Back to Journals » Clinical Ophthalmology » Volume 17
Paracentral Acute Middle Maculopathy Following Acute Primary Angle Closure and Acute Primary Angle Closure Glaucoma
Authors Xiao H, Guo N, Li J, Jin L, Liu Y, Lin S, Fang L, Liu X, Zuo C
Received 26 August 2023
Accepted for publication 2 November 2023
Published 20 November 2023 Volume 2023:17 Pages 3513—3523
DOI https://doi.org/10.2147/OPTH.S437075
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Hui Xiao,* Ni Guo,* Junyi Li, Ling Jin, Yuan Liu, Shufen Lin, Lei Fang, Xing Liu, Chengguo Zuo
State Key Laboratory of Ophthalmology, Zhongshan Ophthalmic Center, Sun Yat-Sen University, Guangdong Provincial Key Laboratory of Ophthalmology and Visual Science, Guangdong Provincial Clinical Research Center for Ocular Diseases, Guangzhou, 510060, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xing Liu; Chengguo Zuo, Zhongshan Ophthalmic Center, Sun Yat-sen University, 7 Jinsui Road, Guangzhou, 510000, People’s Republic of China, Email [email protected]; [email protected]
Purpose: To report the prevalence, clinical characteristics and risk factors for paracentral acute middle maculopathy (PAMM) following acute primary angle closure (APAC) and acute primary angle closure glaucoma (APACG).
Methods: This retrospective study consecutively recruited patients diagnosed with APAC or APACG. Based on the spectral domain optical coherence tomography characteristics, PAMM eyes were divided into three stages. Characteristics of different stages such as the time from symptoms to treatment (TST), retinal thickness and BCVA improvement were analyzed. The risk factors of PAMM were evaluated by binary logistic regression models.
Results: A total of 781 eyes of 781 APAC or APACG patients were included, and PAMM was found in 22 (2.9%) of them. Stage III eyes had a significantly longer TST than stage I eyes (P = 0.008) while exhibiting significantly thinner retinal thicknesses (P < 0.0001). The BCVA improvement was significantly worse in the eyes treated in stage III than in those treated in stage I (P = 0.008). Older age, longer axial length and without type 2 diabetes were associated with a lower risk of incident PAMM (OR = 0.95, P = 0.028; OR = 0.52, P = 0.019; OR = 3.92, P = 0.022).
Conclusion: PAMM can be secondary to APAC or APACG at a rate of 2.9%. Different visual outcomes were observed in patients who received the intervention at different stages of PAMM. Younger patients with a shorter axial length and type 2 diabetes were found to be more susceptible to PAMM.
Keywords: paracentral acute middle maculopathy, acute primary angle closure, acute primary angle closure glaucoma, risk factors, spectral domain optical coherence tomography
Introduction
Acute primary angle closure (APAC) and acute primary angle closure glaucoma (APACG) are ocular emergencies that are vision-threatening diseases that can lead to blindness and require urgent treatment.1 Sudden blockage of the angle results in a rapid elevation of intraocular pressure (IOP) to a critical level, leading to retinal ischemia.2 Numerous animal studies have shown that despite physiological autoregulation, the foveal microcirculation is significantly affected by elevated IOP, particularly within the deep capillary plexus (DCP).3,4
Ischemia of the intermediate capillary plexus (ICP) and DCP has been shown to be related to paracentral acute middle maculopathy (PAMM).5 In 2013, Sarraf et al6 reported the discovery of PAMM, which is characterized by a hyperreflective band located in the inner nuclear layer (INL) on spectral-domain optical coherence tomography (SD-OCT) and can lead to permanent atrophy of the INL. Most previous studies on PAMM were case reports and mainly focused on retinal vascular diseases, such as retinal artery occlusion (RAO) and retinal vein occlusion (RVO).7,8 PAMM can also be secondary to intraocular surgery, such as phacoemulsification, vitrectomy and small incision lenticule extraction surgery (SMILE).9–11 Moreover, some studies have pointed out the systemic causes of PAMM, including viral infections, vaccinations, pregnancy and medications (such as oral isotretinoin, contraceptives, amphetamines, etc.).5,12–14 However, there have been a few reports of PAMM occurring in association with APAC or APACG.15
This study aims to report the prevalence of PAMM following APAC or APACG and to investigate its characteristics and risk factors by retrospectively analyzing the clinical data of patients.
