Back to Journals » Psychology Research and Behavior Management » Volume 16
Parental Pressure on Child Body Image, BMI, Body Image Dissatisfaction Associated with Eating Disorders in School-Age Children in China: A Path Analysis
Authors Chen J, Liu K, Zhang J, Liu S, Wang Y, Cao R, Peng X, Han M, Han H, Yao R, Fu L
Received 27 April 2023
Accepted for publication 5 August 2023
Published 16 August 2023 Volume 2023:16 Pages 3247—3258
DOI https://doi.org/10.2147/PRBM.S418535
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Igor Elman
Jiaoyan Chen, Keke Liu, Juan Zhang, Songhui Liu, Yuanyuan Wang, Ruiyao Cao, Xingwang Peng, Mei Han, Hui Han, Rongying Yao, Lianguo Fu
Department of Child and Adolescent Health, School of Public Health, Bengbu Medical College, Bengbu, Anhui, 233030, People’s Republic of China
Correspondence: Lianguo Fu, Department of child and adolescent health, School of Public Health, Bengbu Medical College, 2600 East Sea Avenue, Bengbu, Anhui, People’s Republic of China, Tel +0086-13195529639, Email [email protected]
Background: Children’s eating behaviors, body shape and body image cognition may be more susceptible to the influence of their parents, but these influences may be weakened with age. There may be different association pathways between parental pressure on children’s body image (PPCBI), body mass index (BMI), body image dissatisfaction (BID) and eating disorders (EDs) among children and adolescents at different developmental stages.
Methods: The stratified cluster sampling method (Stratified by grade, and took the classes as clusters) was used to select 486 students aged 8– 15 years in two 9-year schools. Children’s body height, weight, testicular volume and breast development were measured. PPCBI, BID, and EDs were investigated using the Appearance-related Social Stress Questionnaire, Body Size Questionnaire (BID-14), and EDI-1 scale, respectively.
Results: The boys before puberty initiation had significantly higher EDs score (182.3± 50.8) than girls before puberty initiation (164.1± 58.1) (P< 0.05). There were significant association pathways of PPCBI→BMI→BID→EDs and PPCBI→BID→EDs in boys before puberty initiation (β=0.035, P< 0.01; β=0.059, P< 0.01), in boys after puberty initiation (β=0.032, P< 0.01; β=0.175, P< 0.001), and in girls after puberty initiation (β=0.026, P< 0.01; β=0.172, P< 0.001). There was a positive association pathway of PPCBI→EDs in boys before puberty initiation (β=0.30, P< 0.001) and PPCBI→BID→EDs in girls before puberty initiation (β=0.176, P< 0.01).
Conclusion: Parental pressure on children’s body image may positively associate with children’s eating disorders through BMI and body image dissatisfaction in boys and girls after puberty initiation and directly associate with eating disorders in boys before puberty initiation; however, it may indirectly associate with eating disorders only through BID in girls before puberty initiation.
Keywords: parental pressure, body image dissatisfaction, eating disorders, children, path analysis
Introduction
Eating disorders, mainly manifested by abnormal eating and weight control, are prevalent among children and adolescents. An EDs is an important risk factor for nutritional intake and physical and mental development in children themselves and in adulthood. In a recent Australian survey of children aged 5–13 years, the minimum prevalence of EDs was found to be approximately 2.79/100,000 per year, and the prevalence of EDs in children has nearly doubled in the last 10 years, with a higher rate in younger boys than girls1. A longitudinal study showed that the symptoms of EDs were most common between the ages of 12 and 15 years.2 The excessive expectation of weight loss, unhealthy weight control behaviors, and body image dissatisfaction are major risk factors for EDs.3 Parental pressure on the children’s body image often influences the children’s self-image attitudes and changes in the children’s weight,4,5 and may also promote the development of EDs symptoms in children.6,7 A study suggests that childhood EDs may progress to more severe EDs in mid-adolescence or adulthood symptoms,8 and cause additional psychological distress and physical illness.9,10 This finding reveals that the correlation pathways PPCBI, BMI, BID, and EDs play an important role in promoting children’s healthy eating behavior.
Body image (BI) is a subjective impression of the body portrayed by individuals or others.11 With the popularity of “thin for beauty” and sociocultural pressure on body image and appearance, a BMI that is too high or too low is the direct cause of BID, which will also directly affect the development of EDs.12–16 BI is associated with healthy behaviors and lifestyles, including balanced dietary and nutritional intake behaviors.17 In many studies, boys have been found to have poorer dietary habits than girls, such as more smoking and excessive alcohol consumption,18,19 which may be an important cause of body image dissatisfaction and gender differences in eating disorders. Deborah et al reported that paying too much attention to weight or body shape not only caused serious psychological distress but also promoted binge eating and dieting behaviors in children.20 Adolescent girls with a higher body mass index (BMI) who desire to lose weight and boys who prefer to increase their physical strength appear to be at greater risk for eating disorders.21,22 The development of children’s bodies before puberty is steadily increasing, while that after puberty is rapidly increasing. Body dissatisfaction occurs relatively infrequently in prepubertal children,23 and increases with age in boys and girls.24 From early adolescence onwards, dietary restrictions and dieting are more likely to occur due to the increasing emphasis on physical appearance and weight problems.24,25 Therefore, there may be different association pathways between BMI, BID, and EDs among children at different developmental stages.
