Back to Journals » Clinical Ophthalmology » Volume 13
Outcomes of treatment with sirolimus for non-infectious uveitis: a meta-analysis and systematic review
Authors Cabahug VLO , Uy HS , Yu-Keh E, Sapno KJD
Received 16 December 2018
Accepted for publication 22 February 2019
Published 18 April 2019 Volume 2019:13 Pages 649—669
DOI https://doi.org/10.2147/OPTH.S198401
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Video abstract by Cabahug VL
Views: 638
Vicente Lorenzo O Cabahug,1 Harvey S Uy,1,2 Ellen Yu-Keh,1 Kristine Joy D Sapno3
1St Luke’s Medical Center, Quezon City, Philippines; 2University of the Philippines, Manila, Philippines; 3University of Santo Tomas Hospital, Manila, Philippines
Background: Uveitis is a group of intraocular inflammatory diseases whose primary treatment involves immunosuppression. Although corticosteroids (CSs) remain the mainstay therapy, sirolimus is among the recently studied immunomodulatory drugs for treating noninfectious uveitis (NIU).
Objective: The aim of this review was to assess and summarize the updated evidence on the outcomes of treatment with sirolimus for NIU.
Materials and methods: Two reviewers conducted a systematic search on November 5, 2018, of electronic databases (EMBASE, MEDLINE, and The Cochrane Library) and clinical trial registers having no restrictions on language or publication date. The primary outcome was uveitis activity as measured by vitreous haze (VH), while the secondary outcomes included central macular thickness (CMT), best-corrected visual acuity (BCVA), CS-sparing effect, IOP elevation, and other adverse events. A meta-analysis was conducted on selected studies with appropriate clinical and methodological homogeneity.
Results: Seven studies were included and reviewed. Four randomized clinical trials were eligible for meta-analysis: SAVE 2013, One-year outcomes of the SAVE study, SAVE 2 2016, SAKURA 2016. The pooled proportions of inflammation control (VH improvement) were 38% (95% CI 16.19%–62.66%) during a 6-month follow-up and 49.97% (95% CI 16.19%–83.03%) during a 6- to 12-month follow-up with the latter showing a significantly higher response rate (p=0.0472). BCVA improvement was 62.2% (95% CI 33.17%–87.11%) during a 6-month follow-up and 56.86% (95% CI 20.91%–89.05%) during a 6- to 12-month follow-up with no significant difference between the two (p=0.3705). Increased IOP remained at 7.11% (95% CI 3.46%–12.68%) for both a 6-month follow-up and up to a 12-month follow-up duration. The CS-sparing effect of sirolimus was also well demonstrated. A reduction in CMT was observed, and only minor drug-related adverse events were reported in all the studies reviewed.
Conclusion: This review provided evidence that sirolimus is a promising treatment option for controlling inflammatory activity, improving visual acuity, and sparing CS use with minor adverse events for NIU.
Keywords: non-infectious uveitis, immunosuppression, corticosteroid-sparing, sirolimus, mTOR inhibitors, uveitis treatment, vitreous haze
Introduction
Uveitis is a group of intraocular inflammatory diseases1 with significant clinical, socioeconomic, and quality-of-life impact.2–4 As the third leading cause of preventable blindness in the world (fifth in the US), uveitis should engender greater efforts toward the development of sight-saving treatments.5,6 Potentially blinding complications include cataract, glaucoma or increased IOP, and macular edema (ME).7 Uveitis is responsible for about 5%–20% of visual loss in the USA and Europe and as high as 25% in developing countries.8 Up to 90% of cases affected belong to the working class (20–60 years of age), with nearly half occurring at the third to fourth decade of life.8
Corticosteroids (CSs) have always been the mainstay of treatment for most forms of noninfectious uveitis (NIU). In fact, the Standardization of Uveitis Nomenclature (SUN) Working Group guidelines recommend its use as the first-line therapy for active disease.9,10 Topical CS preparations are usually given for cases of anterior uveitis, while periocular, intravitreal (IVT), or systemic preparations are available for intermediate uveitis, posterior uveitis, and panuveitis. However, certain limitations with CS therapy arise in cases of refractory uveitis and in patients who develop CS-related complications such as hypertension, diabetes, cataract formation, IOP elevation, or glaucoma due to prolonged use.11–15 Thus, uveitis treatment guidelines recommend that chronic use of systemic CSs should be no more than 10 mg/day prednisone-equivalent dose to reduce the incidence of potentially serious adverse events,16 but even adverse outcomes can still occur with a dose as low as 7.5 mg/day.17 In such situations, other forms of immunosuppressive therapy may be warranted.10
Immunomodulatory therapy (IMT) is an alternative for controlling the inflammatory process and serves as adjunctive therapy that helps in reducing CS use. Although CSs are usually required to control acute inflammation, IMT agents are available to downregulate chronic inflammation and prevent recurrences.18 A number of drug classes belong to this group of agents, and choosing which among these drugs to use depends not only on drug efficacy but also on tolerability.19 Such an agent that demonstrates both efficacious steroid-sparing IMT and favorable side effect profile is therefore needed.20
Sirolimus is a recently studied and developed IMT agent for treating noninfectious intermediate uveitis, posterior uveitis, and panuveitis.21 Sirolimus, also known as rapamycin, is a bacteria-derived IMT agent that suppresses T cell proliferation by inhibiting the expression of IL-2, IL-4, and IL-15. This is mediated by the binding of the immunophilin FKBP-12 and, therefore, preventing it from binding and activating the mTOR.22,23 This may have a beneficial effect in the context of uveitis, as the immune dysfunction in NIU is thought to be primarily T cell mediated.24,25
The US Food and Drug Administration has approved the systemic use of sirolimus in preventing kidney transplant rejection as well as a sirolimus-eluting coronary stent for enhancing coronary luminal diameter in patients with ischemic heart disease. Currently, the therapeutic use of sirolimus in ophthalmology is still under investigation.22,23
The systemic use of sirolimus is associated with cytotoxic, especially hematological, adverse effects (AEs) that can limit its use in treating patients with uveitis.21 However, local preparations of the drug that can be administered by subconjunctival (SCJ) or IVT injections have been developed and proven suitable based on preclinical studies.26 Clinical trials are now focused on determining the optimal effective dose of sirolimus in such preparations.27–29
The aim of this article was to systematically review the current evidence concerning the therapeutic use of sirolimus for patients with NIU and to perform a meta-analysis on the available data.