Methods
Study Design and Inclusion Criteria
This study was a hospital-based retrospective, consecutive case study. We were committed to protecting the confidentiality of patient data; informed consent was waived by the Institutional Review Board of the Zhongshan Ophthalmic Center, Sun Yat-sen University, because the data was collected retrospectively. Patients diagnosed with APAC or APACG were consecutively recruited from January 2019 to December 2021 at Zhongshan Ophthalmic Center. All eligible subjects underwent spectral-domain OCT examination.
The diagnostic criteria for APAC were as follows:16 (1) had at least 2 of the following symptoms: ocular or periocular pain, nausea and/or vomiting, and prior episodes of intermittent vision blurring with haloes; (2) Presenting with an IOP level exceeding 21 mmHg and at least 3 of the following signs: conjunctival injection, corneal epithelial edema, mid-dilated unresponsive pupil and shallow anterior chamber. Similarly, APACG was defined as APAC with glaucomatous optic neuropathy (GON) [defined as a vertical cup/disc (C/D) ratio ≥0.7, or C/D asymmetry of ≥0.2 between the eyes, or focal optic disc rim thinning]. If both eyes met the eligibility criteria, the right eye was chosen.
Exclusion criteria included the following: (1) Patients with secondary angle closure conditions, including but not limited to lens-induced glaucoma, neovascular glaucoma, or uveitis; (2) Eyes with low-quality SD-OCT images due to medium cloudiness; (3) Eyes that were affected by other retinal diseases, such as diabetic retinopathy, old retinal vascular occlusion, retinal detachment, and macular disease;5 and (4) Eyes with a documented history of ocular surgery or trauma within the past 6 months.
Data Collection
Demographic and clinical information, including age, sex, the highest recorded IOP (mmHg), time from symptoms to treatment (TST, days), baseline best-corrected visual acuity (BCVA), final BCVA (obtained at a follow-up time of 3 months or more), body mass, body height, systolic blood pressure (SBP), diastolic blood pressure (DBP) and laboratory data, were obtained from an electronic medical record system or follow-up calls to patients. The laboratory data included serum glucose, total cholesterol and triglycerides. Body mass index (BMI) is calculated by dividing body mass by the square of body height.
For all APAC and APACG subjects, the acute attacks were managed by initial topical and oral glaucoma therapy, followed by peripheral iridotomy, lens extraction or trabeculectomy. All patients underwent comprehensive examinations, including BCVA, IOP measurements, slit-lamp evaluation, color fundus photography, axial length, central anterior chamber depth (ACD), gonioscopy and SD-OCT examination. Visual acuity was assessed by the Snellen chart and converted into a logarithm of the minimum angle of resolution (logMAR) for statistical analysis. Goldmann applanation tonometry was used to measure IOP. Axial length (AL) was determined using A-scan ultrasonography (model US-1800, Nidek). ACD was measured with ultrasound biomicroscopy (UBM, model SW-3200 L; Tianjin Suowei Electronic Technology Co., Ltd., Tianjin, China). Gonioscopy was performed with a Goldmann 2-mirror lens (Haag-Streit, UK) by glaucoma specialists. The mean retinal nerve fiber layer thickness (mRNFLT) and subfoveal choroidal thickness (SFCT) were measured with SD-OCT.
Spectralis SD-OCT system (Heidelberg Engineering, Heidelberg, Germany, UK) with enhanced depth imaging and eye tracking was used to acquire OCT images by a well-trained ophthalmologist (HX). A line scan was performed across the center of the lesion, generating 100 averaged B-scans per image. OCT images of both the macula and optic nerve head were obtained during the follow-up after the acute episode.