Parents play an integral role in the child’s body shape development and positive or negative body image cognitive attitudes.26–28 Duchin et al29 reported that parents expected their children to be thinner, and their children tended to have larger body sizes or higher BMIs. Parents who teased their children about their body image or commented on their child’s body shape put great pressure on children’s appearance.30 Parental pressure on children’s appearance has a direct impact on children’s eating behaviors, such as reducing or restricting the frequency of unhealthy eating behaviors.31,32 As the autonomous behavior of young children is relatively weak, their eating behaviors, body shape, and body image cognition may be more susceptible to the influence of their parents, but the influence may be weakened as children’ age. There also may be different association pathways between PPCBI, BMI, and BID among children at different developmental stages. In addition, eating disorders in prepubertal children are more likely to be accompanied by a shorter duration of weight loss.33 With the onset of puberty, children undergo dramatic changes in their physical as well as social perceptions. There are more reports of stress from parents about their body image and eating disorders among adolescents.34 Eating disorders also increase from early adolescence, usually peaking in late adolescence,35 and Abebe et al showed that with increased self-perceptions, children tend to develop in conflict with their ideal body image during adolescence, and girls are more likely to show binge eating symptoms in early.36 Therefore, the purpose of this study was to analyze the different relationship pathways between PPCBI, BMI, BID and EDs to provide a theoretical basis for preventing the occurrence of eating disorders in Chinese children and adolescents with different developmental stages.
Methods
Participants
The stratified cluster random sampling method was used (stratified by grade, and took the classes as clusters) to select participants from 2 nine-year schools. A total of 486 students, including 262 (54%) boys and 224 (46%) girls, were recruited.
Design and Procedures
This study was a cross-sectional study. The Participants who met the following criteria were included in the study: (a) The healthy children with no history of neurological, psychiatric or intellectual disorders; (b) The students’ guardians all signed informed consent forms before the questionnaire survey and measurements in this study; (c) with the assistance of standardized trained researchers, participants filled out the questionnaire on their own in a centralized format. This study was approved by the Ethics Committee of Bengbu Medical College ([2015] No.003) and was conducted according to the Declaration of Helsinki.
Measurements
Body Measurements
Body height, weight and secondary sex index were measured by medical personnel who received standardized training, each test is performed by two or more medical personnel, and the consistent result of the measurement of each measurer is taken as the final result. A mechanical height meter (Shanghai Liheng Instrument Co) was used to measure body height with an accuracy of 0.1 cm. The weight is measured using an electronic scale (Xiaomi Weight Scale 2, Xiaomi Technology Co), and the counting is accurate to 0.1 kg. Boys’ testicular volume was measured using a Prader testicular volume meter.37 Girls’ breast development was examined according to Tanner staging.38 The pubertal developmental stages were divided into two stages (boys before puberty initiation: boys’ testicular volume <4 mL, boys after puberty initiation: boys’ testicular volume ≥4 mL; girls before puberty initiation: girls’ breast development <Tanner II, girls after puberty initiation: girls’ breast development ≥Tanner II).
Questionnaire Survey
Eating Disorders Measurement
The Eating Disorders Inventory (EDI-1)39 was developed by Garner in 1983. In this study, the Chinese version of EDI-1 was used to survey children’s EDs.40 There are 64 items on the EDI-1 scale, and each item is scored 1–6 point from never to always. A higher score indicates a more serious eating disorder. The Cronbach’s coefficient was 0.944, which indicates that the EDI-1 scale has good reliability.
Parental Pressure on Children’s Body Image Measurement
In this study, the parental pressure subscale in the Appearance-Related Social Pressure Questionnaire41 was used to assess parental pressure on children’s body image. The parental pressure subscale includes 16 items, and each item is scored on a 1–5 point scale. Higher total scores indicate greater parental pressure on children’s body image. The Cronbach’s coefficient was a coefficient of 0.902, which indicates that the parental pressure subscale has good reliability.
Body Image Dissatisfaction Measurement
The short version of the body shape questionnaire (BSQ-14)42 was used survey children’s body image dissatisfaction. The BSQ-14 scale includes a total of 14 questions, and each question is scored on a 1–6 point scale from never to always. Higher total scores represent greater body image dissatisfaction. The Cronbach’s coefficient was a coefficient of 0.933, which indicates that the body shape questionnaire has good reliability.
