Back to Journals » Clinical Ophthalmology » Volume 16
Patient Preference, Visual Quality, and Multivariate Regression Analysis with Contralateral Bifocal and Trifocal Intraocular Lenses
Authors Bucci Jnr FA
Received 16 September 2022
Accepted for publication 22 November 2022
Published 13 December 2022 Volume 2022:16 Pages 4097—4107
DOI https://doi.org/10.2147/OPTH.S388462
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Frank A Bucci Jnr
Bucci Laser Vision Institute, Wilkes-Barre, PA, USA
Correspondence: Frank A Bucci Jnr, Bucci Laser Vision Institute, 158 Wilkes-Barre Township Blvd, Wilkes-Barre, PA, 18702, USA, Tel +1 570 825-5949, Fax +1 570 825-2645, Email [email protected]
Purpose: To compare patient preference and visual quality of a bifocal IOL versus a trifocal IOL when one of each lens is implanted in the same patient.
Patients and methods: Patients received a +3.25 Tecnis bifocal IOL in one eye and a PanOptix trifocal IOL in the opposite eye. Eyes were unilaterally evaluated and included UDVA, UIVA, UNVA, mesopic contrast sensitivity testing, and subjective questionnaires about overall satisfaction, and IOL preference. Regression was used to detect which objective or subjective metrics significantly predicted overall satisfaction for each eye.
Results: Sixty eyes of thirty patients were evaluated. Patients preferred (p=0.028) +3.25 to PanOptix. Overall satisfaction was significantly greater (p=0.05) for +3.25 (4.70 vs 4.43/5.00). UDVA (p=0.032) and “freq. of glasses use distance” (p=0.05) were significantly better for +3.25 eyes. Objective intermediate (Jaeger) vision was significantly better (p=0.034) for PanOptix eyes. “Freq. of glasses use intermediate” favored +3.25. Regression revealed variables related to intermediate vision and “ability to read fine print without glasses” were significant predictors of overall satisfaction for both IOLs. Variables related to contrast sensitivity both with and without glare were significant predictors exclusively for PanOptix eyes.
Conclusion: Patient preference favored +3.25 eyes (p=0.022). Individual rankings for each eye of “overall satisfaction” were significantly greater (p=0.05) for +3.25 eyes. UNVA and distance vision trended in favor of +3.25. Regression strongly suggests issues related to contrast sensitivity with PanOptix may be responsible for the significant patient preference of +3.25.
Keywords: cataract surgery, patient satisfaction, IOL preference, multifocal IOLs
Introduction
The percentage of cataract patients seeking spectacle independence with presbyopia-correcting IOLs is increasing.1 Multifocal IOLs have provided functional distance and near vision in patients undergoing cataract surgery and refractive clear lens exchange.2,3 The main limitations with bifocal presbyopia-correcting implants have included dysphotopsias such as halos and glare4,5 and poor intermediate vision.3,6
Trifocal IOLs were developed to add a third foci and improve intermediate function.7 There have been numerous studies comparing visual outcomes and patient satisfaction with bifocal and trifocal IOLs.8–16 These studies, however, have compared the performance of IOLs with bilateral implantation exclusively. There is a lack of, and need for, literature comparing IOLs when one of each has been implanted in the same patient.13 This contralateral study directly compares overall visual satisfaction and patient preference of a bifocal IOL (+3.25 D Tecnis Multifocal 1-Piece model ZLB00) to a trifocal IOL (AcrySof IQ PanOptix model TFNT00) using objective clinical metrics, subjective responses from a patient questionnaire, and multivariate regression analysis.
Assessing patient satisfaction can be challenging, because the subjective perception of each patient to an identical objective stimulus, like an IOL, can be highly variable. Kohnen17 has correctly emphasized that although objective scientific measures will always dominate or evaluation of visual outcomes, we cannot underestimate the patients’ subjective perception of their quality of vision when assessing our surgical results.