Materials and methods
This systematic review and meta-analysis were conducted by using the methods described by the Cochrane Collaboration for systematic reviews of interventions and in concordance with the PRISMA guidelines for systematic reviews and meta-analyses.30,31 The details of the systematic review protocol were submitted for registration on the International Prospective Register of Systematic Reviews (PROSPERO) database (registration number: CRD42018115715).
The aim of this meta-analysis was to assess the effectiveness and treatment outcomes of the mTOR inhibitor sirolimus (rapamycin) for the treatment of NIU. This was achieved by conducting a statistical study of clinical trials, which evaluated or described the use of sirolimus in cases of NIU.
Eligibility criteria
The following criteria were used in the selection of studies for review:
- NIU-related studies with inflammatory activity grading defined based on the SUN working group criteria
- Patients with refractory uveitis receiving a chronic course of immunosuppressive therapy and systemic steroid treatment
- Sirolimus as the intervention competed with or without any comparator (eg, another pharmacological agent or placebo)
- Studies with a median follow-up duration of at least 3 months.
Outcome measurements
The primary outcome assessed is the clinical activity of uveitis by vitreous haze (VH) score after giving sirolimus in different doses and intervals. The following secondary outcomes were recorded and assessed: best-corrected visual acuity (BCVA) in ETDRS letters, clinical measures of uveitis activity (anterior chamber cells, presence of active inflammatory vascular and chorioretinal lesions, and central macular thickness [CMT]), concurrent requirement of CSs and other immunomodulatory treatment to control uveitis, time to treatment failure defined as the time up to a worsening (two-grade increase) in the SUN cell activity score, and occurrence of adverse events.
Searches
The literature search for review was conducted using the electronic databases of published studies namely: Cochrane Library (which comprises a portal to EMBASE and PubMed), PMC (which includes MEDLINE), and registers of clinical trials of ClinicalTrials.gov with the terms “sirolimus” or “rapamycin” matched with “uveitis”. No restrictions were made on uveitis such as using the words “anterior”, “posterior”, “infectious”, “non-infectious” to expand the number of hits in the literature to be reviewed. No restrictions were made on language, year of publication, and study types included to deliver more evidence related to the effectiveness of sirolimus in cases of uveitis. The search strategy for CENTRAL, PMC, and ClinicalTrials.gov is summarized in Tables S2–S4.
Selection of studies
Two reviewers (Cabahug and Sapno) independently screened the titles and abstracts of the searched studies and determined their relevance to this meta-analysis. Full-text articles were retrieved and assessed for eligibility. Evaluations of methodological quality and risk of bias were made using the Cochrane risk of bias tool and a modified Jadad scale.32–35 The Jadad scale assesses three primary quality factors: randomization, blinding, and reported withdrawals. The modified augmented version will also assess other methodological factors such as exclusion criteria, the intervention used, the control used, and data reporting providing a total quality score of 10 (Table 1).34,35
  | Table 1 The modified Jadad questionnaire for assessing the risk of bias |
Key information gathered from the selected articles was listed in a standard form containing relevant details such as study design type, number of patients, type of intervention, dosage, follow-up duration, and outcome measurements. A PRISMA flow diagram was used to illustrate the details of the selection process including reasons for the exclusion of articles.31
Data synthesis and analysis
All collected data from the selected studies were summarized and tabulated for possible statistical treatment. Meta-analysis was undertaken, where appropriate clinical and methodological homogeneity exists.
Meta-analysis on single proportions was utilized in order to identify the pooled response rate of reduction in VH, BCVA improvement, IOP elevation, CMT, CS-sparing effect, and safety outcomes whenever possible. MedCalc uses a Freeman–Tukey transformation (arcsine square root transformation; Freeman and Tukey, 1950)36 to calculate the weighted summary proportion under the fixed- and random-effects model (DerSimonian and Laird, 1986)37.
Results
Selection of studies
A systematic search of multiple electronic databases yielded a total of 277 possible relevant articles; of these, 256 were excluded after screening for the titles and abstracts. After a full-text evaluation of the remaining 21 articles, 15 relevant studies specific to our research questions were included. Eight potentially eligible articles were then removed for failing to meet the inclusion criteria and for having data that could not be synthesized together. Ultimately, seven studies were included for our systematic review, but only four randomized controlled trials (RCTs) out of seven of these studies were eligible for the meta-analysis. The details of the systematic selection process are shown in Figure 1.
  | Figure 1 PRISMA flowchart. |
Characteristics of included studies
A total of seven studies were included for our systematic review, but only four studies were included in our risk of bias assessment and meta-analysis. The SAVE 201328 trial and its follow-up study, Ibrahim et al,21 were Phase I, open-label, randomized clinical trials conducted in one clinical center in USA. SAVE 2 201629 was a prospective randomized, Phase II, open-label interventional clinical trial conducted at four clinical centers also in USA. Lastly, SAKURA 2016,27 the largest clinical trial of sirolimus to date, was a Phase III, randomized, double-masked multinational study conducted in the European Union, India, Israel, Japan, Latin America, and USA. Although all the abovementioned studies were provided by a study drug from Santen, Inc. (Santen Pharmaceutical Co., Ltd., Osaka, Japan), only SAVE 2 201629 and SAKURA 201627 were industry sponsored. Table 2 summarizes all the characteristics of the four studies including the risk of bias assessment.
