Back to Journals » Journal of Blood Medicine » Volume 14
Outcome of Primary Mediastinal Large B Cell Lymphoma Treated with RCHOP
Authors Halahleh K, Yaseen A, Muradi I, Al-Ibraheem A, Sultan I , Ma'koseh M
Received 31 October 2022
Accepted for publication 12 January 2023
Published 20 February 2023 Volume 2023:14 Pages 147—157
DOI https://doi.org/10.2147/JBM.S393180
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Martin H Bluth
Khalid Halahleh,1 Abeer Yaseen,1 Isra Muradi,2 Akram Al-Ibraheem,3 Iyad Sultan,4 Mohammad Ma’koseh1
1Department of Internal Medicine, King Hussein Cancer Center, Amman, Jordan; 2Department of Medicine, University of Tripoli, Tripoli, Libya; 3Department of Nuclear Medicine, King Hussein Cancer Center, Amman, Jordan; 4Department of Pediatric Oncology, King Hussein Cancer Center, Amman, Jordan
Correspondence: Mohammad Ma’koseh, Department of Internal Medicine, King Hussein Cancer Center, Queen Rania Al Abdullah Street, P.O. Box 1269, Amman, 11941, Jordan, Tel +962-6 5300460, Ext 1146, Email [email protected]
Purpose: Primary mediastinal large B-cell Lymphoma (PMLBCL) is a rare aggressive lymphoma with unique clinical, pathological, and molecular features. The optimal frontline therapy is subject of ongoing debate. Our study aims to evaluate the outcomes of PMLBCL treated with rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone (RCHOP) at King Hussein Cancer Center.
Patients and Methods: Adult patients > 18 years of age with PMLBCL treated with RCHOP from January 2011 to July 2020 were identified. All demographics, disease and treatment related variables were retrospectively collected. Correlations of clinical and laboratory variables with progression-free survival (PFS) and overall survival (OS) were determined by univariate and multivariate analyses using backward stepwise Cox regression models. The PFS and OS were plotted using Kaplan‒Meier curves.
Results: 49 patients were included with a median age of 29 years. 14 (28.6%) had stage III or IV, 31 (63.3%) had mediastinal bulky disease. International prognostic index (IPI) was 0– 1 in 35 (71.4%). Radiotherapy was given to 32 (65.3%) patients. End of treatment (EOT) response was complete (CR) in 32 (65.3%), partial response (PR) in 8 (16.3%) and progressive disease (PD) in 9 (18.4%). Patients who achieved CR at EOT, compared favorably with those who did not in regard to 4-year OS (92.5% vs 26.9%, p=< 0.001). Overall objective response to salvage chemotherapies was 26.7%. At a median follow-up of 46 months, 4-year PFS and OS were 60% and 71% respectively. In multivariate analysis, IPI > one correlated with the EOT response (p=0.009), PFS (p=0.004) and OS (p= 0.019).
Conclusion: In PMLBCL, RCHOP chemotherapy backbone in the frontline therapy is suboptimal but can be used in patients with low IPI. Adapting more intensive chemoimmunotherapy regimens may be considered for patients with high IPI. Salvage chemotherapy has limited activity in patients with relapsed or refractory disease.
Keywords: international prognostic index, end of treatment response, radiotherapy, salvage chemotherapy
Introduction
Lymphomas are relatively common tumors in Jordan with 485 reported cases in 2017 and ranked as the third most common tumor.1 Primary mediastinal large B-cell lymphoma (PMLBCL) is a rather infrequent aggressive lymphoma with unique clinical, pathological, and molecular features, accounts for 2–4% of all non-Hodgkin lymphomas (NHL).2–8 The 2022 World Health Organization (WHO) classification of lymphoid neoplasms identified PMLBCL as a unique clinical and biological entity.9 In contrast to diffuse large B cell lymphoma (DLBCL), PMLBCL typically presents at a median age of approximately 35 years and the majority of patients present with an early-stage but bulky mediastinal disease.2,5,10
The optimal therapeutic approach has not been defined due to the rarity of disease and absence of randomized controlled trials. In the pre-rituximab era, retrospective studies suggested that outcomes with more intensified approaches like, V/MACOP-B (etoposide or methotrexate, doxorubicin, cyclophosphamide, vincristine, prednisone, bleomycin) are superior to CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone).11,12 However, the addition of rituximab to CHOP might mitigate this effect.13 Nonetheless, 20–25% of patients treated with rituximab in combination with anthracycline based chemotherapy had relapse or refractory disease.13–15
Recently, dose adjusted etoposide, doxorubicin, cyclophosphamide, vincristine, prednisone, and rituximab (DA-EPOCH-R) regimen and a sequential administration of four doses of RCHOP followed by three cycles of rituximab, Ifosfamide, carboplatin, and etoposide (R-ICE) resulted in favorable outcomes and obviated the need for consolidative radiotherapy (RT), but with higher treatment-related toxicities.16–19
Our study aims to assess the outcomes of primary mediastinal large B cell lymphoma treated with RCHOP in our center.
