Back to Journals » Clinical Ophthalmology » Volume 14
Outcomes and Adverse Events of Sub-Tenon’s Anesthesia with the Use of a Flexible Cannula in 35,850 Refractive Lens Exchange/Cataract Procedures
Authors Lerch D, Venter JA, James AM, Pelouskova M, Collins BM , Schallhorn SC
Received 16 October 2019
Accepted for publication 11 December 2019
Published 31 January 2020 Volume 2020:14 Pages 307—315
DOI https://doi.org/10.2147/OPTH.S234807
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Dagobert Lerch, 1, 2 Jan A Venter, 2 Anca M James, 1, 2 Martina Pelouskova, 2 Barrie M Collins, 2 Steven C Schallhorn 2–4
1Montanamed Ltd., Sankt Gallen, Switzerland; 2Optical Express, Glasgow, UK; 3University of California, Department of Ophthalmology, San Francisco, CA, USA; 4Carl Zeiss Meditec, Dublin, CA, USA
Correspondence: Dagobert Lerch
Montanamed Ltd, Ozartstraße 6, Leipzig D-04107, Germany
Tel +49 152 53447537
Email [email protected]
Purpose: To describe our technique of sub-Tenon’s anesthesia and report adverse events and patient comfort.
Setting: Optical Express, United Kingdom.
Design: Retrospective case series.
Methods: The outcomes of 35,850 intraocular procedures (phacoemulsification and implantation of an intraocular lens) were retrospectively reviewed and the incidence of adverse events related to sub-Tenon’s anesthesia was calculated. On the first postoperative day, patients were asked to complete a questionnaire enquiring about their comfort during and after the procedure. The anesthetic solution consisted of a combination of Lidocaine and Hyaluronidase, which was administered into sub-Tenon’s space with a single-use sterile polyurethane 22G x 1” (0.9 x 25 mm) cannula. Mild conscious sedation (midazolam) was used during anesthetic and surgical procedure.
Results: No significant adverse events that would affect the posterior segment of the eye or result in vision loss were recorded. Subconjunctival haemorrhage related to sub-Tenon’s anesthesia was noted in 4.3% of eyes. Five minutes after the administration of sub-Tenon’s block, 80.6% of eyes had no chemosis, 14.8% had chemosis that affected only 1 quadrant of the eye and 4.5% of eyes had chemosis affecting 2 or more quadrants of the eye. Other adverse events included 14 cases of cyst/granuloma formation in the area of sub-Tenon’s incision and 7 eyes required suturing of the conjunctival cut. Of all patients, 93.2% experienced no or only mild discomfort during or after surgical procedure.
Conclusion: Sub-Tenon’s anesthesia with the use of a flexible cannula is a safe option for ophthalmic anesthesia. No sight-threatening adverse events occurred.
Keywords: sub-Tenon’s anesthesia, flexible cannula, refractive lens exchange, adverse events
Introduction
Various ophthalmic procedures are commonly performed as outpatient surgeries under local anesthesia.1–3 In the past, peribulbar and retrobulbar blocks were frequently used techniques; however, they have been associated with rare, but significant sight-threatening adverse events related to the use of a sharp needle.1–4
Sub-Tenon’s anesthesia has emerged as a safer alternative to ophthalmic blocks, as it is performed with a blunt cannula as opposed to a sharp needle. The technique was first time described in 18845 but gained popularity in the early 1990s6 and variations of the techniques have been described with the use of different cannulae.7–11
Although sub-Tenon’s anesthesia is relatively safe, it is associated with some common and minor complications, most commonly chemosis or subconjunctival hemorrhage.4 It has also been associated with extremely rare but sight-threatening or even life-threatening complications, such as brainstem anesthesia, globe perforation, orbital or retrobulbar hemorrhage, retinal ischemia, optic nerve damage or rectus muscle dysfunction.4 These are mostly the result of inappropriate technique, forceful injection and usually associated with the use of a metal cannula.12 An alternative use of flexible plastic cannula has been advocated to improve the safety of the technique.6,8,12
In this study, we describe our own technique with the use of a flexible cannula and present adverse events and patient comfort in a large population of patients undergoing refractive lens exchange or cataract surgery.