Types of participants
All patients included in the RCT studies were 18 years old and above, clinically diagnosed with NIU (posterior, intermediate, or panuveitis), and assessed using the SUN classification activity score for VH, with sufficient inflammation requiring systemic treatment and with a BCVA of 20/400 or better.
Types of interventions
Sirolimus was administered by either IVT or SCJ injections. IVT doses studied were 44 μg, 352 μg, 440 μg, and 880 μg. Only one study evaluated a 1,320 μg dose of sirolimus given subconjunctivally.
Types of outcomes
The primary outcome of all studies was uveitis activity as measured by VH. Secondary outcomes measured were BCVA, CMT, IOP, and CS-sparing effect as measured by CS dose. Safety outcomes and adverse events were also noted.
Characteristics of studies excluded from the meta-analysis
Sen et al,38 Vigil et al,39 and Shanmuganathan et al40 also studied sirolimus for treating patients with uveitis. The limited time of follow-up and differences in study design precluded their data for undergoing meta-analysis. All three studies, however, supported the potential efficacy of sirolimus. Main characteristics of the studies and level of evidence based on the Scottish Intercollegiate Guidelines Network (SIGN)41 criteria are summarized in Table 3.
Risk of bias of included studies
Two reviewers (Cabahug and Sapno) independently assessed the risk of bias among the included studies. To assess the methodological quality, the “modified Jadad scale” (Table 4) as well as the “Cochrane risk of bias assessment tool” (Figure 2) was used. The mean Jadad score was 8.0 (high quality). Each study was assessed for the presence of any selection bias, performance bias, detection bias, attrition bias, selective reporting, and other potential sources of bias (Figure 3). Three studies had a low overall risk of bias with SAKURA 2016 having the lowest risk, while Ibrahim et al21 had an unclear risk of bias. Collectively, the overall risk of bias of all the selected studies was 75% low risk of bias and 25% unclear risk of bias (Figure 2).
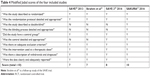  | Table 4 Modified Jadad scores of the four included studies |
  | Figure 2 Risk of bias summary: (+) low risk, (?) unclear risk, (−) high risk. |
  | Figure 3 Risk of bias graph. |
Studies awaiting assessment
The SAKURA 2 trial, which was also sponsored by Santen Inc., was recently completed with supposedly mixed results compared to the original SAKURA trial. However, data were still unavailable. The authors have attempted to contact the representatives of the company requesting their official results.42
The LUMINA trial (ClinicalTrials.gov Identifier: NCT03711929) is the latest Phase III trial yet to be commenced by Santen Inc. The study design is similar to the SAKURA trial except that this study included a sham treatment arm. The expected completion date is April 17, 2021.43
Control of uveitis activity
Figure 4 shows a meta-analysis on percentage improvement in VH with a follow-up duration of 6 months, where the test of heterogeneity of 74.95% I2 (p=0.0185) suggests that a random-effects model is preferred. The resulting overall pooled proportion of percentage improvement in VH is 38%, with 95% CI of 16.19–62.66. The biggest weight given is on SAKURA 201627 (82.73). Forest plot, where the diamond marker did not intersect 0, suggests that the 38% pooled prevalence is significantly higher than 0.
  | Figure 4 The pooled proportion of percentage improvement in VH with a follow-up duration of 6 months. |
Figure 5 shows a meta-analysis on percentage improvement in VH with a follow-up duration of 6–12 months, where the test of heterogeneity of 88.03% I2 (p=0.0002) suggests that a random-effects model is preferred. The resulting overall pooled proportion of percentage improvement in VH is 49.97%, with 95% CI of 16.93–83.03. The biggest weight given is on SAKURA 201627 (37.63). Forest plot, where the diamond marker did not intersect 0, suggests that the 49.97% pooled prevalence is significantly higher than 0.
  | Figure 5 The pooled proportion of percentage improvement in VH with a follow-up duration of 6–12 months. |
The two different meta-analysis runs were compared, specifically, the pooled response rate of 38% and 49.97%, and the resulting p-value of 0.0472 indicates that the run where the 1-year duration was included has significantly higher response rate as compared to the run where all studies are only up to 6 months.