Materials and Methods
We searched Cancer Registry of King Hussein Cancer Center (KHCC) for adults (age >18 years) with non-Hodgkin lymphoma, from January of 2011 to July 2020 (n=1156). Patients with a pathological diagnosis of PMLBCL treated with R-CHOP-21 with or without RT were identified and included. Pathological diagnosis was confirmed by the expression of B cell antigens (CD19, CD20, CD23, and CD79a) and the lack of CD15. CD30 positivity supported the diagnosis but was not required.
All demographics, laboratory, and treatment-related variables, including age, gender, date of diagnosis, Eastern Cooperative Oncology Group (ECOG) performance status, serum lactate dehydrogenase (LDH), erythrocyte sedimentation rate (ESR), beta-2 microglobulin (B2M), number of extranodal sites, disease stage and disease bulk were collected. Bulky disease is defined as a mediastinal mass of ≥10 centimeters.
Staging and response to treatment were determined according to Lugano criteria.20 Initial staging was done with a computed tomography (CT) scan in 30 (61%) patients and with a CT scan and a positron emission tomography (PET)-CT scan in the remaining patients. Response to treatment was determined with PET-CT scan in 44 (89.7%) patients and with a CT scan only in 5 (10.3%) patients. International prognostic index (IPI) was calculated as previously described.21
Consolidative radiotherapy (RT) was given to patients with a tumor diameter >7 cm with no evidence of disease progression after finishing chemotherapy. Descriptive statistics were used to characterize patients at baseline and presented as counts and percentages. Overall survival (OS) was calculated from the date of diagnosis to the date of the last encounter or death from any cause. Progression free survival (PFS) was calculated from the date of diagnosis to the date of relapse or progression. Survival outcomes were calculated using the Kaplan Meier method. The associations between different variables with PFS and OS were analyzed using Log-rank (Mantel-Cox) test in the univariate analysis and Cox proportional hazard models in the multivariate analysis. Patients’ characteristics and the end of treatment (EOT) response were compared using the Fisher’s exact test. ECOG performance status was excluded from the analysis because one patient had an ECOG performance status of >1. The P-values are two-sided and considered significant when < 0.05. The waiver of the written informed consent was granted due to the retrospective nature of the review, and the data were anonymized and maintained with confidentiality. The study was approved by the King Hussein Cancer Center Institutional Review Board (IRB) complaint with the principles of the declaration of Helsinki.
Results
49 patients were included in the analysis with a median age of 29 (range:18–56) years and an almost equal gender distribution. 14 (28.6%) had stage III or IV, and 11 (22.4%) had two or more extranodal sites. CD30 was reported to be positive in 41 (83.7%) patients. About two thirds of patients had mediastinal bulky disease. IPI was 0–1 in 35 (71.4%). All patients received at least six cycles of RCHOP; 39 (79.6%) patients were given six cycles and 10 (20.4%) patients were given 7–8 cycles. Consolidative RT at doses between 30.6Gy to 39.6Gy was given to 32 (65.3%) patients, among which four (12.5%) patients were given involved site radiotherapy and 28 (87.5%) patients received involved field radiotherapy. Patients’ characteristics are detailed in Table 1.
 |
Table 1 Patients Characteristics and Treatment |
After chemotherapy completion, 39 (79.6%) had an objective response among which 30 (61.2%) had complete response (CR) and nine (18.4%) had partial response.
Consolidative RT was given to 22 (73.3%) patients while in CR, all continued to have CR at the last encounter and to 7 out of 9 patients while in PR; 2 of the moved to CR after RT, 2 PR and 3 had disease progression (DP). 3 of the 10 patients who progressed were given salvage RT, all progressed. Based on the decision of the treating physician, four patients with a bulky disease had a CR and two patients with a PR did not receive consolidative radiotherapy.
