Back to Journals » Open Access Emergency Medicine » Volume 15
Outcome of Poisoning and Associated Factors Among Patients Admitted at Referral Hospitals in Northwest Ethiopia, 2022: A Multicenter Retrospective Study
Authors Reda GB , Abate HK , Mekonnen HM, Gared AZ , Beko ZW
Received 28 March 2023
Accepted for publication 1 November 2023
Published 8 November 2023 Volume 2023:15 Pages 415—425
DOI https://doi.org/10.2147/OAEM.S414743
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Hans-Christoph Pape
Gashachew Bayleyegn Reda,1 Hailemichael Kindie Abate,2 Hidja Mustofa Mekonnen,1 Agerie Zerihun Gared,1 Zerko Wako Beko2
1Department of Emergency and Critical Care Nursing, School of Nursing, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia; 2Department of Medical Nursing, School of Nursing, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Correspondence: Gashachew Bayleyegn Reda, Tel +251984251200, Email [email protected]
Background: Poisonings are the most common reason for visiting emergency departments and hospitals globally. Poisoning-related mortalities increase instantly, and it is a principal public health problem in Ethiopia. Hence, understanding the treatment outcome and identifying the associated factors is necessary to reduce poisoning-related mortality.
Objective: To assess outcome of poisoning and associated factors among patients admitted to Referral Hospitals in Northwest Ethiopia, 2022.
Methods: An institutional-based retrospective cross-sectional study was conducted in Western Amhara referral hospitals from June 2019 to May 2022. A total of 400 medical charts were reviewed. A stratified sampling technique was used. The data were entered into Epi Info version 7.2.1.0 and exported to SPSS version 25.0 software for analysis. Multivariable binary logistic regression analysis was used to determine factors associated with the outcome of poisoning.
Results: The mortality rate of poisoning was 18% (95% CI: 14.4– 22.1). Being rural dwellers (AOR=2.65, 95% CI: 1.07– 6.63), being unconscious (AOR=4.86, 95% CI: 1.89– 12.48), not treated in triage area (AOR=4.64, 95% CI: 1.608– 13.407), transport by Bajaj (AOR=6.78, 95% CI: 1.86– 24.73), spo2 < 95% (AOR=4.42, 95% CI: 1.19– 10.78), and stayed > 48 hours in the hospital (AOR=0.08, 95% CI: 0.02– 0.36) were significantly associated with a mortality of poisoning.
Conclusion: The mortality rate from poisoning was considerably high. Residence, level of consciousness, treatment at the triage area, mode of arrival, Spo2, and prolonged hospital stay were significantly associated. All stakeholders should focus on planning and improving care for patients with poisoning. Improving ambulance service in rural areas and providing treatment at the triage area for all patients are recommended.
Keywords: emergency departments, poisoning, referral hospital, treatment outcome
Introduction
The term “poison” refers to any chemical substance, solid, liquid, or gas upon accidentally or intentionally ingesting that can affect the body’s health and lead to death.1 Globally, studies have stated that poisoning is still a principal public health problem.2–4 In the USA alone, mortality rates increased from 25% to 40%, leading to a six-fold increase in mortality rates and ranking suicide tenth among the top 10 leading causes of death.5 According to the Global Burden of Disease (GBD), unintentional poisoning accounted for 0.14% of global deaths, and self-harm accounted for 1.34%.6 In Ethiopia, studies have shown that the mortality rate from poisoning ranges from 0.3% to 27.6%.1,7–16 According to studies of sub-Saharan Africa, in Ethiopia, unintentional poisoning was 3.3 per 100 000.17 A report by the WHO estimated that nearly 200000 people die of unintentional poisoning annually. On the other hand, intentional poisoning outweighs unintentional poisoning in that one-third of a million people die of poisoning, which is highly linked to suicidal attempts.18
Poisonings affect the community by leading to frequent emergency room visits, prolonged hospital admissions, and sharply increasing mortality rates.2–4 The outcome of poisoning negatively affects the community’s physical, emotional, and spiritual well-being and alters the quality of life of patients and their families.19,20 It affects the productive age group and the task forces of agricultural development, leading to low economic growth and poor agricultural reproduction yield.8,11,21 Ethiopia’s economy majorly depends on agriculture, and 85% of the population depends on agriculture as a farmer. Organophosphates (OPs) are the most common cause of poisoning because they are often available and widely used as herbicides by farmers.16,22
Studies have shown that, for instance, personal, environmental, organizational, and clinical factors have a significant effect on the outcome of poisoning. In particular, these factor types of poison, routes, mode of transmission, source of poison, season that occurred, place of residence, dose of poisoning, level of consciousness, time of arrival, modes of transportation, triage category, gender, marital status, and duration of hospital stay.1,7,8,10,12,19,23
Timely and effective prevention and management of poison-related morbidity and mortality requires a concerted effort from all stakeholders to reduce its negative impacts. Prevention is always the best option, as are prevention of exposures, early identification and recognition, supportive and symptomatic care, decontamination, elimination of absorption, and provision of antidotes. Poison control centers should put into practice the provision of education, training, and toxic surveillance for early prevention.1,2,24–27 Eventually decreasing the complications and mortality rates of poisoning.19 Untreated poisoned patients will lead to stress and anxiety for patients and their families.8,11,21
Even though different studies investigated several factors affecting the outcome, the mortality rate is still high due to poisoning and is dramatically increasing. Hence, it remains a public health problem in Ethiopia. Therefore, this study identifies factors associated with the outcome of poisoning at the emergency department in Northwest Ethiopia.