Visual acuity
Figure 6 shows a meta-analysis on percentage improvement in BCVA with a follow-up duration of 6 months, where the test of heterogeneity of 83.75% I2 (p=0.0021) suggests that a random-effects model is preferred. The resulting overall pooled proportion of percentage improvement in BCVA is 62.2%, with 95% CI of 33.17–87.11. The biggest weight given is on SAKURA 201627 (39.1). Forest plot, where the diamond marker did not intersect 0, suggests that the 62.6% pooled prevalence is significantly higher than 0.
  | Figure 6 The pooled proportion of percentage improvement in BCVA with a follow-up duration of 6 months. |
Figure 7 shows a meta-analysis on percentage improvement in BCVA with a follow-up duration of 6–12 months, where the test of heterogeneity of 90.22% I2 (p=0.0001) suggests that a random-effects model is preferred. The resulting overall pooled proportion of percentage improvement in BCVA is 56.86%, with 95% CI of 20.91–89.05. The biggest weight given is on SAKURA 201627 (36.75). Forest plot, where the diamond marker did not intersect 0, suggests that the 56.86% pooled prevalence is significantly higher than 0.
  | Figure 7 The pooled proportion of percentage improvement in BCVA with a follow-up duration of 6–12 months. |
The two different meta-analysis runs about BCVA improvement were compared, specifically, the pooled BCVA improvement of 62.2% and 56.86%, and a resulting p-value of 0.3705 indicates that the two runs resulted in same pooled BCVA improvement indicating that no significant difference exists.
IOP
Figure 8 shows a meta-analysis on percent increase in IOP with a follow-up duration of 6 months, where the test of heterogeneity of 0.00% I2 (p=0.6545) suggests that a fixed-effects model is preferred. The resulting overall pooled proportion of percent increase in IOP is 7.1%, with 95% CI of 3.46–12.68. The biggest weight given is on SAKURA 201627 (80.1). Forest plot, where the diamond marker did not intersect 0, suggests that the 7.1% pooled prevalence is significantly higher than 0.
  | Figure 8 The pooled proportion of percentage increase in IOP with a follow-up duration of 6 months. |
SAVE 201328 and Ibrahim et al21 reported the same number of events for percent increase in IOP indicating no change after 1 year. Thus, a meta-analysis on percent increase in IOP with a follow-up duration of 6–12 months was not performed.
Other outcomes
Outcomes where data were not reported similarly precluded meta-analysis; hence, a narrative synthesis is reported in the following sections.
CS-sparing effect
SAVE 201328 and Ibrahim et al21 reported that 11 subjects (IVT group n=6, SCJ group 2 n=5) with active uveitis who were receiving prednisone ≥10 mg/day and/or at least one systemic IMT (category 2) successfully tapered their CS dose to <10 mg/day, with a median dose reduced up to 8 mg/day and 2 mg/day at month 6 and month 12, respectively, from a 20 mg/day median dose at baseline. Subjects with inactive disease at baseline (category 3) also showed a reduction with a median dose to 3 mg/day and 2 mg/day at months 6 and 12, respectively, from a median dose of 9 mg/day at baseline. CS was stopped completely in five patients from category 2. However, it was impossible to reduce CS dose in one patient and ended the study with a 20 mg/day dose.
In SAVE 2 2016,29 dose reduction was reported in nine out of ten patients who received ≥10 mg daily of systemic CS treatment at baseline to <5 mg daily after 6 months of treatment (440 μg n=4 [100%]; 880 μg n=5 [83.3%]) as a result of improvement in VH.
SAKURA 201627 also reported a dose reduction in 69 patients treated with CS at baseline. CS dosage was ≤5 mg at month 5 in 48 patients (69.6%) and eventually discontinued in all except for one patient (47/69 [68.1%]). Each dose group (44 μg n=14/22 [63.6%]; 440 μg n=20/26 [76.9%]; 880 μg n=14/21 [66.7%]) reached this end point in similar proportions. However, comparing the proportion of patients who met both the primary end point and the CS-tapering end point, the 440 μg dose group had significantly higher number of such patients than the 44 μg dose group (P=0.011).
CMT
SAVE 201328 and Ibrahim et al21 reported that, at baseline, 37% (n=11) of subjects had ME (IVT n=7, SCJ n=4), defined as having an average CMT of >315 μm. In patients without ME (n=17), the average thickness was 272 μm (27), 265 μm (29), and 269 μm (35) at baseline, month 6, and month 12, respectively, with no changes from baseline in any patient during the follow-up at month 6 or 12. In patients who had ME, the baseline average (SD) CMT was 505 μm (156). CMT in the IVT group increased to 615 μm (168) at month 6 and 616 μm (165) at month 12, with a mean change of 105 μm and 106 μm at months 6 and 12, respectively, from an average of 510 μm (194) at baseline. The SCJ group showed a reduction in CMT with a mean change of 30 μm and 47 μm, at months 6 and 12, respectively, to 451 μm (114) at month 6 and to 434 μm (122) at month 12 from 481 μm (131) at baseline. No statistical difference was present between the changes in CMT from baseline at either month 6 or 12 (P=0.169 and 0.182 at month 6 and 12, respectively).
SAVE 2 201629 reported that patients with baseline ME receiving the 440 μg dose (n=7) had a decrease in CMT with a mean change of 42 mm from baseline at month 6, while those receiving 880 μg (n=6) had an increase in CMT with a mean change of 82 mm from baseline. Patients without ME at baseline (n=11) did not have any significant change in mean CMT at month 6.
Lastly, SAKURA 201627 also showed that CMT decreased by 50 mm or more in nearly 50% of all patients with baseline ME (CMT >300 mm, n=99) in each of the three treatment groups (44 μg, 45.5%; 440 μg, 55.2%; 880 μg, 48.6%) with no significant differences between the three groups (P=0.061).
Safety outcomes/AEs
SAVE 201328 and Ibrahim et al21 reported mild-to-moderate ocular and systemic AEs with both IVT and SCJ injections of sirolimus, and no systemic AEs were related to treatment. Vitreous floaters were the common complaint in the IVT group, while in the SCJ group conjunctival hyperemia and chemosis were among the common complaints reported.
