Back to Journals » Patient Preference and Adherence » Volume 12
Patient–doctor relationship and adherence to capecitabine in outpatients of a German comprehensive cancer center
Authors Hefner J, Berberich S, Lanvers E, Sanning M, Steimer AK, Kunzmann V
Received 27 March 2018
Accepted for publication 10 July 2018
Published 21 September 2018 Volume 2018:12 Pages 1875—1887
DOI https://doi.org/10.2147/PPA.S169354
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Jochen Hefner,1 Sara Berberich,2 Elena Lanvers,3 Maria Sanning,4 Ann-Kathrin Steimer,5 Volker Kunzmann6
1Section of Psychosomatic Medicine, Department of Internal Medicine II, University of Wuerzburg, Bavaria, Germany; 2Medical Student, Faculty of Medicine, University of Wuerzburg, Bavaria, Germany; 3Intensive Care Unit, Children’s Hospital of the City of Cologne, North Rhine-Westphalia, Germany; 4Department of Internal Medicine II, St Johannes Hospital Dortmund, North Rhine-Westphalia, Germany; 5Catholic Children’s Hospital Wilhelmsstift, Hamburg, Germany; 6Section of Clinical Oncology, Department of Internal Medicine II, University of Wuerzburg, Bavaria, Germany
Purpose: The prescribing of oral chemotherapy agents has introduced the new challenge of ensuring patients’ adherence to therapy. Aspects of a close patient–doctor relationship are reported to be correlated with adherence to oral anticancer drugs, but data on capecitabine are scarce.
Patients and methods: Sixty-four outpatients with a diagnosis of cancer and prescribed capecitabine were recruited from a German Comprehensive Cancer Center. We used the Patient–Doctor Relationship Questionnaire (PDRQ-9), the Medical Adherence Rating Scale (MARS), the Beliefs about Medicines Questionnaire (BMQ), and the Satisfaction with Information about Medicines Scale (SIMS) to assess patients’ perceptions and behavior. Medical data were extracted from the charts.
Results: Non-adherence was reported by 20% of the 64 participants. The perceived quality of the patient–doctor relationship was high in general, but it did not emerge as a predictor of adherence in our survey (odds ratio [OR]=0.915, P=0.162, 95% CI=0.808–1.036). However, beliefs about medicine (OR=1.268, P<0.002; 95% CI=1.090–1.475) as well as satisfaction with information about medicine (OR=1.252, P<0.040, 95% CI=1.010–1.551) were predictors of adherence and the quality of the patient–doctor relationship was correlated with both variables (r=0.373, P=0.002 for SIMS sum score; r=0.263, P=0.036 for BMQ necessity/concern difference). Overall, adherence to capecitabine was high with a conviction that the therapy is necessary. However, concerns were expressed regarding the long-term effect of capecitabine use. Patients have unmet information needs regarding interactions of capecitabine with other medicines and the impairment of their intimate life.
Conclusions: In order to ensure adherence to capecitabine, our results seem to encourage the default use of modern and perhaps more impersonal means of information brokerage (eg, email, internet). However, the contents of some of patients’ informational needs as well as the associations of patients’ beliefs and satisfaction about the information received suggest a benefit from a trustful patient–doctor relationship.
Keywords: oral anticancer drugs, capecitabine, adherence, patient–doctor relationship, beliefs in medication, satisfaction with information about medicines
Introduction
With progress in diagnostics and therapy, cancer is becoming more and more a chronic disease. In the case of most numerous cancer entities (ie, colon or breast cancer), and especially if the tumor has spread out to surrounding tissue or to lymph nodes, patients will usually receive chemotherapy protocols, some of them based on 5-fluorouracil (5-FU).1 Such protocols are regarded as crucial for the treatment of patients in the upcoming years.2–4 5-FU, which is usually administered intravenously, typically causes various side effects common in drugs directed nonspecifically at fast growing cells.5 The prodrug capecitabine, that converts to 5-FU within tumors, allowed to reduce the spectrum and magnitude of side effects. Its oral administration has also shown efficacy and safety comparable to intravenous fluorouracil, and was preferred by patients.1,6,7 Even though there are apparent benefits to oral drug administration, health care professionals are facing new challenges. Dose is controlled when intravenously administered by a member of the health care staff. With oral therapy self-managed by patients, however, the dosage is not externally controlled. There is little research on adherence to capecitabine, and adherence rates ranging between 60% and 90% have been demonstrated.8–19 Even less is known about the risk of over-adherence in patients receiving capecitabine.20–22 Although the numbers generally appear to be satisfying, even a small variation of adherence may result in adverse clinical consequences.14,20–23
If patients do not take the prescribed medication as intended by the prescribing person, this can happen due to lack of ability or willingness, and may often be a mixture of intentional and unintentional aspects.24
Indicators of a close patient–doctor relationship (ie, to involve patients in the process of decision making, to treat them as equals, and to avoid unresolved issues regarding prescriptions) were linked to adherence to medication in a large study comprising 45,700 patients from 24 European countries.25 Data on oral anticancer drugs are scarce, mostly focusing on endocrine therapy after breast cancer, and indicating that a good and trustful patient–doctor relationship is connected with a higher disposition to execute doctors’ instructions regarding medication and adherence.26–29 To our knowledge, only 1 publication with 130 patients from Malaysia exists reporting a linear relationship between satisfaction with health care and adherence to capecitabine.18
