Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 16
Partial Unilateral Lentiginosis Successfully Treated with the Combination of 511 nm and 578 nm Copper Bromide Laser in an Indonesian Woman
Authors Hindritiani R, Widjaya MRH , Puspitosari D , Rizqandaru T , Ruchiatan K
Received 1 June 2023
Accepted for publication 11 August 2023
Published 21 August 2023 Volume 2023:16 Pages 2271—2276
DOI https://doi.org/10.2147/CCID.S423917
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jeffrey Weinberg
Reti Hindritiani, Muhamad Radyn Haryadi Widjaya, Diah Puspitosari, Trustia Rizqandaru, Kartika Ruchiatan
Department of Dermatology and Venereology, Faculty of Medicine, Universitas Padjadjaran - Dr. Hasan Sadikin General Hospital, Bandung, Indonesia
Correspondence: Reti Hindritiani, Department of Dermatology and Venereology, Faculty of Medicine, Universitas Padjadjaran - Dr. Hasan Sadikin General Hospital, Jl. Pasteur No. 38, Bandung, West Java, Indonesia, 40161, Tel +62222032426 ext. 3449, Fax +62222032426, Email [email protected]
Abstract: Partial unilateral lentiginosis (PUL) is a pigmentation disorder characterized by multiple lentigines restricted to the normal skin in a unilateral and segmental pattern. Various lasers have been used for the treatment of this pigmented disorders, one of which is the copper bromide (CuBr) laser, which emits a dual-wavelength beam at 511 nm and 578 nm. A 35-year-old woman presented with multiple brown macules with a sharp demarcation from the midline of the forehead to the right cheek in a dermatomal distribution. Histopathological results showed increased melanin pigmentation in the basal layer with elongated rete ridges, supporting the diagnosis of PUL. Following photoprotection and skin priming, CuBr laser treatment was performed in two steps using 511 nm and 578 nm wavelength as the first and second steps, respectively, with the second step delivered immediately after. Clinical improvement was achieved after two sessions of treatment at a one-month interval, as shown by an increasing lightness value (L*) in spectrophotometry. No side effects, such as hyperpigmented macules, was observed. The patient also expressed satisfaction at her brighter facial skin. A sustainable favorable result persisted after six months of laser treatment. Interactions between cutaneous vasculature and melanocytes can affect the development of pigmented lesions. Melanocytes express the functional vascular endothelial growth factor receptor (VEGF) and are responsive to angiogenic factors. Ideally, these conditions should be treated with a dual-wavelength CuBr laser. The combination of 511 nm and 578 nm CuBr laser showed favorable results, supporting its potential as an effective treatment choice for PUL.
Keywords: copper bromide, dual wavelength, effective, laser, partial unilateral lentiginosis
Introduction
Lentigines are discrete, irregular, and hyperpigmented macules mainly caused by chronic ultraviolet (UV) light exposure.1 Lentigines with a segmental pattern that do not cross the body midline are referred to as partial unilateral lentiginosis (PUL). The main histopathological feature of PUL is an increase in melanin pigmentation in the epidermal basal layer,2,3 similar to lentigines.3
Patients with PUL often have a psychological burden due to aesthetically-unpleasing skin appearance.4 The treatment of PUL aims to improve the aesthetic aspect of the skin.5 One of the therapeutic options is laser therapy with melanin as its main target, including the 511 nm copper bromide (CuBr) laser, also known as a green laser. The CuBr laser also emits light with a wavelength of 578 nm, known as yellow laser, which is commonly used for vascular lesions.6,7
Laser treatment using vascular targets is becoming increasingly popular. Vascular endothelial growth factor (VEGF) receptors that respond to angiogenic factors have been found in melanocytes.6,7 Lee et al7 reported increased VEGF expression in patients with melasma who were subsequently treated with a 578 nm CuBr laser at two-week intervals. A decrease in VEGF expression was reported one month after the final laser treatment session. The 578 nm CuBr laser may have an effect on melanogenesis through VEGF on keratinocytes, dermal angiogenesis, and inflammatory mediators.7 This case report aims to report a case of improved PUL after treatment with a combination of 511 nm and 578 nm CuBr laser.
