Back to Journals » Therapeutics and Clinical Risk Management » Volume 15
Overnight inpatient admission and revisit rates after pediatric adenotonsillectomy
Authors Alsuhebani M , Walia H, Miller R , Elmaraghy C, Tumin D, Tobias JD , Raman VT
Received 25 August 2018
Accepted for publication 31 March 2019
Published 6 June 2019 Volume 2019:15 Pages 689—699
DOI https://doi.org/10.2147/TCRM.S185193
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Garry Walsh
Mohammad Alsuhebani,1 Hina Walia,1 Rebecca Miller,1 Charles Elmaraghy,2,3 Dmitry Tumin,1 Joseph D Tobias,1,4 Vidya T Raman1,4
1Department of Anesthesiology & Pain Medicine, Nationwide Children’s Hospital, Columbus, OH, USA; 2Department of Pediatric Otolaryngology, Nationwide Children’s Hospital, Columbus, OH, USA; 3Department of Ear, Nose & Throat Surgery, The Ohio State University, Columbus, OH, USA; 4Department of Anesthesiology, The Ohio State University, Columbus, OH, USA
Objective: Overnight admission may be necessary following adenotonsillectomy (T&A) in pediatric patients. This practice may reduce unplanned revisits following hospital discharge.
Study design: Retrospective cohort study.
Subjects: Children from the PHIS database.
Methods: T&A performed in children during the years 2007–2015 were identified in the Pediatric Health Information System. The primary outcome was 7-day, all-cause readmission or emergency department (ED) revisit. Secondary analysis examined specific revisit types and 30-day revisits. The primary exposure was each institution’s annual rate of overnight stay after T&A.
Results: The analysis included 411,876 procedures at 48 hospitals. Hospitals’ annual rates of overnight stay following T&A ranged from 3% to 100%, and 7-day revisit rates varied from 0% to 15%. The percentage or rate of 7-day revisits did not differ based on the use of overnight stay following T&A. At hospitals with higher overnight admission rates after T&A, 7-day revisits were more likely to take the form of inpatient admission rather than an ED visit.
Conclusions: The current study confirms that pediatric hospitals vary widely in inpatient admission practices following T&A. This variation is not associated with differences in revisit rates at 7 and 30 days related to any cause. Although no mortality was noted in the current study, caution is suggested when deciding on the disposition of patients with comorbid conditions as risks related to various patients, anesthetic, and surgical-related issues exist. Risk stratification with appropriate identification of patients requiring overnight stay may be the most important for preventing acute care revisits after T&A.
Keywords: tonsillectomy, emergency room visit, post-tonsillectomy hemorrhage, overnight admission, surgical complication
Introduction
Adenotonsillectomy (T&A) is one of the most commonly performed surgical procedures in children in the United States (US). It is typically performed to treat symptoms of sleep-disordered breathing (SDB), obstructive sleep apnea (OSA), or recurrent tonsillitis.1–3 Although several studies have expressed concern regarding the safety of performing T&A as an outpatient procedure in children with SDB or OSA, these procedures continue to be performed in the ambulatory setting.4–6 The most common complications following pediatric T&A include hemorrhage and respiratory complications, which are estimated to occur in 3% and 9% of cases, respectively.7 In 2011, the American Academy of Otolaryngology-Head and Neck Surgery (AAO-HNS) published a practice guideline recommending that children with complicated medical histories should undergo inpatient rather than outpatient T&A.3 Subsequent research has affirmed the need for overnight monitoring of patients deemed to be at high risk of complications, to prevent morbidity and even mortality after T&A in children with OSA or SDB.8
The adoption of AAO-HNS practice guidelines has been inconsistent across physicians and hospitals, and admission practices after T&A continue to vary widely across institutions.9,10 Meanwhile, revisit rates after pediatric tonsillectomy also show marked variation across institutions, ranging from 3% to 13%.9 Recently, our group has shown that early (7-day) revisits after T&A were reduced in children who received extended postoperative monitoring.11 However, it remains unclear whether institutional practices favoring overnight stay after T&A impact the number of hospital revisits for any reason. Our current study examines whether greater use of overnight stay after T&A is associated with a lower risk of all-cause revisits and readmissions after T&A. We hypothesized that the likelihood of revisits would be lower in hospitals performing a higher proportion of T&A with an overnight stay (as opposed to ambulatory procedures). A secondary aim was to evaluate the rate of overnight admission across all hospitals during the study time period based on the current practice recommendations from the AAO-HNS and the recent anecdotal reports of mortality following T&A.3,8
Methods