Data Analysis
IBM SPSS 23.0 software was used to analyze the data. Quantitative data were described as the mean ± SD. t tests were used to compare differences in PPCBI, BMI, BID and EDs scores between boys and girls at different developmental stages. Pearson’s correlation and multiple linear regression were used to analyze correlations between PPCBI, BMI, BID and EDs. AMOS 24.0 was used to construct an association pathway among PPCBI, BMI, BID and EDs, and the bootstrap procedure was used to test for direct and indirect effects. P < 0.05 was considered statistically significant.
Results
A total of 486 children were validly surveyed in this study, including 168 children with prepuberty initiation (115 boys, 53 girls) and 318 children after puberty initiation (147 boys, 171 girls). Boys before puberty initiation had higher eating disorder score (182.3±50.8) than girls before puberty initiation (164.1±58.1) (P<0.05); however, there was no statistically significant difference between the eating disorder score between boys after puberty initiation (184.9±47.1) and girls after puberty initiation (178.7±48.6) (P>0.05), between boys before puberty initiation (182.3±50.8) and boys after puberty initiation (184.9±47.1) (P>0.05), or between girls before puberty initiation (164.1±58.1) and girls after puberty initiation (178.7±48.6) (P>0.05). See Table 1 for details.
 |
Table 1 Comparisons of PPCBI, BID, EDs, BMI and Age Between Genders ( |
Correlation Analysis of Different Variables
In boys before puberty initiation, the PPCBI score, BMI and BID score were significantly positively correlated with the EDs score (P<0.05), and BMI, the PPCBI score, and the BID score were positively correlated with each other (P<0.05). In girls before puberty initiation, the BID score was positively correlated with the EDs score, BMI, and PPCBI score (P<0.05). In boys after puberty initiation, the BID score was positively associated with the EDs score, BMI, and PPCBI score (P<0.05), and BMI was positively associated with the PPCBI score (P<0.05). In girls after puberty initiation, PPCBI and BID scores were positively correlated with the EDs score (P<0.05), and BMI, the PPCBI score and the BID score were positively correlated with each other (P<0.05). See Table 2 for details.
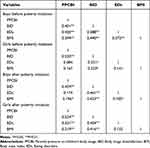 |
Table 2 Correlation Coefficients Between PPCBI, BID, EDs and BMI |
Multifactorial Analysis
After adjusting for age, PPCBI score, BMI, BID score and EDs score as dependent variables, and the variables associated with them as independent variables, multiple linear regression was conducted to analyze their associations (See Table 3 for details).
 |
Table 3 The Results of Multiple Linear Regression of Association Among PPCBI, BMI, BID and EDs Among Children and Adolescent at Different Development Stages |
In boys before puberty initiation, the PPCBI and BID scores were positively associated with the EDs score (P<0.05); the PPCBI score was positively associated with BMI and the BID score (P<0.05); and BMI was positively associated with the BID score (P<0.05). In girls before puberty initiation, the BID score was positively associated with the EDs score (P<0.05); and the PPCBI score was positively associated with the BID score (P<0.001). In boys and girls after puberty initiation, the BID score was positively associated with the EDs score (P<0.001); the PPCBI score was positively associated with BMI and the BID score (P<0.05); and BMI was positively associated with the BID score (P<0.01). Therefore, there may be association pathways between PPCBI, BMI, BID and EDs, as shown in Figure 1.
Fitting of Association Pathways
The preliminary association pathways between PPCBI, BMI, BID and EDs were fitted, and the indices of the fitting models showed that all four association pathways had good fitting effects. See Table 4 for details.
 |
Table 4 Pathways Model Fitting Indices Recommended Indexes |
In boys before puberty initiation, the PPCBI and BID score were positively associate with the EDs score (β=0.30, P<0.001; β=0.23, P<0.05); the PPCBI score and BMI were positively associated with the BID score (β=0.25, P<0.01; β= 0.38, P<0.01); and the PPCBI score was positively associated with BMI (β=0.38, P<0.001). Moreover, indirect association pathways of PPCBI→BMI→BID→EDs and PPCBI→BID→EDs were statistically significant (β=0.035, P<0.01; β=0.059, P<0.01).
In girls before puberty initiation, the BID score was associated with the EDs score (β=0.34, P<0.01); and the PPCBI score was positively associated with the BID score (β=0.52, P<0.001). The indirect association pathway of PPCBI→BID→EDs was statistically significant (β=0.176, P<0.01).
In boys after puberty initiation, the BID score was positively associated with the EDs score (β=0.45, P<0.01); the PPCBI score and BMI were positively associated the BID score (β=0.39, P<0.001; β=0.36, P<0.001); and the PPCBI score was positively associated with BMI (β=0.20, P<0.05). The indirect pathways of PPCBI→BMI→BID→EDs and PPCBI→BID→EDs were statistically significant (β=0.032, P<0.01; β=0.175, P<0.001).