Patients and Methods
This study was deemed exempt from full review by the Committee on Human Research at the University of California, San Francisco, because it used only retrospective, de-identified patient data. All patients provided informed consent to undergo refractive lens exchange or cataract surgery and agreed to use their de-identified data for statistical analysis. The study adhered to the Declaration of Helsinki.
Data of all patients that underwent refractive lens exchange or cataract surgery between May 2013 and December 2017 were extracted from the electronic medical record of Optical Express. The extracted variables were patient’s demographics (age and gender), preoperative clinical data (refraction and visual acuity), adverse events (AEs), anesthesia details (dosage of anesthetic solution and sedation) and day one postoperative patient experience questionnaire. Intraoperative adverse events were recorded by either the surgeon, nurse, or healthcare assistants (surgical technicians) present in the operating room during surgery. Postoperatively, patients were seen by either the surgeon or qualified refractive optometrists who identified and recorded any AEs.
Adverse events were subsequently reviewed searching for any events associated with the local anesthesia (such as subconjunctival hemorrhage, or any events related to the anterior or posterior segment of the eye associated with the anesthesia). All patients were asked to complete day 1 postoperative questionnaire, where one of the questions was “Did you experience any discomfort during or after surgery” with the possible answers ranging between 0 (no discomfort at all) to 3 (severe discomfort).
Additionally, rates of chemosis and achieved akinesia were monitored in a subset of 1920 consecutive eyes treated between 1st April 2017 and 30th June 2017. Chemosis was calculated according to the number of affected eye quadrants on a scale between 0 (no chemosis at all) to 4 (chemosis affecting 4 quadrants), and it was assessed 5 mins after the injection of anesthetic solution. Sub-Tenon’s block performance was also evaluated 5 mins after anesthetic solution administration. The patient was asked to try to look up, down, to the right and to the left and the quality of the block was scored on the following scale: 1 – good: full akinesia achieved, no movement of the eye globe in any direction possible, 2 – moderate: slight movement of the eye globe, but satisfactory to proceed with surgery, 3 – poor: substantial movement of the eye globe requiring additional injection of anesthetic solution.
Surgical Technique
Patients first underwent lens fragmentation and capsulorhexis with a femtosecond laser (Catalys Precision Laser System, Johnson & Johnson Vision Care, Inc, Santa Ana, CA) with the use of topical proxymetacaine hydrochloride 0.5%w/v. Prior to anesthetic procedure, each patient was seen and assessed by an anesthetist. Patient was then moved into anesthetic room, placed into supine position and standard monitoring was applied. All patients had intravenous cannula sited and the left in place until their postoperative discharge. Intravenous sedation (Midazolam) was then administered. The amount of Midazolam varied between patients. Generally, 1.0–1.5mg initial dose was used and, if necessary (depending on patient’s anxiety), the dose increased by 0.50 or 1.0mg every 5 to 10 mins. The maximum dose was limited by establishing a conscious sedation and, if necessary, adjusted for existing medical conditions. From previous experience of patient’s increased awareness of procedure during second-eye surgery, the dose of midazolam was increased by up to 50% for second-eye surgery. The second-eye surgery was typically performed 1 to 7 days after 1st eye surgery. All patients received supplementary oxygen therapy throughout their stay in the operating suite.