End of treatment (EOT) response to either chemotherapy or combined modality treatment revealed CR in 32 (65.3%), no CR in 17 (34.7%) [PR in 8 (16.3%) and DP in 9 (18.4%)], Table 2.
 |
Table 2 Response to Frontline and Salvage Treatments |
After a median follow-up of 46 (range:5–130) months, 4-year PFS and OS were 60% and 71.4% respectively, Figures 1 and 2. The median time to relapse or progression was 7.2 (range: 3.3 −14) months.
 |
Figure 1 Progression free survival in all patients. |
 |
Figure 2 Overall survival in all patients. |
In univariate analysis, IPI >1 (mainly driven by advanced stage and ≥ 2 extranodal sites), Figures 3 and 4, and B2M ≥2.5 correlated with PFS and OS, Table 3. In multivariate analysis, IPI>1 significantly associated with PFS (p=0.005) and OS (p=0.019). In contrast, gender, the presence of B-symptoms, high ESR, and the presence of disease bulk had no statistically significant correlation with either endpoint, Table 4.
 |
Table 3 Univariate Analysis for Progression Free Survival and Overall Survival |
 |
Table 4 Multivariate Analysis |
 |
Figure 3 Progression free survival according to international prognostic index (IPI). |
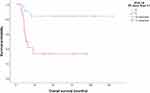 |
Figure 4 Overall survival according to international prognostic index (IPI). |
Advanced stage disease (p=0.009), ≥2 extranodal sites (p=0.005) and IPI >1 (p=0.009) correlated with EOT response, Table 5. The EOT response (CR vs no CR) correlated strongly with PFS (p=<0.001) and OS (p=<0.001), Figure 5.
 |
Table 5 Correlation Between Different Pre-Treatment Variables and End-of Treatment Response |
 |
Figure 5 Overall survival according to end of treatment response. Abbreviation: CR, complete response. |
All patients with a relapsed or refractory disease (n=19) were treated with salvage chemotherapy, Table 1. 5 (26.3%) patients had a response; 3 went into CR (2 received pembrolizumab), and 2 achieved a PR. Patients with a response to salvage chemotherapy (n=5), received high dose chemotherapy and autologous stem cell transplant (ASCT), Table 2.
Among the patients with a relapsed or refractory disease, 4 (21.5%) were alive with no disease on the last follow-up.
Discussion
There is no standard first line therapy for PMLBCL because of the lack of prospective randomized studies and no large registry reports published. The European Society of Medical Oncology (ESMO) guidelines concluded that RCHOP-14, RCHOP-21, DA-EPOCH-R, R-VACOP-B and V-MACOP-B are reasonable first-line options.22 RCHOP-21 with radiotherapy is the standard regimen recommended by the British Society of Haematology (BSH) guidelines and DA-EPOCH-R without radiotherapy can be used alternatively.23 The National Comprehensive Cancer Network (NCCN) guidelines recommended either RCHOP or DA-EPOCH-R as first line therapy.24
The most commonly used frontline regimens, RCHOP and DA-EPOCH-R, were compared in a multicenter retrospective study and showed higher rates of CR in DA-EPOCH-R (84.4% vs 69.6%) but no difference in long-term survival outcomes.25 However, in another recent retrospective study, the use of DA-EPOCH-R was associated with improved PFS and OS in comparison with RCHOP.26 Toxicity is an important consideration when selecting the optimal frontline treatment. DA-EPOCH-R is associated with more acute toxicities including neutropenia, stomatitis, cardiac complications, thrombosis, the need for admission and central venous access.27
The PFS and OS rates in our study compare less favorably to Vassilakopoulos et al report, with 4-year PFS of 59% vs 80%, and OS of 71.4% vs 89%.28 This can be explained by the inclusion of more patients with advanced stage disease in our study (21.4% vs 12%) and the fact that 18.4% of our patients had ≥2 extranodal sites, which was not reported by Vassilakopoulos et al, as the age-adjusted IPI was used to stratify the patients rather than the original IPI used in our study. This group had significantly worse outcomes (4-year PFS of 11% and OS of 22%). However, our results confirmed the reasonable survival outcomes of patients with low IPI (0–1) previously published in the MinT trial subgroup study.15
The results of our study highlight important practical points. First, patients with advanced stage disease or ≥2 extranodal sites had unsatisfactory outcomes when RCHOP was used in the frontline in accordance with the results of a recent study from British Columbia.29 The use of DA-EPOCH-R in this high-risk group compares more favorably to our results (PFS of 60% vs 21.4%).27 Although there are no prospective randomized studies, the use of more intensified approaches may be reasonable to improve long-term outcomes. On the other hand, for patients with limited-stage disease, RCHOP can accomplish the job.