This retrospective study was approved by the Institutional Review Board (IRB) of Nationwide Children’s Hospital (IRB15-00264). The IRB at NCH is a hospital-based, non-University affiliated IRB that reviews and oversees all clinical research performed by members of the faculty. As a retrospective study, the need for informed consent was deemed unnecessary. The Data Resource Center at our institution extracted data from the Pediatric Health Information System (PHIS) on T&A performed among children ≤18 years of age between 2007 and 2015. The PHIS is an anonymized database containing administrative and billing data from over 40 freestanding children’s hospitals affiliated with the Children’s Hospital Association.9 All discharges from member hospitals are included in the database, and data collected include demographic information, diagnosis and procedure codes, service locations, and charges mapped to clinical transaction codes.9 Patients were included in this analysis if they underwent T&A on the day of admission to a participating hospital, and if they were discharged on the same day (outpatient) or 1 or more days after the procedure (overnight stay). Patients were excluded from multivariable analysis if they were missing data on study covariates. The primary outcome was all-cause inpatient readmission or revisit to an emergency department (ED) within 7 days of discharge. Inpatient readmissions or acute care revisits within 7 days are considered a key measure of complications occurring early after hospital discharge. Secondary outcomes included specific revisit types (ED visit vs readmission) and 30-day revisit outcomes.12,13 Additionally, we tracked the percentage of inpatient admission following T&A over the study period.
In the descriptive analysis, we characterized types and reasons for revisits at each time point using counts with percentages. The primary exposure was each institution’s annual rate of overnight stay after T&A, categorized according to quartiles of institutions (≤20%, 21–35%, 36–60%, or >60% of T&A performed with overnight stay). Individual-level covariates included age, gender, race, severity levels classified by the All Patient-Refined Diagnosis Related Groups system, and comorbidities, including presence of OSA or SDB symptoms, asthma, diabetes, and obesity, noted at the time of surgery, as identified from International Classification of Diseases 9th revision (ICD-9) or 10th revision (ICD-10) codes.
For descriptive analysis, hospitals’ revisit rates and other study data were compared according to institutional admission practice over the entire study period (percent of T&A with overnight stay). Categorical data were analyzed using Chi-square tests, and continuous data were analyzed using ANOVA. To evaluate the association between institutional practice and individual patient’s revisit risk while accounting for the clustering of patients within hospitals, we used mixed effects logistic regression adjusted for the institutional use of overnight stay, annual volume of T&A procedures (a proxy for hospital size), individual admission status after T&A (overnight stay vs outpatient), and covariates listed above. To disambiguate among outcomes of ED revisit and readmission, we created a secondary outcome with mutually exclusive categories of 1) no ED visit or readmission, 2) at least one ED visit, but no readmission, and 3) any readmission, with or without ED visits. This secondary outcome was analyzed using a mixed-effects multinomial logistic regression model, which generated pairwise comparisons among each of the three outcome categories.14 Analyses were repeated for 30-day outcomes. To examine whether our multivariable models were influenced by including both institutional rates of overnight stay and individual admission status, analyses were also repeated while omitting individual admission status. Data were analyzed using Stata/IC 14.2 (College Station, TX: StataCorp, LP), and two-tailed p<0.05 was considered statistically significant.
Results
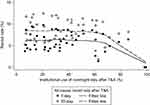
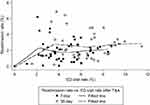
There were 411,876 patients from 48 hospitals meeting inclusion criteria, of whom 344,525 had complete data for multivariable analysis. Hospitals’ annual T&A volume (among cases meeting inclusion criteria) ranged from 7 to 3,143 (1,002±758). Annual rates of overnight stay after T&A ranged from 3% to 100% (44% ±31%). Annual revisit rates at 7 days after discharge ranged from 0% to 15% (5% ±3%), and revisit rates at 30 days after discharge ranged from 0% to 7% (mean: 7% ±4%). Overall, 26,908 (7%) patients had a 7-day revisit, of which 18,656 (69%) were ED visits and 8,252 (31%) were readmissions. Of these readmissions, 862 (10%) were initially seen in the ED. Among the 36,234 (9%) patients who had a 30-day revisit, 25,003 (69%) were ED visits and 11,231 (31%) were readmissions. Of these readmissions, 1,582 (14%) were initially seen in the ED. Figure 1 illustrates the institutions’ use of overnight stay and revisit rates after T&A over the entire study period. There was no trend of decreasing revisit rates at 7 or 30 days after discharge, regardless of the institutions’ practice of using overnight stay, but there were three outlier institutions reporting >98% rates of overnight stay after T&A and no readmissions or revisits within 30 days. In Figure 2, overall rates of ED visits are compared to overall rates of readmission across the 48 institutions; there was no evident correlation between the revisit types, with some institutions having higher rates of readmission than of ED visits after T&A. As shown in Figure 3, there has been a downward trend of performing T&A as an outpatient procedure over the study years, although it is apparent that patients with OSA/SDB symptoms still undergo T&A in the outpatient setting.
