preference for lowering risks of side effects vs increasing overall/progression-free survival,17,19 which may be attributable to population differences in perceived risks of dying.
Both patients who received NAC and patients who did not receive NAC chose adjuvant treatment over no treatment; further, both subgroups valued prolonging survival the most, followed by reduction in risk of a serious side effect. Although NAC is well tolerated, approximately 50% of patients with MIBC have reported side effects after NAC.26 Thus, the finding that decreased risk of nausea was more important in patients who received NAC vs those who did not receive NAC may reflect previous side effect experiences of patients who received NAC.
Despite current guideline recommendations for NAC,5,6 our study reports NAC utilization at only 35%, which is only slightly higher than other recent studies but still low considering it is the standard of care.27,28 Interestingly, despite the low utilization of NAC, these data suggest that receipt of NAC does not change patients’ preference for adjuvant therapy, but instead suggests that the preferences of adjuvant treatment attributes may vary based on prior treatment history.
Prolonging survival from 25 to 78 months was most important for non-US patients, whereas a reduction in the risk of a serious side effect from 69% to 15% was most important for US patients. Further, a dosing regimen with the shortest overall duration was more important for US vs non-US patients. Differences in preferences observed in US vs non-US populations may not necessarily be explained by NAC experience, as the proportions of patients who received NAC were comparable (35% of US and 39% of non-US patients). However, these discrepancies could be attributable to differences in health care systems across countries (eg, hospitalization/insurance policies).29
An association of age with patient preferences for adjuvant therapy was not observed. Clinicians may make treatment decisions based on age by considering either tolerance to aggressive treatment or quality of life as important attributes for older patients.30,31
This study has several limitations. First, the findings may not be generalizable to all patients with MIUC; by virtue of its hypothetical design, the results may not completely reflect the real clinical, financial, and emotional consequences of actual decisions. Moreover, while recruitment methods varied, panel-based recruitment may over- and under-represent certain populations, especially considering patients without access to or who have discomfort with online survey administration. For example, this sample had a larger proportion of women and a younger average age than is typically reported in MIUC. Lastly, as the study was conducted during the COVID-19 pandemic, preference selections may have been influenced by a certain level of discomfort related to interaction with the health care system.
Conclusions
Patients with MIUC preferred adjuvant treatment to no treatment after radical resection, regardless of side effects or inconvenience of treatment. Patients prioritized improvements in OS followed by reduced risk of side effects; however, attribute preferences may be influenced by previous treatment regimens and region of inhabitance. Patients were willing to make tradeoffs between OS and the risks of side effects for the treatments. Overall, this study emphasizes the importance of discussing with patients the potential risks and benefits of adjuvant treatments in MIUC. Further explanation on tumor staging, serious and mild toxicities, and the absolute and relative benefits of adjuvant treatment may facilitate shared decision-making and improve quality of care in MIUC treatment.
Acknowledgments
This study was supported by Bristol Myers Squibb (Princeton, NJ, USA). Analytical and medical writing assistance were provided by Sonali Dalwadi, PhD; Ashwini Atre, PhD; and Sudha Korwar, PhD, of Indegene Pvt. Ltd., funded by Cerner Enviza. Professional editorial assistance was provided by Erika Young, PharmD, of Parexel, funded by Bristol Myers Squibb.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was funded by Bristol Myers Squibb. Cerner Enviza, an Oracle company, has conducted the research. Both entities prepared the article and contributed to the study design, collection, analysis, and interpretation of data.
Disclosure
Kristen King-Concialdi, Kathleen Beusterien, Oliver Will, Dena H. Jaffe, and Steven S. Senglaub are employees of Cerner Enviza, an Oracle company, who was contracted to conduct this research on behalf of Bristol-Myers Squibb (BMS). Miraj Y. Patel is an employee of BMS. Michael R. Harrison has received research funding to his institution from BMS, Genentech, Pfizer, Merck, Astellas Pharma, Bayer, Exelixis, Seattle Genetics, and Propella Therapeutics, as well as consulting fees from AVEO, Exelixis, Fujifilm, Pfizer, BMS, Sanofi, Seattle Genetics, Gilead Sciences, and Myovant Sciences, and is part of the speaker’s bureau for Exelixis.