In girls after puberty initiation, the BID score was positively associated with the EDs score (β=0.38, P<0.001); the PPCBI score and BMI were positively associated with the BID score (β=0.46, P<0.001; β=0.32, P<0.001); and the PPCBI score was positively associated with BMI (β=0.22, P<0.01). The indirect association pathways of PPCBI→BMI→BID→EDs and PPCBI→BID→EDs were statistically significant (β=0.026, P<0.01; β=0.172, P<0.001). The direct and indirect coefficients of association pathways were shown in Figure 2 and Table 5.
 |
Table 5 Indirect Coefficients of Association Pathways Among PPCBI, BMI, BID, EDs in Children and Adolescents at Different Development Stages |
Discussion
With the widespread prevalence of unhealthy eating behaviors among children and adolescents, their healthy eating has received more attention. In this study, we found that parental pressure on children’s body image through child BMI and body image dissatisfaction was positively associated eating disorders in boys before puberty and after puberty initiation and girls after puberty initiation; however, only child BID was positively associated with eating disorders in girls before puberty initiation.
This study found that the eating disorders score in boys before puberty initiation was significantly higher than that in girls before puberty initiation, which showed that eating disorders in boys before puberty initiation were more serious than that of girls before puberty initiation. Although many scholars report that girls account for a greater prevalence of eating disorders,43,44 eating disorders seem to have a more serious impact on boys. Research shows that boys with anorexia nervosa presented a higher standardized mortality rate than girls.45 Pinhas et al46 also reported more signs of growth retardation in boys aged 5–12 years with eating disorders, which may be associated with boys showing less needing to seek treatment.47 Solano et al48 found that boys pay more attention to their parents’ perceptions of their body image. Parents play a significant role in boys’ emotional regulation.49 Therefore, appearance pressure from parents is more likely to aggravate the symptoms of eating disorders in boys. The study also found that prepubertal boys were not as good as girls in regulating emotional strategies,50 which may result in boys at this stage of development having a greater psychological burden than girls when dealing with eating disorders. This may be an important reason why boys before puberty initiation showed higher eating disorder scores than girls before puberty initiation.
Based on the correlation analysis and multiple linear regression analysis, we fitted the relationship pathways between parental pressure on children’s body image, BMI, body image dissatisfaction, and eating disorders. The present study showed that parental pressure on children’s body image was positively associated eating disorders through body image dissatisfaction in boys before puberty initiation and in boys and girls after puberty initiation. Studies have shown that parents, peers, and media influence children’s negative body image perceptions, such as fear of weight gain and body image dissatisfaction.51,52 Parents’ negative comments (such as blaming and teasing) on children’s weight or body shape will cause psychological distress and may promote the development of anxiety, depression and eating disorders.4,53 A meta-analysis found that parents’ encouragement of children to lose weight and negative comments about their weight or body shape were associated with children’s body image dissatisfaction and eating disorders.54 Negative comments on weight, body shape or eating behaviors seem to be common, with more negative information coming from mothers than from fathers.55,56 Therefore, parental pressure on children’s appearance and eating behaviors plays an impact role in children’s eating disorders.
Furthermore, the results of this study showed that body mass index was positively associated eating disorders through body image dissatisfaction. There is a consensus that overweight and obese children have greater body dissatisfaction.57 Most children with eating disorders also expressed dissatisfaction with their body image.58 In this study, parental pressure on children’s body image also influenced children’s BMI, which may be related to parenting styles. For example, parents who are aware that their children are overweight or obese are more likely to try to control eating behaviors or encourage exercise to change their child’s weight.59,60
We also found that parental pressure on children’s body image directly and positively was associated with eating disorders in boys before puberty initiation and was indirectly and positively associated with eating disorders through BID in girls before puberty initiation. As we mentioned earlier, prepubertal boys are less able than girls to regulate their emotions.50 Some intervention studies on eating disorders have found that the intervention effect of parents is more significant in young children,61,62 which suggests that the dietary behavior of young boys may be more affected by their parents. This is probably because parental pressure on children’s body image in boys before puberty initiation is also directly and positively associated with childhood eating disorders and does not manifest in children in late adolescence. Handford et al showed that negative comments from parents about children’s appearance were associated with body image dissatisfaction in preadolescent girls.63 Studies have found that girls aged 3 to 6 years pay more attention to their body parts, such as the abdomen and legs,64,65 and preschool girls also highlight concerns about their appearance, especially clothes and hair.66 Therefore, girls at this age may be more concerned with the evaluation of their body parts and appearance from others, diminishing the influence of weight on them. However, as girls age, dissatisfaction with both appearance and weight becomes more prominent in adolescent girls.67 This may explain why parental body image pressure on prepubertal girls was positively associated with childhood eating disorders only through childhood body image dissatisfaction, whereas postpubertal girls demonstrated the effect of both body image dissatisfaction and BMI on eating disorders. Parental pressure on the child’s body image that results in the child’s eating disorder may stem from the parents’ dissatisfaction with their own image.32,68 A study showed that body imagery perception was only associated with a healthier lifestyle (healthy diet) in older men.69 Perhaps the role of parents’ life background and dietary culture in children with dietary disorders should also be an issue worth considering.