Predictors of adherence that have been more frequently cited are perceptions of illness and medication. These factors are influenced by the information available to patients.30–32 Research results hint to the fact that many patients have a rather negative perspective concerning pharmaceuticals, assessing them generally as harmful, permanently weighing their convictions regarding the necessity of medication (perceived benefits) against their worries about possible negative impacts (perceived risks).31,33 Data from oncological studies show a connection between cancer patients’ doubts concerning the efficacy of the treatment, worries about side effects, depressive symptoms, and poorer adherence, for example.29,34,35 Patients who have doubts about the necessity of their medication may more likely willfully skip or reduce doses, or may be more inclined to forget to take their medication. Likewise, patients who are highly concerned about side effects may reduce the dosage on purpose in order to reduce the suspected risk.31
Regarding capecitabine, 2 studies focused on patients’ medication-related convictions and their satisfaction with the information obtained, and did not find a significant connection with adherence.14,23 The authors claimed that the high adherence rate in both samples could have influenced the results.14,23
However, Bhattacharya et al found that patients’ satisfaction with the information they had received on capecitabine correlated negatively with high concerns regarding the medication.23
To our knowledge, data on the association between the patient–doctor relationship and beliefs about capecitabine as well as satisfaction with information on this specific drug are lacking. Only Grassi et al reported a link between perceptions of a supportive role of the doctor and beliefs about the necessity of an antitumor therapy.36 Regarding the relevance of capecitabine, more insight into factors influencing adherence is needed. Therefore, this study examined associations between patients’ perceptions of their relationship with doctors and adherence. Furthermore, associations between those perceptions and beliefs about their cancer treatment as well as satisfaction with the information about their medicine were examined.
We hypothesized that poorer patient–doctor relationship would be related to negative beliefs about cancer medication, lower satisfaction with information about medication, and lower adherence rates. Exploring those associations and identifying possible opportunities for improvement can help health care professionals to enhance services related to prescribing medicines such as capecitabine in order to ameliorate adherence.
Subjects and methods
Participants
The study design was a cross-sectional single center study. We recruited cancer patients undergoing chemotherapy with capecitabine at outpatient clinics, day hospitals and doctors’ offices of the Comprehensive Cancer Center of the University of Wuerzburg, Germany. These units started to cooperate just recently and our commitment was to monitor adherence from the outset. Participants were recruited from September 1, 2015 to March 1, 2017. They were able to participate in this trial after providing written informed consent. The study procedure was previously approved by the Medical Faculty’s Ethics Committee of Wuerzburg University, Germany, in accordance with the Declaration of Helsinki.
Measures
- The Patient–Doctor Relationship Questionnaire 9 (PDRQ-9) consists of 9 items, and is aimed at capturing patients’ perception of the relationship with their physician.37,38 Central items are inquiring whether patients are experiencing a trustworthy, communicative relationship with an effective and helpful health professional.37,38 The response format is a 5-point scale ranging from 1 (not at all) to 5 (totally). The higher the scores, the higher the patient’s satisfaction with the patient–doctor relationship.37
- The Medication Adherence Report Scale (MARS) is a 5-item self-report instrument focusing on non-adherent behavior (like “I forgot to take them” or “I alter the dose”).39 The possible answers range from 1 (always) to 5 (never) on a 5-point Likert scale (overall range from 5 to 25). Lower scores are interpreted as indicators of lower levels of adherent behavior.39 In our context, patients scoring less than 25 were considered as non-adherent.
- The Satisfaction with Information about Medicines Scale (SIMS) is a questionnaire aiming at evaluating the extent to which patients feel satisfied with the information they have received about prescribed drugs.32 Each of its 17 items refers to a particular aspect of medicine use. Participants can assess the amount of information they have received according to the following response categories: “too much”, “about right”, “too little”, “none received”, “none needed”. There are 3 levels of response analysis: a detailed medicine information profile, resulting from examining the ratings for each individual item in order to identify individual kinds of information that patients feel they are missing; a total satisfaction rating, resulting from summing up the scores for each item; and two subscale scores, identifying patients’ satisfaction with information about the action and usage of medication (items 1–9), and the potential problems of medication (items 10–17). Ratings with “about right” or “none needed,” indicating the patient’s satisfaction with a particular aspect of medication information, are assigned a score of 1. Ratings of “too much,” “too little,” or “none received,” indicating the patient’s dissatisfaction with the information provided, are scored 0. A range from 0 to 17 is covered, with high scores standing for a high degree of overall satisfaction with the amount of information received on the medication.