For the sub-Tenon’s block, the conjunctiva was first anesthetized with a drop of topical proxymetacaine hydrochloride 0.5%w/v and cleaned with povidone iodine solution. A wire speculum was inserted into the eye, and the patient was instructed to look up and out for the anesthetist to access the inferonasal quadrant. A small piece of conjunctiva and Tenon capsule was raised with a pair of fine tooth forceps (Fine Straight Toothed Forceps, Surgitrack Instruments, Hongkong) and a small incision was made with the pair of scissors (Westcott Type Conjunctival Scissors, Surgitract instruments, Hongkong), exposing the sclera below (Figure 1).
 |
Figure 1 Conjunctival cut. |
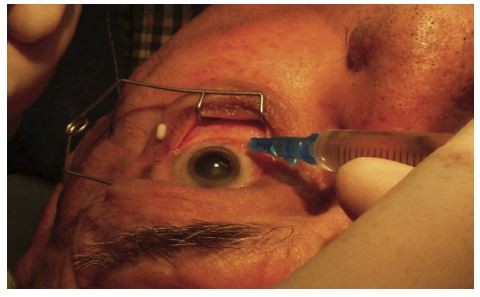
Polyurethane cannula (attached to a syringe with anesthetic solution) was then inserted into the incision and passed posteriorly (Figure 2). Anesthetic solution was then injected. (Lidocaine 2% 2.5–3 mL with Hyaluronidase between 15 units up to 100 units). No pressure was applied on the eye following the injection of anesthetic solution.
 |
Figure 2 Insertion of cannula and injection of anesthetic solution. |
To avoid subconjunctival hemorrhage, a cellulose spear (Eye Spears, Bazever-Visitec International Inc, Waltham, USA) was placed under the lower eyelid on the area of conjunctival cut (Figure 3). The spear was replaced after 2 mins and left in place for as long as the bleeding continued. In most of the cases, only one replacement of the spear was necessary, but if bleeding continued, spears were replaced every 2 mins as many times as it was necessary to stop the bleeding.
 |
Figure 3 Anti-hemorrhage technique. |
The cannula used for injection of anesthetic solution (Figure 4) was Introcan® Certo (B. Braun Melsungen AG, Germany). This is a single use 22G x 1” (0.9 x 25 mm) sterile polyurethane cannula with no port and wings usually used as a pediatric IV indwelling cannula.
 |
Figure 4 Cannula used for sub-Tennon’s block. |
Anesthetic blocks were performed by 12 anesthetists in 21 surgical locations and they all were trained by two experienced anesthetists (D.L or A.M.J.) and strictly supervised until they became confident with the technique.
Statistical Analysis
All adverse events related to sub-Tenon’s anesthesia were reviewed and the incidence was calculated on “per eye” basis. Outcomes of postoperative questionnaire referring to the discomfort during or after surgery were analysed on “per procedure” basis and the correlation between patient-reported discomfort and basic preoperative demographics and clinical data (age, amount of preoperative myopia and hyperopia) was calculated. For binary variables (such as gender or first and second eye), a student’s t-test was used to compare patient-reported discomfort. Chi-square test was used to compare percentages. All calculations were performed with Microsoft Office Excel 2011 program (Microsoft Corp.) and STATISTICA software (StatSoft Inc.).
Preoperative Demographics and Clinical Data
The total number of sub-Tenon’s blocks performed between May 2013 and December 2017 was 35,850 (35,850 eyes of 20,277 patients). The mean age of patients at the time of surgery was 57.9 ± 7.8 (from 23 to 93 years). The age distribution is presented in Figure 5. Male to female ratio was 50.5% (n=10,240 patients) to 49.5% (n=10,037 patients). Of all patients, 94.1% (n=33,735 procedures) underwent refractive lens exchange (for refractive reason, with minimal or no cataract lens changes but corrected distance visual acuity not worse than 20/25) and the remaining 5.9% (n=2115 procedures) had visually significant cataract.
 |
Figure 5 Age at the time of surgery. |
The percentage of eyes with preoperative myopic refractive error was 15.8% (n=5664 eyes) and 84.2% (n=30,186 eyes) of eyes had hyperopia. The mean preoperative myopic refraction was −3.65 ± 3.12 D (−0.25 D to −21.0 D) and the mean preoperative hyperopic refraction was +2.47 ± 1.70 D (+0.25 D to +13.5 D).