Second, the median time to relapse or progression in our study was 7 months and none of our patients relapsed after 14 months. This observation was previously reported,30 and may help to optimize patient’s follow-up plan.
Third, the response to salvage chemotherapy in our study (26.3%), was also reported in other studies,31,32 indicating that refractory or relapsed PMLBCL, compared to DLBCL, is less likely to respond to salvage chemotherapy. Recently, the introduction of CD19 specific chimeric antigen receptor (CAR) T cell therapy has revolutionized the treatment of relapsed DLBCL including PMLBCL. The results of two Phase 3 trials, the ZUMA-7 and the TRANSFORM trails, demonstrated a better event free survival and OS of CAR T cell therapy (axicabtagene ciloleucel in ZUMA-7 and Lisocabtagene maraleucel in TRANSFMORM) relative to salvage chemotherapy and ASCT in patients with primary refractory or early first relapse (<12 months) large B cell lymphoma including PMLBCL.33,34
In line with frequent expression of programmed cell death-1 (PD-1) and CD30 positivity in PMLBCL, CheckMate 436, KEYNOTE-170 and KEYNOTE-013 trails showed high efficacy of immune check point inhibitors as monotherapy or in combination with brentuximab vedotin in relapsed and refractory PMLBCL.35,36 Two of our patients were treated with pembrolizumab as a third line salvage went into CR and received high dose chemotherapy and ASCT. Both patients are still alive and disease free at the last encounter. The use of these agents may be considered in patients not eligible or relapsing after CAR T cell therapy.
The role of consolidative radiotherapy in patients treated with RCHOP is still an area of debate. Recent reports have shown that radiotherapy can be safely omitted in patients having a complete metabolic response on PET-CT scan.26 Due to the small number of patients who achieved a CR and did not receive consolidative radiotherapy in our study (n=8), no solid conclusions can be made. The ongoing IELSG 37 phase 3 trial is investigating the role of consolidative radiotherapy after chemoimmunotherapy in PMLBCL would hopefully help to answer this critical question.37
Our study has several limitations including the retrospective design, small number of patients and no comparator arm.
Conclusion
The use of frontline therapy with RCHOP in PMLBCL is suboptimal but may be reasonable in patients with low IPI score with good long-term survival outcomes. The use of more intensive approaches may be considered for patients with advanced stage disease. Patients with relapsed or refractory disease had a limited response to salvage chemotherapy and CART T cell therapy should be considered.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Cancer Incidence in Jordan. Available from: www.moh.gov.jo//c602eda7-0c36-49cd-bea1-3484e46c0b97.
2. Johnson PW, Davies AJ. Primary mediastinal B-cell lymphoma. Hematology Am Soc Hematol Educ Program. 2008;2008:349–358. doi:10.1182/asheducation-2008.1.349
3. Rosenwald A, Wright G, Leroy K, et al. Molecular diagnosis of primary mediastinal B cell lymphoma identifies a clinically favorable subgroup of diffuse large B cell lymphoma related to Hodgkin lymphoma. J Exp Med. 2003;198(6):851–862. doi:10.1084/jem.20031074
4. Lazzarino M, Orlandi E, Paulli M, et al. Primary mediastinal B-cell lymphoma with sclerosis: an aggressive tumor with distinctive clinical and pathologic features. J Clin Oncol. 1993;11(12):2306–2313. doi:10.1200/JCO.1993.11.12.2306
5. Dabrowska-Iwanicka A, Walewski JA. Primary mediastinal large B-cell lymphoma. Curr Hematol Malig Rep. 2014;9(3):273–283. doi:10.1007/s11899-014-0219-0
6. Savage KJ, Monti S, Kutok JL, et al. The molecular signature of mediastinal large B-cell lymphoma differs from that of other diffuse large B-cell lymphomas and shares features with classical Hodgkin lymphoma. Blood. 2003;102(12):3871–3879. doi:10.1182/blood-2003-06-1841