- The Beliefs about Medicines Questionnaire (BMQ) includes 2 scales of 5 items each assessing patients’ beliefs about the necessity of the prescribed medication in order to control their disease and their concerns about possible negative consequences of taking it.31 The response format to indicate the degree of agreement with each statement is a 5-point Likert scale, ranging from 1 (strongly disagree) to 5 (strongly agree). Individual item scores within both scales are summed up. Thus, total scores for the Necessity and Concerns Scales range from 5 to 25. Higher scores indicate stronger beliefs; scores above 12.5 indicate strong belief.31 A necessity–concerns differential is calculated as the difference between the necessity and the concerns scales, with a possible range of −20 to +20. This differential can be thought of as the cost–benefit analysis for each patient, for whom costs (concerns) are weighed against their perceived benefits (necessity beliefs).31
- Clinical and sociodemographic variables were extracted from the charts. Patients were invited to score their perceived burden of common side effects on a visual analog scale with a range from 0 (not at all) to 100 (maximum).
Statistical analyses
The data were mainly at ordinal or categorical level or did not follow a normal distribution. Hence, non-parametric testing was employed. SPSS version 24 was used for data analysis. Medians and interquartile range (IQR, 25%- and 75%-quantiles) within the participant population were calculated using appropriate descriptive statistics. For categorical parameters, absolute and relative frequencies were reported. The comparison of 2 interval data sets was carried out using Spearman’s rank correlation coefficient, and Mann–Whitney’s U-analysis for dichotomized data.
Multivariate logistic regression models were used to identify the independent factors associated with adherence to capecitabine, with adjustments for age, gender and time since diagnosis.40,41 Variables with a P-value of 0.25 or less in the bivariate analyses were integrated in a multivariate logistic regression model employing the backward variable selection method. Odds ratios and 95% confidence intervals (95% CI) were computed for each variable in the final model, P<0.05 (2-sided) was regarded as statistically significant in all statistical tests.
Results
Sociodemographics and clinical data
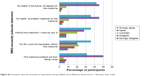
Sixty-four patients completely filled in their questionnaires. Females accounted for 17 participants (27%) of the sample, and the mean (SD) age was 66 (±12.1) years (Table 1). Capecitabine was part of a combination therapy for 22 (34%) participants, while 25 (39%) had a palliative rather than an active treatment regime. Fifty-four (84%) participants were diagnosed with colorectal cancer. Other diagnoses were stomach cancer (n=6; 9%), breast cancer (n=2; 3%), pancreatic cancer (n=1; 2%) and an epithelial tumor of unknown origin (n=1; 2%). Table 1 also presents relevant clinical data for the sample population. Participants were mostly in their second year from cancer diagnosis and in their first year of capecitabine treatment. The most troubling side effect was hand-foot syndrome (median=35, IQR 1.25–80), followed by fatigue (median=30, IQR 15–60). Figure 1 presents the extent to which participants declared to feel troubled by the side effects most frequently reported.
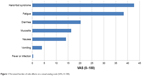  | Figure 1 Perceived burden of side effects on a visual analog scale (VAS, 0–100). |
Satisfaction with patient–doctor relationship
Median of the mean score on the PDRQ-9 was 4.61 (IQR 4–5), indicating a high satisfaction of patients with their relationships with their doctors. Most of the patients were convinced that their physician was dedicated to helping them (67%); they perceived that their physician was easily accessible (63%) and that communication was straightforward (63%, Table S1, Figure S1).
Adherence
Thirteen participants reported non-adherence, and 2 of them reported multiple methods of deviation. Forgetting to take a dose was the method of deviation reported most frequently, and the extent to which this occurred was mainly described as “rarely” by participants (Table S2). Participants reporting non-adherent behavior and those reporting no deviation did not differ significantly in demographic or clinical characteristics.
Patient beliefs about medication
The sample’s positive median (IQR) BMQ differential score was 4.00 (0.26–8.75). This can be interpreted as participants’ beliefs in necessity on average outweighing concerns about capecitabine treatment. Fifty-nine (92%) patients scored >12.5 on the BMQ-N subscale, which indicates their strong beliefs in the necessity of capecitabine treatment. Forty-three (67%) participants scored >12.5 on the BMQ-C subscale, indicating strong concerns regarding capecitabine treatment. The necessity–concerns differential yielded negative results for 13 participants, indicating that concerns regarding oral anticancer therapy outweighed necessity beliefs. The strongest necessity beliefs were for “My health in the future will depend on this medicine”, for “My health, at present, depends on this medicine” and “Without this medicine I would be very ill”. The strongest concerns referred to long term effects of capecitabine intake (Figures S2 and S3).
