Back to Journals » Patient Preference and Adherence » Volume 16
Patient and Health Care Provider Perspectives on Potential Preventability of Hospital Admission for Acute Exacerbation of Chronic Obstructive Pulmonary Disease: A Qualitative Study
Authors Leenders A, Sportel E, Poppink E, van Beurden W , van der Valk P, Brusse-Keizer M
Received 3 August 2022
Accepted for publication 21 October 2022
Published 9 December 2022 Volume 2022:16 Pages 3207—3220
DOI https://doi.org/10.2147/PPA.S380862
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Anna Leenders,1 Esther Sportel,1 Elise Poppink,1 Wendy van Beurden,2 Paul van der Valk,2 Marjolein Brusse-Keizer3,4
1Department of Clinical Pharmacy, Medisch Spectrum Twente, Enschede, the Netherlands; 2Department of Pulmonary Medicine, Medisch Spectrum Twente, Enschede, the Netherlands; 3Health Technology and Services Research, Faculty of Behavioural, Management and Social Sciences, Technical Medical Centre, University of Twente, Enschede, the Netherlands; 4Medical School Twente, Medisch Spectrum Twente, Enschede, the Netherlands
Correspondence: Marjolein Brusse-Keizer, Medisch Spectrum Twente, PO Box 50000, Enschede, 7500 KA, the Netherlands, Tel +31 53 487 20 00, Email [email protected]
Purpose: Chronic obstructive pulmonary disease (COPD) is a highly prevalent chronic disease partly characterised by the occurrence of acute exacerbations (AECOPD). The need for hospital admissions for COPD exacerbations could theoretically be decreased through timely and appropriate outpatient care or self-management. The aim of this study is to explore and compare patients’ and health care providers’ (HCP) perspectives on the potential preventability of COPD hospitalisations and to identify strategies to prevent unnecessary hospitalisations.
Patients and Methods: Semi-structured interviews were conducted with patients admitted for an AECOPD (N = 11), HCPs on the respiratory ward (N = 11), and treating pulmonologists (N = 10). Interviews were transcribed verbatim and analysed using thematic content analysis.
Results: Patient and HCP perspectives on the potential preventability of hospital admissions for AECOPD often conflict. The kappa coefficients were − 0.18 [95% CI: − 0.46– 0.11] for patients and pulmonologists and − 0.28 [95% CI: − 0.80– 0.21] for patients and HCPs, which indicates poor agreement. The kappa coefficient for pulmonologists and HCPs was 0.14 [95% CI: − 0.13– 0.41], which indicates slight agreement. Patient and HCP factors that could potentially prevent hospitalisation for AECOPD were identified, including timely calling for help, recognizing and acting on symptoms, and receiving instruction about COPD, including treatment and action plans.
Conclusion: Patients and their HCPs have different beliefs about the potential preventability of AECOPD hospitalisations. Most patients and HCPs mentioned factors that potentially could have led to a different outcome for the current AECOPD or that could impact the patient’s health status and treatment of AECOPDs in the future. The factors identified in this study indicate that shared decision making is crucial to center the patient’s perspective and individual needs and to provide timely treatment or prevention of AECOPD, thereby potentially decreasing hospital admission rates.
Keywords: patient and provider preferences, hospitalisation, COPD exacerbation, prevention
Introduction
Chronic obstructive pulmonary disease (COPD) is one of the top three causes of death worldwide. Treatment of COPD aims to relieve patient symptoms, improve quality of life, and decrease the number of exacerbations.1 On average, COPD patients experience 1–3 episodes of exacerbation per year;2 of these episodes, 10% result in hospital admission.3 Hospital admissions for COPD have a significant impact on patient mortality and quality of life and generate more than 70% of patients’ direct healthcare costs.4,5 Screening for factors associated with severe exacerbation to understand the variables related to hospital admission for exacerbation is crucial to decrease hospital admission rates.6 The global COPD burden is expected to increase in coming decades due to continued exposure to risk factors and population aging1 thus, the creation and updating of treatment strategies is an important area for investigation.
Despite recent efforts to reduce hospital admission rates for COPD, the total number of COPD hospitalisations has not decreased.7 Self-management is an important intervention that can reduce the impact of exacerbation on patients and thus decrease hospitalisations.8 The aim of self-management interventions is to motivate, engage, and coach patients to positively adapt their health behaviours and develop skills to better manage their COPD on a day-to-day basis. An example of a self-management intervention is an individualised action plan for COPD patients.9 To increase the likelihood that these interventions will successfully prevent admissions for acute exacerbations of COPD (AECOPD) and to improve patient adherence to action plans, health care providers (HCPs) must understand patients’ perspectives on self-management and related needs.10 This information could support the creation of individualized approaches to help patients manage their COPD. Consensus between COPD patients and providers regarding the potential preventability of hospital admissions is likely necessary to improve self-management of COPD. The successful implementation of interventions such as action plans will be hindered if the pulmonologist believes that hospital admission could be prevented but their patient does not. Conversely, it is difficult for the pulmonologist to address their patient’s needs if a patient or HCP believes that the hospital admission is the result of a failed care system or medical advice and the pulmonologist is unaware of these beliefs. A recent Dutch pilot of a transmural care pathway found that concerted action between patients and healthcare professionals resulted in a significant reduction in the number of hospitalisation days.11
Predictors of hospital (re)admission for AECOPD have been identified, yet little is known about patients’ perspectives on the potential preventability of hospital admissions for AECOPD. This study aims to explore and compare patients’, respiratory ward doctors’ and pulmonologists’ perspectives on the potential preventability of hospital admissions for AECOPD. We examine the needs of each group with special attention to self-management and their beliefs about patient and caregiver roles in hospital admission. To the best of our knowledge, this is the first study to focus on patients’ perspectives on the potential preventability of hospital admissions for AECOPD using in-depth interviews. The study findings will provide important insight regarding patient’s beliefs.
