Back to Journals » Clinical Ophthalmology » Volume 14
Outcomes of Femtosecond Laser Arcuate Incisions in the Treatment of Low Corneal Astigmatism
Authors Wortz G , Gupta PK , Goernert P, Hartley C , Wortz B, Chiu J, Jaber N
Received 28 May 2020
Accepted for publication 17 July 2020
Published 7 August 2020 Volume 2020:14 Pages 2229—2236
DOI https://doi.org/10.2147/OPTH.S264370
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Video abstract presented by Gary Wortz and Preeya K Gupta.
Views: 733
Gary Wortz,1 Preeya K Gupta,2 Philip Goernert,3 Caleb Hartley,1 Brayden Wortz,2 Jin Chiu,1 Nikita Jaber1
1Commonwealth Eye Surgery, Lexington, KY 40504, USA; 2Duke Eye Center, Durham, NC 27704, USA; 3Department of Psychology, Brandon University, Brandon, MB R7A 6A9, Canada
Correspondence: Gary Wortz
Commonwealth Eye Surgery, 2353 Alexandria Drive #350, Lexington, KY 40504, USA
Tel +1 859 224-2655
Fax +1 859 223-7147
Email [email protected]
Purpose: To evaluate real-world outcomes of astigmatism management with femtosecond laser arcuate incisions in patients with low corneal astigmatism (< 1.0 D) using a novel formula for arcuate incision calculation compared to outcomes after conventional cataract surgery without surgical management of astigmatism.
Patients and Methods: The Wörtz-Gupta™ Formula (available at www.lricalc.com) was used to calculate femtosecond laser arcuate parameters for 224 patients with < 1 D of corneal astigmatism who underwent cataract surgery; lens power was determined with the Barrett Universal II formula. Uncorrected distance visual acuity (UCDVA) and refractive astigmatism measurements were obtained, with an average follow-up of 4 weeks.
Results: The average preoperative cylinder was similar (0.61 D in the femtosecond group [n=124] and 0.57 D in the conventional group [n=100] (P> 0.05)). More patients had ≤ 0.5 D of postoperative corneal astigmatism in the femtosecond group (n=110/124, 89%) than in the conventional group (n=71/100, 71%), respectively (P=0.001). The mean absolute postoperative refractive astigmatism was higher in the conventional surgery group than in the femtosecond group (0.43 ± 0.4 D vs 0.26 ± 0.28 D); these differences were statistically significant (P< 0.001). The percentage of patients with UCDVA of 20/20 or better vision was higher in the femtosecond group (62%) than the conventional group (48%) (P=0.025).
Conclusion: Using the femtosecond laser for arcuate incisions in combination with a novel nomogram can provide excellent anatomic and refractive outcomes in patients with lower levels of preoperative astigmatism at the time of cataract surgery.
Keywords: femtosecond laser-assisted cataract surgery, arcuate incision, visual acuity, refractive outcome, corneal astigmatism
Plain Language Summary
This goal of this study was to analyze the real-world outcome of patients undergoing femtosecond laser assisted cataract surgery (FLACS) with corneal arcuate incisions in the management of low-level astigmatism under 1 diopter. 224 patients (124 study eyes, 100 control eyes) with less than 1D of astigmatism were studied to determine if correcting lower levels of astigmatism would have an impact on post-operative uncorrected visual acuity. It was found that patients who had FLACS with arcuate incisions were 1.8 times more likely to achieve 20/20 uncorrected visual acuity (UCVA) or better and 3.54 times more likely to achieve 20/25 UCVA or better. There was a corresponding statistically significant reduction in pre-operative astigmatism in the treatment group, but not in the control group. This paper provides statistically significant evidence that correcting astigmatism, however it is done, is vitally important to the post-operative vision of cataract patients, even when it is below 1 diopter. Furthermore, it supports that the femtosecond laser is effective in treating low-level astigmatism at the time of cataract surgery.