Limitations
There are some limitations in the study. First, this cross-sectional study has limitations in explaining causality, and the study found that the relationship pathways need further prospective research verification. Second, there are numerous factors influencing children’s eating disorders, such as peer pressure, media messages, and psychological disorders, such as anxiety and depression, which were not considered in this study. Third, the current findings are only based on Chinese children and adolescents, which may limit their applicability to children and adolescents in other cultural contexts.
Conclusions
The present study found that parental pressure on children’s body image was associated with children’s body mass index and body image dissatisfaction, and was associated with children’s eating disorders through them. Parental pressure on children’s body image was also directly associated with children’s eating disorders in boys before puberty initiation, while was only associated with children’s eating disorders through children’s body image dissatisfaction in girls before the onset of puberty. Parental pressure on children’s body image may play an important role in children’s negative body image cognition and eating disorders, therefore, parents should be guided to form a correct perception of children’s body image to reduce the risk of eating disorders in children.
Abbreviations
PPCBI, parental pressure on children’s body image; BMI, body mass index; BID, body image dissatisfaction; EDs, eating disorders; X2/DF, chi-square/free ratio; GFI, goodness-of-fit index; AGFI, adjusted goodness-of-fit index; SRMR, standardized root mean square residual; NFI, standard fit index; TLI, Tucker-Lewis index; CFI, comparative fit index.
Data Sharing Statement
All data generated or analyzed during this study are not publicly available to maintain the privacy of the individuals’ identities. The dataset supporting the conclusions is available upon request to the corresponding author.
Ethics Approval and Consent to Participate
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Medical Research Ethics Committee of Bengbu Medical College ([2015] NO.003). Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Acknowledgments
We would like to thank the teachers and students who participated in this study, as well as all other members for their support during the different phases of the study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the National Natural Science Foundation of China (Grant Number [81502823]) and 512 Talent Cultivation Plan of Bengbu Medical College (Grant Number [by51201204]).
Disclosure
The authors declare that they have no competing interests.
References
1. Morris A, Elliott E, Madden S. Early-onset eating disorders in Australian children: a national surveillance study showing increased incidence. Int J Eat Disord. 2022;55(12):1838–1842. doi:10.1002/eat.23794
2. Breton É, Dufour R, Côté SM, et al. Developmental trajectories of eating disorder symptoms: a longitudinal study from early adolescence to young adulthood. J Eat Disord. 2022;10(1):84. doi:10.1186/s40337-022-00603-z
3. Stice E, Gau JM, Rohde P, Shaw H. Risk factors that predict future onset of each DSM-5 eating disorder: predictive specificity in high-risk adolescent females. J Abnorm Psychol. 2017;126(1):38–51. doi:10.1037/abn0000219
4. Rodgers RF, Paxton SJ, Chabrol H. Effects of parental comments on body dissatisfaction and eating disturbance in young adults: a sociocultural model. Body Image. 2009;6(3):171–177. doi:10.1016/j.bodyim.2009.04.004
5. Helfert S, Warschburger P. A prospective study on the impact of peer and parental pressure on body dissatisfaction in adolescent girls and boys. Body Image. 2011;8(2):101–109. doi:10.1016/j.bodyim.2011.01.004
6. Lydecker JA, Park J, Grilo CM. Parents can experience impairment because of their children’s weight and problematic eating behaviors. J Adolesc Health. 2020;66(2):189–194. doi:10.1016/j.jadohealth.2019.07.026
7. Saltzman JA, Liechty JM. Family correlates of childhood binge eating: a systematic review. Eat Behav. 2016;22:62–71. doi:10.1016/j.eatbeh.2016.03.027
8. McClelland J, Robinson L, Potterton R, Mountford V, Schmidt U. Symptom trajectories into eating disorders: a systematic review of longitudinal, nonclinical studies in children/adolescents. Eur Psychiatry. 2020;63(1):e60. doi:10.1192/j.eurpsy.2020.55
9. Hornberger LL, Lane MA. Identification and Management of Eating Disorders in Children and Adolescents. Pediatrics. 2021;147(1):56.