References
1. Kaseb H, Aeddula N. Bladder Cancer. Treasure Island (FL): StatPearls Publishing; 2022. Available from: https://www.ncbi.nlm.nih.gov/books/NBK536923/.
2. Saginala K, Barsouk A, Aluru JS, Rawla P, Padala SA, Barsouk A. Epidemiology of bladder cancer. Med Sci. 2020;8(1):15. doi:10.3390/medsci8010015
3. Richters A, Aben KKH, Kiemeney LALM. The global burden of urinary bladder cancer: an update. World J Urol. 2020;38(8):1895–1904. doi:10.1007/s00345-019-02984-4
4. Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–249. doi:10.3322/caac.21660
5. Chang SS, Bochner BH, Chou R, et al. Treatment of non-metastatic muscle-invasive bladder cancer: AUA/ASCO/ASTRO/SUO guideline. J Urol. 2017;198(3):552–559. doi:10.1016/j.juro.2017.04.086
6. Witjes JA, Bruins HM, Carrión A, et al. EAU guidelines on muscle-invasive and metastatic bladder cancer; 2022. Available from: https://d56bochluxqnz.cloudfront.net/documents/full-guideline/EAU-Guidelines-on-Muscle-Invasive-And-Metastatic-Bladder-Cancer-2022.pdf.
7. Galsky MD, Hahn NM, Rosenberg J, et al. A consensus definition of patients with metastatic urothelial carcinoma who are unfit for cisplatin-based chemotherapy. Lancet Oncol. 2011;12(3):211–214. doi:10.1016/S1470-2045(10)70275-8
8. Lopez-Beltran A, López-Rios F, Montironi R, Wildsmith S, Eckstein M. Immune checkpoint inhibitors in urothelial carcinoma: recommendations for practical approaches to PD-L1 and other potential predictive biomarker testing. Cancers (Basel). 2021;13(6):1424. doi:10.3390/cancers13061424
9. Rhea LP, Aragon-Ching JB. Advances and controversies with checkpoint inhibitors in bladder cancer. Clin Med Insights Oncol. 2021;15:11795549211044963. doi:10.1177/11795549211044963
10. Lee HH, Ham WS. Perioperative immunotherapy in muscle-invasive bladder cancer. Transl Cancer Res. 2020;9(10):6546–6553. doi:10.21037/tcr.2020.01.36
11. Hussain SA, Birtle A, Crabb S, et al. From clinical trials to real-life clinical practice: the role of immunotherapy with PD-1/PD-L1 inhibitors in advanced urothelial carcinoma. Eur Urol Oncol. 2018;1(6):486–500. doi:10.1016/j.euo.2018.05.011
12. Bajorin DF, Witjes JA, Gschwend JE, et al. Adjuvant nivolumab versus placebo in muscle-invasive urothelial carcinoma. N Engl J Med. 2021;384(22):2102–2114. doi:10.1056/nejmoa2034442
13. Galsky M, Witjes JA, Gschwend JE, et al. Disease-free survival with longer follow-up from the CheckMate 274 trial of adjuvant nivolumab in patients after surgery for high-risk muscle-invasive urothelial carcinoma. J Urol. 2022;207(Supplement 5):e183. doi:10.1097/JU.0000000000002536.01
14. Opdivo. FDA approves nivolumab for adjuvant treatment of urothelial carcinoma. U.S. Food and Drug Administration; 2021. Available from: https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-nivolumab-adjuvant-treatment-urothelial-carcinoma.
15. Opdivo, European Medicines Agency (Product number EMEA/H/C/003985); 2022. Available from: https://www.ema.europa.eu/en/medicines/human/EPAR/opdivo.