Outcome Measures
PAMM was diagnosed by a hyperreflective band located at the INL or INL thinning on the SD-OCT images.6 Similar to RAO, APAC/APACG patients’ inner retina experienced three pathophysiological processes of edema, edema regression and atrophy in the state of high intraocular pressure-induced retinal ischemia.17 Different pathophysiological stages have unique retinal morphological characteristics which are manifested on SD-OCT. Stage I (edema): single or multiple hyperreflective plaque-like lesions involving the INL; different scanning angles can also present hyperreflective lesions at the junction of the INL and IPL as well as at the junction of the INL and outer plexiform layer (OPL). The lesion produced a corresponding shadow over the outer retinal layers. Stage II (edema resolution) had a weaker hyperreflective band than stage I (edema), accompanied by corresponding atrophy and thinning, which was more obvious in OPL, and the corresponding shadow of the outer retina had also resolved. Stage III (atrophy) was defined as the resolution of the hyperreflective lesions, followed by thinning of the INL and irregular, attenuated OPL (Figure 1).
For the parafoveal region, the retinal thickness at the thickest part of the stage I (edema) lesion and the thinnest part of the stage II (edema resolution) and III (atrophy) lesions were measured manually by ImageJ software (ImageJ Software Inc., MD, USA). The retinal thickness measurements included the entire retina (the inner limiting membrane to the outer boundary of the retinal pigment epithelium) and the inner retina (the inner limiting membrane to the OPL) thickness. The parafoveal region was defined as an annulus centered at the fovea, with an inner diameter of 1 mm and an outer diameter of 3 mm.18 In eyes showing multiple lesions, each lesion was measured and averaged. Two of these PAMM lesions were located in the peripheral region, which was characterized as an annulus, centered at the fovea, with an inner diameter of 3 mm and an outer diameter of 6 mm.
All manual measurements were performed by a trained investigator (NG), who was masked to the clinical characteristics of the patients. After a duration of more than 14 days, 10 randomly selected SD-OCT images of PAMM were measured twice by the same investigator for the intraclass correlation coefficients (ICCs). All SD-OCT images were independently evaluated by two glaucoma specialists (CZ and HX), and inconsistencies between the two doctors were determined by a senior glaucoma expert (XL).
Statistical Analysis
Statistical analysis was conducted with SPSS version 26.0 (SPSS Incorporation, Chicago, Illinois, USA). Continuous variables were presented as the mean ± standard deviation (SD) with the range and evaluated using the t test. Group differences in demographic characteristics were evaluated using the independent sample T test, Mann‒Whitney U-test or chi-square and Fisher’s exact tests. The intergroup analysis of PAMM eyes was performed by one-way ANOVA or Kruskal–Wallis H-test according to whether the variables conformed to a normal distribution. Bonferroni correction was used for multiple comparisons. For unequal variances, the Welch test and Tambane’s T2 were used. Age, gender and the variables with a P value < 0.10 from the univariable analysis were entered into binary logistic regression Model 1. Age, sex and the variables from the Model 1 analysis with a P value < 0.10 were included in binary logistic regression Model 2 for the multivariable analysis. The intraclass correlation coefficient (ICC) was used to assess intraobserver reproducibility. Results with P < 0.05 were considered significantly.
Results
The study included a total of 781 eyes from 781 patients diagnosed with APAC or APACG, with the majority of cases being female patients (74.1%). The average age at onset of APAC or APACG was 62.07 ± 8.91 years. Their baseline demographics, ocular findings and systemic associations are outlined in Table 1 and Table 2. Paracentral acute middle maculopathy was present in 22 of the 781 patients (2.9%) with APAC or APACG. The mean AL in the PAMM group was significantly shorter than that in the control group (21.89 ± 0.78 mm vs 22.39 ± 0.79 mm, 95% confidence Interval 0.161–0.834, P = 0.004).
 |
Table 1 Demographic Characteristics and Ocular Findings of Patients with APAC or APACG (N = 781) |
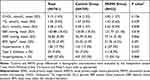 |
Table 2 Systemic Associations of Patients with APAC or APACG (N = 781) |
Characteristics of PAMM in APAC or APACG Patients
Twenty-two patients (22 eyes) with PAMM in APAC or APACG were observed, with a female predominance of 81.8% and a mean age of 57 years (range 25–74). All PAMM eyes in APAC or APACG patients were unilaterally affected.
