Back to Journals » International Medical Case Reports Journal » Volume 17
Outcomes of Proximal Spleno-Renal Shunt Operations for Idiopathic Portal Hypertension in Tertiary Hospital in the Sub-Sahara
Authors Okello M , Srikant S , Darshit D , Ocama P
Received 14 December 2023
Accepted for publication 13 April 2024
Published 23 April 2024 Volume 2024:17 Pages 381—386
DOI https://doi.org/10.2147/IMCRJ.S453341
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Xudong Zhu
Michael Okello,1,2 Sanjanaa Srikant,2 Dave Darshit,3 Ponsiano Ocama2
1Society of Uganda Gastrointestinal and Endoscopic Surgeons (SUGES), Kampala, Uganda; 2Makerere University College of Health Sciences, Kampala, Uganda; 3Department of Surgery, Lubaga Hospital, Kampala, Uganda
Correspondence: Michael Okello, President - Society of Uganda Gastrointestinal and Endoscopic Surgeons (SUGES), P.O Box 154020, Kampala, Uganda, Tel +256782654770, Email [email protected]
Purpose: Idiopathic portal hypertension (IPH) also known as non-cirrhotic portal hypertension is an entity of hepatic conditions including disorders of blood vessels that leads to portal hypertension (PHT). Current management of PHT includes medical or endoscopic therapy. A proximal spleno-renal shunt (PSRS) operation has been shown to improve the outcomes of patients with IPH with upper gastrointestinal bleeding refractory to medical and endoscopic therapy in high income countries but the same has not been well described in our resource limited setting.
Patients and methods: This study consecutively included patients who were diagnosed with IPH on pre-operative imaging and underwent PSRS surgery. Data on four patients across the time period of 3 years was obtained with a male to female ratio of 1:1 and age range of 7 to 34 years.
Results: All patients in this study had features of upper gastrointestinal bleeding and, after an endoscopy they were all diagnosed with grade IV esophageal varices. Symptom duration prior to admission varied between 3 months to 8 years. All these patients had multiple episodes of rebleeding varices with recurrent admissions and were managed conservatively by multiple blood transfusions and propranolol tablets, pre-operatively. Only one patient had previous variceal band ligation done though he developed rebleeding. All four patients underwent both PSRS surgery and splenectomy and were intra-operatively verified to have a normal smooth liver and thus IPH was the cause of the esophageal varices. After an average follow-up period of 26.5 months, we found that all patients were alive with early symptomatic relief, no recurrent bleeding and no long-term complications.
Conclusion: Good outcomes were achieved in terms of symptom resolution, endoscopic variceal resolution at follow-up endoscopy, length of stay ranging from 8 to 15 days and all four patients were alive at the time of follow-up, that ranged from 14 to 46 months.
Keywords: idiopathic portal hypertension, renal shunt, varices, Uganda
Background
Idiopathic portal hypertension (IPH) also known as non-cirrhotic portal hypertension (NCPH) or nodular regenerative hyperplasia can be described as a diverse entity of liver diseases, primarily encompassing disorders of blood vessel origin that leads to an increase of high blood pressures in the portal vein with normal functioning of the hepatocytes and normal or very small increase in the hepatic venous pressure gradient (HVPG). IPH can be categorized on the basis of the site of obstruction to blood flow as, pre-hepatic, hepatic and post-hepatic. Some of the late manifestations of IPH are the clinical features of portal hypertension (PHT) that include hematemesis, melaena stools, and unexplained anaemia, among others.1
However extrahepatic portal venous obstruction (EHPVO) and IPH are two clinical conditions that manifest features like upper gastrointestinal bleeding due to PHT but no or minimal clinical, laboratory or radiological evidence of hepatic dysfunction. Even with histology, IPH has no features of hepatic cirrhosis despite the clinical presence of PHT, it is also characterized by the exclusion of obstruction of the extrahepatic portal vein or the right, middle and left hepatic veins.2
Currently modern management of PHT includes medical or endoscopic treatment with multiple endoscopic variceal banding or obliteration being the procedure of choice. Trans jugular intra-hepatic portosystemic shunts (TIPS) is another alternative in developed countries for treatment of complications of NCPH, but it should be avoided in patients with poor renal function, ascites, and significant extrahepatic comorbidities (eg, prothrombotic condition, hematologic malignancy, solid organ transplantation). Studies have suggested that TIPS may be complicated by hepatic encephalopathy, recurrent variceal bleeding and a risk of mortality especially among patients with extrahepatic comorbidities and elevated creatinine.3