The aim of this study was to directly compare patient preference and visual quality of the bifocal +3.25 Tecnis IOL to the trifocal PanOptix IOL when one of each is implanted in the same patient. In addition, multivariate regression analysis was used to determine which objective and subjective variables contributed significantly to patient responses for “overall satisfaction.” Others have stressed the importance of correlating objective and subjective variables that directly influence the overall satisfaction of the patient.18 Our purpose was not only to quantitate levels of satisfaction and preference, but also to determine “why” they preferred one IOL over another.
Methods
Study Design
In this single-center, comparative study, subjective and objective data from the last preoperative visit and the final postoperative evaluation, from 60 eyes of 30 patients who had undergone bilateral phacoemulsification, were reviewed. Patients received a +3.25 D Tecnis Multifocal 1-Piece model ZLB00 (Johnson and Johnson Vision) in one eye, and an AcrySof IQ PanOptix model TFNT00 (Alcon) in the other eye. Eye dominance and “first eye surgery” were equally randomized.
Inclusion criteria included bilateral cataract extraction with phacoemulsification, a clear intraocular media other than cataract, and a desire to pursue spectacle independence. Subjects also had 1) at least four months of neuroadaptation, 2) all necessary nd:YAG laser capsulotomies completed, 3) residual refractive error corrected to ≤ 0.5 D of spherical and cylindrical error, and 4) a well-managed ocular surface.25 Exclusion criteria included ocular comorbidities that might threaten optimal postoperative visual outcomes such as epiretinal membranes, corneal endothelial dystrophies, moderate macular thickening, irregular astigmatism, or mild to moderate amblyopia.
The study was conducted in accordance with the tenets of the Declaration of Helsinki and in compliance with Good Clinical Practice. IRB Approval (Salus IRB, Austin, TX) was granted prior to enrolling subjects, and the informed consent was signed in advance of any study measurements; HIPAA regulations were followed.
Patients
All subjects had a comprehensive, preoperative examination, which included manifest refraction, pupillometry, corneal topography, aberrometry, optical coherence tomography, and pachymetry. All surgeries were performed by the same experienced surgeon (FAB). The independent preoperative variables collected at the initial evaluation that were regressed against “overall satisfaction” are shown in Table 1.
 |
Table 1 Preoperative Clinical Metrics |
Subjective questionnaire responses and postoperative objective metrics were collected at a final comprehensive postoperative visit. The independent postoperative clinical metrics regressed against “overall satisfaction” are presented in Table 2.
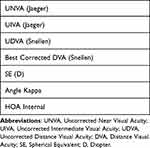 |
Table 2 Postoperative Clinical Metrics |
Objective testing at the final postoperative visit included uncorrected and best corrected visual acuities, with manifest refractions using a standard ETDRS chart. Intermediate and near visual acuities were tested at fixed focal lengths with the Colenbrander Mixed Contrast Card (Precision Vision, Woodstock, IL). Reading Acuity and reading speed (words per minute) were evaluated with the MNREAD Acuity Chart (Precision Vision). The M&S computerized Clinical Trial Suite (M&S Technologies, Niles, IL) was used to assess linear sine wave, contrast acuity, and bullseye contrast sensitivity under mesopic conditions with and without glare. A previously published25 patient questionnaire, which recorded the patient’s responses to 17 variables was administered for each eye and is presented in Supplemental Table 1.
Multiple regression analysis was performed to detect which independent variables from the preoperative examination, postoperative examination, and postoperative patient questionnaire were significant predictors for patient self-ranking scores of “overall satisfaction” for each eye (IOL) independently.
Intraocular Lenses
3.25 D Tecnis Multifocal 1-Piece Model ZLB00
The Tecnis +3.25 is a diffractive 1-piece hydrophobic acrylic IOL with a full diffractive posterior surface, an anterior aspheric surface, and a +3.25 D add at the IOL plane. The overall IOL length is 13.0 mm with an optic diameter of 6.0 mm. The design of the IOL includes a central 1.00 mm optical zone containing one half the add power (+1.63) of the full add which is capable of assisting the patient with intermediate vision. The anterior surface is designed with a negative spherical aberration −0.27 diopters.