During the initial examination, among the 22 eyes with PAMM, 11 eyes (50%) were classified as stage I, 5 eyes (22.7%) as stage II, and 6 eyes (27.3%) as stage III. The median TST for stages I, II and III was 1, 3 and 38 days, respectively. Stage III had a significantly longer TST compared to stage I (P = 0.008); no significant difference was found in TST between the other stages (Figure 2). The inner retinal thickness was significantly thicker in stage I eyes compared to stage II and III eyes (all P < 0.0001). Likewise, the full retinal thickness in stage I eyes was significantly thicker than that in stage II and stage III eyes (P < 0.001 and P < 0.0001, respectively). No significant difference was observed in the mean highest recorded IOPs between eyes in stages I, II and III (P = 0.225), with values of 52.1 ± 9.0, 53.6 ± 11.2 and 58.4 ± 9.4, respectively. BCVAs between the 3 stages were compared, and no significant differences were found in the baseline BCVA or final BCVA (Table 3). However, statistical significance was found in BCVA improvement. The BCVA improvement was significantly better in eyes treated in stage I than in those treated in stage III (a mean of 4 lines of vision improvement vs a mean of 0.67 lines of vision worsening, P = 0.008; Figure 3).
 |
Table 3 BCVA Comparison Between the Three Stages |
Spearman or Pearson correlation analysis revealed significant positive correlations between inner retinal thickness and full retinal thickness with BCVA improvement (r = 0.498, P = 0.018; r = 0.504, P = 0.017), while TST showed a significant negative correlation with BCVA improvement (r = −0.513, P = 0.015; Table 4).
 |
Table 4 The Pearson or Spearman Correlations Between BCVA and Other Factors in PAMM Eyes |
Case Report
Figure 4 shows the evolution of PAMM lesions in an APACG patient by SD-OCT.
Possible Risk Factors for PAMM in APAC or APACG Patients
The results of the univariate analysis showed that age, AL, SFCT and type 2 diabetes were potential risk factors for PAMM (P < 0.10; Figure 5) following APAC or APACG. In the multivariate regression analysis models, after adjusting for age and sex (Model 1), age, AL and type 2 diabetes were significantly correlated with PAMM (P = 0.009, 0.022 and 0.025, respectively). After further adjustment for other confounding factors (Model 2), older age and longer AL were associated with a lower risk of incident PAMM (OR = 0.95 per year, P = 0.028; OR = 0.52 per mm, P = 0.019, respectively). Type 2 diabetes was found to have a 3.92 times higher risk of developing PAMM in the APAC or APACG (P = 0.022).
Reproducibility Analysis of the Manual Measurements
Inner and full retinal thickness exhibited high intraclass correlation coefficients of 0.990 and 0.976, respectively (both P < 0.001), indicating excellent agreement between measurements.
Discussion
Findings from this study revealed that PAMM can be secondary to APAC or APACG with a prevalence of 2.9% (22/781). Based on our observations, we described PAMM lesions based on morphological characteristics of the 3 pathophysiological stages and found that different pathophysiological stages had different visual prognoses. Moreover, we found that age, AL and type 2 diabetes mellitus were significantly associated with PAMM.
PAMM was commonly reported in retinal vascular diseases: 22% (9/40) in RAO,7 5.2% (25/484) in nonischemic central retinal vein occlusion.8 Unlike vascular occlusions in retinal vascular disease, PAMM may be caused by acute IOP elevation-induced retinal ischemia in APAC or APACG.