Satisfaction with information about medicines
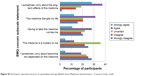
Figure 2 demonstrates the distribution of responses of the SIMS. Eleven participants reported complete satisfaction with the information provided about capecitabine therapy. Missing information or dissatisfaction with the information provided was mostly reported for the questions of whether the medication will affect one’s sex life and whether capecitabine interferes with other drugs. The median of the subscale on patients’ satisfaction with information about the action and usage of medication was 6.7 (IQR 6–9). The median of the subscale on potential problems of medication was 5 (IQR 4–7).
  | Figure 2 Participant satisfaction with information received (Satisfaction with Information about Medicines Scale, n=64). |
Potential predictors of outcome measures
Sociodemographic variables, clinical variables including side effects and adherence did not correlate significantly (Tables 2 and 3). The P-value in the bivariate analyses of PDRQ-9 sum score and adherence was 0.23. Furthermore, there were no significant correlations between the PDRQ-9 single item score and adherence.
  | Table 3 Correlations between adherence and sociodemographic and medical variables (n=64) using Fishers exact test |
Significant small to moderate positive correlations could be found between the PDRQ-9 sum score and the SIMS sum score (Spearman’s r=0.373, P=0.002), the SIMS subscale on action and usage of medication (Spearman’s r=0.268, P=0.032), and the SIMS subscale on potential problems of medication (Spearman’s r=0.408, P=0.001), respectively. These results illustrate that patients who were more satisfied with the patient–doctor relationship were generally more satisfied with the information received about their medicine. Those patients also reported greater satisfaction with the received information about action, usage and potential problems of their medication.
Furthermore, a small positive correlation between the PDRQ-9 and the BMQ necessity–concerns differential (Spearman’s r=0.263, P=0.036) was detected, suggesting that those patients outweigh necessities against concerns and fears regarding their therapy.
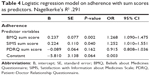
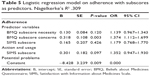
Two logistic regression models were investigated, both with adherence as dependent variable. In the first model, the sum scores of BMQ, SIMS and PDRQ-9 were used as predictors. In the second model, the predictors were the sub-scores of BMQ and of SIMS. There were no confounding factors adjusted for as we found no significant correlations between sociodemographic and medical variables with adherence in our sample. The requirements of logistic regression (no multicollinearity, no outliers, log linearity) were checked with appropriate methods and were met in both models.
Nagelkerke’s R2 for the logistic regression model including sum scores of BMQ, SIMS and PDRQ-9 was 0.291, and for the model including subscores of BMQ and SIMS was 0.309, respectively. The BMQ sum score (OR=1.268, P=0.002, 95% CI=1.090–1.475), the SIMS sum score (OR=1.252, P=0.040; 95% CI=1.010–1.551) and the BMQ concern subscore (OR=1.374, P=0.003, 95% CI=1.112–1.699) were detected as significant positive predictors of adherence. The effect of the PDRQ-9 sum score (OR=0.915, P=0.162; 95% CI=0.808–1.036) as well as of the BMQ-necessity subscale (OR=1.139, P=0.120, 95% CI=0.967–1.343) or the SIMS subscales (action and usage OR=1.179, P=0.426, 95% CI=0.768–1.770; potential problems OR=1.352, P=0.097, 95% CI=0.947–1.930) on adherence were not significant (Tables 4 and 5).
Discussion
We initiated a survey on the associations between the patient–doctor relationship and beliefs or satisfaction with information about capecitabine in a sample of outpatients treated with oral capecitabine in the clinical setting of a German Comprehensive Cancer Center. The patient-reported adherence rate to capecitabine of 80% in our study is in line with previous research results based on different types of monitoring.8–19 The non-adherence reported was primarily “forgetting,” a reason for deviation which is thought of as more socially acceptable by patients than intentional behaviors (ie, missing or altering a dose).23,42–45 Almost three-quarters of the participants were men (n=47, 73%), and about one third suffered from metastatic illness. The primary tumor sites were mainly colorectal (84%), gastric (9%), and breast cancer (3%). Sixty-four percent of patients received capecitabine as a monotherapy. The mean time since tumor diagnosis and start of capecitabine therapy was 19 and 7 months, respectively. Hand-foot syndrome followed by fatigue was reported by most participants to be troubling, which is in line with other studies.23
We found no correlations between sociodemographic or clinical characteristics, perceived intensity of side effects and adherence, which is counterintuitive at first sight but in line with other studies reporting mixed results.8,10,12,13,19,46,47
Results of the PDRQ-9 show a high level of patients’ satisfaction with the relationship with their doctors (M=4.43, SD=0.63). The levels of satisfaction regarding the total score as well as single items are in fact higher than in a representative German survey focusing on the relationship with the family physician.48
Contrary to our assumption, neither the patients’ evaluation of the patient–doctor relationship in general nor single aspects of this relationship were predictors of adherence to oral capecitabine therapy. Our results seem to contradict those of Zahrina et al, where satisfaction with care was associated with adherence.18 In our study, we focused primarily on the patient–doctor relationship, whereas Zahrina et al examined satisfaction with appointments and pharmacy services as well.18
Our data represent the association between the perceived interactions with doctors and satisfaction with information about capecitabine. At the same time, fewer patients in our study (17%) were totally satisfied with the information received than in previous reports (60%).23 The participants expressed their request for (more) information on how capecitabine may affect their sex life. Further studies may help to ascertain the importance of the topic to this population. However, we believe that health care professionals may increase levels of satisfaction by referring empathically to this topic and providing information. Although connections between the use of capecitabine, alcohol intake and hand-foot syndrome have been reported, many patients did not know whether alcohol consumption was allowed during therapy.49 The lack of satisfaction with information regarding drug interactions was also of concern in a sample where the majority used additional medication.49
We found associations between patients’ perceptions of their interactions with their doctors and beliefs about anticancer treatment, a result also described by Grassi et al.36 In line with their results we show that patients perceiving their doctors as supportive and empathic were more likely to believe that their therapy was necessary and were less likely to be concerned about it. These data confirm and expand the literature on cancer patients’ beliefs about medication by highlighting the possible role of the patient–doctor relationship.36 Regarding the BMQ questionnaire, our patients valued the beliefs about necessities of medication over the concerns about medication (4.77); the difference is notably smaller than in previous studies (7.8).23 Although patients reported concerns about capecitabine therapy, these were outweighed by the conviction that it is necessary. Regarding other chronic conditions, it is known that perceived necessity can be considerably lower and our results may reflect patients’ notions of cancer as an especially threatening condition.31,50
In contrast to studies with similar adherence rates, we found that satisfaction with information as well as beliefs about capecitabine were predictive of adherence (CI=1.2–1.3).14,23 We did not examine mediator effects of the PDRQ-9 in this context.