Methods
Study Design and Period
A multicenter retrospective cross-sectional study design was conducted among poisoned patients admitted from June 2019 to May 2022, and the actual data collection or extraction period was from May 1 to 31, 2022.
Study Setting
This study was conducted at five public university referral hospitals (University of Gondar, Debre Markos, Tibebe Ghion, Felege Hiwot, and Debre Tabor comprehensive specialized hospital), located in the Western Amhara regional state, Northwest Ethiopia. Each hospital provides health-care services to more than 5 million people in Tibebe Gion, Debre Tabor, and Debre Markos comprehensive specialized hospitals. Felege Hiwot and the University of Gondar Comprehensive specialized hospital give health-care services to more than 7 million people. There were 3713 poisoned cases in the 5 Western Amhara referral hospitals from June 1, 2019, to May 31, 2022.
Populations
All poisoned patients admitted to the emergency department of Western Amhara referral hospital were the source population. Poisoned patients whose charts were available during data collection from June 1, 2019, to May 31, 2022, were the study population. However, those with incomplete medical records were excluded.
Sample Size Determination
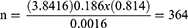
For the independent variables: The required sample size for this particular study was determined using a single population proportion formula, and the proportion was taken from a previous study conducted in Debre Tabor referral hospital, the proportion of mortality of poisoning = 18.6%.8 Considering the following assumptions, A 95% confidence level, margin of error (0.04), and P = 18.6% were substituted in the following single population proportion formula.
Where; n = required sample size, P = Mortality rate of poisoning from previous study = 18.6%, d = margin of error = 4%, q = 1-p, Z = critical value for normal distribution at 95% confidence level, which equals to 1.96 (z value at α = 0.05). Adding 10% to the calculated sample size was added to compensate for incomplete and missing patient cards.
Therefore; from all calculated sample sizes the largest was 364. To get the final sample size, add 15% contingency to incomplete or missing patient cards. Therefore, the total sample size for this study was 419.
Sampling Technique and Procedure
A stratified sampling procedure was used to select the study participants in each stratum from each ED of the five Western Amhara referral hospitals. From each stratum, the calculated sample size was proportionally allocated to the study participants. The first lists each poisoned patient that was found in each Western Amhara referral hospital and determines how many poisoned patients in each stratum, which use proportionally allocated and the medical charts of poisoning cases were selected by a simple random sampling technique were implemented (Figure 1).
 |
Figure 1 Schematic presentation of sampling procedure of poisoning patients to the emergency department of referral hospitals in Western Amhara 2022. |
Operational Definition
Improved: Those poisoned patients discharged upon improvement.7
Death: Those poisoned patients have a death certificate.7
Data Collection Tool and Procedure
The data were collected using a data collection checklist adapted from various previous literature with slight modifications.1,7,10–12,16 The checklist was prepared by addressing possible important variables for the study. Then, checking the completeness and consistency of the variables in the chart was performed. Five trained emergency and critical care nurses collected the data and one MSc nurse was selected to supervise the data collection period. Then, by using a computer-generated random number, they selected the required medical record number after listing the medical card number of poisoning cases from the ED patient’s registration books. The data collectors filtered the patient’s chart from the medical record room and collected the necessary information from patients’ medical records using a prepared data collection checklist. The checklist was filled by searching for appropriate information. The collected data was examined for completeness, consistency, and accuracy during data collection to ensure the checklist was filled appropriately.