10. Treasure J, Duarte TA, Schmidt U. Eating disorders. Lancet. 2020;395(10227):899–911. doi:10.1016/s0140-6736(20)30059-3
11. Ábrahám I, Jambrik M, John B, Németh AR, Franczia N, Csenki L. Body image and body image distortion. Orv Hetil. 2017;158(19):723–730. doi:10.1556/650.2017.30752
12. Štefanová E, Bakalár P, Baška T. Eating-Disordered Behavior in Adolescents: associations with Body Image, Body Composition and Physical Activity. Int J Environ Res Public Health. 2020;17(18):6665. doi:10.3390/ijerph17186665
13. Prnjak K, Hay P, Mond J, et al. The distinct role of body image aspects in predicting eating disorder onset in adolescents after one year. J Abnorm Psychol. 2021;130(3):236–247. doi:10.1037/abn0000537
14. Cerea S, Doron G, Manoli T, Patania F, Bottesi G, Ghisi M. Cognitive training via a mobile application to reduce some forms of body dissatisfaction in young females at high-risk for body image disorders: a randomized controlled trial. Body Image. 2022;42:297–306. doi:10.1016/j.bodyim.2022.07.010
15. Izydorczyk B, Sitnik-Warchulska K, Lizińczyk S, Lipowska M. Socio-Cultural Standards Promoted by the Mass Media as Predictors of Restrictive and Bulimic Behavior. Front Psychiatry. 2020;11:506. doi:10.3389/fpsyt.2020.00506
16. Harrison A, Francesconi M, Flouri E. Types of Eating Disorder Prodrome in Adolescence: the Role of Decision Making in Childhood. Front Psychol. 2022;13:743947. doi:10.3389/fpsyg.2022.743947
17. Wawrzyniak A, Myszkowska-Ryciak J, Harton A, et al. Dissatisfaction with Body Weight among Polish Adolescents Is Related to Unhealthy Dietary Behaviors. Nutrients. 2020;12(9):57.
18. von Bothmer MI, Fridlund B. Gender differences in health habits and in motivation for a healthy lifestyle among Swedish university students. Nurs Health Sci. 2005;7(2):107–118. doi:10.1111/j.1442-2018.2005.00227.x
19. Varì R, Scazzocchio B, D’Amore A, Giovannini C, Gessani S, Masella R. Gender-related differences in lifestyle may affect health status. Annali dell’Istituto superiore di sanita. 2016;52(2):158–166. doi:10.4415/ann_16_02_06
20. Mitchison D, Hay P, Griffiths S, et al. Disentangling body image: the relative associations of overvaluation, dissatisfaction, and preoccupation with psychological distress and eating disorder behaviors in male and female adolescents. Int J Eat Disord. 2017;50(2):118–126. doi:10.1002/eat.22592
21. Murray SB, Blashill AJ, Calzo JP. Prevalence of Disordered Eating and Associations With Sex, Pubertal Maturation, and Weight in Children in the US. JAMA Pediatr. 2022. doi:10.1001/jamapediatrics.2022.2490
22. Tremblay L, Lariviere M. The influence of puberty onset, body mass index, and pressure to be thin on disordered eating behaviors in children and adolescents. Eat Behav. 2009;10(2):75–83. doi:10.1016/j.eatbeh.2008.12.001
23. Smolak L. Body image in children and adolescents: where do we go from here? Body Image. 2004;1(1):15–28. doi:10.1016/s1740-1445(03)00008-1
24. Allen KL, Crosby RD, Oddy WH, Byrne SM. Eating disorder symptom trajectories in adolescence: effects of time, participant sex, and early adolescent depressive symptoms. J Eat Disord. 2013;1:32. doi:10.1186/2050-2974-1-32
25. Davison KK, Markey CN, Birch LL. A longitudinal examination of patterns in girls’ weight concerns and body dissatisfaction from ages 5 to 9 years. Int J Eat Disord. 2003;33(3):320–332. doi:10.1002/eat.10142
26. Siegel JA, Ramseyer Winter V, Cook M. “It really presents a struggle for females, especially my little girl”: exploring fathers’ experiences discussing body image with their young daughters. Body Image. 2021;36:84–94. doi:10.1016/j.bodyim.2020.11.001
27. de Vries DA, Vossen HGM, van der Kolk-van der Boom P. Social Media and Body Dissatisfaction: investigating the Attenuating Role of Positive Parent-Adolescent Relationships. J Youth Adolesc. 2019;48(3):527–536. doi:10.1007/s10964-018-0956-9
28. Hart LM, Cornell C, Damiano SR, Paxton SJ. Parents and prevention: a systematic review of interventions involving parents that AIM to prevent body dissatisfaction or eating disorders. Int J Eat Disord. 2015;48(2):157–169. doi:10.1002/eat.22284
29. Duchin O, Marin C, Mora-Plazas M, Villamor E. Maternal body image dissatisfaction and BMI change in school-age children. Public Health Nutr. 2016;19(2):287–292. doi:10.1017/s1368980015001317