Scores of the SIMS and the BMQ were correlated in the sense that patients who were more satisfied with the information they had received were more convinced that medication with capecitabine was necessary. Satisfaction with information about capecitabine, however, was negatively related to concerned beliefs about the drug, as has been described before.23 This named relationship is likely to be mutually reinforcing. Patients who are unhappy with the information provided are likely to be more concerned about their therapy. At the same time, those more concerned about drug intake are likely to wish for more information.23
Our study has several limitations. The sample size is small and has been drawn from a single Comprehensive Cancer Center (CCC). The single units of the CCC started only recently and we conducted this initial survey for about 18 months. Due to organizational reasons, we could not obtain data on the majority of breast cancer patients and were not able to obtain data on dropouts. Larger sample sizes and preferentially multicenter studies are necessary to produce more generalizable results. For example, we cannot explain why concerns about medication also predicted adherence. It would be of great interest to us whether these data will be replicated in larger surveys.
We believe that a good patient–doctor relationship may act indirectly on adherence via beliefs and satisfaction with information about capecitabine. From a mathematical point of view though, we refrained from calculating moderator effects due to the small sample size. Furthermore, the number of variables and interrelationships in our study may lead to errors by multiple testing. The significant P-value was not adjusted as we intended to broadly explore patients’ experiences in daily practice. Regarding the screening instruments, patients’ perceptions were surveyed with questionnaires, while clinical interviews could have provided more specific information. Also, due to a self-presentation bias possibly resulting in overestimation, self-reported adherence ratings should be treated cautiously.51 Ultimately, all existing measures of adherence have their shortcomings, as they are neither objective nor very suitable for daily practice.52,53 Up till today, a well-validated scale designed particularly for oral anticancer drugs adherence has not yet been developed.54 Most adherence scales used contain items focusing on measuring patients’ behavior related to taking their medication rather than their perceptions and beliefs. Another major limitation of our approach is the fact that we did not screen for over-adherence, a phenomenon which may lead to adverse reactions and may result from misunderstandings or flawed communication.20 We are therefore not able to expand the literature on this issue of increasing relevance.20–22 Finally, future studies may also benefit from measuring changes of patients’ perceptions and adherence over time, as we only adopted a cross-sectional design. Longitudinal studies may reveal significant associations at certain timepoints, ie, at the beginning of treatment.
On the other hand, our study provides valuable information and constructive suggestions for future research. It is well established that adherence should be monitored not only in clinical trials but also in daily routine, since the rates of adherence with oral medication in the structured environment of clinical trials are commonly greater.43,55,56
We decided to use mainly patient-reported outcome (PRO) measures, as perceptions that doctors may sometimes not be aware of are often the ones that really motivate the patient to follow a given treatment.57
In contrast to other reports, information about capecitabine as well as beliefs about the drug were examined in a narrow sense, ie, restricted to 1 specific pharmaceutical. More research on distinct types of cancer medication may provide further information.
Summing up, the perceived quality of the patient–doctor relationship did not predict adherence to capecitabine in our sample. Nevertheless, our findings highlight the importance for oncologists to consider patients’ satisfaction within the patient–doctor interaction as variables influencing patients’ satisfaction with information, as well as variables influencing their beliefs and representations of capecitabine. There were no distinct results as to whether the quality of the patient–doctor relationship moderated the effects of information and beliefs regarding capecitabine on adherence. We believe that this question is worth more specific exploration in larger studies. Another implication leads to reports describing that the introduction of modern means of communication such as text messaging and mobile telephone reminders has improved adherence to therapy.58,59 It may well be that the direct patient–doctor relationship is less important than beliefs and information, which could also be addressed by medical professionals other than oncologists. Large studies with intensive pharmaceutical interventions are underway in order to optimize adherence management.60,61 First results on capecitabine are promising.62 Approaches using modern means of communication to ameliorate adherence to oral anticancer drugs have been proven feasible and well accepted, and their results are awaited eagerly.63,64
Publication rights of the German version of the MARS Questionnaire
“Department of General Practice and Health Services Research and Department of Internal Medicine VI, Clinical Pharmacology and Pharmacoepidemiology, University Hospital Heidelberg, Heidelberg, Germany”.