Data Quality Assurance
First careful modifications of the data collection checklist from previous research were done. To ensure the quality of data, check the availability of variables on 15 randomly selected medical charts from UoGCSH to ensure the agreement of the data abstraction format with the objective of the study. After checking the availability of variables in medical charts, amendments were conducted. Then data collectors and supervisors were recruited based on their experience in research, and one-day training was given on the objective of the study, data collection tool, and data collection procedures by the principal investigator. Supervision was conducted by the principal investigator and supervisors daily. The supervisors and principal investigator reviewed the collected data daily and checked for completeness, accuracy, and consistency immediately after collection and appropriately arranged and kept in a secure place for compilation and analysis.
Data Processing and Analysis
The collected data were checked for completeness and consistency and then entered into Epi Info version 7.2.1.0. The entered data were exported, cleaned, and analyzed using SPSS Version 25 statistical software. Frequencies and cross-tabulations were used to summarize descriptive statistics of the data. Both bivariable and multivariable logistic regression analyses were performed to identify factors associated with the treatment outcome of poisoning. The variables in bivariate analysis with p < 0.2 were entered into multivariable logistic regression. The strength of the association of factors associated with the treatment outcome of poisoning was demonstrated by computing an adjusted odds ratio (AOR) with a 95% confidence interval (CI). Finally, the analyzed data were organized and presented in tabular, graphical, and descriptive forms accordingly. After adjusting their effect on the outcome variable, those variables with a P-value <0.05 with a 95% confidence interval were considered as factors significantly associated with the treatment outcome of poisoning.
Results
Socio-Demographic Characteristics
A total of 419 poisoned patients’ medical charts were reviewed retrospectively. Of these, 400 (95.5%) patients’ medical charts had complete information. About 238 (59.5%) were females, 192 (48.0%) were in the age group of 19–34 years, and 203 (50.7%) lived in rural areas (Table 1).
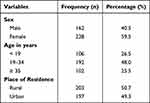 |
Table 1 Socio-Demographics Characteristics of Poisoned Patients Admitted at the Emergency Department of Western Amhara Referral Hospitals, Northwest Ethiopia, 2022 (n=400) |
Poisoning Related Factors
Of all poisoning cases, organophosphate poisoning (OPP) and metallo phosphide poisoning (MPP) were 272 (68.0%) and 129 (32.3%), respectively (Figure 2), 359 (89.8%) happened unintentionally, 260 (65.0%) were in liquid form, 380 (95.0%) were ingested orally, 241 (60.3%) sustained poisoning at day time, 323 (80.8%) poisoning incidents occurred at home, and 169 (42.3%) pharmaceutical agents were the source of poisoning (Table 2). Among the reasons reported by the poisoned patient’s family disharmony and unwanted pregnancy were 129 (32.3%) and 7 (1.8%), respectively (Figure 3).
 |
Table 2 Poison-Related Characteristics of Poisoned Patients Admitted at the Emergency Department of Western Amhara Referral Hospitals, Northwest Ethiopia, 2022 (n=400) |
 |
Figure 2 Types of poisoning used by the patients admitted in emergency department of Western Amhara referral hospitals, Northwest Ethiopia, 2022. |
 |
Figure 3 Reason for poisoning among poisoned patients admitted in emergency department of Western Amhara referral hospitals, Northwest Ethiopia, 2022. |
Clinical-Related Factors
In total, 279 (69.8%) were conscious upon arrival, 17 (4.3%) had comorbidities, 141 (35.3%) developed complications, 14 (3.5%) attempted suicide, 148 (37.0%) were accompanied by ambulances, 241 (60.3%) had not received pre-hospital care, 336 (84.0%) received triage treatment, 328 (82.0%) stayed at the hospital for less than 48 hr, and 337 (84.3%) arrived after 1 hr (Table 3).
 |
Table 3 Clinical Related Factors of Poisoned Patients Who Had Been Admitted at the Emergency Department of Western Amhara Referral Hospitals, Northwest Ethiopia, 2022 (n=400) |
Treatment Outcome of Poisoning
From 400 reviewed patients’ charts, 72 (18.0%) (95% CI: 14.4–22.1) and 328 (82.0%) (95% CI: 77.9–85.6) died and improved, respectively (Figure 4).