Introduction
Cataract surgery is one of the most prevalent refractive procedures worldwide annually, and modern refractive cataract surgery aims to provide enhanced uncorrected vision. Reducing or eliminating pre-existing corneal astigmatism is recognized to play an important role in achieving optimal uncorrected visual outcomes after cataract surgery. Astigmatism remains the most common refractive error worldwide, with studies showing that more than 75% of patients have >0.5 D of corneal astigmatism and between 40 and 50% of cataract patients have >1 D.1,2 Correcting corneal astigmatism at the time of cataract surgery has been suggested as a means to provide patients with better refractive outcomes at the time of surgery.3 Several techniques exist to surgically correct astigmatism at the time of cataract surgery, the most common of which is the implantation of toric lenses and corneal arcuate incisions/limbal relaxing incisions that can be created manually or via a femtosecond laser.4–8 However, a large percentage of astigmatism is left untreated at the time of surgery. In a Marketscope Q1 2017 survey of cataract surgeons, 42.8% of patients with ≥1 D of corneal astigmatism were left untreated. For patients with <1 D of astigmatism, the number of patients left untreated is unknown. It is possible that an even greater proportion of patients with these lower levels of astigmatism are left untreated because meaningful evidence to support surgical treatment is lacking.
Corneal arcuate incisions are the most commonly performed procedure for astigmatic reduction of lower levels of astigmatism.8 In the past decade, femtosecond laser-assisted cataract surgery (FLACS) has gained market acceptance and has been shown to be both stable and effective in varying steps throughout the cataract procedure, particularly in more complicated cases.8–11 However, the benefit of the femtosecond laser in creating arcuate incisions in non-complicated cataract surgery cannot be overlooked. Multiple studies have shown the benefit of using femtosecond lasers via penetrating or intrastromal astigmatic keratotomy (AK) to treat corneal astigmatism. Additional studies have found patients with higher levels of preoperative astigmatism have a residual postoperative astigmatism >0.5 D.11–18 This suggests a role for the femtosecond laser in treating lower levels of preoperative astigmatism. For example, Day et al found 32% of eyes that had undergone FLACS with femtosecond laser-produced intrastromal arcuate incisions were able to achieve <0.5 D of astigmatism postoperatively from a baseline of 1.21 ± 0.42 D preoperatively.18 Visco et al used a modified Nichamin-Woodcock nomogram for femtosecond laser-produced penetrating arcuate incisions and showed over 95% of the 189 eyes achieved 0.5 D of postoperative refractive astigmatism, with a preoperative astigmatism range of 0.5 to 2.0 D.19
Little remains known about the outcomes of femtosecond laser arcuate incisions to treat low-level astigmatism. The purpose of this study was to evaluate real-world outcomes of astigmatism management with femtosecond laser arcuate incisions in patients with low corneal astigmatism (<1.0 D) using a novel formula for arcuate incision calculation and compare these outcomes to those from patients who had conventional cataract surgery without surgical management of astigmatism at the time of cataract surgery. A secondary outcome was to report uncorrected visual acuity (UCVA) outcomes. To the best of the authors’ knowledge, this is the first study to evaluate the femtosecond laser for this purpose.
Patients and Methods
This study was a retrospective review of adult subjects who underwent cataract surgery by a single surgeon (GW), between January 1, 2018, and December 31, 2018, who had <1 D of preoperative corneal astigmatism. Patients were divided into two groups: those who opted for FLACS, including surgical correction of astigmatism by femtosecond laser (Catalys Precision Laser System, Johnson & Johnson, Irvine, CA) created arcuate incisions, and those who had conventional cataract surgery and did not have their astigmatism surgically corrected and did not have a toric intraocular lens (IOL) implanted. All patients were targeted for distance vision. To prevent torsional misalignment, all FLACS patients maintained binocular focus on a ceiling target while the laser interface was applied to the eye. This study was approved by the Sterling Institutional Review Board (Atlanta, GA) and was conducted in accordance with the Declaration of Helsinki and the Health Insurance Portability and Accountability Act. A waiver of informed consent was granted due to the retrospective nature of this study.
Arcuate Incision Methods
A novel and proprietary arcuate incision formula was developed for treating patients with <1.0 D of astigmatism using the Wörtz-Gupta™ Formula. Some clinicians have suggested to use a modified Donnenfeld nomogram20 for patients undergoing femto arcuate incisions (compared to manual incisions) by treating 80% of against-the-rule (ATR) and 70% of with-the-rule (WTR) as determined by the online calculator. The novel formula used in this study makes several assumptions: that there will be temporal near-clear corneal incision of ≤2.75 mm, that the ∆K is the difference of anterior keratometry reading on the optical biometry, that ATR is defined by having a steep corneal axis of 0° to 40° or 140° to 180°, and that WTR is defined by having a steep corneal axis of 41° to 139°. In addition, the surgically induced astigmatism (SIA) rate (0.38) was calculated for the single surgeon in this study and has been incorporated into the calculator formula. Given that the SIA was within <0.25 D of the average posterior corneal astigmatism, the net effect was considered to be offsetting. Since this new formula dictates that the incision be placed at 0° in left eyes or 180° in right eyes, the SIA is built into the algorithm.