Materials and Methods
Design and Participant Recruitment
In this study, a qualitative approach was used. Patients and their HCPs were recruited from the population of patients diagnosed with COPD who were admitted to the hospital Medisch Spectrum Twente for an AECOPD between December 2020 and March 2021. Medisch Spectrum Twente is a large single-site community hospital in the Netherlands. A gatekeeper approach was used for participant selection. Pulmonologists and nurse practitioners were asked to identify patients who fulfilled the following eligibility criteria: (1) diagnosed with COPD according to the GOLD 2019 criteria,9 (2) 40 years or older, (3) smoker or ex-smoker, (4) admitted to Medisch Spectrum Twente for an AECOPD, and (5) willing to provide written consent to participate in the study. Participants were excluded if they were unable to speak or understand the Dutch language or if they were treated in a palliative care setting.
All patients provided written informed consent, including consent for publication of anonymized responses. After each participant provided informed consent, one of the researchers scheduled an interview during the hospital admission. Most interviews occurred on the day the participant provided informed consent or the following day. Face-to-face semi-structured interviews were conducted by a single researcher in the patient’s single-bed hospital room using a predetermined interview protocol. Recruitment of patients continued until data saturation (no new topics emerged from the interviews during the final phase of analysis12) was reached for the patients and HCPs. The interview with each patient’s HCP occurred shortly after the patient interview. Each patient’s treating pulmonologist in outpatient setting (hereafter noted as pulmonologist) was interviewed, as was the responsible HCP on the respiratory ward during the patient’s hospital admission for AECOPD (hereafter noted as HCP “ward”). The hospital’s review board judged the study as not being subject to the Dutch Medical Research Involving Human Subjects Act (WMO) (K20-22). The study was conducted according to the principles of the Declaration of Helsinki. The two interviewing researchers (AL and EP) were pharmacists and had no prior relationship with the included patients.
Data Collection
Patients and their HCPs were interviewed by the responsible researcher and a research assistant using a semi-structured interview protocol with open-ended questions. This protocol was validated through face validity with a pulmonologist and nurse practitioner who were not otherwise involved in the study. A pilot interview was performed with a COPD patient who met the inclusion criteria but was not otherwise involved in the study. Minor changes were discussed and implemented before the interview protocol was finalized. The interview protocol was based on the topics presented in Table 1.
 |
Table 1 Interview Topics Protocol |
The interviews with COPD patients began with basic sociodemographic questions regarding the patient’s age, highest level of education, working status, living situation, and mobility. Prior to the interview, patients completed the Beliefs about Medicines Questionnaire (BMQ) General (BMQ-Harm, BMQ-Overuse) and the BMQ Specific (BMQ-Necessity, BMQ-Concern).13–15 The BMQ General measures beliefs about the possible negative effects (harm) of medication (4 items) and prescribing medication (possible overuse) in general by doctors (4 items) also on a Likert scale with scores 1–5. A low score on the harm means high confidence in the positive outcomes of the use of medication in general. A low score on possible overuse represents high confidence in responsible prescribing of medication by doctors. High scores mean the opposite. The BMQ Specific measures beliefs about the necessity of the prescribed medication (5 items) and concerns about negative side effects and consequences of prescribed medication (5 items) on a Likert scale with scores 1–5. A low score on necessity means low confidence in the necessity of prescribed medication. A low score on concerns means high trust in positive effects of prescribed medication. High scores mean the opposite.
All interviews were anonymously audio recorded using a digital voice recorder (Philips DVT1150) and transcribed verbatim in Dutch using F4transkript (v7.06).
Additional demographic data were collected by one of the researchers (EP) by consulting the patient’s medical record (ie, GOLD classification, number of pack years, presence of comorbidities, number of hospital admissions in the past year, latest lung function). A complete medication overview for each patient was extracted from the medication-prescribing system in the hospital, for which a list of all medications used at home is verified as a part of standard care. The care tool “Landelijk Schakelpunt” (LSP) was assessed to check pharmacy refill records to identify the number of oral corticosteroid prescriptions for each patient. This measure was used to determine the number of exacerbations the patient had experienced in the year prior to hospital admission.
Data Analysis
A thematic content analysis was performed with an inductive approach using Atlas (v9.0.20). The transcripts were read in detail, and the first five interviews were separately coded by AL, EP, and MB. The three researchers compared codes from the first five interviews for patients, HCPs “ward” and pulmonologists and discussed them until consensus was reached. The remaining interviews were coded and discussed by AL and EP until consensus was reached. The identified topics were clustered by theme and reviewed and discussed by AL, EP, and MB.
Descriptive data analysis was used to compare the patients’ and HCPs’ perspectives on the potential preventability of the hospital admission for AECOPD. Data were presented as means with standard deviation (SD) or as median with interquartile range (IQR), depending upon the distribution for continuous variables, or as numbers with percentages (%) for categorical data. A kappa coefficient including the 95% confidence interval was used to measure the level of agreement between patients’ and HCP perspectives on potential preventability.16
Results
Demographic Data
Between November 2020 and March 2021, a total of 11 patients were included in the study. Figure 1 shows the participant selection for patients and their HCPs “ward” and pulmonologists. The study population of interviewed patients was diverse. Six male and five female patients (mean age: 71.6 years, SD: 8.8 years) participated. At the time of the interview, four patients were smokers and forced expiratory volume in 1 second (FEV1) ranged from 22% to 71% of predicted value, representing GOLD guidelines stage II–IV where I is a mild disease and IV is most severe.1 The number of hospital admissions in the year prior to the interview ranged from 0–6. Ten participants were identified as patients with polypharmacy (ie, regularly used at least 5 medications).17 An overview of patient characteristics is presented in Table 2.
 |
Table 2 Patient Characteristics |
 |
Figure 1 Participant selection. |
A total of 11 HCPs wards participated (N = 5 pulmonologists, N = 6 other HCPs “ward”). The other HCPs“ward” included one nurse in training who specialised in pulmonology, one physician assistant, three registrars (pulmonologists in training), and one registrar cardiologist in training. One of the patients was primarily treated by their general practitioner; thus, no pulmonologist interview was conducted for that patient, resulting in a total of 10 pulmonologist interviews.