Acknowledgments
E Göbel, J Haas, E Hupp, B Schoettker, and H Reinel provided and cared for study patients. This publication was funded by the German Research Foundation (DFG) and the University of Wuerzburg in the funding programme Open Access Publishing.
Author contributions
All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
American Cancer Society. Cancer Facts & Figures; 2016. Available from: https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2016/cancer-facts-and-figures-2016.pdf. Accessed March 1, 2018. | ||
Carrillo E, Navarro SA, Ramírez A, et al. 5-Fluorouracil derivatives: a patent review (2012–2014). Expert Opin Ther Pat. 2015;25(10):1131–1144. | ||
Weinberg BA, Marshall JL, Hartley M, Salem ME. A paradigm shift from one-size-fits-all to tailor-made therapy for metastatic colorectal cancer. Clin Adv Hematol Oncol. 2016;14(2):116–128. | ||
Mcquade RM, Stojanovska V, Bornstein JC, Nurgali K. Colorectal cancer chemotherapy: the evolution of treatment and new approaches. Curr Med Chem. 2017;24(15):1537–1557. | ||
Twelves C. Vision of the future: capecitabine. Oncologist. 2001;6(Suppl 4):35–39. | ||
Górnaś M, Szczylik C. Oral treatment of metastatic breast cancer with capecitabine: what influences the decision-making process? Eur J Cancer Care. 2010;19(1):131–136. | ||
van Cutsem E, Hoff PM, Harper P, et al. Oral capecitabine vs intravenous 5-fluorouracil and leucovorin: integrated efficacy data and novel analyses from two large, randomised, phase III trials. Br J Cancer. 2004;90(6):1190–1197. | ||
Hirao C, Mikoshiba N, Shibuta T, et al. Adherence to oral chemotherapy medications among gastroenterological cancer patients visiting an outpatient clinic. Jpn J Clin Oncol. 2017;47(9):786–794. | ||
Font R, Espinas JA, Layos L, et al. Adherence to capecitabine in preoperative treatment of stage II and III rectal cancer: do we need to worry? Ann Oncol. 2017;28(4):831–835. | ||
Figueiredo Junior AG, Forones NM. Study on adherence to capecitabine among patients with colorectal cancer and metastatic breast cancer. Arq Gastroenterol. 2014;51(3):186–191. | ||
Amlani A, Kumar A, Ruan JY, Cheung WY. Compliance with adjuvant capecitabine in patients with stage II and III colon cancer: comparison of administrative versus medical record data. Cancer Med. 2016;5(8):1776–1782. | ||
Fernández-Ribeiro F, Olivera-Fernández R, Crespo-Diz C. Adherence and safety study in patients on treatment with capecitabine. Farm Hosp. 2017;41(2):204–221. | ||
Winterhalder R, Hoesli P, Delmore G, et al. Self-reported compliance with capecitabine: findings from a prospective cohort analysis. Oncology. 2011;80(1–2):29–33. | ||
Timmers L, Swart EL, Boons CC, et al. The use of capecitabine in daily practice: a study on adherence and patients’ experiences. Patient Prefer Adherence. 2012;6:741–748. | ||
Mayer EL, Partridge AH, Harris LN, et al. Tolerability of and adherence to combination oral therapy with gefitinib and capecitabine in metastatic breast cancer. Breast Cancer Res Treat. 2009;117(3):615–623. | ||
Partridge AH, Archer L, Kornblith AB, et al. Adherence and persistence with oral adjuvant chemotherapy in older women with early-stage breast cancer in CALGB 49907: adherence companion study 60104. J Clin Oncol. 2010;28(14):2418–2422. | ||
Walter T, Wang L, Chuk K, Ng P, Tannock IF, Krzyzanowska MK. Assessing adherence to oral chemotherapy using different measurement methods: Lessons learned from capecitabine. J Oncol Pharm Pract. 2014;20(4):249–256. | ||
Zahrina AK, Norsa’adah B, Hassan NB, et al. Adherence to capecitabine treatment and contributing factors among cancer patients in Malaysia. Asian Pac J Cancer Prev. 2014;15(21):9225–9232. | ||
Kawakami K, Yokokawa T, Kobayashi K, et al. Self-reported adherence to capecitabine on XELOX treatment as adjuvant therapy for colorectal cancer. Oncol Res. 2017;25(9):1625–1631. | ||
Allen J, Williamson S. Over compliance with capecitabine oral chemotherapy. Int J Clin Pharm. 2014;36(2):271–273. | ||
Spoelstra SL, Given BA, Given CW, et al. An intervention to improve adherence and management of symptoms for patients prescribed oral chemotherapy agents: an exploratory study. Cancer Nurs. 2013;36(1):18–28. | ||
Bourmaud A, Henin E, Tinquaut F, et al. Adherence to oral anticancer chemotherapy: What influences patients’ over or non-adherence? Analysis of the OCTO study through quantitative-qualitative methods. BMC Res Notes. 2015;8:291. | ||