Adverse Events
There were no postoperative adverse events that would affect posterior segment of the eye or resulting in vision loss. No systemic complications occurred in the presented population of patients. There were 14 cases (14 eyes or 14 patients, incidence 0.04%, 1:2561 eyes) of cyst or granuloma formation in the area of sub-Tenon’s incision. These were usually managed with the use of topical steroid drops, except for one case, which required surgical extraction. Additionally, 7 eyes of 7 patients (incidence 0.02%, 1:5121 eyes) required suturing of the conjunctival cut, because the opening incision in conjunctiva was larger than usual and caused irritation, discomfort and prolonged healing.
Subconjunctival haemorrhage related to sub-Tenon’s anesthesia was evaluated based on day 1 clinical outcomes and recorded in 4.3% of cases (n=1542 eyes, incidence 1:23 eyes).
Figure 6 shows the chemosis rates for the subset of 1920 patients. Most of the patients had no chemosis or only chemosis affecting one quadrant of the eye (usually temporal-inferior). Three or four quadrant chemosis was rare and there was no case of chemosis necessitating surgery cancellation.
 |
Figure 6 Chemosis assessed 5 mins after the administration of anesthetic solution. |
Akinesia and sub-Tenon’s block quality is evaluated in Figure 7. The vast majority of patients achieved full akinesia 5 mins following administration of anesthetic solution, and only a very small number of patients required an additional injection of anesthetic solution. No correlation was found between the quality of sub-Tenon’s block and the presence and severity of chemosis. As an example, 4.3% of eyes with a good quality block, 6.8% of eyes with a moderate quality block, and 5.6% of eyes with a poor quality block had chemosis affecting two or more quadrants of the eye (p = 0.26).
Questionnaire Outcomes
The mean score for patient discomfort (measured on scale between 0 and 3) was 0.62 ± 0.63. Of all patients 93.2% (n=33,412 procedures) experienced no or mild discomfort, 6.1% (n=2187 procedures) experienced moderate discomfort and 0.7% (n=251 procedures) experienced severe discomfort. Patients who experienced severe discomfort usually referred to the discomfort after surgery (for example burning sensation when instilling eye drops).
There was no statistically significant correlation between patient’s age, or between the amount of preoperative myopia and hyperopia (which is usually correlated to the axial length of the eye) and discomfort score. The only variable associated with the discomfort was first or second eye surgery. The mean score for discomfort during first eye surgery was 0.60 ± 0.62 and 0.69 ± 0.57 for second eye surgery (p<0.01), despite the increased dose of midazolam during second eye surgery.
Discussion
Local anesthesia is an important part of many ophthalmic procedures. There are several choices of local anesthetic techniques, from simple topical anesthesia to needle/cannula techniques that induce akinesia. Nowadays, cataract surgery is increasingly performed with the assistance of femtosecond lasers and the use of foldable lenses; therefore, topical anesthesia is regaining popularity for its cost-effectiveness and fewer side effects. However, topical anesthesia has some important limitations: it requires patient’s cooperation, greater surgical skills, and may have inconstant efficiency. Most importantly, patients experience greater discomfort during surgery.13,14 It can also potentially have an impact on the incidence of intraoperative adverse events in non-compliant patients.13,14
In private cataract surgery or refractive lens exchange, great emphasis is placed on patient’s journey, experience and comfort. Additionally, many surgeons in our practice indicated that the surgery is technically easier if akinesia is achieved with local anesthesia, which is the reason why sub-Tenon’s anesthesia with mild sedation is the main technique in our clinical practice. However, refining this technique and reducing the number of adverse events is of utmost importance.