7. Twa DD, Chan FC, Ben-Neriah S, et al. Genomic rearrangements involving programmed death ligands are recurrent in primary mediastinal large B-cell lymphoma. Blood. 2014;123(13):2062–2065. doi:10.1182/blood-2013-10-535443
8. Steidl C, Gascoyne RD. The molecular pathogenesis of primary mediastinal large B-cell lymphoma. Blood. 2011;118(10):2659–2669. doi:10.1182/blood-2011-05-326538
9. Alaggio R, Amador C, Anagnostopoulos I, et al. The 5th edition of the world health organization classification of haematolymphoid tumours: lymphoid neoplasms. Leukemia. 2022;36(7):1720–1748. doi:10.1038/s41375-022-01620-2
10. Hamlin PA, Portlock CS, Straus DJ, et al. Primary mediastinal large B-cell lymphoma: optimal therapy and prognostic factor analysis in 141 consecutive patients treated at Memorial Sloan Kettering from 1980 to 1999. Br J Haematol. 2005;130(5):691–699. doi:10.1111/j.1365-2141.2005.05661.x
11. Todeschini G, Secchi S, Morra E, et al. Primary mediastinal large B-cell lymphoma (PMLBCL): long-term results from a retrospective multicentre Italian experience in 138 patients treated with CHOP or MACOP-B/VACOP-B. Br J Cancer. 2004;90(2):372–376. doi:10.1038/sj.bjc.6601460
12. Zinzani PL, Martelli M, Bertini M, et al. Induction chemotherapy strategies for primary mediastinal large B-cell lymphoma with sclerosis: a retrospective multinational study on 426 previously untreated patients. Haematologica. 2002;87(12):1258–1264.
13. Avigdor A, Sirotkin T, Kedmi M, et al. The impact of R-VACOP-B and interim FDG-PET/CT on outcome in primary mediastinal large B cell lymphoma. Ann Hematol. 2014;93(8):1297–1304. doi:10.1007/s00277-014-2043-y
14. Savage KJ, Al-Rajhi N, Voss N, et al. Favorable outcome of primary mediastinal large B-cell lymphoma in a single institution: the British Columbia experience. Ann Oncol. 2006;17(1):123–130. doi:10.1093/annonc/mdj030
15. Rieger M, Österborg A, Pettengell R, et al. Primary mediastinal B-cell lymphoma treated with CHOP-like chemotherapy with or without rituximab: results of the Mabthera international trial group study. Ann Oncol. 2011;22(3):664–670. doi:10.1093/annonc/mdq418
16. Wilson WH, Grossbard ML, Pittaluga S, et al. Dose-adjusted EPOCH chemotherapy for untreated large B-cell lymphomas: a pharmacodynamic approach with high efficacy. Blood. 2002;99(8):2685–2693. doi:10.1182/blood.v99.8.2685
17. Dunleavy K, Pittaluga S, Maeda LS, et al. Dose-adjusted EPOCH-rituximab therapy in primary mediastinal B-cell lymphoma. N Engl J Med. 2013;368(15):1408–1416. doi:10.1056/NEJMoa1214561
18. Dunleavy K. Primary mediastinal B-cell lymphoma: biology and evolving therapeutic strategies. Hematology Am Soc Hematol Educ Program. 2017;2017(1):298–303. doi:10.1182/asheducation-2017.1.298
19. Moskowitz CH, Schöder H, Teruya-Feldstein J, et al. Risk-adapted dose-dense immunochemotherapy determined by interim FDG-PET in Advanced-stage diffuse large B-Cell lymphoma. J Clin Oncol. 2010;28(11):1896–1903. doi:10.1200/JCO.2009.26.5942
20. Cheson BD, Fisher RI, Barrington SF, et al. Recommendations for initial evaluation, staging, and response assessment of Hodgkin and non-Hodgkin lymphoma: the Lugano classification. J Clin Oncol. 2014;32(27):3059–3068. doi:10.1200/JCO.2013.54.8800
21. International Non-Hodgkin’s Lymphoma Prognostic Factors Project. A predictive model for aggressive non-Hodgkin’s lymphoma. N Engl J Med. 1993;329(14):987–994. doi:10.1056/NEJM199309303291402
22. Vitolo U, Seymour JF, Martelli M, et al. Extranodal diffuse large B-cell lymphoma (DLBCL) and primary mediastinal B-cell lymphoma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2016;27(suppl 5):v91–v102. doi:10.1093/annonc/mdw175