AcrySof IQ PanOptix Model TFNT00
The AcrySof IQ PanOptix is an ultraviolet absorbing and blue light filtering foldable multifocal IOL. The IOL is a single-piece design with a central optic and two open-loop haptics. The optic consists of a proprietary high refractive index hydrophobic acrylic material with a blue light filtering chromophore. The anterior surface is designed with a negative spherical aberration to compensate for the positive spherical aberration of the cornea.
Data Analysis
SPSS (Version 28.0; IBM, NY) was used to perform statistical analysis. In all cases, p<0.05 indicated a statistically significant difference. Multiple regressions were carried out to investigate which independent variables could significantly predict patients’ overall satisfaction for ZLB00 and PanOptix. Stepwise/forward linear regression was conducted and adjusted R2 and the AIC (Akaike Information Criterion) was used to assess the model fit.
Results
A total of 60 eyes of 30 patients were evaluated in this study. The demographics are presented in Table 3. When patients were asked to choose which eye (IOL) they preferred, all things considered, they significantly preferred (p=0.021, Chi Square Test) the +3.25 IOL over the PanOptix IOL. Eighteen patients chose the +3.25 IOL, 7 chose the PanOptix IOL, and 5 patients choose no preference. The results of the patient subjective questionnaire are presented in Table 4. The results for “overall satisfaction” just reached significance (p=0.05) in favor of the +3.25 over the PanOptix. On a scale of 5 to 1 (best to worst), the mean score for the +3.25 was 4.70 ± 0.65 versus a mean score of 4.42 ± 0.94 for the PanOptix IOL. Both objective and subjective evaluations of uncorrected distance vision statistically favored the +3.25 IOL. Objectively, the Snellen uncorrected distance vision was 20/24 (logMAR 0.07) for PanOptix and significantly better for the +3.25 at 20/21.82 (logMAR 0.03) (p=0.032). Results of postoperative objective variables are presented in Table 5. The best corrected distance acuity trended in favor (p=0.059) of the +3.25 IOL at 20/18.33 (logMAR −0.04) versus 20/19.17 (logMAR −0.02) for the PanOptix IOL.
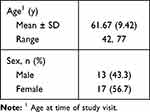 |
Table 3 Demographics |
 |
Table 4 Results of Patient Questionnaire |
 |
Table 5 Results of Postoperative Clinical Metrics |
Subjective questionnaire responses related to distance vision were consistent with findings for the objective Snellen acuities. Table 6 demonstrates significantly better results with the +3.25 IOL for “frequency of glasses use at distance” (p=0.05). For the variable “ability to perform activities when looking far away without glasses” there was a slight trend (p=0.10) in favor of the +3.25 IOL (Table 7).
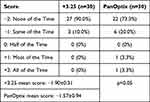 |
Table 6 Frequency of Glasses Use Distance |
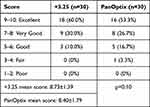 |
Table 7 Ability to Perform Distance Vision Activities Without Glasses |
There were no significant differences between the groups for objective uncorrected near (Jaeger) visions. The subjective near variable of “ability to read very small print without glasses” and the “ability to read moderately sized print” also revealed no significant differences. The subjective near vision variable of “frequency of glasses use – moderately sized print” revealed a trend (p=0.083) in favor of the +3.25 (Table 8).
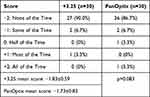 |
Table 8 Frequency of Glasses Use Moderately Sized Print |
There was somewhat of a dichotomy between the objective and subjective results for variables related to intermediate vision. The objective UIVA Jaeger clearly favored (p=0.034) the PanOptix IOL (J 1.17 PanOptix versus J 1.63 +3.25) (Figure 1). However, the subjective intermediate vision variable of “ability to perform arm’s length activities without glasses” showed no significant difference between groups (Table 9), and “frequency of glasses use for arm’s length activities” showed a slight trend (p=0.10) in favor of the +3.25 IOL (Table 10).