Case
A 35-year-old Indonesian woman of Sundanese ethnicity presented with brownish hyperpigmented macules at the level of the V1 and V2 nerves on the forehead and right cheek (Figure 1). Eleven years before admission, the patient worked as a tour guide and was often exposed to sunlight. The patient had Fitzpatrick-type IV skin. The lightness (L*) values of spectrophotometry were 56.16, 58.12, and 59.77 on the right forehead, upper right cheek, and lower right cheek, respectively. Histopathological examination showed increased melanin pigmentation in the basal layer of the epidermis and inflammatory cell lymphocytes in the papillary dermis fibrocollagenous connective tissue (Figure 2), which confirmed the diagnosis of PUL in the forehead and right cheek.
 |
Figure 1 (A) Hyperpigmented macules at the level of the V1 and V2 nerves on the forehead and right cheek. (B) Hyperpigmented macules on the forehead. (C) Hyperpigmented macules on the right cheek. |
 |
Figure 2 Histopathological features of a punch biopsy of the hyperpigmented macule on the right cheek showed an increase in melanin pigmentation in the basal layer of the epidermis (red circle). |
Topical treatment given included sun protection factor (SPF) 50 cream and the priming agent, a mixture of 0.01% tretinoin cream and 4% hydroquinone cream in a 1:1 ratio. The priming agent was applied to the entire face at night because the patient would undergo laser treatment in “shining bright” mode, which targeted the entire face. The patient also underwent a two-step CuBr laser treatment at different wavelengths. The first step involved the 511 nm, 30 J/cm2 fluence, and 125 ms with a 0.6 mm handpiece until a grayish lesion is observed, which serves as the endpoint. The second step continued immediately after the first step, using the 578 nm laser in “shining bright” mode at 3.2 kW peak power for 100 cm2 with a 1 mm handpiece until the skin became brighter. Informed consent related to the treatment has been obtained from the patient.
The hyperpigmented macules reduced and faded after one session of treatment (Figures 3A and B), and the spectrophotometry L* values became 57.04, 59.38, and 60.1 on the right forehead, upper right cheek, and lower right cheek, respectively (Figure 4). Significant improvement was observed after the two treatment sessions (Figure 3C). Spectrophotometry L* values were increased to 57.77, 59.56, and 61.45 on the right forehead, upper right cheek, and lower right cheek, respectively (Figure 4). The patient felt that she had brighter facial skin. We also observed that a favorable and sustainable result persisted after six months of laser treatment.
 |
Figure 3 Comparison of hyperpigmented macules on the forehead and right cheek. (A) Before treatment. (B) After one session of treatment. (C) After two sessions of treatment. |
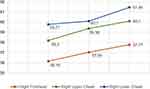 |
Figure 4 The L* values of spectrophotometry. |
Discussion
Partial unilateral lentiginosis is a skin pigmentation disorder in the form of asymptomatic lentigines7 that appear as brownish macules8 scattered on normal skin2,3 in a segmental pattern with the involvement of one or more dermatomes3,6 with well-defined midlines.2 Park et al9 reported that the onset of PUL occurs at a mean age of 14 years (range = 6–26 years) and is mainly diagnosed between 7–41 years, with a mean age of 27 years. The prevalence is similar in males and females.10 PUL can occur anywhere on the body, including the face, neck, trunk, and extremities,2 in one or more dermatomes.2,3 The patient in this case report is a 35-year-old woman complaining of brown patches on her forehead and right cheek, which first appeared at age 15.
The pathogenesis of PUL is not fully understood but is thought to be related to somatic mosaicism during embryonic development due to mutations confined to melanoblasts from the neural crest.2 Both melanocytes and nerve cells have an ectodermal origin.3 Mosaicism occurs in somatic cells, meaning that it is not inherited by subsequent generations. Several pigmentary genes in germ cells, such as SNAI2, KITLG, EDNRB, EFNB1, and EFNB2, are associated with pigmentary mosaicism, which plays a role in neural crest differentiation and melanoblast migration.2
The histopathological appearance of PUL is similar to that of lentigines,3 including increased melanin pigmentation in the basal layer of the epidermis2,3 and elongation of rete ridges.10 Histopathological examination of the lesion on the current patient’s right cheek showed increased melanin pigmentation in the basal layer and elongation of the rete ridges, suggestive of lentigines, supporting the diagnosis of PUL.