From the choice of cannulae available for sub-Tenon’s block, 2.54cm Stevens-type metal cannula is still the most frequently used.6 The use of a polyethylene plastic cannula was first described by Greenbaum in 1992.11 This was a 14 gauge cannula with an approximate length of 10 mm. The advantage of this cannula was that it was flexible, atraumatic and delivered anesthetic solution into anterior sub-Tenon’s space, thus minimizing the risk of potential trauma to the structures begin the globe.5,11 The disadvantage of the short length of this cannula was mainly increased risk of chemosis and conjunctival hemorrhage.5
Because polyethylene cannula had major advantages of being flexible and atraumatic, but had the shortcomings described above, there have been attempts to develop a longer cannula made of polyethylene plastic, intended to deliver anesthetic solution into mid/posterior sub-Tenon’s space. In 2001, Kumar and Dodds,8 in an attempt to design their own cannula, accidentally came across a polyethylene cannula used in plastic surgery. The cannula had a 22 gauge, internal diameter of 0.41 mm and a total length of 40 mm. The cannula had a proximal hub portion (10 mm), a middle taper portion (12 mm), a distal straight portion (18 mm) and round blunt tip and was great the purpose of delivering anesthetic agent into mid sub-Tenon’s space.
The pediatric intravenous cannula we use in our practice has some great advantages. Compared to the one used by Kumar and Dodds8 it is sterile, single use and cheap. The cannula is 25 mm long and has no port or wings that would obstruct the view and handling of anesthetist. The length of the cannula is sufficient to safely deliver anesthetic solution to the posterior sub-Tenon’s space, and due to its flexibility, there is no concern about perforation or damage to the structures of the eye.
In this review, we have not found any significant adverse events related to the use of sub-Tenon’s anesthesia. There were a few adverse events related to the conjunctival cut which were extremely rare considering the large number of performed procedures, and other minor events included chemosis and subconjunctival hemorrhage. However, their incidence was very low compared to that reported in the previous literature. There was no vision loss recorded as a result of sub-Tenon’s anesthesia.
Chemosis (swelling or ballooning of the conjunctiva) is common and it is considered to be a minor complication of sub-Tenon’s anesthesia. Only in a small number of cases reported in the literature was chemosis significant enough to interfere with surgery. For example, Guise et al15 retrospectively evaluated 6000 sub-Tenon’s blocks and found that in only 0.06% cases edema interfered with the ophthalmic surgery. The main cause of chemosis is the spread of anesthetic solution into the anterior sub-Tenon’s space, and can be minimized by administering local anesthetic solution mainly into the posterior sub-Tenon’s space. With the use of a long cannula, the reported incidence rate ranges between 5.6% and 39.4%15,16 and can be significantly higher with shorter cannulae.17 However, the comparison of literature is difficult because many authors do not report on the severity of chemosis. Also, chemosis might not always be obvious immediately after the administration of anesthetic solution, and its incidence might vary depending on the time point at which it is recorded. With our technique and the length of the cannula, we achieved minimal chemosis and there was no case of significant chemosis that would lead to cancellation of surgery. We believe that correct identification of sub-Tenon’s space is mandatory for reducing the incidence of chemosis. Proper insertion of a flexible cannula through all layers is also important, and in our opinion, significantly reduces chemosis compared to the metal cannula, where the liquid is often applied between tissue layers. A correct application also minimizes efflux of anesthetic solution, and we found this to be minimal with our technique.
In order to minimize, or possibly completely eliminate the incidence of chemosis, we are currently investigating the effect of dividing the dose of anesthetic solution. We noticed that when a single dose application of a 3.0mL local anesthetic is split into two separate applications approximately 3 mins apart, the sub-Tenon’s block outcome (in terms of achieved akinesia) is equivalent to a single dose application, while the incidence of chemosis is significantly reduced. A similar technique has been previously described by Khan at al,18 but opposite outcomes were found so the authors concluded that a single dose is superior to a divided dose of anesthetic solution. However, anesthetic solution used in the study was different from ours (lignocaine with adrenaline, bupivacaine and hyaluronidase) and there was only a limited number of patients (30 in each group). For that reason, the technique requires further investigation.