The duration of interviews ranged from 41–71 minutes (median = 50) for patients and from 5–25 minutes (median = 9) for HCPs.
Patient participants were asked to fill out the BMQ General and BMQ Specific. Some patients (N = 5) requested assistance to complete the BMQ. The BMQ results are presented in Table 3.15 Most patients (73%) scored lower than the midpoint of 12 on harm, which indicates that they had high confidence in the positive effect of medication use. Half of patients (54%) scored higher than the midpoint of 12 on overuse, which indicates that they were not confident in the responsible use of medication by doctors. Almost all patients (91%) scored higher than the midpoint of 15 on necessity, which means that they have confidence in the necessity of prescribed medications. Most patient scores on concern were lower than the midpoint of 18 (73%), which indicates that they had confidence in the positive effect of prescribed medications. For 63% of the patients the benefits of medication (>15 necessity) outweighed the disadvantages of medication (<18 concern).
 |
Table 3 Beliefs About Medicine Questionnaire (BMQ) Scores |
Potential Preventability Perspectives
Perspectives on the potential preventability of AECOPD hospitalisations differed between patients and HCPs. The findings presented in Table 4 indicate that 73% of patients and 90% of pulmonologists did not think that the AECOPD hospital admission could have been avoided. In contrast, most HCPs “ward” (64%) thought that the current hospitalization could have been avoided.
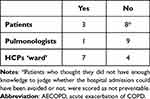 |
Table 4 Answer to Whether Te AECOPD Hospital Admission Was Preventable |
The perspectives of patients, pulmonologists and HCPs “ward” on the potential preventability of hospitalisation were compared. Table 5 presents the results of this comparison and the level of agreement between the perspectives of these groups. There was disagreement between the patient and pulmonologist in four cases as to whether the hospital admission could have been prevented. The kappa coefficient is −0.18, which indicates poor agreement between patients and pulmonologists.16 In most cases (N = 8) there was disagreement between patient and the HCP “ward” regarding the potential preventability of the hospital admission, and the kappa coefficient of −0.28 indicates poor agreement. Pulmonologists and HCPs “ward” had an equal number of disagreements (N = 5) and agreements (N = 5) regarding the potential preventability of the hospital admission. The kappa coefficient is 0.14, indicating slight agreement between pulmonologists and HCPs “ward”.
 |
Table 5 Agreement of Perspectives About Potential Preventability of the Patient’s Hospital Admission for AECOPD |
Patient Perspective – Not Preventable
Some patients mentioned that they did not have the necessary knowledge to make a judgment on potential preventability (Q1) or that they had never thought about preventability because they assumed that the hospitalisation could not be prevented (Q2). Others mentioned that their hospital admission could not have been prevented due to the acuteness of the deterioration of their symptoms (Q3).
Q1 – P9 patient: “I do not know the answer. I could not give an honest answer to that”.
Q2 – P3 patient: “You do not think about that beforehand, that it can be prevented or something. I do not assume that it could be”.
Q3 – P1 patient: “No, you cannot tell (it is going to happen). In the morning, there was nothing wrong. Nothing at all”.
HCP Perspective – Not Preventable
Almost all pulmonologists described the patient’s hospital admission as unpreventable, unlike the HCPs “ward”, most of whom most considered the admission potentially preventable (see Table 4). Some pulmonologists mentioned that they were often unaware that their patients were being admitted in the moment, so they judged the potential preventability of the hospital admission based on information in the patient’s electronic health record. Some pulmonologists mentioned that their patient was admitted before the control visit had occurred; thus, optimisation of the patient’s COPD management had not yet occurred (Q5).
Q5 – P2 pulmonologist: “And then I gave her some different medications and made an appointment for a control visit. […] That appointment should have been in February, but in the meantime, she was apparently readmitted for an AECOPD recently”.
Patient visibility was another theme that emerged during interviews. HCPs “ward” and pulmonologists recognized that some patients did not have adequate outpatient follow up (Q6 and Q7). One pulmonologist mentioned that if the patient cancelled an appointment, their treating pulmonologist would be unaware of it (Q8).
Q6 – P10 HCP “ward”: “I see he disappeared from control visits at some point. August 2020 was the last time he was here. The pulmonologist then did not follow up on this patient until this hospital admission where the patient presents himself here again. […] I think this patient got out of sight”.
Q7 – P5 pulmonologist: “As I just mentioned, I have known her for way too short a time. We do not have an idea why her condition is now worse, just like that”.
Q8 – P4 pulmonologist: “A new appointment is scheduled with me, and then the patient cancels. That all happens behind our backs; we cannot see that”.
One pulmonologist and HCP “ward” mentioned a patient’s lack of motivation as an important factor in hospital admission preventability (Q9 and Q10). They explained that the patient was not following treatment advice, such as smoking cessation or other lifestyle interventions.
Q9 – P10 HCP “ward”: “His biggest problem is that he will not quit smoking and probably still drinks (alcohol) a lot. And on top of that, he is not following the rules, lifestyle rules, and advice. That is. Well. These kinds of people, you can explain as much as you want, but they will not act upon it”.
Q10 – P10 pulmonologist: “It just proves that, in my opinion, he just does whatever he wants, and he is not motivated to live as long as possible or anything.”