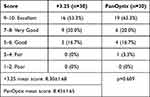 |
Table 9 Ability to Perform Arm’s-Length Activities Without Glasses |
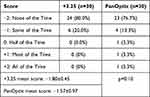 |
Table 10 Frequency of Glasses Use for Arm’s-Length Activities |
The regression equation of “overall satisfaction” for the +3.25 eyes with a R2 of 0.49 is presented in Table 11. The ranked scores for “ability to read very small print without glasses” (p=0.001) and “UIVA Jaeger” (p=0.024) were significant predictors of “overall satisfaction” in the eyes receiving a +3.25 IOL. The regression equation of “overall satisfaction” for the PanOptix eyes with an R2 of 0.93 is presented in Table 11. As observed with the +3.25 eyes, variables related to near and intermediate vision were also very significant predictors of “overall satisfaction” for the PanOptix eyes (UIVA Jaeger, p<0.001, “frequency of glasses use very small print”, p<0.001, and “ability to perform arm’s length activities without glasses”, p<0.001).
 |
Table 11 Multivariate Regression Equations |
However, the regression equation for the PanOptix eyes differs from the +3.25 eyes with the notable addition of two variables related to contrast sensitivity. The computer generated (M&S CTS) response for both “linear mesopic sine wave” contrast sensitivity with glare (p=0.001) and without glare (p=0.015) were significant predictors of patient’s ranked scores for “overall satisfaction.” A data point for analysis was collected at four different spatial frequencies (1.5, 3.0, 6.0, and 12.0 cycles per degree) for linear mesopic sine wave contrast sensitivity both with and without glare. An additional linear mesopic sine wave contrast sensitivity variable was created by analyzing the area under the curve (AUC) created by plotting all four spatial frequencies against the log of contrast sensitivity with glare (Figure 2A) and without glare (Figure 2B).
The two “linear mesopic sine wave” variables significantly influencing patient responses for “overall satisfaction” in the PanOptix eyes represented the entire area under the curve (AUC) for contrast sensitivity with and without glare. There were no significant differences in the actual amounts of contrast sensitivity between the +3.25 eyes and the PanOptix eyes. However, multivariate regression analysis revealed that there is a dramatic difference in how much this given amount of mesopic linear contrast sensitivity influences patient responses regarding overall satisfaction between the two IOLs.
Two of the five variables in the “overall satisfaction” regression equation for the PanOptix eyes were related to intermediate vision. To further explore patient satisfaction scores with the PanOptix eyes, the science of statistics allows us to perform additional regression by using variables related to intermediate vision as dependent variables to be regressed against all other independent variables. When “frequency of glasses use for arm’s length activities” was the dependent variable (Supplemental Table 2), a regression equation with an R2 of 0.44 detected two contrast sensitivity variables significantly influencing patient responses for the need to wear glasses when performing tasks involving intermediate vision. “Linear mesopic sine wave” contrast sensitivity (p<0.001) and “bullseye mesopic” contrast sensitivity (p=0.004) significantly influenced patients’ ranked scores for intermediate function in the eyes with the PanOptix IOL. This is noteworthy because of the strong link between intermediate vision and “overall satisfaction” in PanOptix eyes as established by the original regression and the consistent detection of variables related to contrast sensitivity.
Variables related to intermediate vision for the +3.25 eyes were also analyzed as dependent variables and regressed against all other independent variables. When “UIVA Jaeger” (a significant predictor of “overall satisfaction” for +3.25 eyes) was regressed as the dependent variable (Supplemental Table 3), a regression equation with an R2 of 0.89 detected the single variable of “photopic pupil size” as a significant predictor of “UIVA Jaeger” in the +3.25 eyes.
The relationship between pupillary size and uncorrected intermediate vision in +3.25 eyes is also very noteworthy and will be addressed in the discussion.