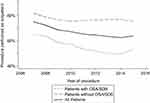 | Figure 3 Outpatient procedures as a proportion of pediatric adenotonsillectomies performed over 2007–2015, by the presence of obstructive sleep apnea (OSA) or sleep-disordered breathing (SDB). |
The primary reasons for 36,234 unique revisits are compared according to revisit timing and type in Table 1. The most common specific reasons for 7-day revisits were dehydration (22%), bleeding (19%), and pain (15%). Readmissions within 7 days of discharge were primarily due to bleeding (42%) and dehydration (28%). Reasons for 7-day revisits were broadly similar across the categories of hospital overnight stay rates (Table S1). Study outcomes and patient characteristics are compared according to institutional use of overnight stay after T&A in Table 2. There were few substantive differences in patient characteristics across hospital categories, apart from relatively younger age among patients at hospitals favoring an overnight stay. Among patients undergoing T&A in each category of hospitals, 7-day revisit rates were generally similar, ranging from 6% to 7%.
 | Table 1 Reasons for revisit after adenotonsillectomy by revisit type and timing (N=411,876 patients) |
 | Table 2 Patient characteristics and outcomes according to overnight stay after adenotonsillectomy (N=411,876 patients) |
Results from the multivariable analysis of the primary study outcome are shown in Table 3 for cases with complete data on study variables. Individual overnight admission after T&A was associated with lower odds of all-cause 7-day revisits (OR =0.74; 95% CI: 0.72, 0.77; p<0.001). Among other covariates, asthma, diabetes, moderate APR DRG severity level, older age, and African American race were associated with a higher risk of 7-day revisits. However, hospital practice favoring greater use of overnight stay was not independently associated with lower 7-day revisit odds, compared to hospitals admitting ≤20% of the children undergoing T&A. The lack of association between greater institutional rates of overnight stay and lower revisit risk was confirmed after excluding individual admission status from the model (Table S2), or when applying the model shown in Table 2 to 30-day all-cause revisits (Table S3). However, hospitals with overnight stay rates of 21–35% (OR =0.93; 95% CI: 0.88, 0.98; p=0.012) or >60% (OR =0.85; 95% CI: 0.78, 0.94; p=0.001) were associated with lower odds of 30-day revisits compared to hospitals with the highest rate of ambulatory procedures, when individual admission status was omitted from the model (Table S3).
 | Table 3 Multivariable mixed-effects logistic regression analysis of 7-day revisits among patients following T&A (N=344,525) |
To further explore the association between institutional practice and revisit type, we fitted a multinomial logistic regression model as shown in Table 4. When predicting the likelihood of ED visit (without readmission) as opposed to no revisits, individual admission status was associated with lower likelihood of ED visit (OR =0.96; 95% CI: 0.92, 0.996; p=0.033), but there was no trend of lower ED visit likelihood at institutions with greater use of overnight stay after T&A. When predicting the likelihood of readmission as opposed to no revisits, individual overnight stay was associated with lower need for readmission (OR=0.36; 95% CI: 0.33, 0.38; p<0.001), but greater institutional use of overnight stay was associated with higher likelihood of readmission. Notably, when comparing revisit types among patients requiring ED visit or readmission within 7 days of discharge, readmissions were more likely than ED visits when institutions had >60% overnight stay after T&A as compared to ≤20% (OR =1.48; 95% CI: 1.18, 1.84; p=0.001).