Potential Preventability
The next paragraphs show the patient and HCP factors that could potentially prevent hospitalisation for AECOPD that were identified in our study. Things that the patient could have done different to potentially prevent hospitalisation or specific patients’ beliefs were considered a “patient factor”, and things that an HCP could have done different or specific HCP beliefs were considered a “HCP factor”.
Patient Factors
Calling for Help
Most patients discussed their symptoms or exacerbation with a family member or direct caregiver only when their complaints became severe. Calling for help sooner was an important factor that could affect preventability of hospital admission mentioned by patients (N = 3) and HCPs (N = 10). Some patients mentioned they would prefer calling the pulmonologist or nurse specialist directly instead of their general practitioner (GP), whereas doing so was already part of standard care for others. Some patients mentioned that the situation may have turned out differently if they had called their GP or pulmonologist sooner (Q11 and Q12).
Q11 – P8 patient: (Interviewer: “Is there something you could have done differently to prevent you from being admitted?”) “Contact the doctor sooner”.
Q12 – P6 patient: “I waited too long. Every time, I thought it would go away. But in hindsight, it just got worse and worse”. […] (Interviewer: “Do you think the hospital admission for your AECOPD could have been prevented?”) “Yes, maybe I should have gone to the doctor sooner, it could be. To the GP. Maybe sooner”.
Some HCPs explained that they depended on patients to initiate contact, because they cannot act if they are unaware of patients’ deterioration (Q13). Remarkably, this factor was mentioned by HCPs for almost all patients, but only three patients mentioned it themselves. Notably, the patients who mentioned calling for help sooner as a factor were not necessarily associated with the HCPs who reported this factor.
Q13 – P10 HCP “ward”: “Calling help sooner because the patient has been increasingly short of breath for a week. The patient could have called the GP earlier”.
Recognition of Symptoms
Almost all patient participants had poor or little understanding of COPD and the corresponding treatment. Most were unable to explain what COPD is, nor could they mention which medications they were using. Some patients mentioned difficulty with recognizing early symptoms of a COPD exacerbation due to comorbidity with similar complaints (Q14). Thus, they were unable to respond to or act upon their deterioration.
Q14 – P3 patient: “So it is just. Well, I am just a layman, so where it [the symptoms] comes from, you just do not know […] but I never thought about my lungs, I just thought it was my blood sugar”.
Some patients did experience symptoms of an exacerbation but did not think the symptoms would lead to an exacerbation. Rather, they predicted that the symptoms would go away without an intervention (Q15). These and other patients were experiencing symptoms, then had a “sudden” drop in well-being and were surprised by the deterioration (Q16 and Q17).
Q15 – P4 patient: (Interviewer: “Did you think you might end up with a hospital admission?”) “No. No, because I am actually very hard on myself in that regard.” (Interviewer: “Did you recognize your deterioration?”) “Yes, but every time, I just told myself that it would go away. But here we are”.
Q16 – P7 patient: (Interviewer: “Could you tell your symptoms could lead to an exacerbation?”) “Yes, I could actually, it was just going to happen. […] You can just feel your body being rushed, so you want to go to the bathroom quickly but you just cannot go quickly. And if your actions are carried out too fast, you will be out of breath. So, then you are gasping for breath and starting to panic. All those sort of small things. And then in a sudden moment, well yes, BOOM. Then it [the exacerbation] is there”.
Q17 – P10 patient: (Interviewer: “Did you see your exacerbation coming?”) “No, not exactly. Just like I told you, there are no signposts, like. It does not say that when you are at signpost 7, you are there [having an exacerbation]. It just comes. If you do indeed have an exacerbation, it comes really unexpectedly”.
While most patients did not foresee the exacerbation or hospital admission, although almost all patients mentioned specific symptoms other than day-to-day symptoms of COPD in the period before hospital admission (eg, up to two weeks prior). Patients experienced a wide range of symptoms prior to hospitalisation, including feeling short of breath, feeling rushed, being anxious, being able to walk shorter distances, having a reduced appetite, having a reduced physical condition, and being unable to walk.
Several HCPs mentioned that patients learning to recognise their symptoms was an important factor that could potentially prevent hospital admissions (Q18). Patient comorbidities or lack of experience with exacerbation were mentioned by HCPs as possible explanations for the lack of symptom recognition (Q19).
Q18 – P3 HCP “ward”: “The patient did not recognise it [symptoms of an exacerbation], and so it resulted in a hospital admission. The first step must be that they recognise it themselves; otherwise, an HCP cannot do anything”.
Q19 – P8 HCP “ward”: “It is difficult when you experience your first COPD exacerbation, to recognise it”.
Acting on Symptoms
Acting on symptoms is another factor mentioned by patients (N = 2) and HCPs (N = 5) that could potentially prevent hospital admission for AECOPD (Q20 and Q21). Acting on symptoms could include taking medication, such as extra inhalation medication, earlier when experiencing symptoms. It could also include establishing and using an action plan to self-treat exacerbations with prednisone and/or antibiotics.
Q20 – P5 patient: “I do think that in the future, when I feel a cough or cold, I would increase the number of puffs of inhalation medication sooner. That I would become more alert”.
Q21 – P4 pulmonologist: “The patient could have started the prednisone treatment earlier by himself, the emergency prednisone treatment that the patient had available at home”.
Patients were often unaware of the additional treatment options with their inhalation medication if they experienced an increase in symptoms, or they did not know how to react properly to such a situation (Q22 and Q23).
Q22 – P10 patient: (Interviewer: “When you were experiencing more symptoms, what did you do then?”) “Nothing. I just hoped it would go away. Just sit down first. They were not new symptoms; it was not something I did not know or anything”.