 |
Figure 4 Treatment outcome of poisoning patients admitted in emergency department of Western Amhara referral hospitals, Northwest Ethiopia, 2022. |
Bivariate and Multivariate Analysis of Factors Affecting Poisoning
In the bivariable analysis, a total of 24 variables were used. However, in the multivariable binary logistic regression analysis, only seven variables were significantly associated with the outcome. These include the place of residence, the marital status of the patient, the level of consciousness at the time of arrival, the mode of transport to the hospital, the treatments given at the triage area, the level of oxygen saturation, and the length of stay in the hospital (Table 4).
Discussion
This study aimed at determining treatment outcomes and associated factors in poisoning cases. The mortality rate of the current study was 18% (95% CI: 14.4–22.1). This finding is consistent with studies conducted in Hiwot Fana, Eastern Ethiopia 16.7%,28 and Debre Tabor 18.6%.8 Possible reasons could be similarity in types of poisoning agents, modes of poisoning, time of arrival to the hospital after exposure, the season of poisoning, and similar socio-demographic characteristics.
This finding is also in line with studies conducted in South India 14.6%,29 in West Bengal, India, 15.03,30 and in the tertiary care hospital, India, 18.6%.21 One possible reason might be sample size variation: the majority were rural dwellers, time of arrival to the hospital after exposure, nature of poisoning, and referral status.
The mortality rate of this study is lower than studies conducted in India 24%,31 35%,32 in Egypt 25%33 and in Ethiopia 27.6%.16 The possible justification could be due to the difference in a study setting, type of poison exposure, the season of poisoning, the time elapsed from exposure to arrival to the hospital, proper assessment of the severity of poisoning, availability of life-saving measures, and transport services.
The mortality rate of the current study is higher when compared with studies conducted in China (6.7%), Addis Ababa (10.2%), Black lion (8.6%), Dessie (6.6%), and Wolega (7.10%).10–12,15,34 The possible justification could be due to sample size difference, the severity of poisoning agents, a lack of early diagnosis and treatments, difference in the poisoning agent, a season of poisoning, and pre-hospital care.
Those poisoned patients who live in rural areas were 2.65 times more likely to die as compared to poisoned patients who lived in urban areas. This study is inconsistent with a study conducted in Wollega.10 One possible justification for this might be that most of the participants were urban dwellers. However, the current study shows rural dwellers predominantly presented with poison cases. That was to time on arrival, and unable to get early advanced and pre-hospital care.
Being unconscious was 4.86 times more likely to die than compared to being conscious during arrival to ED. The result of this study was in line with studies conducted in Royal, London,35 and Adada, Turkey.36 This result is congruent with study of Sweden.37 A possible justification could be the presence of hypoxia or hypercarbia, respiratory distress, hypoglycemia, and decreased airway protection posed to aspiration, hence leading to airway obstruction. Moreover, unconscious patients are at risk of developing multi-organ failure.
In this study, poisoned patients whose Spo2 was less than or equal to 95% were 4.42 times more likely to die compared to those whose Spo2 >95%. This finding is agreeable with studies conducted in Norway38 and Peru.39 A possible justification could be that brain tolerates only 4–6 min without oxygen, an imbalance between oxygen demand and supply. In fact, the mortality rate increases with decreasing oxygen saturation levels.
Poisoned patients who stayed longer than 48 hr in the hospital were 91.6% less likely to die compared to those who spent less than 48 hr. This study is different from a study conducted in Ambo.1 One possible reason could be late arrival to the hospital after exposure and advanced care.
Poisoned patients transported to hospital by Bajaj were 6.78 times more likely to die from poisoning, with poisoned cases transported by ambulance. This result is in line with a study by Ohio State University Medical Center.40 The possible reason may be the difference in the health-care providers’ preparedness and approach to receiving patients who come by private car and ambulance, number of patients come by Bajaj, whereby drivers do not respond to the call, finish benzene or oil on the way, and the distance from health facility lead to late arrival to the hospital.
