Back to Journals » OncoTargets and Therapy » Volume 10
Parity association with clinicopathological factors in invasive breast cancer: a retrospective analysis
Authors Shen SD , Zhong SZ, Xiao GF, Zhou HB, Huang WH
Received 5 October 2016
Accepted for publication 29 November 2016
Published 21 January 2017 Volume 2017:10 Pages 477—481
DOI https://doi.org/10.2147/OTT.S123888
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Carlos E Vigil
Sandi Shen,1,2 Shizhen Zhong,1 Gaofang Xiao,3 Haibo Zhou,2 Wenhua Huang1
1Department of Human Anatomy, Guangdong Provincial Key Laboratory of Tissue Construction and Detection, School of Basic Medicine Science, Southern Medical University, Guangzhou, 2Thoracic Surgery, Qingyuan People’s Hospital, The Sixth Affiliated Hospital of Guangzhou Medical University, Qingyuan, 3Department of Pathology, Yuebei People’s Hospital, Shaoguan, People’s Republic of China
Abstract: The aim of this study was to determine the relationship between parity and age at diagnosis, primary tumor size, axillary lymph node (ALN) metastasis, histological grade, and subtype classification in patients with breast cancer. Data from 392 patients with invasive breast cancer were collected and divided into four groups: nulliparous (parity 0), parity 1, parity 2, and parity ≥3. The relationship between parity and age at diagnosis was assessed using post hoc Dunnett’s T3 test, and tumor size, the number of ALN metastases, and histological grade were analyzed using Spearman’s rho test. Breast cancer subtypes were analyzed using the chi-square (χ2) test. The results showed that the mean age at diagnosis increased with increased parity, and the mean age of patients with parity ≥3 was significantly greater than that of patients with parity 0, parity 1, and parity 2. The mean age at diagnosis of patients with parity 2 was greater than that of patients with parity 1. There was no significant difference in the mean age between patients with parity 0 and parity 1 or parity 0 and parity 2. Parity was negatively correlated with ALN metastasis. Parity was not correlated with tumor size or histological grade and the proportion of the four subtypes in breast cancer. So, increased parity deferred the onset of breast cancer and inhibited the metastasis of ALN, but did not affect tumor size, histological grade, or the proportion of subtypes. Increased parity was a protective factor against breast cancer.
Keywords: parity, invasive breast cancer, clinicopathological factors, age
Introduction
Parity is an important modulator of breast cancer risk and age at diagnosis.1,2 Multiple last birth was found to be protective against breast cancer.3 Late age at first full-term birth and low parity are high risk factors for breast cancer.4 Giving birth before the age of 30 was shown to reduce breast cancer risk, and women with their first full-term birth before the age of 20 had a 50% reduced risk of developing breast cancer compared with nulliparous women. In contrast, those who gave birth after the age of 35 had a 22% increased risk of breast cancer compared to women giving first birth before age 30, and this risk was the same as that of nulliparous women, with no risk reduction with increased parity.5 Indeed, increased parity was found to decrease the age at diagnosis of breast cancer.2
The morbidity of breast cancer was not very high (~40/10 million), but the rate of growth was dramatical in China. The family planning policy has been amended this year: one child policy was abrogated, and all couples were allowed to have two children. Many women would have parity ≥2 in the future; therefore, it was necessary to investigate the effect of parity on breast cancer.
The effect of parity on age of onset, primary tumor size, axillary lymph node (ALN) metastasis, histological grade, and the classification of breast cancer subtype has been seldom reported in breast cancer. The aim of our study was to analyze the effect of parity on the abovementioned clinicopathological factors in patients with breast cancer.
Patients and methods
A total of 392 patients with primary invasive breast cancer from 2010 to 2015 were reviewed at Yuebei People’s Hospital and divided into four groups: 15 nulliparous cases (parity 0), 165 cases with parity 1, 152 cases with parity 2, and 60 cases with parity ≥3. There were no cases with pregnancy-associated breast cancer. All data were analyzed anonymously, and the information that could identify individual participants during or after data collection was preserved well and could be accessed. Breast cancer patients had no family history of cancer and had not undergone radiotherapy, chemotherapy, or hormone therapy before the pathological specimens were extracted. The samples were fixed with 10% neutral buffered formalin and then embedded in paraffin. According to the TNM stage criterion of the seventh edition of the AJCC,6 tumor size was divided into three categories: ≤2 cm, 2–5 cm, and >5 cm; ALN metastasis was divided into four categories: no cancer metastasis, cancer metastasis in 1–3 lymph nodes, cancer metastasis in 4–9 lymph nodes, and cancer metastasis in ≥10 lymph nodes. Histological grade was divided into three categories based on the modified Nottingham criteria of Bloom and Richardson.7,8 Breast cancer was classified into four subtypes according to the 13th St Gallen International Breast Cancer Conference.9 All clinicopathological factors were analyzed retrospectively. Parity and age were defined at the time of breast cancer diagnosis.