Q23 – P5 patient: (Interviewer: “But did you take inhalations one after the other then?”) “Yes, a lot in a row.”
Additionally, not all patients had access to self-treatment with prednisone and/or antibiotics. Only one patient mentioned having an action plan. However, the patient did not feel comfortable using the action plan and was unable to explain its use, and the HCP “ward” could not confirm that the patient actually had an action plan (Q24). Most patients had never heard of an action plan (N = 10) and were unable to explain what it was, though the patient’s HCP believed they had an action plan in at least six cases.
Q24 – P6 HCP “ward”: “I cannot find it anywhere […] I do not have a clue, of all the files that have been uploaded [to the electronic health record] in the past years, it is not there”.
In several cases (N = 4), there was disagreement between HCPs “ward” and pulmonologists regarding whether the patient had an action plan (Q25 and Q26). There was no specified place in the patient’s health record to indicate whether a patient had an action plan. There were also no regular assessments of the suitability and use of the action plan.
Q25 – P4 HCP “ward”: (Interviewer: “Does the patient have an action plan?”) “No. So there is room for improvement.” (Interviewer: “Why does the patient not have an action plan?”) “Hmm. I am not sure why she does not have one, but I have to check if there is a reason. I have not been able to discuss that with her, but that is something we are going to start with”.
Q26 – P4 pulmonologist: “I can see here [in the electronic health record], action plan or something like that was scanned to her file. So that was explained to her in May 2019”.
Smoking Cessation
Smoking cessation was only relevant for the four patients who smoked, but only one patient mentioned smoking cessation as a potential factor to prevent hospitalisation (Q27). Conversely, HCPs mentioned smoking cessation as an important patient-driven factor to potentially prevent hospitalisations for all smoking patients (Q28).
Q27 – P4 patient: “Definitely not smoking.”
Q28 – P10 HCP “ward”: “Mainly that the patient should just not smoke anymore”.
Concern About Home Situation
Some patients explained that having an exacerbation and being admitted to the hospital strongly impacted their family members (Q29 and Q30). Patients’ concerns regarding their home situation may influence their motivation to prevent future exacerbations or hospital admissions.
Q29 – P2 patient: (Interviewer: “How did you respond to the decision to have you admitted?”) “Well, I did not like it. Normally I have to care for my wife, and I know that she is in good hands, but still. You have to leave your wife alone while she is sick. I do not like that. But still, there was no other option”.
Q30 – P5 patient: “I really hope we can find a way [to prevent AECOPD]. That people just especially for the people at home. Because the patient that is having the exacerbation. Well, that can of course also be different, but I am not someone who is easily panicked. It is a very bad experience for the other people at home. And for them, I hope to never experience an exacerbation again”.
HCP Factors
The majority of patients (N = 6) and HCPs (N = 17) did not think that one of the caregivers involved in the patient’s treatment (ie, physiotherapist, community pharmacist, pulmonologist, GP, nurse specialist) could have done anything to prevent the patient from being admitted to the hospital. Some HCPs mentioned being unable to act upon the deterioration of their patients because they were unaware of the situation (Q31).
Q31 – P4 pulmonologist: “If I do not know what is going on, I cannot anticipate it”.
Patient Needs
Some patients expressed specific expectations of their caregivers that were in accordance with their specific needs. Examples of such expectations include more pushing to seek help from others, such as care personnel at the nursing home (Q32); adequate instructions for how to address specific symptoms and exacerbation (Q33); specific treatment changes; more personal care; and more attention to the patient’s situation.
Q32 – P2 patient: “Even more pushing for me to see a doctor. Maybe it would have been better if they had sent me to a GP in an earlier stage”.
Q33 – P5 patient: “Adequate instructions about how to use the inhalation medication and what to do when you get additional symptoms. What you can do then”.
Instruction on COPD, Treatment and Action Plans
The HCP factors mentioned by HCPs included instructing patients on action plans, COPD, and treatment. Several HCPs mentioned an action plan as a factor that could have potentially prevented the hospital admission (Q34). In most cases, starting an action plan was the next treatment step for the patient to possibly prevent AECOPD hospitalisations in the future (Q35). In one case, a patient had an action plan but needed to receive additional instruction about it due to low adherence to the action plan during the latest deterioration (Q36).
Q34 – P10 HCP “ward”: “If the patient had a clear step-by-step plan or an action plan that he could follow at home. The patient is competent enough to follow this. Then, maybe it could have been prevented”.
Q35 – P5 pulmonologist: “And now we agreed, after this admission, that the patient would receive an action plan with regard to COPD”.
Q36 – P6 HCP “ward”: “That the patient has to adhere to the action plan, so that has to be discussed again with the respiratory nurse. That will take place. He just needs to know what to do, that he can increase the number of inhalations or take more nebulisations, because he has a nebuliser. And he needs to have a prednisone prescription at home”.
Another factor mentioned by HCPs was instruction on COPD and treatment. This instruction could address patients’ lack of knowledge about COPD and their condition (Q37), as well as optimisation of treatment, medication, and inhalation techniques (Q38).
Q37 – P1 pulmonologist: “I don’t know if she fully understands. I do try to tell her every time: if you do this, then you have to do that, and if this, then you have to do that. But if it completely sticks, I dare not say that with 100% certainty. That is indeed a point of attention, to check that”.
Q38 – P4 HCP “ward”: “I do not know if physiotherapy was ever discussed with her, but at least she had never done it”.
Assessing Treatment Adherence and Inhalation Technique
Patients were unaware of the potential for suboptimal therapy adherence or inhalation technique. Most patients experienced inhaling the different medicines as easy, and some claimed that they always took the same medication with the same frequency.
Documentation of assessments of inhalation technique and treatment adherence was not easy to find for HCPs; thus, they were unable to tell when the last assessment had taken place in most cases. Some pulmonologists stated that they do not do assessments of inhalation technique or treatment adherence (Q39).