The SD-OCT observations offered detailed information on the 3 stages of PAMM lesions. For patients in the edema stage, the IOP increases sharply and the medial retinal circulation in the parafoveal region is prone to intracellular edema caused by ischemia and hypoxia, thus resulting in a high reflection band of the INL on SD-OCT (stage I). For patients in the edema resolution stage, ischemic hypoxia was relieved for a short time, and their edema began to subside. The return of blood to the tissue, however, leads to the production of a variety of oxidants and free radicals, which ultimately lead to retinal cell necrosis.19 This was presented as distinctly thinning OPL around the lesion accompanied by weaker hyperreflective bands of the INL (stage II). For atrophy stage patients, ischemic hypoxia was not relieved for a short time, and the compensatory mechanism of cells would be exceeded or would completely fail, resulting in the death of massive swollen cells and the regression of edema.20,21 Therefore, ischemic infarction occurred at the corresponding site, with loss of cells and DCP, as manifested by severe thinning INL on the SD-OCT images (stage III).
During the follow-up, we found that different PAMM stages had different degrees of BCVA improvement. The patients who received the intervention in stage III (atrophy) had worse vision recovery than those who received the intervention in stage I (edema) (P = 0.008). It can also be intuitively seen that once atrophy formed, it is too late for irreversible anatomic damage to lead to visual improvement. Moreover, we found that the atrophy stage of PAMM patients had a significantly longer TST than the edema stage. TST was a confirmed risk factor for blindness after APAC according to a multicenter retrospective case study.22 Our patients with a longer TST were more likely to experience multiple APAC events and have more ischemic hypoxia, which can lead to thinning of the retina.23 The measurement results revealed that the atrophy stage had the thinnest inner and full retinal thickness. This might be the anatomical basis of worse BCVA. In a previous study, retinal thickness was documented to be an important predictor of vision.24,25 Additionally, we also found a significantly positive correlation between BCVA improvement and retinal thickness in our correlation analysis. Therefore, the three pathophysiological stages indicated different degrees of visual impairment in the current study by PAMM. Certainly, there are other possible factors that could influence visual outcomes as well.26,27 Some previous studies divided PAMM into 2 stages mainly according to the disease course.5,6 However, the exact onset time of PAMM in APAC/APACG patients is difficult to determine. And similar to RAO, APAC/APACG patients’ inner retina experienced three pathophysiological processes of edema, edema regression and atrophy in the state of high intraocular pressure-induced retinal ischemia.17 In addition, different pathophysiological processes demonstrated unique morphological characteristics, which related to different visual prognosis. Therefore, in the study, we described PAMM lesions based on morphological characteristics of the 3 pathophysiological processes in APAC/APACG patients.
A lower risk of PAMM was observed with increasing age and longer AL, based on the study’s findings; in other words, younger age and shorter AL were risk factors for PAMM. Previous studies pointed out that patients with PAMM tend to be younger,8,10 which was in accordance with our findings. Vasospasm is more frequently observed in younger people and is generally located within the microcirculation,28,29 resulting in retinal ischemia, while ischemia itself can cause spasm, creating a vicious cycle. Additionally, Lin et al30 found that younger primary angle-closure disease patients had a shorter AL, and a shorter AL was also confirmed as an independent risk factor for PAMM in this study.
Anatomically, the central retinal blood vessels pass through the scleral canal into the eyeball and finally into the lamina cribrosa. In patients with a shorter AL, the scleral canal is smaller; the lamina cribrosa space is narrower; and the retinal vessels are easier to compress.31 Therefore, the retinal capillary network supplying the INL is more vulnerable to ischemia when the perfusion pressure of the main trunk decreases. In addition, studies have shown that a longer AL reduces retinal function and oxygen consumption,32 implying that relatively fewer ischemic and hypoxic events occur in patients with a longer AL during acute elevation of IOP and retinal hypoperfusion.