Subconjunctival hemorrhage is a minor complication of sub-Tenon block and the reported incidence greatly varies in the literature (7.4%15 32%19 56%16 100%17). Subconjunctival hemorrhage is caused by fine vessels cut on making the conjunctival opening. Larger bleeds may be caused by damage to vortex veins in the posterior sub-Tenon’s space, mainly if a rigid cannula is used.5 Some techniques have been proposed to reduce the incidence of subconjunctival hemorrhage. Kumar and Dowd proposed the use of vasoconstrictor-soaked cotton buds to limit the spread of haemorrhage.4 Gauba et al20 demonstrated a significant reduction in subconjunctival haemorrhage (especially in patients with known coagulopathy) using controlled conjunctival cautery. This was performed by an ophthalmologist under the operating microscope in the area of sub-Tenon’s conjunctival entry site, prior to tissue dissection. However, Kumar et al21 have not found any benefit of cautery when this was applied by an anesthetist. Our technique of preventing hemorrhage is simple and non-invasive with very good outcomes. We used a simple cellulose spear (without the use of adrenaline or vasoconstrictor), kept in the place as long as bleeding persisted. Previous techniques mostly concentrated on bleeding prevention, whereas our technique aims to drain the blood until there is none left to cause hemorrhage. The reported incidence of subconjunctival hemorrhage was less than 5%, usually confined to the incision area, and did not interfere with surgery in any single case.
The postoperative questionnaire on pain experienced during and after surgery revealed an absence of association with any clinical parameters other than the timing of surgery (first or second eye surgery). We found a subtle, but statistically significant increase in pain in patients undergoing second eye surgery. This has previously been reported for various types of ophthalmic anesthesia22–27 and is likely to be related to the lower preoperative anxiety prior to second eye surgery,25,26 or amnestic effect of intravenous sedation.26
In this study, sub-Tenon’s anesthesia achieved great results with complete akinesia and we highlighted some advantages of this technique over cataract/refractive lens exchange performed with topical anesthesia only. There is a new challenge in intraocular surgery at the moment with the advent of immediate sequential bilateral cataract surgery (ISBCS) and its progressive acceptance in modern ophthalmic practice,28 our clinics including. With this approach, full sub-Tenon’s block is not practical, as it would result in postoperative diplopia and therefore topical anesthesia is often the preferred choice. However, we are currently investigating a technique called analgetic sub-Tenon’s block (ASTB). In sub-Tenon’s anesthesia, the nerve blocking, reduction of pain and motoric function/akinesia depend on the concentration of the local anesthetic solution. On the other hand, the spread of anesthesia and its duration depend on the volume applied. In our new ASTB technique, we use 0.5% of Lidocaine concentration and a 2.0 mL volume of local anesthetic solution and achieve some advantages of sub-Tenon’s block (elimination of pain, patient unable to squeeze the eye and blink and at least partial akinetic effect) without inducing postoperative diplopia. This, in combination with mild conscious sedation, significantly improves patient’s journey during ISBCS compared to topical anesthesia; however, the technique will be discussed and further analysed in our future studies.
Our study had a few limitations. It was retrospective and there is a possibility some of the adverse events might have been under-reported or patients were lost to follow-up. However, adverse events related to anesthesia either manifest on the day of surgery or on early follow-ups, which are attended by most of our patients (99.9% of patient attend day 1 follow-up). Optical Express electronic medical system has strict procedures for recording of any significant adverse events that might result in vision loss, for that reason, it is unlikely any sight-threatening adverse events have been missed. Another limitation of the study was that it was mostly performed on younger patients with minimal or no cataract changes who underwent the procedure for refractive reasons. Such procedures generally require shorter surgical time compared to the removal of a mature cataract. However, the technique described in the paper offers a minimum of 40 mins of lasting effect, which should be sufficient to operate on more complicated cases. A small percentage of patients in this study had a dense cataract and the sub-Tenon’s technique was used with no issues.