In this study, poisoned patients who never received treatment in triage areas are 4.64 times more likely to die related to those who received treatment in triage areas. This result is in agreement with a study conducted in Belgium. An appropriate triage reduces overcrowding, delays the management of patients, reduces the length of stay in the emergency unit, and improves the management of patients and total time spent in the ED.41
Limitations
The retrospective nature of the study design prohibits the necessary variables, like laboratory data, to determine the severity of the cases as a determinant of the treatment outcome of poisoning.
Conclusion
In this study, the mortality rate from poisoning was considerably high. This problem should require the stakeholder to give more attention to planning and improving care for poisoning at the hospital. Improved ambulance services are needed in rural areas. Give treatment at the triage area for all poisoned patients, and frequently follow the unconscious and poisoned patients whose Spo2 is less than 95% and treat them accordingly in ED.
Abbreviation
AOR, Adjusted Odd Ratio; CI, Confidence Interval; COR, Crude Odd Ratio; DMCSH, Debre Markos Comprehensive Specialized Hospital; DTCSH, Debre Tabor Comprehensive Specialized Hospital; ED, Emergency Department; EMCCN, Emergency Medicine and Critical Care Nursing; FHCSH, Felege Hiwot Comprehensive Specialized Hospital; OP, Organophosphate; OPP, Organophosphate Poisoning; PR, Pulse Rate; RBS, Random Blood Sugar; RR, Respiration Rate; SRS, Simple Random Sampling; SOB, Shortness of breath; SPSS, Statistical Package for Social Science; SBP, Systolic Blood pressure; TGCSH, Tibebe Gion Comprehensive Specialized Hospital; UoGCSH, University of Gondar Comprehensive Special Hospital; WHO, World Health Organization.
Data Sharing Statement
All relevant data are available within the manuscript.
Ethical Approval and Consent to Participate
Ethical approval was obtained from the School of Nursing, College of Medicine and Health Science, University of Gondar Research and Ethics Committee (Ref No: S/N/245/2014). Since it was a retrospective cross-sectional study, informed consent was waived by the ethics committee. All procedures were made according to the Helsinki declaration. Confidentiality was maintained at all levels of the study.
Acknowledgments
The authors’ heartfelt gratitude goes to the university of Gondar, Northwest Amhara comprehensive Specialized Hospital managers, emergency department coordinators, and medical record room staff and data collectors.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The authors were not funded for this work.
Disclosure
The authors have declared that they have no competing interests in this work.
References
1. Tefera GM, Teferi LG. Prevalence, Predictors and Treatment Outcome of Acute Poisoning in Western Ethiopia. Open Access Emerg Med. 2020;12:365–375. doi:10.2147/OAEM.S277269
2. Amir A, Haleem F, Mahesar G, et al. Epidemiological, Poisoning Characteristics and Treatment Outcomes of Patients Admitted to the National Poisoning Control Centre at Karachi, Pakistan: a Six Month Analysis. Cureus. 2019;11(11):e6229. doi:10.7759/cureus.6229
3. Wang L, Wu Y, Yin P, et al. Poisoning deaths in China, 2006–2016. Bull World Health Organ. 2018;96(5):314–26A. doi:10.2471/BLT.17.203943
4. Pourmand A, Wang J, Mazer M. A Survey of Poison Control Centers Worldwide. Springer; 2012:1–3.
5. Warner M, Chen LH, Makuc DM, Anderson RN, Minino AM. Drug poisoning deaths in the United States, 1980–2008. NCHS Data Brief. 2011;81(81):1–8.
6. Karimkhani C, Dellavalle RP, Coffeng LE, et al. Global skin disease morbidity and mortality: an update from the global burden of disease study 2013. JAMA Dermatol. 2017;153(5):406–412. doi:10.1001/jamadermatol.2016.5538
7. Nigussie S, Demeke F, Getachew M, Amare F. Treatment outcome and associated factors among patients admitted with acute poisoning in a tertiary hospital in Eastern Ethiopia: a cross-sectional study. SAGE Open Med. 2022;10:20503121221078155. doi:10.1177/20503121221078155
8. Endayehu Y, Shenkutie E. Magnitude of acute poisoning and associated factors in Debre Tabor General Hospital, Ethiopia. J Clin Toxicol. 2019;9(5):57.