All patients had optical biometry performed using the Lenstar LS 9000 (Haag Streit, Switzerland) and topography was performed using the OPD-III (Nidek Inc., Tokyo, Japan) to confirm a regular astigmatism pattern. The Barrett Universal II formula was used for all IOL calculations. Arcuate incision parameters included a single nasal arc on steep axis for ATR, and paired arcs on the steep axis for WTR, at 80% depth with a 9.0 mm zone. The Wörtz-Gupta™ Formula is available for free access at www.lricalc.com.
The primary near-clear corneal incision of 2.75 mm was located temporally at 0° or 180° for the majority of patients, though in four of the 124 patients the incision was moved between 0° and 25° (or 180°-205°) so that it would be on axis. All femtosecond laser arcuate incisions were penetrating at 80% depth in the 9.0 mm zone, and all were opened with a Sinsky hook and then irrigated/washed out with a balanced salt solution. All but seven patients received the Lenstec Softec HD, a bi-aspheric IOL that uses an enhanced optic to result in zero spherical aberration. The other seven patients received a Symfony lens (Johnson & Johnson Vision, CA). For the control group, all patients had conventional manual cataract surgery with phacoemulsification, a temporal 2.75 mm near-clear corneal incision, and received the Softec 1 lens.
Only patients records that showed a preoperative astigmatism between 0.25 and 0.99 D and that had complete postoperative data were included in the statistical analysis. Patient records were excluded if patients had been lost to follow-up, if they had other pathology preventing best-corrected visual acuity (BCVA) of less than 20/20, if their astigmatism at the time of surgery was <0.25 D or >1.0 D, or if they received a toric IOL. For the control group, patients were excluded if they had other pathology preventing best-corrected visual acuity of less than 20/20, if their astigmatism at the time of surgery was <0.25 D or >1.0 D, or if they received a toric lens.
Primary Outcome Analysis
The primary outcome was postoperative residual refractive astigmatism. Secondary outcomes included postoperative UCVA (as measured by Snellen), and difference between postoperative spherical equivalent and predicted spherical equivalent from biometry. This was calculated by finding the absolute value of the difference between the postoperative spherical equivalent refraction and the predicted spherical equivalent based on preoperative biometry. Unless otherwise noted, all analyses were calculated using the Pearson Chi-Square test, with a 95% confidence interval. A P-value of <0.05 was considered statistically significant.
Results
There were 224 patient records that met the inclusion criteria. Of these, 124 patients underwent FLACS. There were no statistically significant differences between the two patient groups preoperatively. The average age at the time of femtosecond laser cataract surgery was 66.8 years (range 46.6–85.1 years); there were more females (n=71, 57%) than males (n=53, 43%). For the conventional surgery group, the average age was 68.2 years, and there were 61 females (61%). See Table 1. The average preoperative cylinder was 0.61 D in the femtosecond group and 0.57 D in the conventional surgery group; this was not statistically significant (P > 0.05). Patients were followed for an average of 4 weeks postoperatively.
 |
Table 1 Patient Demographics |
Refractive Outcomes
Postoperative Corneal Astigmatism (Cylinder) Comparison
There was a greater percentage of patients who had ≤0.5 D of postoperative corneal astigmatism in the FLACS group (n=110/124, 89%) than in the conventional cataract surgery group (n=71/100, 71%), respectively; Figure 1A and b). Patients in the FLACS group were 3.2 times more likely than the conventional surgery group to achieve ≤0.5 D of corneal astigmatism postoperatively (95% CI, 1.557–6.490). This difference was statistically significant (P = 0.001).
 |
Figure 1 Preoperative corneal astigmatism and postoperative refractive astigmatism in eyes that underwent femtosecond laser cataract surgery (A) and the conventional cataract surgery (B). |
The mean absolute of the preoperative corneal astigmatism was also similar between the two groups, but the mean absolute postoperative refractive astigmatism was substantially higher in the conventional surgery group (0.43 ± 0.4 D) than in the FLACS group (0.26 ± 0.28 D); these differences were statistically significant (P<0.001; Figure 2A and b).
 |
Figure 2 Double-angle plot for eyes in the femtosecond laser cataract surgery group (A) and the conventional cataract surgery group (B). |
The postoperative refractive astigmatism prediction error (defined as the vector difference between the actual and the predicted postoperative refractive astigmatism)21 also differed between the two groups, with the FLACS group having a much smaller centroid (0.11 D @ 177° ± 0.37 D) than the conventional surgery group (0.20 D @ 176° ± 0.55 D). Figure 3A and B show these differences, although they were not statistically significant (P>0.05).