Discussion
Intermediate vision has become progressively more important with increasing use of handheld devices and computers. Several studies have reported that the PanOptix trifocal IOL provides reasonably adequate uncorrected distance, intermediate, and near vision leading to consistent high levels of patient satisfaction.19–24
It is widely accepted that dividing light into multiple foci can negatively impact the quality of vision by decreasing contrast sensitivity. An objective of this study was to investigate if the advantages of enhancing intermediate vision, as perceived by the patient, would outweigh the potential negative impact on the quality of vision from splitting light into 3 foci. The contralateral design with patient preference and regression analysis created a model allowing the patient to directly compare the quality of vision provided by each multifocal IOL. This facilitated the simultaneous “side by side” comparison of subjective perceptions of visual quality and the quantification of objective clinical metrics. Reporting “good” bilateral objective visual results for uncorrected distance, intermediate, and near vision with multifocal IOLs, without collecting subjective data regarding patient satisfaction and/or spectacle independence, has been increasingly viewed as an inadequate assessment of a multifocal IOL’s true overall performance.
There are no other reports in the literature where the PanOptix IOL is directly compared to other multifocal or EDOF IOLs using a contralateral design. The results of this study suggests that the “optical cost” of splitting light into 3 foci influenced the patient preference outcomes. What else is known that may help explain the results observed for patient preference and overall satisfaction. The neutralization of spherical aberration is much greater for the +3.25 (−.27) compared to the PanOptix (−.10). The Abbe number which indicates the efficiency in neutralizing chromatic aberrations is also more favorable for the +3.25 IOL (Abbe # TMF +3.25 equals 55 and Abbe # PanOptix equals 37).
What might explain the dichotomy between the objective and subjective results for uncorrected intermediate vision. In a well-illuminated exam room with a near card that has a very white background with perfectly contrasted black letters, the PanOptix eye performed significantly better than the +3.25 (J 1.17 vs J 1.63) for uncorrected intermediate vision. In contrast, the subjective variables for intermediate vision showed either no difference between IOLs or a trend in favor of the +3.25 representing the daily functional experience of everyday life. When “frequency of glasses use for arm’s length activities” for the PanOptix IOL (Supplemental Table 2) was used as the dependent variable in the regression analysis, multiple variables related to contrast sensitivity were detected as significant predictors of satisfaction when performing intermediate tasks. No variables related to contrast sensitivity were significant predictors of intermediate vision or overall satisfaction for the +3.25 IOL.
Interestingly, the only significant variable affecting intermediate vision for the +3.25 eyes was photopic pupil size. The correlation between pupil size and intermediate vision with the Tecnis +4.00 and Tecnis +3.25 multifocal IOLs has been previously reported.25 It showed that as pupil size decreases, uncorrected intermediate vision increases. The manufacturer subsequently reported identical findings (Supplemental Figure 1) from the original IDE trial that corroborated the strong correlation between pupil size and intermediate vision. The 1.00 mm central zone contained in all Tecnis multifocal IOLs facilitates the increase in intermediate vision as the size of the pupil decreases. The 1.00 mm central zone is essentially functioning as an intermediate lens because it has one half the power of the full near add for that particular Tecnis multifocal IOL. For example, the central zone of the +3.25 multifocal contains a 1.63 D add. It is theorized that, as the pupil diameter decreases, a greater percentage of light passes through the central intermediate zone which further enhances the uncorrected intermediate vision. The intermediate vision is enhanced, especially in patients with smaller pupils, without splitting light into 3 foci. The optics of this pupillary effect are probably more similar to those observed with an extended depth of focus IOL rather than with a classic multifocal IOL. This would provide more of a range of intermediate vision in contrast to the specific “peak” at 60 cm observed with the PanOptix IOL and likely have a less negative impact on contrast sensitivity.
The contrast sensitivity issues related to intermediate vision for the PanOptix IOL and the central intermediate zone of the +3.25 IOL may help explain the dichotomy between the objective and subjective findings for intermediate vision. It may also help explain the core findings of the study – that the so-called bifocal +3.25 was significantly preferred to the trifocal PanOptix IOL.