In our study, patients with type 2 diabetes were found to have a 3.92 times higher risk of developing PAMM in the APAC or APACG. PAMM has previously been reported in non-proliferative diabetic retinopathy (NPDR).33 Thus, our study excluded patients with diabetic retinopathy (DR) to rule out its potential role. Patients with type 2 diabetes may have a variety of vascular insults, such as embolization, inflammation, and endothelial cell damage, which can lead to precapillary retinal arteriole occlusion.34 From a hemodynamic perspective, there is evidence that retinal perfusion is reduced in the early stages of diabetes.35 Another common phenomenon is endothelial-leukocyte interaction, which prevents leukocytes from moving smoothly through the capillary bed, resulting in capillary obstruction.36 A decrease in retinal blood flow may not only promote this effect but may also affect oxygen delivery,37 leading to tissue hypoxia early in the disease.38 A recent prospective study monitored a cohort of patients with type 2 diabetes without DR and illustrated a significant decrease in parafoveal microvascular perfusion.39 These changes may account for the predisposition of PAMM following APAC or APACG in type 2 diabetic patients without DR.
The study had several limitations, such as its retrospective, hospital-based design, and relatively small number of PAMM cases despite a large sample size. The findings of this study need to be confirmed through a large-scale, longitudinal, and prospective study involving multiple centers.
Conclusion
We reported that PAMM can occur following APAC or APACG with a rate of 2.9%. SD-OCT scans revealed that PAMM lesions had three pathophysiological stages: edema, edema resolution, and atrophy. The patients who received the intervention at different PAMM stages indicated different visual outcomes. Moreover, younger age, shorter AL and type 2 diabetes were found to have a higher risk for PAMM in the APAC or APACG.
Acknowledgments
We would like to acknowledge Dingqiao Wang, Huanyang Shi, Zhihong Huang and Shaoyang Zheng who are the research group members for their guidance and support in completing this project, and all the participants who made our study possible.
Ethics Approval
Approval for this study was obtained from the Institutional Review Board of the Zhongshan Ophthalmic Center, Sun Yat-sen University (Approval number: 2022KYPJ250) and the study followed the principles of the Declaration of Helsinki. Informed consent from patients in the study was waived because the data were collected retrospectively. We only analyzed patient case data without any intervention or additional examinations. All patient data were protected and kept confidential by the researchers.
Funding
This study was supported by the National Natural Science Foundation of China grants 81970808, and by Natural Science Foundation of Guangdong Province grants 2022A1515011469.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Jonas JB, Aung T, Bourne RR, et al. Glaucoma. Lancet. 2017;390(10108):2183–2193. doi:10.1016/S0140-6736(17)31469-1
2. Sonty S, Schwartz B. Vascular accidents in acute angle closure glaucoma. Ophthalmology. 1981;88(3):225–228. doi:10.1016/S0161-6420(81)35046-5
3. Choi M, Kim SW, Vu TQA, et al. Analysis of microvasculature in nonhuman primate macula with acute elevated intraocular pressure using optical coherence tomography angiography. Invest Ophthalmol Vis Sci. 2021;62(15):18. doi:10.1167/iovs.62.15.18
4. Cheung CMG, Teo KYC, Tun SBB, et al. Differential reperfusion patterns in retinal vascular plexuses following increase in intraocular pressure an OCT angiography study. Sci Rep. 2020;10(1):16505. doi:10.1038/s41598-020-73585-0