 | Table 4 Multivariable mixed-effects multinomial logistic regression analysis of revisit type within 7 days of discharge |
Discussion
In 2011, the American Academy of Otolaryngology and Head and Neck Surgery published guidelines for high-quality tonsillectomy care, which recommend overnight admission after tonsillectomy for patients with a co-morbid disease such as prematurity, failure to thrive, recent respiratory infection, obesity, OSA, SDB, and neuromuscular disorders.3 Even with such guidelines, admission rates after tonsillectomy vary substantially across institutions. Practice variation is recognized as a critical issue in health care quality and has been identified as a serious issue in both the field of pediatric care and in the area of tonsillectomy.2,15,16 Despite the significant practice variation with regard to overnight stay after T&A, our study demonstrates a lack of association between hospital-level use of overnight stay, and patients’ risk of acute care revisits. Therefore, there may be limited potential for reducing acute care revisits after tonsillectomy by increasing the proportion of patients who are admitted for overnight stay. However, given the rare but lethal risk of post-discharge death associated with failure to admit and monitor patients with SDB/OSA following T&A, an evaluation of admission practices is needed to ensure the safety of this common surgical procedure. Such issues continue to represent a major health care concern as, although their incidence is extremely low, the impact is obviously high. While many of these cases can be the result of the injudicious or inappropriate use of opioids in this at-risk population, continued risk stratification is needed to identify these patients and help maintain the balance between safety and effective use of health care resources. Such data may help clarify the optimal strategy for overnight admission or extended monitoring of high-risk patients undergoing T&A. Furthermore, investigations into the effective use of non-opioid adjunctive medications, including acetaminophen and non-steroidal anti-inflammatory drugs to limit perioperative opioid needs, are needed.
Previous studies have suggested revisit rates of 3.0–12.6% within 30 days after T&A in children.13 Planned overnight admission following T&A in children has been suggested for patients under 3 years of age, those with comorbid conditions, and those with severe OSA documented on PSG (apnea-hypopnea index of 10 or more obstructive events/hour, oxygen saturation nadir less than 80%, or both).3,17 However, the association of admission status after T&A with the risk of unplanned revisits remains contradictory. Inpatient T&A patients may have a higher risk for revisits, but this was likely confounded by greater comorbidity burden or medical complexity among patients selected for inpatient admission.18 We have recently demonstrated in an analysis of children enrolled in a Medicaid Accountable Care Organization that overnight admission may, in fact, be associated with a reduced risk of revisits in the short term (7 days).11
The present study adds an institution-level perspective on this controversy. Contrary to our expectations, institutional variability in admission rates after T&A was not associated with institutional rates of revisits. However, this finding may be less surprising when considering that among institutions participating in the PHIS, variability in admission practice was much greater than variability in revisit outcomes after T&A Therefore, differences in hospital revisit rates after T&A may be explained by other institutional characteristics, apart from the use of overnight stay (eg, rural vs urban hospital location, availability of other institutions where patients may seek care after discharge) and differences in the case mix (eg, patients at higher risk for all-cause revisits due to greater morbidity burden).
Our secondary analysis examined specific types of revisits, distinguishing between only an ED visit versus the need for inpatient readmission. Surprisingly, institutional rates of ED visits and institutional rates of readmissions after T&A were not correlated with one another. This result suggests another reason for the possible discrepancies among the findings of prior studies, as some have defined revisits after T&A as readmissions only, while others have included both readmissions and ED visits, or readmissions, ED visits, and urgent care visits.1,9 Our study suggests that a low rate of the need for inpatient readmission alone does not necessarily suggest an overall low rate of revisits after T&A at a given institution, requiring a broad definition of revisits to draw accurate conclusions regarding post-discharge outcomes of T&A. Differences in institutional use of overnight stay for patients returning after T&A may also explain discrepancies in the past summaries of leading readmission causes. For example, some studies have reported leading causes of acute care revisits after T&A to be pain, nausea, and vomiting.18 However, our data showed the major reasons for revisits to be dehydration, bleeding, and fever, as described in other prior work.11
At our institution, new guidelines for risk stratification of patients scheduled for T&A were implemented in 2011, determining which procedures were performed in the main operating room (OR) with inpatient admission as opposed to a free-standing ambulatory care facility.19 The guidelines scheduled high-risk patients who required T&A to be performed in the main OR with overnight admission. Our criteria for inpatient admission with ongoing monitoring included patients <3 years of age; sleep study findings with an apnea-hypopnea index >10, pulse oximetry reading <80% or end-tidal CO2>50 mmHg; clinical history of severe OSA/SDB; obesity (BMI>95% percentile for age); craniofacial syndromes or abnormalities; and the presence of co-morbid conditions (eg, asthma, diabetes mellitus).18–21 Implementation of these guidelines reduced unanticipated admissions, while only slightly increasing planned admissions.19 Our success with improving risk stratification for T&A suggests that changing the group of patients who are admitted may have a greater effect on postoperative outcomes than simply increasing the proportion of patients who are admitted.