Differences in methodology and inconsistencies with results make it difficult to directly compare contrast sensitivity outcomes in studies with the PanOptix IOL. Menucci12 reported better contrast sensitivity under both photopic and mesopic conditions for the Symfony EDOF versus the PanOptix. Vilar24 reported that a blended combination of bifocal implants performed better at 3, 6, and 12 cycles per degree for mesopic contrast sensitivity with glare versus the PanOptix IOL. Better contrast sensitivity under photopic conditions without glare was better at 3 and 6 cycles per degree for a combination of Tecnis IOLs (Symfony and Tecnis +4.00) compared to bilateral PanOptix IOLs.9
In conclusion, the patients in this study significantly preferred the Tecnis +3.25 IOL to the PanOptix trifocal IOL when given the chance to compare them side by side. Multivariate regression analysis strongly suggested that issues related to contrast sensitivity with the PanOptix IOL may be responsible for the significant preference for the Tecnis +3.25.
Conclusion
- Despite achieving better objective uncorrected intermediate vision with a trifocal IOL, patients still prefer and can achieve greater levels of overall satisfaction with a bifocal IOL.
- Regression analysis strongly suggested that issues related to contrast sensitivity may be responsible for the patient’s subjective preference for the bifocal IOL.
Disclosure
The author has received financial support for the conduct of this study and receives financial support for the conduct of investigator-initiated studies outside this work from Johnson & Johnson Vision (Santa Ana, CA, USA). The author has no proprietary or commercial interest in medical devices involved in this manuscript.
References
1. de Silva SR, Evans JR, Kirthi V, Ziaei M, Leyland M. Multifocal versus monofocal intraocular lenses after cataract extraction. Cochrane Database Syst Rev. 2016;12(12):CD003169. doi:10.1002/14651858.CD003169.pub4
2. Nuzzi R, Tridico F. Comparison of visual outcomes, spectacles dependence and patient satisfaction of multifocal and accommodative intraocular lenses: innovative perspectives for maximal refractive-oriented cataract surgery. BMC Ophthalmol. 2017;17(1):12. doi:10.1186/s12886-017-0411-9
3. Crispim J, Nose R, Yogi M, Nose W. Refractive and visual outcomes of different intraocular lenses with femtosecond laser cataract surgery: the expectation of Independence from spectacles. Open Ophthalmol J. 2015;9(1):145–148. doi:10.2174/1874364101509010145
4. de Vries NE, Nuijts RMMA. Multifocal intraocular lenses in cataract surgery: literature review of benefits and side effects. J Cataract Refract Surg. 2013;39(2):268–278. doi:10.1016/j.jcrs.2012.12.002
5. de Vries NE, Webers CAB, Touwslager WRH, et al. Dissatisfaction after implantation of multifocal intraocular lenses. J Cataract Refract Surg. 2011;37(5):859–865. doi:10.1016/j.jcrs.2010.11.032
6. Gundersen KG, Potvin R. Comparison of visual outcomes and subjective visual quality after bilateral implantation of a diffractive trifocal intraocular lens and blended implantation of apodized diffractive bifocal intraocular lenses. Clin Ophthalmol. 2016;10:805–811. doi:10.2147/OPTH.S107162
7. Ribeiro FJ, Ferreira TB. Comparison of visual and refractive outcomes of 2 trifocal intraocular lenses. J Cataract Refract Surg. 2020;46(5):694–699. doi:10.1097/j.jcrs.0000000000000118
8. Gatinel D, Houbrechts Y. Comparison of bifocal and trifocal diffractive and refractive intraocular lenses using an optical bench. J Cataract Refract Surg. 2013;39(7):1093–1099. doi:10.1016/j.jcrs.2013.01.048