30. Webb HJ, Zimmer-Gembeck MJ, Waters AM, Farrell LJ, Nesdale D, Downey G. “Pretty Pressure” From Peers, Parents, and the Media: a Longitudinal Study of Appearance-Based Rejection Sensitivity. J Res Adolesc. 2017;27(4):718–735. doi:10.1111/jora.12310
31. Claydon EA, Zullig KJ, Lilly CL, et al. An exploratory study on the intergenerational transmission of obesity and dieting proneness. Eating Weight Disorders. 2019;24(1):97–105. doi:10.1007/s40519-018-0478-1
32. Webb HJ, Haycraft E. Parental body dissatisfaction and controlling child feeding practices: a prospective study of Australian parent-child dyads. Eat Behav. 2019;32:1–6. doi:10.1016/j.eatbeh.2018.10.002
33. Nicholls D, Chater R, Lask B. Children into DSM don’t go: a comparison of classification systems for eating disorders in childhood and early adolescence. Int J Eat Disord. 2000;28(3):317–324. doi:10.1002/1098-108x(200011)28:3
34. Gruber M, König D, Holzhäuser J, et al. Parental feeding practices and the relationship with parents in female adolescents and young adults with eating disorders: a case control study. PLoS One. 2020;15(11):e0242518. doi:10.1371/journal.pone.0242518
35. Slane JD, Klump KL, McGue M, Iacono WG. Developmental trajectories of disordered eating from early adolescence to young adulthood: a longitudinal study. Int J Eat Disord. 2014;47(7):793–801. doi:10.1002/eat.22329
36. Abebe DS, Lien L, von Soest T. The development of bulimic symptoms from adolescence to young adulthood in females and males: a population-based longitudinal cohort study. Int J Eat Disord. 2012;45(6):737–745. doi:10.1002/eat.20950
37. Marshall WA, Tanner JM. Variations in the pattern of pubertal changes in boys. Arch Dis Child. 1970;45(239):13–23. doi:10.1136/adc.45.239.13
38. Marshall WA, Tanner JM. Variations in pattern of pubertal changes in girls. Arch Dis Child. 1969;44(235):291–303. doi:10.1136/adc.44.235.291
39. Garner DM, Olmsted MP. Scoring the eating disorder inventory. Am J Psychiatry. 1986;143(5):680–681. doi:10.1176/ajp.143.5.aj1435680
40. Lee S, Lee AM, Leung T, Yu H. Psychometric properties of the Eating Disorders Inventory (EDI-1) in a nonclinical Chinese population in Hong Kong. Int J Eat Disord Mar. 1997;21(2):187–194. doi:10.1002/(sici)1098-108x(199703)21:2
41. Helfert S, Warschburger P. The face of appearance-related social pressure: gender, age and body mass variations in peer and parental pressure during adolescence. Child Adolesc Psychiatry Ment Health. 2013;7(1):16. doi:10.1186/1753-2000-7-16
42. Dowson J, Henderson L. The validity of a short version of the Body Shape Questionnaire. Psychiatry Res. 2001;102(3):263–271. doi:10.1016/s0165-1781(01)00254-2
43. Javaras KN, Runfola CD, Thornton LM, et al. Sex- and age-specific incidence of healthcare-register-recorded eating disorders in the complete Swedish 1979-2001 birth cohort. Int J Eat Disord. 2015;48(8):1070–1081. doi:10.1002/eat.22467
44. van Eeden AE, Van Hoeken D, Hoek HW. Incidence, prevalence and mortality of anorexia nervosa and bulimia nervosa. Curr Opin Psychiatry. 2021;34(6):515–524. doi:10.1097/yco.0000000000000739
45. Himmerich H, Hotopf M, Shetty H, et al. Psychiatric comorbidity as a risk factor for the mortality of people with bulimia nervosa. Soc Psychiatry Psychiatr Epidemiol. 2019;54(7):813–821. doi:10.1007/s00127-019-01667-0
46. Pinhas L, Morris A, Crosby RD, Katzman DK. Incidence and age-specific presentation of restrictive eating disorders in children: a Canadian Paediatric Surveillance Program study. Arch Pediatr Adolesc Med. 2011;165(10):895–899. doi:10.1001/archpediatrics.2011.145
47. Thapliyal P, Mitchison D, Mond J, Hay P. Gender and help-seeking for an eating disorder: findings from a general population sample. Eat Weight Disord. 2020;25(1):215–220. doi:10.1007/s40519-018-0555-5
48. Solano-Pinto N, Sevilla-Vera Y, Fernández-Cézar R, Garrido D. Can Parental Body Dissatisfaction Predict That of Children? A Study on Body Dissatisfaction, Body Mass Index, and Desire to Diet in Children Aged 9-11 and Their Families. Front Psychol. 2021;12:650744. doi:10.3389/fpsyg.2021.650744
49. Peisch V, Dale C, Parent J, Burt K. Parent Socialization of Coping and Child Emotion Regulation Abilities: a Longitudinal Examination. Fam Process. 2020;59(4):1722–1736. doi:10.1111/famp.12516