The main etiology of lentigines is chronic exposure to UV light,1 so counseling on photoprotection measures such as shelter or avoiding sun exposure, use of photoprotective clothing, hats, glasses, and sunscreen with an SPF of 30 or more is necessary.11 Avoiding sun exposure and applying sunscreen regularly can also prevent post-inflammatory hyperpigmentation, which occurs 7–14 days after laser treatment.11 Decreasing the melanin content in the skin before the laser treatment can decrease the rate of post-inflammatory hyperpigmentation.12 Tretinoin works by motivating epidermal and dermal turn-over, which may cause rapid loss of cell pigment.13 Hydroquinone is considered the primary and most effective topical agent for blocking melanin production through inhibition of the tyrosinase enzyme in melanocytes.12,13 The patient in this case report was counseled on photoprotection and given SPF 50 sunscreen cream on the first day of treatment. A mixture of 0.01% tretinoin and 4% hydroquinone cream at a ratio of 1:1 was applied nightly to the whole face to prime it for laser treatment. Complication in the form of post-inflammatory hyperpigmentation after laser treatment have not been reported.
The CuBr laser can emit two wavelengths, 511 nm and 578 nm.7 The 511 nm wavelength is often used for pigmented lesions and tends to be absorbed to a greater degree by melanin, resulting in a more selective damage.14 Dinehart et al14 reported the success of lentigine treatment after the administration of a CuBr 511 nm laser. The 578 nm CuBr laser is primarily used for vascular lesions; however, its targets consist not only of hemoglobin but also melanin. Melanocytes have VEGF receptors, which can respond to angiogenic factors.6 The interaction between skin vasculature and melanocytes is also associated with the development of pigmented lesions. Therefore, the CuBr 578 nm laser has direct and indirect effects on skin vasculatures and pigmented lesions, such as melasma.6,7 Cho et al6 reported improvements of lentigines after two months of two-stage CuBr 578 nm laser at a one-month interval. The first stage was given in the fast edge micropulse (FEM) mode setting, 3 kW peak power, 100 cm2 area, 2–3 passes with continuous movement using a 1 mm handpiece in contact with the gel. In the second stage, the gel was cleaned, then given an energy of 30 J/cm2, off time of 250 ms, and 1 pass, using a 0.6 mm handpiece.6 In the first treatment session, a two-wavelength combination treatment of the CuBr laser was performed in two stages. The first stage was administered with a wavelength setting of 511 nm, 30 J/cm2, and an off time of 125 ms using a 0.6 mm handpiece. In the current patient, the endpoint appeared grey. The second stage was set at a wavelength of 578 nm, Shining Bright mode, 3 kW peak power, 25 cm2 area, and continuous movement using a 1 mm handpiece in contact with the gel. The endpoint of immediate whitening was observed in the patient. In the second treatment session, there was a clinically significant improvement as the brown spots on the forehead and right cheek faded. In addition, the skin appeared brighter. A significant improvement was also observed in the spectrophotometry of hyperpigmented macules on the forehead, upper right cheek, and lower right cheek as there was an increase in L* values from 56.16, 58.12; and 59.77, to 57.77, 59.56; and 61.45, respectively.
Conclusion
The favorable response in this case report were achieved by addressing interaction of cutaneous vasculature and melanocyte which detained the development of pigmented lesions. Although this is only one case report presented successful outcome, the use of the combination of 511 nm and 578 nm CuBr laser can be considered as an alternative and effective therapeutic option particularly in PUL.
Ethics Statement
Publication of images was included in the patient’s consent for case publication. Institutional approval from The Research Ethic Committee of Dr. Hasan Sadikin General Hospital Bandung, Indonesia has been obtained to publish the case details (approval number: LB.02.01/X.6.5/255/2023).