23. Cwynarski K, Marzolini MAV, Barrington SF, et al. The management of primary mediastinal B-cell lymphoma: a British society for haematology good practice paper. Br J Haematol. 2019;185(3):402–409. doi:10.1111/bjh.15731
24. Zelenetz AD, Gordon LI, Chang JE, et al. NCCN guidelines® insights: b-cell lymphomas, version 5.2021. J Natl Compr Canc Netw. 2021;19(11):1218–1230. doi:10.6004/jnccn.2021.0054
25. Shah NN, Szabo A, Huntington SF, et al. R-CHOP versus dose-adjusted R-EPOCH in frontline management of primary mediastinal B-cell lymphoma: a multi-centre analysis. Br J Haematol. 2018;180(4):534–544. doi:10.1111/bjh.15051
26. Zhou H, Xu-Monette ZY, Xiao L, et al. Prognostic factors, therapeutic approaches, and distinct immunobiologic features in patients with primary mediastinal large B-cell lymphoma on long-term follow-up. Blood Cancer J. 2020;10(5):49. doi:10.1038/s41408-020-0312-7
27. Morgenstern Y, Aumann S, Goldschmidt N, Gatt ME, Nachmias B, Horowitz NA. Dose-adjusted EPOCH-R is not superior to sequential R-CHOP/R-ICE as a frontline treatment for newly diagnosed primary mediastinal B-cell lymphoma: results of a bi-center retrospective study. Cancer Med. 2021;10(24):8866–8875. doi:10.1002/cam4.4387
28. Vassilakopoulos TP, Pangalis GA, Katsigiannis A, et al. Rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone with or without radiotherapy in primary mediastinal large B-cell lymphoma: the emerging standard of care. Oncologist. 2012;17(2):239–249. doi:10.1634/theoncologist.2011-0275
29. Hayden AR, Tonseth P, Lee DG, et al. Outcome of primary mediastinal large B-cell lymphoma using R-CHOP: impact of a PET-adapted approach. Blood. 2020;136(24):2803–2811. doi:10.1182/blood.2019004296
30. Giulino-Roth L. How I treat primary mediastinal B-cell lymphoma. Blood. 2018;132(8):782–790. doi:10.1182/blood-2018-04-791566
31. Kuruvilla J, Pintilie M, Tsang R, Nagy T, Keating A, Crump M. Salvage chemotherapy and autologous stem cell transplantation are inferior for relapsed or refractory primary mediastinal large B-cell lymphoma compared with diffuse large B-cell lymphoma. Leuk Lymphoma. 2008;49(7):1329–1336. doi:10.1080/10428190802108870
32. Vardhana S, Hamlin PA, Yang J, et al. Outcomes of relapsed and refractory primary mediastinal (Thymic) large B cell lymphoma treated with second-line therapy and intent to transplant. Biol Blood Marrow Transplant. 2018;24(10):2133–2138. doi:10.1016/j.bbmt.2018.06.009
33. Locke FL, Miklos DB, Jacobson CA, et al. Axicabtagene ciloleucel as second-line therapy for large B-cell lymphoma. N Engl J Med. 2022;386(7):640–654. PMID: 34891224. doi:10.1056/NEJMoa2116133
34. Kamdar M, Solomon SR, Arnason J, et al. Lisocabtagene maraleucel versus standard of care with salvage chemotherapy followed by autologous stem cell transplantation as second-line treatment in patients with relapsed or refractory large B-cell lymphoma (TRANSFORM): results from an interim analysis of an open-label, randomised, phase 3 trial. Lancet. 2022;399(10343):2294–2308. doi:10.1016/S0140-6736(22
35. Armand P, Rodig S, Melnichenko V, et al. Pembrolizumab in relapsed or refractory primary mediastinal large B-cell lymphoma. J Clin Oncol. 2019;37(34):3291–3299. doi:10.1200/JCO.19.01389
36. Zinzani PL, Santoro A, Gritti G, et al. Nivolumab combined with brentuximab vedotin for relapsed/refractory primary mediastinal large B-cell lymphoma: efficacy and safety from the phase II checkMate 436 study. J Clin Oncol. 2019;37(33):3081–3089. doi:10.1200/JCO.19.01492
37. IELSG37. A randomized, open-label, multicentre, two-arm phase III comparative study assessing the role of involved mediastinal radiotherapy after rituximab containing chemotherapy regimens to patients with newly diagnosed primary mediastinal large B-cell lymphoma (PMLBCL). Available from: https://clinicaltrials.gov/ct2/show/NCT01599559.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