The use of the PHIS database results in some study limitations. As this database only contains information from a select number of affiliated pediatric hospitals, it may not contain a nationally representative population of children undergoing T&As. In addition, although this database contains most inpatient readmission or ED revisits, a small number of children may have been readmitted to a hospital or ED that is not included in this database. These readmissions and revisits would be unidentified in our analysis. Finally, as with any administrative database, the PHIS database is limited by the accuracy of its data entry. In particular, since we identified patients with OSA or SDB, asthma, and diabetes and who were obese according to ICD-9 or ICD-10 codes noted at the time of surgery, correct classification of patients is determined by the accurate entry of these codes.
Our study is the first to examine whether the institutional practice of overnight stay was related to all-cause revisits after T&A. The absence of this association, particularly for 7-day outcomes that are most likely to be influenced by admission type, suggests that implications of institutional differences in the use of overnight admission may have been overstated. Nevertheless, other institutional differences in practice may be driving the institution-level variability seen in revisit rates after pediatric T&A. Although a recent study of post-discharge outcomes in older adults suggested that analyzing readmissions alone led to similar conclusions as analyzing all acute care received after discharge, our study shows that conclusions about revisits after pediatric tonsillectomy were highly sensitive to the inclusion of revisits other than readmissions in the outcome measure.22
In the meantime, our present investigation of revisits in a multi-institutional registry does not support the conclusion that increasing the rate of inpatient T&A with an overnight stay will impact the revisit rate, either early (7 days) or late (30 days). Rather, current judicious use of overnight stay appears to perform well at limiting the risk of early revisits, notwithstanding practice variations across free-standing pediatric hospitals. Despite its low incidence, given the potentially lethal outcome of hospital discharge after T&A in patients with various risk factors, including clinical signs of OSA/SDB, overnight admission or prolonged postoperative monitoring is suggested in these patients. Furthermore, alterations in postoperative pain management practices with avoidance or limited use of opioids are suggested given the increased sensitivity of this patient population to the respiratory depressant effects of opioids.23,24 While there were no postoperative deaths reported in the database used for our study, the literature, and closed claims data clearly outline the risk in this patient population.
Acknowledgment
We thank Alice Lu and Nidhi Punja of the Data Resource Center at Nationwide Children’s Hospital for their assistance with data collection for this study.
Disclosure
Dr. Charles Elmaraghy reports personal fees from Smith and Nephew, during the conduct of the study. The authors report no other conflicts of interest in this work.
References
1. Shay S, Shapiro NL, Bhattacharyya N. Revisit rates and diagnoses following pediatric tonsillectomy in a large multistate population. Laryngoscope. 2015;125:457–461. doi:10.1002/lary.24783
2. Boss EF, Marsteller JA, Simon AE. Outpatient tonsillectomy in children: demographic and geographic variation in the United States. J Pediatr. 2012;160:814–819. doi:10.1016/j.jpeds.2011.11.041
3. Baugh RF, Archer SM, Mitchell RB, et al. American academy of otolaryngology-head and neck surgery foundation. Clinical practice guideline: tonsillectomy in children. Otolaryngol Head Neck Surg. 2011;144:1–30. doi:10.1177/0194599810389949
4. Shah RK, Welborn L, Ashktorab S, Stringer E, Zalzal GH. Safety and outcomes of outpatient pediatric otolaryngology procedures at an ambulatory surgery center. Laryngoscope. 2008;118:1937–1940. doi:10.1097/MLG.0b013e3181817b9a
5. Bhattacharyya N. Ambulatory pediatric otolaryngologic procedures in the United States: characteristics and perioperative safety. Laryngoscope. 2010;120:821–825. doi:10.1002/lary.20852