Statistical analysis
Data were analyzed using SPSS Version 20.0 software (SPSS Inc., Chicago, IL, USA). Continuous variables are presented as mean ± standard error of the mean (SEM). The relationship between parity and age was assessed using one-way analysis of variance (ANOVA) with post hoc Dunnett’s T3 test. Tumor size, the number of ALN metastases, and histological grade were analyzed using Spearman’s rho test, and breast cancer subtypes were analyzed using the chi-square (χ2) test. All statistical analyses were two-sided with significance defined as a P-value of <0.05.
Ethical standards
The study complied with the current laws of China and was approved by the institutional review board of Southern Medical University; this institutional review board waived the need for patient consent to use patient data, due to the retrospective nature of the research.
Results
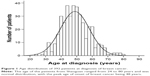
The age distribution is shown in Figure 1. The age range was from 24 to 80 years; the median age was 48 years; and the mean age was 48.8±9.3 years. The mean age at diagnosis increased with increased parity (Figure 2), and the mean age of patients with parity ≥3 was significantly greater than that of patients with parity 0 (P=0.005), parity 1 (P<0.001), and parity 2 (P<0.001). The mean age of patients with parity 2 was greater than that of patients with parity 1 (P=0.021). There was no significant difference in the mean age of patients with parity 0 and parity 1 (P=0.997) or between patients with parity 0 and parity 2 (P=0.539), the result may be due to the few nulliparous patients.
The clinicopathological data from all patients and the statistical analyses are summarized in Table 1. Parity was negatively correlated with ALN metastasis (correlation coefficient [CC] =−0.340, P<0.001), and the number of ALN metastases decreased with increased parity in patients with breast cancer.
  | Table 1 Associations between parity and clinicopathological factors in invasive breast cancer |
Parity was not correlated with tumor size (CC =0.081, P=0.109) or histological grade (CC =0.024, P=0.633), and there was no obvious relationship between parity and the proportion of the four subtypes in breast cancer (χ2=10.184, P=0.336).
Discussion
Breast cancer is the most common malignant tumor in females,10 and its morbidity has been dramatically increasing by 3%–5% each year in China. The peak age of onset was previously estimated to be 45 years. While the peak age of onset of breast cancer in our study was 48 years, with a mean age of 48.8 years now, representing an ~3 years peak age delay. The proportion of women giving childbirth in advanced age has increased (but seldom >35 years), and the age at the completion of the last pregnancy and lactation has increased. The cycle effect of hormones on the breast can be avoided during pregnancy or lactation (breast feeding is common in China). Lower estrogen and higher progesterone are known to protect the breast from canceration.11,12 In addition, the maternal serum alpha-fetoprotein (AFP) level was high during pregnancy, and the AFP had direct antibreast cancer activity.13,14 Therefore, the age at diagnosis of breast cancer increased with increased parity. Albrektsen et al15 found that women with multiparity had a slightly lower risk of breast cancer compared with women with parity 1. Nevertheless, the reduction in risk diminished with increasing parity. Furthermore, the risk elevated among women with parity ≥3.15 Woods et al2 reported that the age at breast cancer diagnosis decreased with increased parity.16 These contradictory results were attributed to a higher proportion of women who delivered after the age of 35, the lower rates of lactation in Western women, ethnic difference, and so on.
To date, the status of ALN is a very powerful prognostic factor for patients with breast cancer. The prognosis of patients with ALN metastasis was poorer than that of those without ALN metastasis.17 Age at diagnosis of breast cancer is a predictor of ALN metastasis, younger patients have more ALN metastasis than older patients.18 Our study showed that parity was correlated with ALN metastasis, and the number of ALN metastasis declined with increased parity. This was attributed to the increase in age at diagnosis with increased parity.
In breast cancer, tumor size is a powerful predictor for local recurrence and regional and systemic spread. Oppidan women seldom had parity ≥1, while the women in rural area in China were often multiparous. Although breast mass was palpated easily in women with more parity and lactation, these women often acquired few health-care resources, did not pay more attention to their breast health, seldom performed self-examination and received physical examination, so their breast lesions were not detected early. Therefore, parity was not associated with tumor size at the time of breast cancer diagnosis.
Histological grade is an indicator of malignant degree.8 A high histological grade indicated that the tumor grew fast and had strong invasion, resulting in a poor prognosis. Our study showed that there were no significant differences in histological grade in the four groups of patients. The result was consistent with the report of Somasegar et al19 that there was no association of parity with breast cancer histological grade.
Each breast cancer subtype has its own biological characteristics, and treatment plan optimization is based on the subtype classification. The proportion of each subtype was not significantly different in the four groups of patients. Ursin et al20 reported that parity reduced the risk of estrogen/progesterone receptor-positive breast cancer and lactation reduced the risk of both receptor-positive and -negative breast cancer. Lambertini et al21 reported that parity reduced the risk of luminal subtype, lactation reduced the risk of both luminal and triple-negative (TN) subtypes. Besides, the subtype classification was involved in the expression status of HER2 and Ki67. Thus, the effect of only parity on the subtype classification was uncertain.