50. López-Pérez B, Pacella D. Interpersonal emotion regulation in children: age, gender, and cross-cultural differences using a serious game. Emotion. 2021;21(1):17–27. doi:10.1037/emo0000690
51. Jankauskiene R, Baceviciene M. Media Pressures, Internalization of Appearance Ideals and Disordered Eating among Adolescent Girls and Boys: testing the Moderating Role of Body Appreciation. Nutrients. 2022;14(11):2227. doi:10.3390/nu14112227
52. Shroff H, Thompson JK. The tripartite influence model of body image and eating disturbance: a replication with adolescent girls. Body Image. 2006;3(1):17–23. doi:10.1016/j.bodyim.2005.10.004
53. Kluck AS. Family influence on disordered eating: the role of body image dissatisfaction. Body Image. 2010;7(1):8–14. doi:10.1016/j.bodyim.2009.09.009
54. Gillison FB, Lorenc AB, Sleddens EF, Williams SL, Atkinson L. Can it be harmful for parents to talk to their child about their weight? A meta-analysis. Prev Med. 2016;93:135–146. doi:10.1016/j.ypmed.2016.10.010
55. Dahill L, Mitchison D, Morrison NMV, et al. Prevalence of Parental Comments on Weight/Shape/Eating amongst Sons and Daughters in an Adolescent Sample. Nutrients. 2021;13(1):158. doi:10.3390/nu13010158
56. Dahill LM, Morrison NMV, Mannan H, et al. Exploring associations between positive and negative valanced parental comments about adolescents’ bodies and eating and eating problems: a community study. J Eat Disord. 2022;10(1):43. doi:10.1186/s40337-022-00561-6
57. Jiménez Flores P, Jiménez Cruz A, Bacardi Gascón M. Body-image dissatisfaction in children and adolescents: a systematic review. Nutr Hosp. 2017;34(2):479–489. doi:10.20960/nh.455
58. McLean SA, Paxton SJ. Body Image in the Context of Eating Disorders. Psychiatr Clin North Am. 2019;42(1):145–156. doi:10.1016/j.psc.2018.10.006
59. Brann LS, Skinner JD. More controlling child-feeding practices are found among parents of boys with an average body mass index compared with parents of boys with a high body mass index. J Am Diet Assoc. 2005;105(9):1411–1416. doi:10.1016/j.jada.2005.06.005
60. Min J, Wang VH, Xue H, Mi J, Wang Y. Maternal perception of child overweight status and its association with weight-related parenting practices, their children’s health behaviours and weight change in China. Public Health Nutr. 2017;20(12):2096–2103. doi:10.1017/s1368980017001033
61. Russell CG, Haszard JJ, Taylor RW, Heath AM, Taylor B, Campbell KJ. Parental feeding practices associated with children’s eating and weight: what are parents of toddlers and preschool children doing? Appetite. 2018;128:120–128. doi:10.1016/j.appet.2018.05.145
62. Allen KL, Gibson LY, McLean NJ, Davis EA, Byrne SM. Maternal and family factors and child eating pathology: risk and protective relationships. J Eat Disord. 2014;2:11. doi:10.1186/2050-2974-2-11
63. Handford CM, Rapee RM, Fardouly J. The influence of maternal modeling on body image concerns and eating disturbances in preadolescent girls. Behav Res Ther. 2018;100:17–23. doi:10.1016/j.brat.2017.11.001
64. Hayes S, Tantleff-Dunn S. Am I too fat to be a princess? Examining the effects of popular children’s media on young girls’ body image. Br J Dev Psychol. 2010;28(Pt 2):413–426. doi:10.1348/026151009x424240
65. Rodgers RF, Wertheim EH, Damiano SR, Gregg KJ, Paxton SJ. A qualitative, prospective study of children’s understanding of weight gain. Br J Dev Psychol. 2019;37(3):369–381. doi:10.1111/bjdp.12279
66. McCabe MP, Ricciardelli LA, Stanford J, Holt K, Keegan S, Miller L. Where is all the pressure coming from? Messages from mothers and teachers about preschool children’s appearance, diet and exercise. Eur Eat Disord Rev. 2007;15(3):221–230. doi:10.1002/erv.717
67. Carlson Jones D. Body image among adolescent girls and boys: a longitudinal study. Dev Psychol. 2004;40(5):823–835. doi:10.1037/0012-1649.40.5.823
68. Laboe AA, Hocking JE, Gondoli DM. Body dissatisfaction and disordered eating within the mother-daughter dyad: an actor-partner interdependence approach. Body Image. 2022;43:25–33. doi:10.1016/j.bodyim.2022.08.004
69. Patrão AL, Almeida MDC, Matos SMA, Chor D, Aquino EML. Gender and psychosocial factors associated with healthy lifestyle in the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil) cohort: a cross-sectional study. BMJ open. 2017;7(8):e015705. doi:10.1136/bmjopen-2016-015705
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