Liver transplantation is another option for IPH with similar indications as those for cirrhosis with liver decompensation manifesting with ascites, jaundice, upper gastrointestinal bleeding due to esophageal varices, coagulopathy and different grades of hepatic encephalopathy. Outcome data are not as numerous as that for cirrhosis, non-alcoholic fatty disease, non-alcoholic steatohepatitis, liver cancer, etc. however, small case series suggest favorable survival rates for liver transplant patients following IPH especially with portal biliopathy.4 The risk of IPH recurrence after liver transplantation is uncommon though reported in a handful of case reports and case series.5
The procedure of anastomosing the splenic vein to the left renal vein treats IPH with upper gastrointestinal bleeding not responding to medical and/or endoscopic treatment. It offers a one-time long-lasting control of bleeding as opposed to multiple variceal banding ligations for this group of patients. Thus, it might be more appropriate for resource limited settings like Uganda and most sub-Saharan countries which have limited access to interventional endoscopy services like endoscopic banding. Blood transfusion products are also not readily available and healthcare facilities may not be near to the patients.6
Before the advancement of endoscopy, creation of surgical portosystemic shunts was almost the only treatment for IPH. Nowadays, portosystemic surgical shunt procedures are less advocated since medical, endoscopic and radiologic interventions have improved. This surgery still prevents multiple treatment sessions offered by both endoscopic and radiological interventions. The patients who opt for the shunt surgery too have good long-term survival and low procedure related morbidity.7
The patients were managed at the Uganda Martyrs Hospital Lubaga, Surgery Department. Lubaga hospital is found in Kampala, Uganda and is a private, not for profit, tertiary level hospital founded by the Catholic Church in 1899, with a bed capacity of 275.
This study was done due to the paucity of data about IPH and the corresponding surgical management by PSRS surgery in the sub-Saharan setting. It was therefore aimed at documenting the short- and long-term outcomes of IPH patients undergoing PSRS surgery in our setting.
This case series has been reported in line with the PROCESS 2020 criteria.
Case Presentation
From June 2019 to March 2022, all patients with non-cirrhotic portal hypertension, who had abdominal surgery were retrospectively reviewed. In this case series, we consecutively included patients who were diagnosed with non-cirrhotic liver disease on pre-operative imaging and underwent proximal splenorenal shunt surgery. One case was excluded who was found to have cirrhotic liver disease intra-operatively.
Data on four patients across the time period of 3 years was obtained (Table 1). The parameters included patients’ demographics, comorbid diseases, overall survival, type of performed operative procedures, duration of symptoms and the procedure outcomes. Two of the patients were male and two females. These patients’ ranged in age between 7 years and 34 years old (mean age of 19 years).
 |
Table 1 Socio-demographics and clinical findings of the patients |
All patients in our case series presented with variceal bleeding in addition to a diversity of signs and symptoms with a varied duration from 3 months to 8 years. All the patients had multiple episodes of rebleeding varices with recurrent admissions and were managed conservatively by multiple blood transfusions and propranolol tablets pre-operatively as prophylaxis. Only one patient had previous variceal band ligation done, though he developed rebleeding. In our case series, all four patients underwent proximal splenorenal shunt with splenectomy with intraoperatively verified non-cirrhotic liver disease. All received a comprehensive post-surgical treatment plan aimed at addressing their unique health including fluid balance, pain management, blood transfusions, and clot prophylaxis (aspirin, heparin). Two patients aged 7 years and 16 years received post-splenectomy prophylactic immunisation against Streptococcus pneumoniae, Neisseria meningitidis and Haemophilus influenzae type-b, 2 weeks after the surgery. All patients were successfully discharged within one to two weeks post-operatively.
Discussion
Idiopathic portal hypertension is reported in both developing and developed countries. This condition is far more common in low resource settings where the advanced endoscopic, medical and radiological treatment options are still limited.8 Main portal vein obstruction at its extrahepatic segment (EHPVO) is a heterogeneous entity characterized by partial or complete blockage of the main portal vein, with or without involvement of the intra-hepatic portal veins, and does not include thrombosis of the splenic vein or superior mesenteric vein (SMV) that occurs in isolation.9 In this case series, one case of portal vein thrombus was identified with portal cavernoma formation and three cases were idiopathic portal hypertension.