SAVE 2 201629 also reported mild-to-moderate non-ocular AEs (eg, sinus infection), but all were treatment unrelated. Ocular AEs (eg, ocular pain) were reported in both treatment groups (440 μg, 36.4%; 880 μg, 46.2%), while more serious events tended to be reported in the 880 μg group (eg, anterior uveitis and cataract) not commonly seen in the 440 μg group. Fourteen patients who received bilateral IVT sirolimus injections also tolerated treatment well. Systemic AEs (eg, sinus infection) were reported in three patients (21.4%), while local AEs (eg, floaters) were reported in two patients (14.3%) suggesting that bilateral IVT injections of sirolimus may be given safely on the same day. The SAVE 2 study also suggested that both monthly 440 μg and every other monthly 880 μg IVT sirolimus injections provide sufficient control of ocular inflammation in most cases of NIU, while the monthly injections were noted to be more beneficial in reducing ME.
Lastly, SAKURA 201627 demonstrated that treatment-related ocular serious AEs with sirolimus were uncommon, but the severity tended to be dose dependent. Sterile endophthalmitis was reported in 0%, 0.9%, and 3.4% of patients in the 44 μg, 440 μg, and 880 μg dose groups, respectively. Similarly, cataract progression was seen in 0.9%, 0.9%, and 2.6% of patients in the 44 μg, 440 μg, and 880 μg dose groups, respectively. Two patients, one of each from the 44 μg and 440 μg dose groups, had glaucoma. The mean IOP in all three treatment groups remained nearly constant (≤1.1 mmHg difference) from baseline up to month 5. All of the abovementioned findings suggest that IVT sirolimus may not be associated with AEs commonly reported in previous studies involving intraocular CS treatment and that non-ocular AEs occurred with low frequency unrelated to treatment (eg, headache in 4.6% of all patients). Finally, SAKURA 201627 suggested that a 440 μg IVT sirolimus injection was the optimal dose in having a better benefit-to-risk profile for treating most cases of NIU leading to improvement in ocular inflammation with a low incidence of AEs commonly associated with intraocular CS treatment in patients with active disease.
Discussion
Summary of evidence
The data provided in this review and meta-analysis summarize the available evidence for the use of sirolimus in the treatment of NIU. Currently, the potential use of sirolimus in such cases is limited by the paucity of RCTs available. We have presented a pooled proportion of the outcomes studied with sirolimus treatment at 6 months and up to 1-year follow-up. It should be noted that there was only one study evaluating the 1-year outcomes.28
The pooled proportion of VH improvement with a 6-month follow-up was 38%, but this increased to nearly 50% when 1-year follow-up study data were included. This suggests a trend to further improvement in uveitis control when longer follow-ups are included which was not usually evaluated with current trials available. The pooled proportion of BCVA improvement was relatively the same after 6 months (62.2%) and 1 year (56.86%). An improvement in visual acuity can probably be appreciated early in the course of treatment, although it is still not clear whether good visual acuity and its duration can be maintained. Improvement in visual acuity follows inflammation control as seen by the reduction in VH in these patients.
CSs are still the mainstay of treatment in uveitis, used both as rescue therapy for acute disease and as long-term therapy in chronic or even refractory cases.12,44 CSs have many desirable features, including speed of onset and efficacy in both local and systemic forms. In the MUST trial, disease inactivity was reported in 88% of eyes randomized to the fluocinolone acetonide implant and in 71% of eyes randomized to systemic CS usage.12,44 They do however have an unfavorable side effect profile, with dose- and duration-dependent adverse systemic effects. Alternative IMT has been developed to address these concerns. These “steroid-sparing agents” have improved tolerability while maintaining similar inflammation controls. Unfortunately, these agents may be associated with different, but equally severe, side effects, and in many cases lack both the speed of onset and efficacy of CS. Nevertheless, among these agents, sirolimus remains a promising option as a potential CS-sparing IMT.
The pooled proportion of IOP elevation after both 6 months and 1 year of treatment with sirolimus was roughly 7%. This relatively low rate can be causally attributed to the overall CS-sparing effect of sirolimus. As summarized in our results, the majority of patients successfully tapered their CS dose to as low as ≤5–10 mg/day.
Blair et al44 also reported a comprehensive review of the role of mTOR inhibitors for treating NIU, including evidence on everolimus. Although a meta-analysis was not conducted, their conclusions from the data they gathered also supported our results. Published evidence thus to date suggests that sirolimus (and everolimus) appears to be well tolerated especially when locally administered and may prove useful in the management of NIU.44,45
In general, therapeutic agents administered locally provide a more rapid onset of action with fewer systemic side effects, and recent trials mainly focused on such preparations of sirolimus. In effect, the data from our meta-analysis will only apply to IVT and perhaps SCJ administrations of sirolimus. Overall, it appears that this is the most optimal and favorable route for the drug when considered for ocular conditions.
Limitations
The strength of evidence provided in this review is limited by the small number of clinical trials evaluating sirolimus. The trials available used an active control or a dose–response control. Although the existence of an effect can be readily documented, measuring the drug’s absolute effect size is not possible unless a placebo-controlled design is available. RCTs with sham treatment arms are therefore recommended. It should also be noted that there are various possible etiologies for uveitis which may be difficult to account with present clinical trial designs. The wide range of percentage improvement in VH may be attributable to this factor. Lastly, our review also did not include unpublished studies which would result in publication bias. Nevertheless, we are confident that the evidence we provide is enough to overcome this small fraction. Although there seems to be an increasing trend of evidence supporting the efficacy of sirolimus, the remaining gaps may be addressed once further evidence from ongoing or future high-quality clinical trials are available.