5. Rahimy E, Kuehlewein L, Sadda SR, et al. Paracentral acute middle maculopathy: what we knew then and what we know now. Retina. 2015;35(10):1921–1930. doi:10.1097/IAE.0000000000000785
6. Sarraf D, Rahimy E, Fawzi AA, et al. Paracentral acute middle maculopathy: a new variant of acute macular neuroretinopathy associated with retinal capillary ischemia. JAMA Ophthalmol. 2013;131(10):1275–1287. doi:10.1001/jamaophthalmol.2013.4056
7. Yu S, Pang CE, Gong Y, et al. The spectrum of superficial and deep capillary ischemia in retinal artery occlusion. Am J Ophthalmol. 2015;159(1):53–63.e1–2. doi:10.1016/j.ajo.2014.09.027
8. Rahimy E, Sarraf D, Dollin ML, et al. Paracentral acute middle maculopathy in nonischemic central retinal vein occlusion. Am J Ophthalmol. 2014;158(2):372–380.e1. doi:10.1016/j.ajo.2014.04.024
9. Groeneveld E. Paracentral acute middle maculopathy as a finding in patients with severe vision loss following phacoemulsification cataract surgery: comment. Clin Experiment Ophthalmol. 2018;46(5):576–577. doi:10.1111/ceo.13117
10. Nakashima H, Iwama Y, Tanioka K, et al. Paracentral acute middle maculopathy following vitrectomy for proliferative diabetic retinopathy: incidence, risk factors, and clinical characteristics. Ophthalmology. 2018;125(12):1929–1936. doi:10.1016/j.ophtha.2018.07.006
11. Meng LH, Zhao XY, Yu WH, et al. A case of paracentral acute middle maculopathy after small incision lenticule extraction surgery. Int J Ophthalmol. 2022;15(1):169–171. doi:10.18240/ijo.2022.01.25
12. Elshafie MA, Radi AM, Abdelmawla MO, et al. Paracentral acute middle maculopathy after isotretinoin. Egypt Retina J. 2022;9(2):31. doi:10.4103/erj.erj_2_23
13. Yeo S, Kim H, Lee J, et al. Retinal vascular occlusions in COVID-19 infection and vaccination: a literature review. Graefes Arch Clin Exp Ophthalmol. 2023;261(7):1793–1808. doi:10.1007/s00417-022-05953-7
14. Scott RA, Bhat N, Bindiganavile SH, et al. Paracentral acute middle maculopathy in pregnancy. J Neuroophthalmol. 2022;42(1):e440–e442. doi:10.1097/WNO.0000000000001307
15. Li J, Li YX, Zhao J, et al. Paracentral acute middle maculopathy secondary to high intraocular pressure: a case report. Int J Ophthalmol. 2022;15(10):1723–1725. doi:10.18240/ijo.2022.10.25
16. Aung T, Friedman DS, Chew PT, et al. Long-term outcomes in asians after acute primary angle closure. Ophthalmology. 2004;111(8):1464–1469. doi:10.1016/j.ophtha.2003.12.061
17. Ritter M, Sacu S, Deák GG, et al. In vivo identification of alteration of inner neurosensory layers in branch retinal artery occlusion. Br J Ophthalmol. 2012;96(2):201–207. doi:10.1136/bjo.2010.198937
18. Ito H, Ito Y, Kataoka K, et al. Association between retinal layer thickness and perfusion status in extramacular areas in diabetic retinopathy. Am J Ophthalmol. 2020;215:25–36. doi:10.1016/j.ajo.2020.03.019
19. Nemiroff J, Kuehlewein L, Rahimy E, et al. Assessing deep retinal capillary ischemia in paracentral acute middle maculopathy by optical coherence tomography angiography. Am J Ophthalmol. 2016;162:121–132.e1. doi:10.1016/j.ajo.2015.10.026
20. Szabó C. Mechanisms of cell necrosis. Crit Care Med. 2005;33(12 Suppl):S530–4. doi:10.1097/01.CCM.0000187002.88999.CF
21. Liang D, Bhatta S, Gerzanich V, et al. Cytotoxic edema: mechanisms of pathological cell swelling. Neurosurg Focus. 2007;22(5):E2. doi:10.3171/foc.2007.22.5.3
22. Li S, Tang G, Fan SJ, et al. Factors associated with blindness three months following treatment for acute primary angle glaucoma. Br J Ophthalmol. 2021;105(4):502–506. doi:10.1136/bjophthalmol-2020-316259