Q39 – P9 pulmonologist: “I don’t think so, we [pulmonologists] don’t do assessments [on inhalation technique or treatment adherence], and maybe the nurse specialist did it some time, but in general I don’t do assessments”.
Although assessments were not done regularly, some HCPs doubted whether their patient had used medication or the proper inhalation technique correctly (Q40). Other HCPs did not have reason to expect suboptimal therapy adherence (Q41 and Q42).
Q40 – P5 HCP “ward”: “Well, I do not think the patient uses her inhalation medication optimally. So, I think that with some optimisation, things could have gone better”.
Q41 - P6 pulmonologist: “I assume. I have no reason to doubt that [adherence]”.
Q42 - P5 pulmonologist: “I do not know. But she seemed a pretty intelligent lady to me, so I assume she is. But I do not know, I did not check it”.
One HCP explained that there was no reason to suspect suboptimal medication use because the patient had requested multiple iterations of the prescribed medication (Q43). Notably, eight patients depended on medication delivery from their community pharmacy or care facility or daily dose dispensing systems (Baxter), in which case there was no direct interaction between the patient and pharmacist. Nearly all patients needed repeat medication service; thus, pharmacists would not be expected to check therapy adherence.
Q43 - P7 pulmonologist: “We did not check the therapy adherence if that is what you are asking. But we do know that a pretty big part of our COPD population is not always adherent. Definitely not regarding the inhalation medication. [….] knowing the fact that there are requests for iterations, it means he is using his medication at least. But whether he takes them every single day or sometimes forgets, I do not know that”.
Discussion
This study explored and compared the perspectives of patients, respiratory ward doctors, and pulmonologists on the potential preventability of hospital admission for AECOPD. Perspectives between patients and their pulmonologists and HCPs “ward” differed substantially. Most patients and pulmonologists considered the hospital admission unpreventable, whereas most HCPs “ward” believed that the hospital admission could have been avoided. Despite the fact that not all participants and pulmonologists believed in potential preventability of hospital admission, most did mention specific causes for hospital admission or factors for optimisation. Patient and HCP factors that were reported that could potentially prevent hospitalisation included recognizing and acting on symptoms, timely calling for help and receiving instruction about COPD, including treatment and action plans.
In most cases, pulmonologists and HCPs “ward” did not agree on the potential preventability of hospital admission for AECOPD. HCPs “ward” often suggested treatment interventions that may have prevented the deterioration of COPD or the exacerbation itself, whereas pulmonologists tended to place responsibility for hospitalisation on the severity of COPD or patients’ behaviour rather than a lack of successful self-management interventions.7 A possible cause for this phenomenon is the treating pulmonologists’ insensitivity to patient signals because they often have a long-term treatment relationship with their patients. HCPs “ward” have a more naïve view of these patients which could be partly due to the lack of designated space for documentation regarding action plans and other self-management interventions (eg physiotherapy or smoking cessation) in the patients’ electronic health records. As nine pulmonologists judged the hospital admission as unpreventable, we can also imagine that they lacked information related to the AECOPD that HCPs “ward” did have. For example, discussing the causes for hospital admission with their patient to look for optimisation factors was not offered to pulmonologists in our study, but HCPs “ward” did have this opportunity during admission as it is part of standard care. However, it is also possible that patients provided different information to HCPs “ward” at the time of hospital admission (the acute phase) than to pulmonologists at an outpatient appointment that generally occurs some time after the hospital admission (the non-acute phase). Patients may also experience a different connection with their HCP “ward” than their pulmonologist due to long exposure to this provider during hospitalisation.
COPD patients who face difficulty in recognising the onset of an exacerbation may delay their decision as to whether to contact an HCP.18 The present study findings support this claim in that almost all patients described their exacerbation or hospital admission as unpreventable and unforeseen, whereas when asked about their feelings, symptoms, and behaviour in the 1–2 weeks prior to admission, patients were able to identify that their symptoms had worsened. Symptoms varied between patients, but for most patients, their symptoms were recognisable and consistent with those of other exacerbations in hindsight. These individual patient observations, often described somewhat vaguely, should be discussed with the pulmonologist to implement a more individualised approach or strategy for treatment19 and to identify when patients should call for help in the future or follow their self-management action plan. Comorbidities can hinder recognition of AECOPD; thus, instruction on when a patient should call for help or increase therapy must be individualised for the patient’s ability to recognise situations and symptoms.
Despite current guidelines and decades of evidence on the benefits of a self-management approach, self-management of COPD remains relatively underutilized.20 Action plans are a key self-management intervention,9 and it is remarkable that only one patient was able to define an action plan, and none of the patients reported having an action plan in place, despite 6 HCPs reporting that they had discussed an action plan with the patient in the past. This finding is in line with other study findings that adherence to action plans is generally low.21,22 Inadequate health literacy is generally recognised as a factor that can influence adherence to exacerbation action plans.10 The patient sample in this study had relatively low educational attainment, and some participants may have been illiterate based on their need for help in filling out the study questionnaires. These patient factors may have contributed to the discrepancy regarding action plans. It is likely that HCPs were unaware of their patients’ health literacy status because measuring health literacy skills is often not part of standard care and no documentation of health literacy existed in the patients’ electronic health records. This finding indicates that clear and ongoing instruction and training on action plans is necessary and that the action plans can be improved by considering patients’ ideas, concerns, (health) literacy23 and preferences, as well as involving patients in decision making (shared decision making).