Conclusion
The efficacy of sirolimus in treating NIU was positively determined in a meta-analysis done on three RCTs and established that potent control of uveitis activity as a result of the reduction in VH was well demonstrated up to 12-month follow-up duration. Sirolimus treatment also resulted in moderate visual acuity improvement and had relatively low adverse events with good CS-sparing effect. However, data from ongoing and future large-scale clinical trials of appropriate design are needed to further strengthen the evidence provided.
Abbreviations
AE, adverse effects; BCVA, best-corrected visual acuity; CMT, central macular thickness; CS, corticosteroid; ETDRS, Early Treatment of Diabetic Retinopathy Study; IMT, immunomodulatory therapy; IVT, intravitreal; ME, macular edema; MUST, Multicenter Uveitis Steroid Treatment; NIU, noninfectious uveitis; PROSPERO, Prospective Register of Systematic Reviews; RCT, randomized controlled trial; SAKURA, Sirolimus study assessing double-masked uveitis treatment; SAVE, sirolimus as a therapeutic approach for uveitis; SCJ, subconjunctival; SIGN, Scottish Intercollegiate Guidelines Network; SUN, Standardization of Uveitis Nomenclature; VH, vitreous haze.
Acknowledgments
Reginald Arimado was a hired biostatistician who assisted us in conducting the meta-analysis and provided the necessary software to perform the task. No funding from any sponsor or external source was received.
Author contributions
All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
Harvey S Uy has received research funding from Santen, Inc. for an unrelated study. The other authors report no conflicts of interest in this work.
References
Krishna U, Ajanaku D, Denniston A, Gkika T. Uveitis: a sight-threatening disease which can impact all systems. Postgrad Med J. 2017;93(1106):766–773. doi:10.1136/postgradmedj-2017-134891 | ||
Fabiani C, Vitale A, Orland I, et al. Impact of uveitis on quality of life: a prospective study from a tertiary referral rheumatology-ophthalmology collaborative uveitis center in Italy. Isr Med Assoc J. 2017;19:478–483. | ||
Thorne J, Skup M, Tundia N, et al. Direct and indirect resource use, healthcare costs and work force absence in patients with non-infectious intermediate, posterior or panuveitis. Acta Ophthalmol. 2016;94(5):e331–e339. doi:10.1111/aos.12987 | ||
Chu D, Johnson S, Mallya U, Davis M, Sorg R, Duh M. Healthcare costs and utilization for privately insured patients treated for non-infectious uveitis in the USA. J Ophthalmic Inflamm Infect. 2013;3(1):64. doi:10.1186/1869-5760-3-64 | ||
The Ocular Immunology and Uveitis Foundation. Glossary of terms, incidence and prevalence of Uveitis. Uveitis.org | OIUF. Published April 10, 2017. Available from: http://www.uveitis.org/patients/education/glossary. Accessed November 10, 2018. | ||
NIH study shows two treatments for uveitis equally effective. National Eye Institute. Published August 17, 2011. Available from: https://nei.nih.gov/news/statements/uveitis. Accessed November 5, 2018. | ||
Jones N. The Manchester Uveitis Clinic: the first 3000 patients, 2: uveitis manifestations, complications, medical and surgical management. Ocul Immunol Inflamm. 2014;23(2):127–134. doi:10.3109/09273948.2014.968671 | ||
de Smet M, Taylor S, Bodaghi B, et al. Understanding uveitis: the impact of research on visual outcomes. Prog Retin Eye Res. 2011;30(6):452–470. doi:10.1016/j.preteyeres.2011.06.005 | ||
Jabs DA, Nussenblatt RB, Rosenbaum JT. Standardization of uveitis nomenclature (SUN) working group. Standardization of uveitis nomenclature for reporting clinical data. Results of the First International Workshop. Am J Ophthalmol. 2005;140(3):509–516. | ||
Rosenbaum J, Pasadhika S. Update on the use of systemic biologic agents in the treatment of noninfectious uveitis. Biologics Targets Ther. 2014;8:67–81. | ||
Yap YC, Papathomas T, Kamal A. Results of intravitreal dexamethasone implant 0.7 mg (Ozurdex®) in noninfectious posterior uveitis. Int J Ophthalmol. 2015;8:835–838. | ||
Kempen J, Altaweel M, Holbrook J, et al. Randomized comparison of systemic anti-inflammatory therapy versus fluocinolone acetonide implant for intermediate, posterior, and panuveitis: the multicenter uveitis steroid treatment trial. Ophthalmol. 2011;118(10):1916–1926. doi:10.1016/j.ophtha.2011.07.027 | ||
Lowder C, Belfort R Jr, Lightman S, et al. Dexamethasone intravitreal implant for noninfectious intermediate or posterior uveitis. Arch Ophthalmol. 2011;129(5):545. doi:10.1001/archophthalmol.2010.339 | ||
Jaffe G, Martin D, Callanan D, Pearson P, Levy B, Comstock T. Fluocinolone acetonide implant (Retisert) for noninfectious posterior uveitis. Ophthalmol. 2006;113(6):1020–1027. doi:10.1016/j.ophtha.2006.02.021 | ||
You C, Sahawneh H, Ma L, Kubaisi B, Schmidt A, Foster S. A review and update on orphan drugs for the treatment of noninfectious uveitis. Clin Ophthalmol. 2017;11:257–265. doi:10.2147/OPTH.S121734 | ||
Jabs D, Rosenbaum J, Foster C, et al. Guidelines for the use of immunosuppressive drugs in patients with ocular inflammatory disorders: recommendations of an expert panel. Am J Ophthalmol. 2000;130(4):492–513. | ||