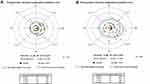 |
Figure 3 Postoperative refractive astigmatism prediction error in femtosecond laser cataract surgery group (A) and the conventional cataract surgery group (B). |
The difference between postoperative spherical equivalent and predicted spherical equivalent from biometry in the FLACS group was −0.112 ± 0.383, compared to −0.176 ± 0.431in the conventional group. This difference was not found to be statistically significant based on t-test (p > 0.05). However, more patients in the FLACS group achieved 20/20 postoperative VA (n=78/124) than in the conventional cataract surgery group (n=48/100): 62.9% vs 48%, respectively (Figure 4). Patients in the FLACS group were 1.8 times more likely than those in the conventional surgery group to achieve 20/20 vision or better postoperatively (95% CI, 1.075–3.138). This difference was statistically significant (P = 0.025). Additionally, more patients in the FLACS group achieved postoperative vision of 20/25 or better (n=107/124) than patients who had conventional cataract surgery (n=64/100): (86.3% vs 64%, respectively). Patients in the femtosecond laser cataract surgery group were 3.54 times more likely than the conventional surgery group to achieve 20/25 vision or better postoperatively (95% CI, 1.84–6.814). This difference was statistically significant (P = 0.001).
 |
Figure 4 Postoperative visual acuity in femtosecond laser vs conventional group. |
Discussion
This study is the first to show efficacy in visual and astigmatic outcomes with a novel nomogram for femtosecond laser-assisted arcuate incisions to treat astigmatism of <1.0 D. Using this new nomogram produced a statistically significant reduction in refractive astigmatism postoperatively, even though these patients had low cylinder preoperatively. More importantly, this reduction in astigmatism led to improved UCVA for those patients when compared to the patients who underwent conventional cataract surgery. The control group used in this retrospective analysis was chosen as the best representation of real-world patients seen in clinics in the US; it was not the intent of this study to compare manual LRI procedures to penetrating limbal arcuate incisions.
It is generally well accepted that astigmatism ≥0.75 D is visually significant, and nomograms consider multiple variables (length, depth, optical zone, number of incisions) to help surgeons perfect the accuracy of their surgical techniques. Our results suggest the novel nomogram can help further reduce astigmatism with the use of a femtosecond laser. In this analysis, all patients had been targeted for distance vision. Postoperatively, there was no difference between the groups in spherical equivalent outcomes. However, there was a statistically significant improvement in residual astigmatism and UCVA in the FLACS group. As wound creation can create up to 0.5 D of astigmatism;22,23 planning to leave even <0.5 D of preoperative corneal astigmatism untreated can result in visually significant postoperative astigmatism. This confirms that low levels of astigmatism, if left untreated, can negatively impact UCVA. Our study suggests that the combined use of the femtosecond laser and a novel formula for arcuate incisions is an effective approach to managing low levels of astigmatism.
Lower levels of astigmatism are highly prevalent, with one UK study finding almost 60% of patients presenting for cataract surgery had <1.0 D (24.47% with 0.5 D or less; 35.12% between 0.51 D and 1.0 D).4 Anecdotally, to determine how common our percentage of patients with a specific axis of astigmatism were in this study’s population compared to the overall patient population, the authors evaluated 10,307 scans with complete data from all preoperative patients from the same single center as was used for this study’s population (unpublished data). The average astigmatism was 1.07 D, but 50.9% of patients had between 0.25 and 0.99 D of astigmatism (n=5,251). This correlates with other published studies.4,24 If we consider the data to be a normalized set and extrapolate it to a larger population, it suggests that about 50% of cataract patients have lower levels of astigmatism that may benefit from the combination of femtosecond laser-assisted arcuate incisions derived from the novel nomogram. Further, the magnitude and axis of postoperative astigmatism can influence perceived patient satisfaction and overall refractive outcomes.3 Yet the benefit to patients of correcting <0.5 D has been questioned.25
There are numerous published nomograms for manually constructed LRIs, including online calculators, but their applicability in femtosecond laser-created AKs is unknown. Little has been reported on femtosecond laser-created AKs, and even less in eyes with <1.0 D of preoperative astigmatism. Chan et al11 reported on a modified Wallace LRI nomogram, where 33% of the subjects had ≤0.5 D postoperatively, but noted further revising the nomogram could have improved outcomes even further. Baharozian et al26 allowed for preoperative astigmatism between 0.25 and 2.0 D, and 50% of the 161 patients had a postoperative astigmatism of ≤0.5 D, most commonly in the oblique astigmatism group. Those authors found their modified nomogram to be optimized for ≤1.25 D, and that an increase in the magnitude or reduction of the optical zone size may further improve refractive outcomes.