EHPVO is common in the paediatric age group in comparison to adults, and this disease is mostly in low-income countries with low socio-economic status accounting for as high as 15–20% cases. It accounts for 5–10% of cases in high income countries.10 In our case series, the average age of patients was 19 years with an age range of 7 years to 34 years old. The cause of upper gastrointestinal bleeding in many of the patients is esophageal varices.11 All patients in our case series presented with variceal bleeding in addition to other signs and symptoms. The duration of the clinical features prior to admission to our hospital also varied among the patients from 1 week to 8 years.
The majority of centres in resource limited settings currently practice conventional procedures: endoscopic sclerotherapy (EST), band ligation done during upper gastrointestinal endoscopy and other endoscopic techniques of variceal obliteration using N-butyl-2-cyanoacrylate glue as the mainstay treatment for varices in the oesophagus that are bleeding due to IPH. While most available literature on PHT is among cirrhotic patients there is limited literature regarding optimal management of gastric/esophageal variceal bleeding in patients with IPH. Other treatment options like balloon-occluded retrograde transvenous obliteration (BRTO) and transjugular intrahepatic portosystemic shunts (TIPS) are routinely used to manage PHT due to IPH in developed nations where endoscopic and interventional radiology services are readily available.
However, all these procedures have a high rebleeding rate between 22% and 50%. Besides this, patients have a debilitating distress of undergoing multiple procedure sessions regarding burden of cost and resource utilization making it unsuitable for those in rural and remote areas.12 All the patients had multiple episodes of rebleeding varices with recurrent admissions and were managed conservatively by multiple blood transfusions and propranolol tablets, pre-operatively. Only one patient had previous variceal band ligation done, though he developed rebleeding. Management of these patients should not just be restricted to treatment of variceal bleeding alone. Proximal splenorenal shunt (PSRS) surgery in bleeding varices patients may be an effective and safe single-step therapy for prevention of rebleeding as well as correction of hypersplenism with acceptable morbidity and mortality.13,14 In our case series, all four patients underwent proximal splenorenal shunt with splenectomy with intraoperatively verified non-cirrhotic liver disease.
The main complications after shunt surgery, include porto-systemic encephalopathy, myelopathy, nephropathy and rebleeding, have been reported in various case series of IPH.15 Though our patients did not develop any such complications until the last follow-up. However, one patient developed a portal vein thrombosis immediately post-operatively, which resolved on conservative management with subcutaneous heparin. Whereas one patient developed surgical site infection with sepsis that later resolved. Good outcomes have also been shown in case series and long-term studies from India and elsewhere with 90% to 95% shunt patency, rebleeding rates as low as 5% to 10%, and 15-year survival rates of 90%.16
The prognosis of PSRS surgery in IPH, when compared with cirrhotic portal hypertension, is better with operative mortality reported <1% and five-year survival around 80% but these results were found to mostly depend on how well the liver was functioning before surgery, whether the surgery was done electively or as an emergency and if the shunt was still functional and patent after the surgery.17 After an average follow-up period of 26.5 months, we found that all patients were alive with early symptomatic relief, no recurrent bleeding and no long-term complications (Figures 1 and 2).
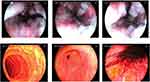 |
Figure 1 Upper GI endoscopy showing grade IV esophageal varices for patient 1 in March 2021. |
 |
Figure 2 Follow up upper GI endoscopy for the same patient 1 done in April/2022 after proximal splenorenal shunt surgery, showing complete resolution of the esophageal varices. |
Limitations of the Study
This is a case series of only four patients, therefore the reported outcomes in these few patients may not mean much statistically but it’s a good start and we recommend a bigger study of this nature in a sub-Saharan setting.
Conclusion
Good outcomes were achieved in terms of symptom resolution, endoscopic variceal resolution at follow-up endoscopy, length of stay ranging from 8 to 15 days and all four patients being alive at the time of follow-up that ranged from 14 to 46 months.
Ethical Approval and Consent
Written informed consent was obtained from all the patients/legal guardians for publication of this case series and the accompanying images. A copy of the written consent is available for review by the Editor-in Chief of this journal on request. Ethical approval was not required for this case series.
Acknowledgment
We thank the operation theatre staff of Lubaga Hospital.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors have no conflicts of interest to declare in this work.