16. Fernández O, Lázaro-Quintela M, Crespo G, et al. Preferences for renal cell carcinoma pharmacological treatment: a discrete choice experiment in patients and oncologists. Front Oncol. 2022;11:773366. doi:10.3389/fonc.2021.773366
17. Stone RL, Cambron-Mellott MJ, Beusterien K, et al. Patients’ and oncologists’ preferences for second-line maintenance PARP inhibitor therapy in epithelial ovarian cancer. Future Oncol. 2022;18(4):491–503. doi:10.2217/fon-2021-0567
18. Weilandt J, Diehl K, Schaarschmidt ML, et al. Patient preferences in adjuvant and palliative treatment of advanced melanoma: a discrete choice experiment. Acta Derm Venereol. 2020;100(6):adv00083. doi:10.2340/00015555-3422
19. Srinivas S, Mohamed AF, Appukkuttan S, et al. Patient and caregiver benefit-risk preferences for nonmetastatic castration-resistant prostate cancer treatment. Cancer Med. 2020;9(18):6586–6596. doi:10.1002/cam4.3321
20. Johnson FR, Lancsar E, Marshall D, et al. Constructing experimental designs for discrete-choice experiments: report of the ISPOR Conjoint Analysis Experimental Design Good Research Practices Task Force. Value Health. 2013;16(1):3–13. doi:10.1016/j.jval.2012.08.2223
21. Hauber AB, González JM, Groothuis-Oudshoorn CGM, et al. Statistical methods for the analysis of discrete choice experiments: a report of the ISPOR Conjoint Analysis Good Research Practices Task Force. Value Health. 2016;19(4):300–315. doi:10.1016/j.jval.2016.04.004
22. Wang Y, Wang Z, Wang Z, Li X, Pang X, Wang S. Application of discrete choice experiment in health care: a bibliometric analysis. Front Public Health. 2021;9:673698. doi:10.3389/fpubh.2021.673698
23. Lodde G, Forschner A, Hassel J, et al. Factors influencing the adjuvant therapy decision: results of a real-world multicenter data analysis of 904 melanoma patients. Cancers (Basel). 2021;13(10):2319. doi:10.3390/cancers13102319
24. Havrilesky LJ, Lim S, Ehrisman JA, et al. Patient preferences for maintenance PARP inhibitor therapy in ovarian cancer treatment. Gynecol Oncol. 2020;156(3):561–567. doi:10.1016/j.ygyno.2020.01.026
25. Amin S, Tolaney SM, Janelle Cambron-Mellott M, et al. Benefit-risk trade-offs in treatment choice in advanced HER2 negative breast cancer: patient and oncologist perspectives. Future Oncol. 2022;18(16):1927–1941. doi:10.2217/fon-2021-0761
26. Salminen AP, Perez IM, Klén R, et al. Adverse events during neoadjuvant chemotherapy for muscle invasive bladder cancer. Bladder Cancer. 2019;5(4):273–279. doi:10.3233/BLC-190246
27. Liu W, Tian J, Zhang S, et al. The utilization status of neoadjuvant chemotherapy in muscle-invasive bladder cancer: a systematic review and meta-analysis. Minerva Urol Nephrol. 2021;73(2):144–153. doi:10.23736/s2724-6051.19.03648-8
28. Orf J, Barressi D, Davaro F, et al. Age related trends in the utilization of neoadjuvant chemotherapy for muscle invasive bladder cancer. J Urol. 2023;209(4):e1126. doi:10.1097/JU.0000000000003354.05
29. Ridic G, Gleason S, Ridic O. Comparisons of health care systems in the United States, Germany and Canada. Mater Sociomed. 2012;24(2):112. doi:10.5455/msm.2012.24.112-120
30. Shrestha A, Martin C, Burton M, Walters S, Collins K, Wyld L. Quality of life versus length of life considerations in cancer patients: a systematic literature review. Psychooncology. 2019;28(7):1367–1380. doi:10.1002/pon.5054
31. Seghers PALN, Wiersma A, Festen S, et al. Patient preferences for treatment outcomes in oncology with a focus on the older patient - a systematic review. Cancers (Basel). 2022;14(5):1147. doi:10.3390/cancers14051147
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.