This study is not without its limitations. First, the study is retrospective, thus impacting follow-up time. The patients were followed for a typical postoperative period; however, they were not followed longitudinally as could be seen in a long-term prospective analysis. While unlikely, there is the possibility that outcomes would differ if all patients had undergone a stricter follow-up schedule or were followed for a greater time period prospectively. Similarly, there was a difference in IOLs used in our patients, which may have affected outcomes. We chose to include all patients regardless of IOL used to better reflect real-world situations. However, since both IOLs used for the overwhelming majority of cases are monofocal lenses, we do not believe this would have impacted the measurement of postoperative astigmatism. In the future, prospective studies with larger sample size and longitudinal follow-up will allow for further refinement of the nomogram. While there is some suggestion that limbal relaxing incisions may regress over time, femtosecond laser-created arcuate incisions have shown both early and late stability with no change for upwards of 5 years.27 The authors believe the strengths of the study more than outweigh these few limitations.
Conclusion
The present study shows that using the femtosecond laser for corneal arcuate incisions using a novel nomogram can provide excellent anatomic and refractive outcomes in patients with lower levels of preoperative astigmatism at the time of cataract surgery. Surgeons should consider correcting lower levels of astigmatism to achieve the best UCVA.
Acknowledgment
This was an investigator-initiated analysis with no commercial support. Michelle Dalton, ELS, of Dalton & Associates, Inc., provided medical writing and editorial assistance; this support was funded by the investigators.
Disclosure
The authors report no conflicts of interest in this work. This was an investigator-initiated study that received no outside financial support.
References
1. Vitale S, Ellwein L, Cotch MF, Ferris FL
2. Michelitsch M, Ardjomand N, Vidic B, Wedrich A, Steinwender G. [Prevalence and age-related changes of corneal astigmatism in patients before cataract surgery] [article in German]. Ophthalmologe. 2017;114(3):247–251. doi:10.1007/s00347-016-0323-8. German.
3. Wolffsohn JS, Bhogal G, Shah S. Effect of uncorrected astigmatism on vision. J Cataract Refract Surg. 2011;37(3):454–460. doi:10.1016/j.jcrs.2010.09.022
4. Khan MI, Muhtaseb M. Prevalence of corneal astigmatism in patients having routine cataract surgery at a teaching hospital in the United Kingdom. J Cataract Refract Surg. 2011;37(10):1751–1755. doi:10.1016/j.jcrs.2011.04.026
5. Ferrer-Blasco T, Montés-Micó R, Peixoto-de-Matos SC, González-Méijome JM, Cerviño A. Prevalence of corneal astigmatism before cataract surgery. J Cataract Refract Surg. 2009;35(1):70–75. doi:10.1016/j.jcrs.2008.09.027
6. Byun YS, Kim S, Lazo MZ, et al. Astigmatic correction by intrastromal astigmatic keratotomy during femtosecond laser-assisted cataract surgery: factors in outcomes. J Cataract Refract Surg. 2018;44(2):202–208. doi:10.1016/j.jcrs.2017.11.018
7. Kessel L, Andresen J, Tendal B, Erngaard D, Flesner P, Hjortdal J. Toric intraocular lenses in the correction of astigmatism during cataract surgery: a systematic review and meta-analysis. Ophthalmology. 2016;123(2):275–286. doi:10.1016/j.ophtha.2015.10.002
8. Rückl T, Dexl AK, Bachernegg A, et al. Femtosecond laser-assisted intrastromal arcuate keratotomy to reduce corneal astigmatism. J Cataract Refract Surg. 2013;39(4):528–538. doi:10.1016/j.jcrs.2012.10.043
9. Chan TC, Ng AL, Cheng GP, Wang Z, Woo VC, Jhanji V. Corneal astigmatism and aberrations after combined femtosecond-assisted phacoemulsification and arcuate keratotomy: two-year results. Am J Ophthalmol. 2016;170:83–90. doi:10.1016/j.ajo.2016.07.022