23. Liu X, Li M, Zhong YM, et al. Damage patterns of retinal nerve fiber layer in acute and chronic intraocular pressure elevation in primary angle closure glaucoma. Int J Ophthalmol. 2010;3(2):152–157. doi:10.3980/j.issn.2222-3959.2010.02.14
24. Sandberg MA, Brockhurst RJ, Gaudio AR, et al. The association between visual acuity and central retinal thickness in retinitis pigmentosa. Invest Ophthalmol Vis Sci. 2005;46(9):3349–3354. doi:10.1167/iovs.04-1383
25. Lee SS, Lingham G, Alonso-Caneiro D, et al. Macular thickness profile and its association with best-corrected visual acuity in healthy young adults. Transl Vis Sci Technol. 2021;10(3):8. doi:10.1167/tvst.10.3.8
26. Lee JW, Wong BK, Yick DW, et al. Primary acute angle closure: long-term clinical outcomes over a 10-year period in the Chinese population. Int Ophthalmol. 2014;34(2):165–169. doi:10.1007/s10792-013-9806-7
27. Andreatta W, Elaroud I, Nightingale P, et al. Long-term outcomes after acute primary angle closure in a White Caucasian population. BMC Ophthalmol. 2015;15:108. doi:10.1186/s12886-015-0100-5
28. Flammer J, Pache M, Resink T. Vasospasm, its role in the pathogenesis of diseases with particular reference to the eye. Prog Retin Eye Res. 2001;20(3):319–349. doi:10.1016/s1350-9462(00)00028-8
29. Magge SN, Chen HI, Ramakrishna R, et al. Association of a younger age with an increased risk of angiographic and symptomatic vasospasms following subarachnoid hemorrhage. J Neurosurg. 2010;112(6):1208–1215. doi:10.3171/2009.9.JNS081670
30. Lin S, Zuo C, Liu Y, et al. Ocular biometry of primary angle-closure disease in younger patients. Front Med. 2021;8:772578. doi:10.3389/fmed.2021.772578
31. Shi A, Chen S, Choi M, Kim S-W. 眼球轴长与视网膜中央静脉阻塞关系的探讨 [Relationship between ocular axial length and central retinal vein occlusion]. Zhonghua Yan Ke Za Zhi. 2001;37(5):373–374. Chinese.
32. Man RE, Lamoureux EL, Taouk Y, et al. Axial length, retinal function, and oxygen consumption: a potential mechanism for a lower risk of diabetic retinopathy in longer eyes. Invest Ophthalmol Vis Sci. 2013;54(12):7691–7698. doi:10.1167/iovs.13-12412
33. Yu S, Wang F, Pang CE, et al. Multimodal imaging findings in retinal deep capillary ischemia. Retina. 2014;34(4):636–646. doi:10.1097/IAE.0000000000000048
34. Kim JS, Maheshwary AS, Bartsch DU, et al. The microperimetry of resolved cotton-wool spots in eyes of patients with hypertension and diabetes mellitus. Arch Ophthalmol. 2011;129(7):879–884. doi:10.1001/archophthalmol.2011.51
35. Curtis TM, Gardiner TA, Stitt AW. Microvascular lesions of diabetic retinopathy: clues towards understanding pathogenesis? Eye. 2009;23(7):1496–1508. doi:10.1038/eye.2009.108
36. Joussen AM, Murata T, Tsujikawa A, et al. Leukocyte-mediated endothelial cell injury and death in the diabetic retina. Am J Pathol. 2001;158(1):147–152. doi:10.1016/S0002-9440(10)63952-1
37. Alder VA, Su EN, Yu DY, et al. Diabetic retinopathy: early functional changes. Clin Exp Pharmacol Physiol. 1997;24(9–10):785–788. doi:10.1111/j.1440-1681.1997.tb02133.x
38. Dean FM, Arden GB, Dornhorst A. Partial reversal of protan and tritan colour defects with inhaled oxygen in insulin dependent diabetic subjects. Br J Ophthalmol. 1997;81(1):27–30. doi:10.1136/bjo.81.1.27
39. Aschauer J, Pollreisz A, Karst S, et al. Longitudinal analysis of microvascular perfusion and neurodegenerative changes in early type 2 diabetic retinal disease. Br J Ophthalmol. 2022;106(4):528–533. doi:10.1136/bjophthalmol-2020-317322
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.