Based on our results, we can speculate that tumor initiation occurred at the end of the last parity and lactation and not before the first birth. In contrast, Woods et al2 concluded that tumor growth was initiated before the first birth. Accordingly, the high levels of estrogen and progesterone during pregnancy would promote hormone-dependent tumor growth and decrease the age at diagnosis. However, our findings were in direct opposition to that conclusion.
Conclusion
In our study, increased parity deferred the onset of breast cancer and inhibited metastasis of ALN, but did not affect tumor size, histological grade, and the proportion of the subtypes at diagnosis of breast cancer. Therefore, increased parity was a protective factor against breast cancer, and parity should be taken into account when we schedule the optimum age to screen for breast cancer.
Acknowledgments
We acknowledge the support of the directors and pathologists (Xin Xu, Kangsheng Bei, Richang Du, and Caiyun Tan) involved in the collection and analysis of the current data. The study was supported by National Natural Science Foundation of China No 61427807; Fujian Province Introduction of Major Research and Development Institution Funding Project No 2012I2004; and Hebei Science and Technology Support Project No 14277731D.
Disclosure
The authors report no conflicts of interest in this work.
References
Kelsey JL, Gammon MD. The epidemiology of breast cancer. CA Cancer J Clin. 1991;41(3):146–165. | ||
Woods KL, Smith SR, Morrison JM. Parity and breast cancer: evidence of a dual effect. Br Med J. 1980;281(6237):419–421. | ||
Jacobson HI, Thompson WD, Janerich DT. Multiple births and maternal risk of breast cancer. Am J Epidemiol. 1989;129(5):865–873. | ||
MacMahon B, Cole P, Lin TM, et al. Age at first birth and breast cancer risk. Bull World Health Organ. 1970;43(2):209–221. | ||
Ewertz M, Duffy SW, Adami HO, et al. Age at first birth, parity and risk of breast cancer: a meta-analysis of 8 studies from the Nordic countries. Int J Cancer. 1990;46(4):597–603. | ||
Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A. AJCC Cancer Staging Manual. 7th ed. New York, NY: Springer; 2010. | ||
Singletary SE, Allred C, Ashley P, et al. Revision of the American Joint Committee on Cancer staging system for breast cancer. J Clin Oncol. 2002;20(17):3628–3636. | ||
Harris L, Fritsche H, Mennel R, et al. American Society of Clinical Oncology 2007 update of recommendations for the use of tumor markers in breast cancer. J Clin Oncol. 2007;25(33):5287–5312. | ||
Goldhirsch A, Winer EP, Coates AS, et al; Panel Members. Personalizing the treatment of women with early breast cancer: highlights of the St Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2013. Ann Oncol. 2013;24(9):2206–2223. | ||
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin. 2015;65(1):5–29. | ||
Okobia MN, Bunker CH. Epidemiological risk factors for breast cancer – a review. Niger J Clin Pract. 2005;8(1):35–42. | ||
Kobayashi S, Sugiura H, Ando Y, et al. Reproductive history and breast cancer risk. Breast Cancer. 2012;19(4):302–308. | ||
Jacobson HI, Andersen TT, Bennett JA. Development of an active site peptide analog of alpha-fetoprotein that prevents breast cancer. Cancer Prev Res. 2014;7(6):565–573. | ||
Richardson BE, Hulka BS, Peck JL, et al. Levels of maternal serum alpha-fetoprotein (AFP) in pregnant women and subsequent breast cancer risk. Am J Epidemiol. 1998;148(8):719–727. | ||
Albrektsen G, Heuch I, Kvale G. Multiple births, sex of children and subsequent breast-cancer risk for the mothers: a prospective study in Norway. Int J Cancer. 1995;60(3):341–344. | ||
Nagata C, Hu YH, Shimizu H. Effects of menstrual and reproductive factors on the risk of breast cancer: meta-analysis of the case-control studies in Japan. Jpn J Cancer Res. 1995;86(10):910–915. | ||
Aitken E, Osman M. Factors affecting nodal status in invasive breast cancer: a retrospective analysis of 623 patients. Breast J. 2010;16(3):271–278. | ||
Li L, Chen LZ. Factors influencing axillary lymph node metastasis in invasive breast cancer. Asian Pac J Cancer Prev. 2012;13(1):251–254. | ||
Somasegar S, Li L, Thompson CL. No association of reproductive risk factors with breast cancer tumor grade. Eur J Cancer Prev. Epub 2016 Nov 7. | ||
Ursin G, Bernstein L, Lord SJ, et al. Reproductive factors and subtypes of breast cancer defined by hormone receptor and histology. Br J Cancer. 2005;93(3):364–371. | ||
Lambertini M, Santoro L, Del Mastro L, et al. Reproductive behaviors and risk of developing breast cancer according to tumor subtype: A systematic review and meta-analysis of epidemiological studies. Cancer Treat Rev. 2016;49:65–76. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.