Adherence to inhaled COPD treatment is associated with fewer hospital admissions in patients with moderate-to-severe COPD.24 Previous studies have shown that adherence to inhaled therapy in COPD patients is generally poor.25–29 It is also reported that 19.8% to 59% of COPD patients make one or more critical errors regarding inhalation technique.30 In our study, therapy adherence and inhalation technique were not regularly assessed, which may have resulted in suboptimal medication use. All patients described taking inhalation medication as an easy and minor task, yet most mentioned that they occasionally forgot to take their medication. The measured BMQ scores indicate that patients are aware of the necessity of the medication they use and are willing to be adherent to their prescribed medication. Community pharmacists can play a vital role in optimising inhalation technique and therapy adherence.31 As van der Molen et al propose in their literature review, pharmacists can assist patients with disease management by providing advice and education regarding dosage, inhaler technique, treatment expectations, and the importance of adherence, as well as by supporting self-management.32 Pharmacists and pulmonologists must share awareness and consult with one another about these elements. In the present study, one pulmonologist assumed that their patient was adherent to medication therapy because iterated requests for the medication were sent by the pharmacy. However, this patient was dependent on delivery services and repeat medication services provided by the pharmacy. Rather than signalling patient adherence, the iterated request was an automatically generated signal by the pharmacy. Such miscommunications and assumptions could be addressed by optimising pulmonologist-pharmacist collaboration. This requires adequate peer communication and an adequate transmural care pathway because COPD treatment is provided by several caregivers.
We recommend that the question whether the hospitalisation could have been prevented should be discussed more frequent in regular care between HCPs and patients. As patients’ preferences and beliefs may change due to important life events or progression of the disease, using a holistic approach when discussing potential preventability can identify the individual experienced barriers by patients (for example concerns about their home situation) to which pulmonologists and HCPs “ward” can respond.
Based on the study findings, we also recommend increased continuity between admission and outpatient control visits to discuss self-management behaviour and patient needs and support patients in acting upon their symptoms. For example, better peer communication and documentation in EHR can be organised through consultation with the nurse specialist or pulmonologist during hospital admission. Patients who experienced deterioration before the outpatient control visits could particularly benefit from timely and appropriate interventions during or shortly after hospitalisation. The study findings indicate that treatment for these patients was not optimised, because the patients were readmitted for AECOPD prior to the outpatient control visit appointment.
To our knowledge, this is the first study to compare perspectives of patients and HCPs. A strength of the study is the use of in-depth interviews, which provide insight regarding patient and HCP perspectives and beliefs and indicate potential opportunities for improvements in care. These qualitative findings support and complement the quantitative work that has been published on this topic by providing insight into current practice. An inductive approach was used to enable the development of new theories that can be explored in future (quantitative) studies. The use of a pilot interview and performance of face validity are additional strengths of the study. This study has limitations. This study was not designed or powered to show the level of agreement in the perspectives of potential preventability, as shown by the large confidence intervals of the kappa’s. It does however show us that patients and their pulmonologists and HCPs on the ward have different ideas about preventability. The research was conducted during the COVID-19 pandemic, which may have created an inclusion bias in that this population could have had more severe COPD than the general population, because others with more mild cases may have chosen to delay seeking care due to the pandemic. In addition, patients who were unable to speak Dutch were excluded from the study. The generalisability of the findings is therefore questionable. Nearly all patients were willing to participate in this study, which resulted in a sample population that was representative of the patients being admitted for AECOPD at the time of the study.
Conclusion
Patient and HCP perspectives on the potential preventability of hospital admission for AECOPD do not match. Hospital admission due to AECOPD provides a good opportunity to discuss and evaluate a patient’s self-management, preferably in consultation with the treating pulmonologist. Patient preferences and beliefs may change due to important life events or progression of the disease. A holistic approach will support the implementation and update of successful self-management interventions through shared decision making. Patient needs identified in this study include adequate and ongoing education on the disease and its treatment tailored to the patient’s health literacy. Pharmacists can play an key role in monitoring adherence and should be considered part of integrated care for COPD patients.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Vogelmeier CF, Criner GJ, Martinez FJ, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2017 report. GOLD executive summary. Am J Respir Crit Care Med. 2017;195(5):557–582. doi:10.1164/rccm.201701-0218PP
2. Dhamane AD, Moretz C, Zhou Y, et al. COPD exacerbation frequency and its association with health care resource utilization and costs. Int J Chron Obstruct Pulmon Dis. 2015;10:2609–2618. doi:10.2147/COPD.S90148
3. Soler-Cataluna JJ. Severe acute exacerbations and mortality in patients with chronic obstructive pulmonary disease. Thorax. 2005;60(11):925–931. doi:10.1136/thx.2005.040527
4. Mannino DM, Braman S. The epidemiology and economics of chronic obstructive pulmonary disease. Proc Am Thorac Soc. 2007;4(7):502–506. doi:10.1513/pats.200701-001FM
5. Soler-Cataluña JJ, Martínez-García MÁ, Serra PC. Multidimensional impact of COPD exacerbations. Arch Bronconeumol. 2010;46(Suppl 11):12–19. doi:10.1016/S0300-2896(10)70057-0
6. Vestbo J, Hurd SS, Agustí AG, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2013;187(4):347–365. doi:10.1164/rccm.201204-0596PP
7. Harries TH, Thornton H, Crichton S, Schofield P, Gilkes A, White PT. Hospital readmissions for COPD: a retrospective longitudinal study. NPJ Prim Care Respir Med. 2017;27(1):31. doi:10.1038/s41533-017-0028-8
8. Korpershoek YJG, Vervoort SCJM, Trappenburg JCA, Schuurmans MJ. Perceptions of patients with chronic obstructive pulmonary disease and their health care providers towards using mHealth for self-management of exacerbations: a qualitative study. BMC Health Serv Res. 2018;18(1):1. doi:10.1186/s12913-018-3545-4
9. Global Initiative for Chronic Obstructive Lung Disease - GOLD. GOLD 2022 global strategy for the diagnosis, management, and prevention of COPD; 2021. Available from: https://goldcopd.org/2022-gold-reports-2/.