Nguyen Q, Hatef E, Kayen B, et al. A cross-sectional study of the current treatment patterns in noninfectious uveitis among specialists in the United States. Ophthalmol. 2011;118(1):184–190. doi:10.1016/j.ophtha.2010.03.029 | ||
Pujari S, Kempen J, Newcomb C, et al. Cyclophosphamide for ocular inflammatory diseases. Ophthalmol. 2010;117(2):356–365. doi:10.1016/j.ophtha.2009.06.060 | ||
Durrani K, Zakka FR, Ahmed M, Memon M, Siddique SS, Foster CS. Systemic therapy with conventional and novel immunomodulatory agents for ocular inflammatory disease. Surv Ophthalmol. 2011;56(6):474–510. doi:10.1016/j.survophthal.2011.05.003 | ||
Denniston A, Barry R, Nguyen QD, Lee R, Murray P. Pharmacotherapy for uveitis: current management and emerging therapy. Clin Ophthalmol. 2014;1891. doi:10.2147/OPTH | ||
Ibrahim MA, Sepah YJ, Watters A, et al. One-year outcomes of the SAVE study: sirolimus as a therapeutic approach for UVEitis. Transl Vis Sci Technol. 2015;4(2):4. doi:10.1167/tvst.4.2.4 | ||
Napoli KL, Taylor PJ. From beach to bedside: history of the development of sirolimus. Ther Drug Monit. 2001;23:559–586. doi:10.1097/00007691-200110000-00012 | ||
Sehgal SN. Rapamune® (RAPA, rapamycin, sirolimus): mechanism of action immunosuppressive effect results from blockade of signal transduction and inhibition of cell cycle progression. Clin Biochem. 1998;31(5):335–340. | ||
Curnow SJ, Scheel-Toellner D, Jenkinson W, et al. Inhibition of T cell apoptosis in the aqueous humor of patients with uveitis by IL-6/soluble IL-6 receptor trans-signaling. J Immunol. 2004;173(8):5290–5297. | ||
Agarwal A, Rajagopalan N, Hassan M, et al. Sirolimus for retinal and uveitic diseases. Dev Ophthalmol Retinal Pharmacotherapeutics. 2016;55:276–281. | ||
Dugel PU, Blumenkranz MS, Haller JA, et al. A randomized, dose-escalation study of subconjunctival and intravitreal injections of sirolimus in patients with diabetic macular edema. Ophthalmol. 2012;119(1):124–131. doi:10.1016/j.ophtha.2011.07.034 | ||
Nguyen QD, Merrill PT, Clark WL, et al. Intravitreal sirolimus for noninfectious uveitis: a phase III Sirolimus study Assessing double-masKed Uveitis TReAtment (SAKURA). Ophthalmol. 2016;123(11):2413–2423. doi:10.1016/j.ophtha.2016.07.029 | ||
Nguyen QD, Ibrahim MA, Watters A, et al. Ocular tolerability and efficacy of intravitreal and subconjunctival injections of sirolimus in patients with non-infectious uveitis: primary 6-month results of the SAVE study. J Ophthalmic Inflamm Infect. 2013;3(1):32. doi:10.1186/1869-5760-3-32 | ||
Nguyen QD, Sadiq MA, Soliman MK, et al. The effect of different dosing schedules of intravitreal sirolimus, a mammalian target of rapamycin (mTOR) inhibitor, in the treatment of non-infectious uveitis (An American Ophthalmological Society Thesis). Trans Am Ophthalmol Soc. 2016;114:T3(1–14). | ||
Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions. Cochrane Handbook for Systematic Reviews of Interventions. Published March 2011. Available from: http://handbook-5-1.cochrane.org/. Accessed November 10, 2018. | ||
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8(5):336–341. doi:10.1016/j.ijsu.2010.02.007 | ||
Higgins JPT, Altman DG, Gotzsche PC, et al. The Cochrane Collaboration tool for assessing risk of bias in randomised trials. BMJ. 2011;343(2):d5928. doi:10.1136/bmj.d5928 | ||
Berger V, Alperson S. A general framework for the evaluation of clinical trial quality. Rev Recent Clin Trials. 2009;4(2):79–88. | ||
Jadad AR, Moore R, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17(1):1–12. | ||
Sarris J, Byrne GJ. A systematic review of insomnia and complementary medicine. Sleep Med Rev. 2011;15(2):99–106. doi:10.1016/j.smrv.2010.04.001 | ||
Freeman MF, Tukey JW. Transformations Related to the Angular and the Square Root. The Annals of Mathematical Statistics. 1950;21(4):607–611. doi:10.1214/aoms/1177729756. | ||
Dersimonian R, Laird N. Meta-analysis in clinical trials. Controlled Clinical Trials. 1986;7(3):177–188. doi:10.1016/0197-2456(86)90046-2. | ||
Sen HN, Larson TA, Meleth AD, Smith WM, Nussenblatt RB. Subconjunctival sirolimus for the treatment of chronic active anterior uveitis: results of a pilot trial. Am J Ophthalmol. 2012;153(6):1038–1042. doi:10.1016/j.ajo.2011.12.018 | ||
Vigil EM, Sepah YJ, Watters AL, et al. Assessment of changes in quality of life among patients in the SAVE study – sirolimus as therapeutic approach to uVEitis: a randomized study to assess the safety and bioactivity of intravitreal and subconjunctival injections of sirolimus in patients with non-infectious uveitis. J Ophthalmic Inflamm Infect. 2015;5(1):13. | ||
Shanmuganathan VA, Casely EM, Raj D, et al. The efficacy of sirolimus in the treatment of patients with refractory uveitis. Br J Ophthalmol. 2005;89(6):666–669. doi:10.1136/bjo.2004.048199 | ||
Harbour R, Miller J. A new system for grading recommendations in evidence based guidelines. BMJ. 2001;323(7308):334–336. | ||