The other limitation of our study is the use of a non-validated questionnaire, which refers to the discomfort during and after the procedure. This does not accurately evaluate discomfort related to anesthesia. If patients experienced some discomfort during the procedure, they had an option to write comments to describe the discomfort, and these comments were usually related to postoperative rather than intraoperative pain. For this reason, we can assume that discomfort related to the actual anesthesia was minimal.
Despite some limitations, this is one of the largest studies presenting the outcomes of sub-Tenon’s anesthesia with the use of a flexible cannula. We believe that with appropriate training this technique is extremely safe and generally improves the patient’s journey.
Disclosure
Steven C Schallhorn is a Chief Medical Officer for, and received personal fees from Carl Zeiss Meditec, he is also a chairman of Medical Advisory Board for Optical Express. None of the other authors have a financial or proprietary interest in the products and materials presented in this paper. The authors report no other conflicts of interest in this work.
References
1. Malik A, Fletcher EC, Chong V, Dasan J. Local anesthesia for cataract surgery. J Cataract Refract Surg. 2010;36(1):133–152. doi:10.1016/j.jcrs.2009.10.025
2. Navaleza JS, Pendse SJ, Blecher MH. Choosing anesthesia for cataract surgery. Ophthalmol Clin North Am. 2006;19(2):233–237. doi:10.1016/j.ohc.2006.02.001
3. Nouvellon E, Cuvillon P, Ripart J, Viel EJ. Anaesthesia for cataract surgery. Drugs Aging. 2010;27(1):21–38. doi:10.2165/11318590-000000000-00000
4. Kumar CM, Dowd TC. Complications of ophthalmic regional blocks: their treatment and prevention. Ophthalmologica. 2006;220(2):73–82. doi:10.1159/000090570
5. Guise P. Sub-tenon’s anesthesia: an update. Local Reg Anesth. 2012;5:35–46. doi:10.2147/LRA.S16314
6. Kumar CM, Eid H, Dodds C. Sub-tenon’s anaesthesia: complications and their prevention. Eye (Lond). 2011;25(6):694–703. doi:10.1038/eye.2011.69
7. Allman KG, Theron AD, Byles DB. A new technique of incisionless minimally invasive sub-tenon’s anaesthesia. Anaesthesia. 2008;63(7):782–783. doi:10.1111/j.1365-2044.2008.05592.x
8. Kumar CM, Dodds C. A disposable plastic sub-tenon cannula. Anaesthesia. 2001;56(4):399–400. doi:10.1046/j.1365-2044.2001.01976-48.x
9. Mather CM. Comparison of i.v. cannula and Stevens’ cannula for sub-tenon’s block. Br J Anaesth. 2007;99(3):421–424. doi:10.1093/bja/aem162
10. McNeela BJ, Kumar CM. Sub-tenon’s block with an ultrashort cannula. J Cataract Refract Surg. 2004;30(4):858–862. doi:10.1016/S0886-3350(03)00555-8
11. Greenbaum S. Parabulbar anesthesia. Am J Ophthalmol. 1992;114(6):776. doi:10.1016/S0002-9394(14)74066-8
12. Riad W, Ahmad N, Kumar CM. Comparison of metal and flexible sub-tenon cannulas. J Cataract Refract Surg. 2012;38(8):1398–1402. doi:10.1016/j.jcrs.2012.03.035
13. Vielpeau I, Billotte C, Kreidie J, Lecoq P. Comparative study between topical anesthesia and sub-tenon’s capsule anesthesia for cataract surgery. J Fr Ophtalmol. 1999;22(1):48–51.