9. de Medeiros AL, de Araujo Rolim AG, Motta AFP, et al. Comparison of visual outcomes after bilateral implantation of a diffractive trifocal intraocular lens and blended implantation of an extended depth of focus intraocular lens with a diffractive bifocal intraocular lens. Clin Ophthalmol. 2017;11:1911–1916. doi:10.2147/opth.s145945
10. Cochener B, Boutillier G, Lamard M, Auberger-Zagnoli C. A comparative evaluation of a new generation of diffractive trifocal and extended depth of focus intraocular lenses. J Refract Surg. 2018;34(8):507–514. doi:10.3928/1081597X-20180530-02
11. Hayashi K, Sato T, Igarashi C, Yoshida M. Comparison of visual outcomes between bilateral trifocal intraocular lenses and combined bifocal intraocular lenses with different near addition. Jpn J Ophthalmol. 2019;63(6):429–436. doi:10.1007/s10384-019-00693-4
12. Mencucci R, Favuzza E, Caporossi O, Savastano A, Rizzo S. Comparative analysis of visual outcomes, reading skills, contrast sensitivity, and patient satisfaction with two models of trifocal diffractive intraocular lenses and an extended range of vision intraocular lens. Arbeitsphysiologie. 2018;256(10):1913–1922. doi:10.1007/s00417-018-4052-3
13. Monaco G, Gari M, Di Censo F, Poscia A, Ruggi G, Scialdone A. Visual performance after bilateral implantation of 2 new presbyopia-correcting intraocular lenses: trifocal versus extended range of vision. J Cataract Refract Surg. 2017;43(6):737–747. doi:10.1016/j.jcrs.2017.03.037
14. Vilar C, Hida WT, de Medeiros AL, et al. Comparison between bilateral implantation of a trifocal intraocular lens and blended implantation of two bifocal intraocular lenses. Clin Ophthalmol. 2017;11:1393–1397. doi:10.2147/OPTH.S139909
15. Yesilirmak N, Akova YA, Donmez O. Comparison of mix-and-match implanted bifocal IOLs and bilateral implanted trifocal IOLs after femtosecond laser-assisted cataract surgery. J Refract Surg. 2019;35(9):559–564. doi:10.3928/1081597X-20190806-01
16. Zamora-de-la-Cruz D, Garzón M, Chávez-Mondragón E. Comparison of visual results and quality of vision after bilateral implantation of trifocal intraocular lenses versus bifocal intraocular lenses. Rev Mex Oftalmol. 2019;92:2. doi:10.24875/rmoe.m18000004
17. Kohnen T. Questionnaires for cataract and refractive surgery. J Cataract Refract Surg. 2019;45(2):119–120. doi:10.1016/j.jcrs.2018.12.020
18. Lwowski C, Pawlowicz K, Petermann K, et al. Visual and patient-reported factors leading to satisfaction after implantation of diffractive extended depth-of-focus and trifocal intraocular lenses. J Cataract Refract Surg. 2022;48(4):421–428. doi:10.1097/j.jcrs.0000000000000780
19. García-Pérez JL, Gros-Otero J, Sánchez-Ramos C, Blázquez V, Contreras I. Short term visual outcomes of a new trifocal intraocular lens. BMC Ophthalmol. 2017;17(1):72. doi:10.1186/s12886-017-0462-y
20. Kohnen T, Herzog M, Hemkeppler E, et al. Visual performance of a quadrifocal (trifocal) intraocular lens following removal of the crystalline lens. Am J Ophthalmol. 2017;184:52–62. doi:10.1016/j.ajo.2017.09.016
21. Lawless M, Hodge C, Reich J, et al. Visual and refractive outcomes following implantation of a new trifocal intraocular lens. Eye Vis. 2017;4(1):10. doi:10.1186/s40662-017-0076-8
22. Alió JL, Plaza-Puche AB, Alió Del Barrio JL. Clinical outcomes with a diffractive trifocal intraocular lens. Eur J Ophthalmol. 2018;28(4):419–424. doi:10.1177/1120672118762231
23. Alfonso JF, Fernández-Vega-Cueto L, Fernández-Vega L, Montés-Micó R. Visual function after implantation of a presbyopia-correcting trifocal intraocular lens. Ophthalmic Res. 2020;63(2):152–164. doi:10.1159/000500834
24. Bissen-Miyajima H, Ota Y, Hayashi K, Igarashi C, Sasaki N. Results of a clinical evaluation of a trifocal intraocular lens in Japan. Jpn J Ophthalmol. 2020;64(2):140–149. doi:10.1007/s10384-019-00712-4
25. Bucci FA
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.