Consent Statement
The authors certify that they have obtained all appropriate patient consent forms. The patient signed a consent form for the publication of case details and images.
Acknowledgments
The authors would like to thank the staff of the Department of Dermatology and Venereology, Faculty of Medicine, Universitas Padjadjaran, Bandung, West Java, Indonesia.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Kothiwala SK. Young female with multiple pigmented macules on face. In: Kothiwala SK, Tiwary AK, Kumar P, editors. Clinical Cases in Dermatology. Cham: Springer; 2020:23–30.
2. Imren IG, Yay FA, Eksioglu HM, Duygulu S. A rare case of adult onset partial unilateral lentiginosis. Dermatol Cosmet JOJ. 2020;2(4):35–50. doi:10.19080/JOJDC.2020.02.555594
3. Kim HT, Choi ME, Na H, et al. Partial unilateral lentiginosis: a clinicopathological analysis of 32 cases on the head and neck area in Korea. Int J Dermatol. 2021;60(11):1376–1384. doi:10.1111/ijd.15630
4. Vachiramon V, Leerunyakul K, Kositkuljorn C, Chayavichitsilp P. Combined isobutylamido thiazolyl resorsinol and low-fluence Q-switched Nd: YAG laser for the treatment of facial hyperpigmentation: a randomized, split-face study. J Cosmet Dermatol. 2021;20(6):1724–1731. doi:10.1111/jocd.13790
5. Hong JK, Han HS, Shin SH, Yoo KH. Partial unilateral lentiginosis successfully treated with a high fluence 1064-nm Q-switched Neodymium: yttrium-aluminum-garnet laser. Med Laser. 2021;10(2):120–122. doi:10.25289/ML.2021.10.2.120
6. Cho S, Choi YJ, Kang JS. Treatment of epidermal pigmented lesions with 578 nm yellow laser. Med Laser. 2015;4(1):35–38. doi:10.25289/ML.2015.4.1.35
7. Lee HI, Lim YY, Kim BJ, et al. Clinicopathologic efficacy of copper bromide plus/yellow laser (578 nm with 511 nm) for treatment of melasma in Asian patients. Dermatol Surg. 2010;36(6):885–893. doi:10.1111/j.1524-4725.2010.01564.x
8. Gupta V, Neha T, Binod K, Manish S. Partial unilateral lentiginosis with ipsilateral ocular involvement and seizures. Indian J Dermatol Venereol Leprol. 2019;85(1):130. doi:10.4103/ijdvl.IJDVL_1025_16
9. Yasar S, Ersanli A, Goktay F, Ayketin S, Cebeci D, Gunes P. Partial unilateral lentiginosis is mosaic neurofibromatosis type 1 or not? J Dermatol. 2017;44(1):29–35. doi:10.1111/1346-8138.13510
10. Gurel G, Sahin S, Colgecen E. Partial unilateral lentiginosis and colon polyp in a young male patient. J Clin Exp Invest. 2018;9(1):45–47. doi:10.5799/jcei.413079
11. Lyons AB, Trullas C, Kohli I, Hamzavi IH, Lim HW. Photoprotection beyond ultraviolet radiation: a review of tinted sunscreens. J Am Acad Dermatol. 2021;84(5):1393–1397. doi:10.1016/j.jaad.2020.04.079
12. Archer KA, Carniol PJ. Pre- and postoperative care for interventional skin rejuvenation. Facial Plast Surg Clin N Am. 2020;8(1):119–126. doi:10.1016/j.fsc.2019.09.010
13. Nasrollahi SA, Nematzadeh MS, Samadi A, et al. Evaluation of the safety and efficacy of a triple combination cream (hydroquinone, tretinoin, and fluocinolone) for treatment of melisma in Middle Eastern skin. Clin Cosmet Invest Dermatol. 2019;12:437–444. doi:10.2147/CCID.S202285
14. Dinehart SM, Waner M, Flock S. The copper vapor laser for treatment of cutaneous vascular and pigmented lesions. J Dermatol Surg Oncol. 1999;19(4):370–375. doi:10.1111/j.1524-4725.1993.tb00359.x
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