14. Ioannidis AS, Papageorgiou K, Alexandraki KI, Massaoutis P, Sinha AJ, Andreou PS. Light sensitivity and pain sensation during cataract surgery. A comparative study of two modes of anaesthesia. Int Ophthalmol. 2010;30(6):703–707. doi:10.1007/s10792-010-9344-5
15. Guise PA. Sub-tenon anesthesia: a prospective study of 6000 blocks. Anesthesiology. 2003;98(4):964–968. doi:10.1097/00000542-200304000-00025
16. Roman SJ, Chong Sit DA, Boureau CM, Auclin FX, Ullern MM. Sub-tenon’s anaesthesia: an efficient and safe technique. Br J Ophthalmol. 1997;81(8):673–676. doi:10.1136/bjo.81.8.673
17. Kumar CM, Dodds C. Evaluation of the greenbaum sub-tenon’s block. Br J Anaesth. 2001;87(4):631–633. doi:10.1093/bja/87.4.631
18. Khan EI, Mustafa J, McAdoo J, Shorten G. Efficacy of sub-tenon’s block using an equal volume of local anaesthetic administered either as a single or as divided doses. A randomised clinical trial. BMC Anesthesiol. 2009;9:2. doi:10.1186/1471-2253-9-2
19. Stevens JD. A new local anesthesia technique for cataract extraction by one quadrant sub-tenon’s infiltration. Br J Ophthalmol. 1992;76(11):670–674. doi:10.1136/bjo.76.11.670
20. Gauba V, Saleh GM, Watson K, Chung A. Sub-tenon anaesthesia: reduction in subconjunctival haemorrhage with controlled bipolar conjunctival cautery. Eye (Lond). 2007;21(11):1387–1390. doi:10.1038/sj.eye.6702447
21. Kumar CM, Dowd TC, Adams WE, Puckering S. Methodology of evaluating conjunctival appearance following sub-tenon’s block for phacoemulsification cataract surgery. Eye (Lond). 2006;20(9):1110–1111. doi:10.1038/sj.eye.6702146
22. Adatia FA, Munro M, Jivraj I, Ajani A, Braga-Mele R. Documenting the subjective patient experience of first versus second cataract surgery. J Cataract Refract Surg. 2015;41(1):116–121. doi:10.1016/j.jcrs.2014.04.041
23. Bardocci A, Ciucci F, Lofoco G, Perdicaro S, Lischetti A. Pain during second eye cataract surgery under topical anesthesia: an intraindividual study. Graefes Arch Clin Exp Ophthalmol. 2011;249(10):1511–1514. doi:10.1007/s00417-011-1803-9
24. Hari-Kovacs A, Lovas P, Facsko A, Crate ID. Is second eye phacoemulsification really more painful? Wien Klin Wochenschr. 2012;124(15–16):516–519. doi:10.1007/s00508-012-0205-2
25. Jiang L, Zhang K, He W, Zhu X, Zhou P, Lu Y. Perceived pain during cataract surgery with topical anesthesia: a comparison between first-eye and second-eye surgery. J Ophthalmol. 2015;2015:383456.
26. Ursea R, Feng MT, Zhou M, Lien V, Loeb R. Pain perception in sequential cataract surgery: comparison of first and second procedures. J Cataract Refract Surg. 2011;37(6):1009–1014. doi:10.1016/j.jcrs.2011.01.020
27. Yu JG, Ye T, Huang Q, et al. Comparison between subjective sensations during first and second phacoemulsification eye surgeries in patients with bilateral cataract. J Ophthalmol. 2016;2016:6521567.
28. Herrinton LJ, Liu L, Alexeeff S, Carolan J, Shorstein NH. Immediate Sequential vs. Delayed Sequential Bilateral Cataract Surgery: Retrospective Comparison of Postoperative Visual Outcomes. Ophthalmology. 2017;124(8):1126–1135.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