10. Vickers LA, Gupta PK. Femtosecond laser-assisted keratotomy. Curr Opin Ophthalmol. 2016;27(4):277–284. doi:10.1097/ICU.0000000000000267
11. Chan TC, Cheng GP, Wang Z, Tham CC, Woo VC, Jhanji V. Vector analysis of corneal astigmatism after combined femtosecond-assisted phacoemulsification and arcuate keratotomy. Am J Ophthalmol. 2015;160(2):250–255 e2. doi:10.1016/j.ajo.2015.05.004
12. Harissi-Dagher M, Azar DT. Femtosecond laser astigmatic keratotomy for postkeratoplasty astigmatism. Can J Ophthalmol. 2008;43(3):367–369. doi:10.3129/i08-043
13. Nubile M, Carpineto P, Lanzini M, et al. Femtosecond laser arcuate keratotomy for the correction of high astigmatism after keratoplasty. Ophthalmology. 2009;116(6):1083–1092. doi:10.1016/j.ophtha.2009.01.013
14. Wetterstrand O, Holopainen JM, Krootila K. Treatment of postoperative keratoplasty astigmatism using femtosecond laser-assisted intrastromal relaxing incisions. J Refract Surg. 2013;29(6):378–382. doi:10.3928/1081597X-20130515-01
15. Nejima R, Terada Y, Mori Y, Ogata M, Minami K, Miyata K. Clinical utility of femtosecond laser-assisted astigmatic keratotomy after cataract surgery. Jpn J Ophthalmol. 2015;59(4):209–215. doi:10.1007/s10384-015-0383-3
16. Yoo A, Yun S, Kim JY, Kim MJ, Tchah H. Femtosecond laser-assisted arcuate keratotomy versus toric IOL implantation for correcting astigmatism. J Refract Surg. 2015;31(9):574–578. doi:10.3928/1081597X-20150820-01
17. St Clair RM, Sharma A, Huang D, et al. Development of a nomogram for femtosecond laser astigmatic keratotomy for astigmatism after keratoplasty. J Cataract Refract Surg. 2016;42(4):556–562. doi:10.1016/j.jcrs.2015.12.053
18. Day AC, Lau NM, Stevens JD. Nonpenetrating femtosecond laser intrastromal astigmatic keratotomy in eyes having cataract surgery. J Cataract Refract Surg. 2016;42(1):102–109. doi:10.1016/j.jcrs.2015.07.045
19. Visco DM, Bedi R, Packer M. Femtosecond laser-assisted arcuate keratotomy at the time of cataract surgery for the management of preexisting astigmatism. J Cataract Refract Surg. 2019;45(12):1762–1769. doi:10.1016/j.jcrs.2019.08.002
20. Donnenfeld E, Rosenbert E. Assisting femto incisions with nomograms. Ophthalmo Management. [online]. Https://Www.Ophthalmologymanagement.Com/Issues/2015/June-2015/Assisting-Femto-Incisions-with-Nomograms.
21. Abulafia A, Koch DD, Holladay JT, Wang L, Hill W. Pursuing perfection in intraocular lens calculations: IV. Rethinking astigmatism analysis for intraocular lens-based surgery: suggested terminology, analysis, and standards for outcome reports. J Cataract Refract Surg. 2018;44(10):1169–1174. doi:10.1016/j.jcrs.2018.07.027
22. Gross RH, Miller KM. Corneal astigmatism after phacoemulsification and lens implantation through unsutured scleral and corneal tunnel incisions. Am J Ophthalmol. 1996;121(1):57–64. doi:10.1016/S0002-9394(14)70534-3
23. Hill W. Expected effects of surgically induced astigmatism on AcrySof toric intraocular lens results. J Cataract Refract Surg. 2008;34(3):364–367. doi:10.1016/j.jcrs.2007.10.024
24. Curragh DS, Hassett P. Prevalence of corneal astigmatism in an NHS cataract surgery practice in Northern Ireland. Ulster Med J. 2017;86(1):25–27.
25. Villegas EA, Alcón E, Artal P. Minimum amount of astigmatism that should be corrected. J Cataract Refract Surg. 2014;40(1):13–19. doi:10.1016/j.jcrs.2013.09.010
26. Baharozian CJ, Song C, Hatch KM, Talamo JH. A novel nomogram for the treatment of astigmatism with femtosecond-laser arcuate incisions at the time of cataract surgery. Clin Ophthalmol. 2017;11:1841–1848. doi:10.2147/OPTH.S141255
27. Krader CG. Laser cataract surgery making complex cases more routine. Ophthalmol Times. [online]. https://www.ophthalmologytimes.com/article/laser-cataract-surgery-making-complex-cases-more-routine.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