Bhattacharya D, Easthall C, Willoughby KA, Small M, Watson S. Capecitabine non-adherence: exploration of magnitude, nature and contributing factors. J Oncol Pharm Pract. 2012;18(3):333–342. | ||
Bhattacharya D, Wright DJ, Purvis JR, Corlett AJ. Non-adherence in older people; intentional or unintentional? Int J Pharm Pract. 2004;12:R63. | ||
Stavropoulou C. Non-adherence to medication and doctor-patient relationship: Evidence from a European survey. Patient Educ Couns. 2011;83(1):7–13. | ||
Trevino KM, Fasciano K, Prigerson HG, Alliance P-Oncologist. Patient-oncologist alliance, psychosocial well-being, and treatment adherence among young adults with advanced cancer. J Clin Oncol. 2013;31(13):1683–1689. | ||
Ruddy K, Mayer E, Partridge A. Patient adherence and persistence with oral anticancer treatment. CA Cancer J Clin. 2009;59(1):56–66. | ||
Brett J, Fenlon D, Boulton M, et al. Factors associated with intentional and unintentional non-adherence to adjuvant endocrine therapy following breast cancer. Eur J Cancer Care. 2018;27(1):e12601. | ||
Stanton AL, Petrie KJ, Partridge AH. Contributors to nonadherence and nonpersistence with endocrine therapy in breast cancer survivors recruited from an online research registry. Breast Cancer Res Treat. 2014;145(2):525–534. | ||
Horne R, Buick D, Fisher M, Leake H, Cooper V, Weinman J. Doubts about necessity and concerns about adverse effects: identifying the types of beliefs that are associated with non-adherence to HAART. Int J STD AIDS. 2004;15(1):38–44. | ||
Horne R, Weinman J. Patients’ beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illness. J Psychosom Res. 1999;47(6):555–567. | ||
Horne R, Hankins M, Jenkins R. The Satisfaction with Information about Medicines Scale (SIMS): a new measurement tool for audit and research. Qual Health Care. 2001;10(3):135–140. | ||
Heller MK, Chapman SC, Horne R. Beliefs about medication predict the misattribution of a common symptom as a medication side effect – Evidence from an analogue online study. J Psychosom Res. 2015;79(6):519–529. | ||
Hershman DL, Kushi LH, Shao T, et al. Early discontinuation and nonadherence to adjuvant hormonal therapy in a cohort of 8,769 early-stage breast cancer patients. J Clin Oncol. 2010;28(27):4120–4128. | ||
Corter AL, Findlay M, Broom R, Porter D, Petrie KJ. Beliefs about medicine and illness are associated with fear of cancer recurrence in women taking adjuvant endocrine therapy for breast cancer. Br J Health Psychol. 2013;18(1):168–181. | ||
Grassi L, Meggiolaro E, Berardi MA, et al. Beliefs about medicines, doctor-patient relationship, and coping among European patients with cancer. Psychooncology. 2017;26(2):282–285. | ||
van der Feltz-Cornelis CM, van Oppen P, van Marwijk HW, de Beurs E, van Dyck R. A patient-doctor relationship questionnaire (PDRQ-9) in primary care: development and psychometric evaluation. Gen Hosp Psychiatry. 2004;26(2):115–120. | ||
Zenger M, Schaefert R, van der Feltz-Cornelis C, Brähler E, Häuser W. Validation of the Patient-Doctor-Relationship Questionnaire (PDRQ-9) in a representative cross-sectional German population survey. PLoS One. 2014;9(3):e91964. | ||
Mahler C, Hermann K, Horne R, et al. Assessing reported adherence to pharmacological treatment recommendations. Translation and evaluation of the Medication Adherence Report Scale (MARS) in Germany. J Eval Clin Pract. 2010;16(3):574–579. | ||
Partridge AH, Wang PS, Winer EP, Avorn J. Nonadherence to adjuvant tamoxifen therapy in women with primary breast cancer. J Clin Oncol. 2003;21(4):602–606. | ||
Noens L, van Lierde MA, de Bock R, et al. Prevalence, determinants, and outcomes of nonadherence to imatinib therapy in patients with chronic myeloid leukemia: the ADAGIO study. Blood. 2009;113(22):5401–5411. | ||
Atkins L, Fallowfield L. Intentional and non-intentional non-adherence to medication amongst breast cancer patients. Eur J Cancer. 2006;42(14):2271–2276. | ||
Barthélémy P, Asmane-de La Porte I, Meyer N, et al. Adherence and patients’ attitudes to oral anticancer drugs: a prospective series of 201 patients focusing on targeted therapies. Oncology. 2015;88(1):1–8. | ||
Kirk MC, Hudis CA. Insight into barriers against optimal adherence to oral hormonal therapy in women with breast cancer. Clin Breast Cancer. 2008;8(2):155–161. | ||