Santen Pharmaceutical Co., Ltd. Santen announces phase III SAKURA program topline results in patients with non-infectious Uveitis of the posterior segment. PR Newswire: news distribution, targeting and monitoring. Published November 28, 2016. Available from: https://www.prnewswire.com/news-releases/santen-announces-phase-iii-sakura-program-topline-results-in-patients-with-non-infectious-uveitis-of-the-posterior-segment-300368781.html. Accessed November 10, 2018. | ||
Santen Pharmaceutical Co. A phase III study assessing the efficacy and safety of intravitreal injections of 440 ug DE-109 for the treatment of active, non-infectious uveitis of the posterior segment of the eye – full text view. Search of: Spain – list results – Clinicaltrials.gov. Available from: https://clinicaltrials.gov/ct2/show/NCT03711929. Accessed November 10, 2018. | ||
Blair J, Barry R, Moore DJ, Denniston AK. A comprehensive review of mTOR-inhibiting pharmacotherapy for the treatment of non-infectious uveitis. Curr Pharm Des. 2017;23:20. doi:10.2174/1381612823666170111125550 | ||
Nguyen QD, Merrill PT, Sepah YJ, et al. Intravitreal sirolimus for the treatment of noninfectious uveitis. Ophthalmol. 2018;125(12):1984–1993. doi:10.1016/j.ophtha.2018.06.015 |
Supplementary materials
Supplementary appendix
Intravitreal Sirolimus in Active Noninfectious Uveitis of the Posterior Segment: The Multinational, Randomized, Phase 3 SAKURA Study 1
Nguyen QD, Merrill PT, Clark WL, Banker AS, Fardeau C, Franco P, LeHoang P, Ohno S, Rathinam SR, Thurau S, Abraham A, Wilson L, Yang Y, Shams N; for the SAKURA Study Group
Randomization and Masking
Randomization occurred after subjects met all eligibility requirements at screening and Day 1. Each subject was assigned a unique randomization number. A permuted-block randomization stratified by pre-defined geographic region and baseline vitreous haze score of the study eye (1.5+, 2+, 3+, or 4+) was employed to randomize eligible subjects, and a separate permuted-block randomization scheme with a fixed block was generated for each stratum by an Interactive Voice Response System (IVRS)/Interactive Web Response System (IWRS). A computer algorithm for random number generation produced the treatment assignments.
All study sponsor personnel (with the exception of clinical supplies personnel), vendors, contract research organization staff, clinical investigators, site staff, and study subjects were masked to the treatment assignments during the Double-Masked Treatment Period. The study drug, which is formulated as a clear, nondispersive, non-aqueous solution of sirolimus in a vehicle composed of polyethylene glycol 400 and ethanol, was provided to site staff in numbered vials assigned to each subject by the randomization system. Each vial contained 20 μL of sirolimus at a concentration of 2.2 μg/μL (44 μg), 22 μg/μL (440 μg), or 44 μg/μL (880 μg). Study sites received the drug vials frozen and stored them in secure, locked, dark, temperature-controlled freezers with restricted access until the time of use. A sterile, single-use 250-μL syringe custom-marked at 20 μL was provided separately for intravitreal injection use and filled on site. The clinical investigator was required to use the syringe provided and administer sirolimus according to intravitreal injection guidelines.
Changes to Study Design
This study was originally planned as two studies to be conducted in separate predefined geographic regions (Region 1: United States and Latin America; Region 2: European Union and Asia) under a single protocol. Given that NIU of the posterior segment is an orphan disease, enrollment in each study was slower than anticipated. The sponsor, in consultation with the US FDA, restructured the studies to include the 347 subjects randomized up to March 31, 2013, in a single study, regardless of geographic region. The 347 subjects randomized up to that date comprise the population of the present study (SAKURA Study 1), with subjects enrolling from April 1, 2013, randomized into a second study (SAKURA Study 2).
Under the original plan to conduct two studies defined by geographic region, a sample size of 213 subjects (71 per treatment group) subjects per study was calculated as necessary to provide sufficient statistical power to assess the primary endpoint. Revised calculations based on the new study population defined by date of enrollment indicated that 348 subjects (116 subjects per group) would provide >80% power to detect a difference of 16% in response rate between sirolimus 44 μg (assuming aresponse rate of 8%) and sirolimus 440 μg or 880 μg (assuming a response rate of 24%) by Fisher’s exact test (two-sided, Bonferroni corrected α=0.025).
  | Table S1 Inclusion and exclusion criteria1 |
  | Table S2 CENTRAL search strategy |
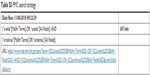  | Table S3 PMC search strategy |
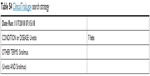  | Table S4 ClinicalTrials.gov search strategy |
Reference
Nguyen QD, Ibrahim MA, Watters A, et al. Ocular tolerability and efficacy of intravitreal and subconjunctival injections of sirolimus in patients with non-infectious uveitis: primary 6-month results of the SAVE study. J Ophthalmic Inflamm Infect. 2013;3(1):32. doi:10.1186/ 1869-5760-3-32 |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