10. Schrijver J, Effing TW, Brusse-Keizer M, van der Palen J, van der Valk P, Lenferink A. Predictors of patient adherence to COPD self-management exacerbation action plans. Patient Educ Couns. 2021;104(1):163–170. doi:10.1016/j.pec.2020.06.015
11. Westbroek LF, Klijnsma M, Salomé P, et al. Reducing the number of hospitalization days for COPD: setting up a transmural-care pathway. Int J Chron Obstruct Pulmon Dis. 2020;15:2367–2377. doi:10.2147/COPD.S242914
12. Brod M, Tesler LE, Christensen TL. Qualitative research and content validity: developing best practices based on science and experience. Qual Life Res. 2009;18(9):1263–1278. doi:10.1007/s11136-009-9540-9
13. Horne R, Weinman J, Hankins M. The beliefs about medicines questionnaire: the development and evaluation of a new method for assessing the cognitive representation of medication. Psychol Health. 1999;14(1):1–24. doi:10.1080/08870449908407311
14. de Ridder D, Theunissen N. Beliefs about Medicine Questionnaire (BMQ) BMQ specific & BMQ general Dutch translation; 2003. Available from: https://meetinstrumentenzorg.nl/instrumenten/beliefs-about-medicine-questionnaire-bmq-bmq-specific-bmq-general/.
15. van Gastel M, van Engelen E. Beliefs about Medicine Questionnaire (BMQ) toelichtingsformulier; 2011. Available from: https://meetinstrumentenzorg.nl/instrumenten/beliefs-about-medicine-questionnaire-bmq-bmq-specific-bmq-general/.
16. Landis JR, Koch GG. An application of hierarchical kappa-type statistics in the assessment of majority agreement among multiple observers. Biometrics. 1977;33(2):363. doi:10.2307/2529786
17. Verduijn M, Leendertse A, Moeselaar A, de Wit N, van Marum R. Multidisciplinaire richtlijn polyfarmacie bij ouderen. Huisarts Wet. 2013;56(8):414–419. doi:10.1007/s12445-013-0215-y
18. Ure J, Pinnock H, Hanley J, et al. Piloting tele-monitoring in COPD: a mixed methods exploration of issues in design and implementation. Prim Care Respir J. 2012;21(1):57–64. doi:10.4104/pcrj.2011.00065
19. Pinnock H, Steed L, Jordan R. Supported self-management for COPD: making progress, but there are still challenges. Eur Respir J. 2016;48(1):6–9. doi:10.1183/13993003.00576-2016
20. Cravo A, Attar D, Freeman D, Holmes S, Ip L, Singh SJ. The importance of self-management in the context of personalized care in COPD. Int J Chron Obstruct Pulmon Dis. 2022;17:231–243. doi:10.2147/COPD.S343108
21. Bucknall CE, Miller G, Lloyd SM, et al. Glasgow supported self-management trial (GSuST) for patients with moderate to severe COPD: randomised controlled trial. BMJ. 2012;344(mar061):e1060–e1060. doi:10.1136/bmj.e1060
22. Bischoff EWMA, Hamd DH, Sedeno M, et al. Effects of written action plan adherence on COPD exacerbation recovery. Thorax. 2011;66(1):26–31. doi:10.1136/thx.2009.127621
23. Yadav UN, Hosseinzadeh H, Lloyd J, Harris MF. How health literacy and patient activation play their own unique role in self-management of chronic obstructive pulmonary disease (COPD)? Chron Respir Dis. 2019;16:147997311881641. doi:10.1177/1479973118816418
24. Vestbo J, Anderson JA, Calverley PMA, et al. Adherence to inhaled therapy, mortality and hospital admission in COPD. Thorax. 2009;64(11):939–943. doi:10.1136/thx.2009.113662
25. Restrepo R, Alvarez M, Wittnebel LD, et al. Medication adherence issues in patients treated for COPD. Int J Chron Obstruct Pulmon Dis. 2008;3:371–384. doi:10.2147/COPD.S3036
26. George M. Adherence in asthma and COPD: new strategies for an old problem. Respir Care. 2018;63(6):818–831. doi:10.4187/respcare.05905
27. Rand CS. Patient adherence with COPD therapy. Eur Respir Rev. 2005;14(96):97–101. doi:10.1183/09059180.05.00009604
28. Humenberger M, Horner A, Labek A, et al. Adherence to inhaled therapy and its impact on chronic obstructive pulmonary disease (COPD). BMC Pulm Med. 2018;18(1):163. doi:10.1186/s12890-018-0724-3
29. Huurne KK, Movig K, van der Valk P, et al. Differences in adherence to common inhaled medications in COPD. J Chron Obstruct Pulmon Dis. 2015;12(6):643–648. doi:10.3109/15412555.2014.995292
30. Batterink J, Dahri K, Aulakh A, Rempel C. Evaluation of the use of inhaled medications by hospital inpatients with chronic obstructive pulmonary disease. Can J Hosp Pharm. 2012;65:2. doi:10.4212/cjhp.v65i2.1118
31. van der Molen T, van Boven JFM, Maguire T, Goyal P, Altman P. Optimizing identification and management of COPD patients – reviewing the role of the community pharmacist. Br J Clin Pharmacol. 2017;83(1):192–201. doi:10.1111/bcp.13087
32. Fathima M, Bawa Z, Mitchell B, Foster J, Armour C, Saini B. COPD management in community pharmacy results in improved inhaler use, immunization rate, COPD action plan ownership, COPD knowledge, and reductions in exacerbation rates. Int J COPD. 2021;16:519–533. doi:10.2147/COPD.S288792
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