Eliasson L, Clifford S, Barber N, Marin D. Exploring chronic myeloid leukemia patients’ reasons for not adhering to the oral anticancer drug imatinib as prescribed. Leuk Res. 2011;35(5):626–630. | ||
Kawakami K, Nakamoto E, Yokokawa T, et al. Patients’ self-reported adherence to capecitabine on XELOX treatment in metastatic colorectal cancer: findings from a retrospective cohort analysis. Patient Prefer Adherence. 2015;9:561–567. | ||
Kimura M, Nakashima K, Usami E, et al. Adherence and awareness of the therapeutic intent of oral anticancer agents in an outpatient setting. Oncol Lett. 2015;9(5):2341–2346. | ||
Dinkel A, Schneider A, Schmutzer G, Brähler E, Henningsen P, Häuser W. The quality of the family physician-patient relationship. Patient-related predictors in a sample representative for the German population. Psychother Psychosom Med Psychol. 2016;66(3–4):120–127. | ||
Lassere Y, Hoff P. Management of hand-foot syndrome in patients treated with capecitabine (Xeloda). Eur J Oncol Nurs. 2004;8(Suppl 1):S31–S40. | ||
Jefford M, Tattersall MH. Informing and involving cancer patients in their own care. Lancet Oncol. 2002;3(10):629–637. | ||
Haynes RB, Taylor DW, Sackett DL, Gibson ES, Bernholz CD, Mukherjee J. Can simple clinical measurements detect patient noncompliance? Hypertension. 1980;2(6):757–764. | ||
Feely M, Lindsay S, Swinn R, Williams C, Bird H, Pullar T. An evaluation of therapeutic drug (metabolite) monitoring to study compliance with allopurinol for gout. Proc BPS. 1993:112P–113P. | ||
Deschamps AE, de Geest S, Vandamme AM, Bobbaers H, Peetermans WE, van Wijngaerden E. Diagnostic value of different adherence measures using electronic monitoring and virologic failure as reference standards. AIDS Patient Care STDS. 2008;22(9):735–743. | ||
Huang WC, Chen CY, Lin SJ, Chang CS. Medication adherence to oral anticancer drugs: systematic review. Expert Rev Anticancer Ther. 2016;16(4):423–432. | ||
Partridge AH, Avorn J, Wang PS, Winer EP. Adherence to therapy with oral antineoplastic agents. J Natl Cancer Inst. 2002;94(9):652–661. | ||
Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353(5):487–497. | ||
Wu S, Chee D, Ugalde A, Butow P, Seymour J, Schofield P. Lack of congruence between patients’ and health professionals’ perspectives of adherence to imatinib therapy in treatment of chronic myeloid leukemia: A qualitative study. Palliat Support Care. 2015;13(2):255–263. | ||
Hardy H, Kumar V, Doros G, et al. Randomized controlled trial of a personalized cellular phone reminder system to enhance adherence to antiretroviral therapy. AIDS Patient Care STDS. 2011;25(3):153–161. | ||
Wu JY, Leung WY, Chang S, et al. Effectiveness of telephone counselling by a pharmacist in reducing mortality in patients receiving polypharmacy: randomised controlled trial. BMJ. 2006;333(7567):522. | ||
Krolop L, Ko YD, Schwindt PF, Schumacher C, Fimmers R, Jaehde U. Adherence management for patients with cancer taking capecitabine: a prospective two-arm cohort study. BMJ Open. 2013;3(7):e003139. | ||
Twigg MJ, Wright D, Kirkdale CL, Desborough JA, Thornley T. The UK Pharmacy Care Plan service: Description, recruitment and initial views on a new community pharmacy intervention. PLoS One. 2017;12(4):e0174500. | ||
Simons S, Ringsdorf S, Braun M, et al. Enhancing adherence to capecitabine chemotherapy by means of multidisciplinary pharmaceutical care. Support Care Cancer. 2011;19(7):1009–1018. | ||
Spoelstra SL, Sikorskii A, Given CW, et al. Adult Cancer Patient Recruitment and Enrollment into Cell Phone Text Message Trials. Telemed J E Health. 2016;22(10):836–842. | ||
Spoelstra SL, Sikorskii A, Majumder A, Burhenn PS, Schueller M, Given B. Oral Anticancer Agents: An Intervention to Promote Medication Adherence and Symptom Management. Clin J Oncol Nurs. 2017;21(2):157–160. |
Supplementary materials
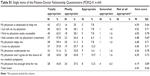  | Table S1 Single items of the Patient–Doctor Relationship Questionnaire (PDRQ-9, n=64) |
  | Figure S1 Participant satisfaction with Patient–Doctor relationship (PDRQ-9, n=64). |
  | Figure S2 Participant reported necessities of capecitabine therapy (Beliefs about Medicines Questionnaire – Nnecessity Sscale, n=64). |
  | Figure S3 Participant reported concerns of capecitabine therapy (Beliefs about Medicines Questionnaire – Concerns Scale, n=64). |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.