References
1. Schouten JN, Garcia-Pagan JC, Valla DC, Janssen HL. Idiopathic noncirrhotic portal hypertension. Hepatology. 2011;54(3):1071–1081. doi:10.1002/hep.24422
2. Kmeid M, Liu X, Ballentine S, Lee H. Idiopathic non-cirrhotic portal hypertension and porto-sinusoidal vascular disease: review of current data. Gastroenterology Res. 2021;14(2):49–65. doi:10.14740/gr1376
3. Bissonnette J, Garcia-Pagán JC, Albillos A, et al. Role of the transjugular intrahepatic portosystemic shunt in the management of severe complications of portal hypertension in idiopathic noncirrhotic portal hypertension. Hepatology. 2016;64(1):224–231. doi:10.1002/hep.28547
4. Krasinskas AM, Eghtesad B, Kamath PS, Demetris AJ, Abraham SC. Liver transplantation for severe intrahepatic noncirrhotic portal hypertension. Liver Transpl. 2005;11(6):627–634. doi:10.1002/lt.20431
5. Dumortier J, Bizollon T, Scoazec JY, et al. Orthotopic liver transplantation for idiopathic portal hypertension: indications and outcome. Scand J Gastroenterol. 2001;36(4):417–422. doi:10.1080/003655201300051298
6. Wancata LM, Connelly CR, Orloff SL. Portal Hypertension. Curr Surg Manag Dig Dis Interven. 2022;06(02):075–85. doi:10.1055/s-0042-1748021
7. Mishra PK, Patil NS, Saluja S, Narang P, Solanki N, Varshney V. High patency of proximal splenorenal shunt: a myth or reality ? – a prospective cohort study. Int J Surg. 2016;27:82–87. doi:10.1016/j.ijsu.2015.12.071
8. Rajekar H, Vasishta RK, Chawla YK, Dhiman RK. Noncirrhotic portal hypertension. J Clin Experim Hepatol. 2011;1(2):94–108. doi:10.1016/S0973-6883(11)60128-X
9. de Franchis R. Revising consensus in portal hypertension: report of the Baveno V consensus workshop on methodology of diagnosis and therapy in portal hypertension. J Hepatol. 2010;53(4):762–768. doi:10.1016/j.jhep.2010.06.004
10. Khanna R, Sarin SK. Non-cirrhotic portal hypertension – diagnosis and management. J Hepatol. 2014;60(2):421–441. doi:10.1016/j.jhep.2013.08.013
11. Poddar U, Thapa BR, Rao KL, Singh K. Etiological spectrum of esophageal varices due to portal hypertension in Indian children: is it different from the West? J Gastroenterol Hepatol. 2008;23(9):1354–1357. doi:10.1111/j.1440-1746.2007.05102.x
12. Anand U, Kumar R, Priyadarshi RN, Parasar K, John AG. Proximal splenorenal shunt surgery for bleeding gastric varices in non-cirrhotic portal hypertension. Cureus. 2020;12(9):e10464. doi:10.7759/cureus.10464
13. Rajalingam R, Javed A, Sharma D, et al. Management of hypersplenism in non-cirrhotic portal hypertension: a surgical series. Hepatobiliary Pancreat Dis Int. 2012;11(2):165–171. doi:10.1016/S1499-3872(12)60143-X
14. Amarapurkar P, Bhatt N, Patel N, Amarapurkar D. Primary extrahepatic portal vein obstruction in adults: a single center experience. Indian J Gastroenterol. 2014;33(1):19–22. doi:10.1007/s12664-013-0368-4
15. Pal S, Radhakrishna P, Sahni P, Pande GK, Nundy S, Chattopadhyay TK. Prophylactic surgery in non-cirrhotic portal fibrosis:is it worthwhile? Indian J Gastroenterol. 2005;24(6):239–242.
16. Orloff MJ, Orloff MS, Girard B, Orloff SL. Bleeding esophagogastric varices from extrahepatic portal hypertension: 40 years’ experience with portal-systemic shunt. J Am Coll Surg. 2002;194(6):717–728. doi:10.1016/S1072-7515(02)01170-5
17. Marti J, Gunasekaran G, Iyer K, Schwartz M. Surgical management of noncirrhotic portal hypertension. Clin Liver Dis. 2015;5(5):112–115. doi:10.1002/cld.470
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