6. De Luca Canto G, Pachêco-Pereira C, Aydinoz S, et al. Adenotonsillectomy complications: a meta-analysis. Pediatrics. 2015;136:702–718. doi:10.1542/peds.2015-1283
7. Coté CJ, Posner KL, Domino KB. Death or neurologic injury after tonsillectomy in children with a focus on obstructive sleep apnea: houston, we have a problem! Anesth Analg. 2014;118:1276–1283. doi:10.1213/ANE.0b013e318294fc47
8. Mahant S, Keren R, Localio R, et al. Variation in quality of tonsillectomy perioperative care and revisit rates in children’s hospitals. Pediatrics. 2014;133:280–288. doi:10.1542/peds.2013-1884
9. Murray R, Logvinenko T, Roberson D. Frequency and cause of readmissions following pediatric otolaryngologic surgery. Laryngoscope. 2016;126:199–204. doi:10.1002/lary.25250
10. Coller RJ, Klitzner TS, Saenz AA, Lerner CF, Nelson BB, Chung PJ. The medical home and hospital readmissions. Pediatrics. 2015;136:1550–1560. doi:10.1542/peds.2015-1618
11. Tumin D, Walia H, Raman VT, Tobias JD. Acute care revisits after adenotonsillectomy in a pediatric medicaid population in Ohio. Inter J Pediatr Otorhinolary. 2017;94:17–22. doi:10.1016/j.ijporl.2017.01.008
12. Brown EG, Anderson JE, Burgess D, Bold RJ, Farmer DL. Pediatric surgical readmissions: are they truly preventable? J Pediatr Surg. 2017;52:161–165. doi:10.1016/j.jpedsurg.2016.10.037
13. Tumin D, Li SS, Kopp BT, et al. The effect of the affordable care act dependent coverage provision on patients with cystic fibrosis. Pediatr Pulmonol. 2017;52:458–466. doi:10.1002/ppul.23648
14. Mahant S, Keren R, Localio R, et al. Pediatric Research in Inpatient Settings (PRIS) Network. Variation in quality of tonsillectomy perioperative care and revisit rates in children‘s hospitals. Pediatrics. 2014;133:280–288. doi:10.1542/peds.2013-1884
15. Goyal SS, Shah R, Roberson DW, Schwartz ML. Variation in post-adenotonsillectomy admission practices in 24 pediatric hospitals. Laryngoscope. 2013;123:2560–2566. doi:10.1002/lary.24172
16. Wasson JD, Prinsley PR. Tonsillectomy: variation in practice reflecting regional variation in disease presentation. Clin Otolaryngol. 2011;36:522–524. doi:10.1111/j.1749-4486.2011.02390.x
17. Roland PS, Rosenfeld RM, Brooks LJ, et al. Clinical practice guideline: polysomnography for sleep-disordered breathing prior to tonsillectomy in children. Otolaryngol Head Neck Surg. 2011;145(1 Suppl):S1–S15. doi:10.1177/0194599811409837
18. Edmonson MB, Eickhoff JC, Zhang C. A population-based study of acute care revisits following tonsillectomy. J Pediatr. 2015;166:607–612. doi:10.1016/j.jpeds.2014.11.009
19. Raman VT, Jatana KR, Elmaraghy CA, Tobias JD. Guidelines to decrease unanticipated hospital admission following adenotonsillectomy in the pediatric population. Int J Pediatr Otorhinolaryngol. 2014;78:19–22. doi:10.1016/j.ijporl.2013.10.010
20. Kako H, Tripi J, Walia H, et al. Utility of screening questionnaire and polysomnography to predict postoperative outcomes in children. Int J Pediatr Otorhinolaryngol. 2017;30(102):71–75. doi:10.1016/j.ijporl.2017.09.006
21. Brown KA. Outcome, risk, and error and the child with obstructive sleep apnea. Paediatr Anaesth. 2011;21:771–780. doi:10.1111/j.1460-9592.2011.03597.x
22. Raman VT, Splaingard M, Tumin D, Rice J, Jatana K, Tobias JD. Utility of screening questionnaire, obesity, neck circumference, and sleep polysomnography to predict sleep disordered breathing in children and adolescents. Pediatr Anesth. 2016;26:655–664. doi:10.1111/pan.12911
23. Horwitz L, Wang Y, Altaf F, et al. Hospital characteristics associated with postdischarge hospital readmission, observation, and emergency department utilization. Med Care. 2018;56:281–289. doi:10.1097/MLR.0000000000000882
24. Brown KA, Moss IR. Opiate usage in children with obstructive sleep apnea syndrome. Anesth Analg. 2007;105:547–548. doi:10.1213/01.ane.0000268543.56134.c4
Supplementary materials
 | Table S1 Reasons for 7-day revisits according to hospital use of overnight stay after adenotonsillectomy (N=26,908 revisits) |
 | Table S2 Multivariable mixed-effects logistic regression analysis of 7-day revisits among patients following T&A, omitting individual admission status (N=344,525) |
 | Table S3 Multivariable mixed-effects logistic regression analyses of 30-day revisits among patients following T&A, including or omitting individual admission status. (N=344,525) |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.