9. Chelkeba L, Mulatu A, Feyissa D, Bekele F, Tesfaye BT. Patterns and epidemiology of acute poisoning in Ethiopia: systematic review of observational studies. Arch Public Health. 2018;76(1):1–10. doi:10.1186/s13690-018-0275-3
10. Woyessa AH, Palanichamy T. Patterns, Associated Factors, and Clinical Outcomes of Poisoning among Poisoning Cases Presented to Selected Hospitals in Western Ethiopia: hospital-Based Study. Emerg Med Int. 2020;2020:5741692. doi:10.1155/2020/5741692
11. Getie A, Belayneh YM. A Retrospective Study of Acute Poisoning Cases and Their Management at Emergency Department of Dessie Referral Hospital, Northeast Ethiopia. Drug Healthc Patient Saf. 2020;12:41–48. doi:10.2147/DHPS.S241413
12. Zemedie B, Sultan M, Zewdie A. Acute Poisoning Cases Presented to the Addis Ababa Burn, Emergency, and Trauma Hospital Emergency Department, Addis Ababa, Ethiopia: a Cross-Sectional Study. Emerg Med Int. 2021;2021:6028123. doi:10.1155/2021/6028123
13. Adinew GM, Woredekal AT, DeVos EL, Birru EM, Abdulwahib MB. Poisoning cases and their management in emergency centres of government hospitals in northwest Ethiopia. Af j em med. 2017;7(2):74–78. doi:10.1016/j.afjem.2017.04.005
14. Kassahun M, Wongiel S. Food poisoning outbreak investigation in Dewachefa woreda, Oromia Zone, Amhara Region, Ethiopia, 2018. BMC Res Notes. 2019;12(1):1–6. doi:10.1186/s13104-019-4407-9
15. Desalew M, Aklilu A, Amanuel A, Addisu M, Ethiopia T. Pattern of acute adult poisoning at Tikur Anbessa specialized teaching hospital, a retrospective study, Ethiopia. Hum Exp Toxicol. 2011;30(7):523–527. doi:10.1177/0960327110377520
16. Bereda G, Bereda G. Incidence, circumstances and predictors of acute poisoning in emergency department of Mettu Karl Referral hospital, South Western, Ethiopia: a retrospective cross sectional study. Int J Adv Res Biol Sci. 2021;8(7):81–89.
17. Organization WH. Mortality Rate Attributed to Unintentional Poisoning (per 100 000 Population). Geneva: World Health Organization; 2021.
18. Kopec KT, Vohra R, Santos C, Kazzi Z, Wong A. The Global Educational Toxicology Toolkit (GETKIT): a 1-day course for teaching poisoning essentials in low-and middle-income countries (LMIC): course development and pilot data analysis. J Med Toxicol. 2020;16(3):255–261. doi:10.1007/s13181-019-00745-8
19. Mathew R, Jamshed N, Aggarwal P, Patel S, Pandey RJ. Profile of acute poisoning cases and their outcome in a teaching hospital of north India. J Family Med Primary Care. 2019;8(12):3935.
20. Mehrpour O, Akbari A, Jahani F, et al. Epidemiological and clinical profiles of acute poisoning in patients admitted to the intensive care unit in eastern Iran (2010 to 2017). BMC Emerg Med. 2018;18(1):1–9. doi:10.1186/s12873-018-0181-6
21. Mittal N, Shafiq N, Bhalla A, Pandhi P, Malhotra S. A prospective observational study on different poisoning cases and their outcomes in a tertiary care hospital. SAGE Open Med. 2013;1:2050312113504213. doi:10.1177/2050312113504213
22. Getie A, Belayneh YM. A retrospective study of acute poisoning cases and their management at emergency department of Dessie Referral Hospital, Northeast Ethiopia. Drug, healthcare and patient safety. Drug, Healthcare and Patient Safety. 2020;12:41.
23. Afshari M, Poorolajal J, Assari MJ, Rezapur-Shahkolai F, Karimi-Shahanjarini A. Acute pesticide poisoning and related factors among farmers in rural Western Iran. Toxicol Ind Health. 2018;34(11):764–777. doi:10.1177/0748233718795732
24. Tintinalli J. Tintinalli's Emergency Medicine a Comprehensive Study Guide. McGraw-Hill Education; 2015.
25. Lusa S, Punakallio A, Mänttäri S, et al. Interventions to promote work ability by increasing sedentary workers’ physical activity at workplaces–A scoping review. Appl Ergon. 2020;82:102962. doi:10.1016/j.apergo.2019.102962
26. Dart RC, Goldfrank LR, Erstad BL, et al. Expert consensus guidelines for stocking of antidotes in hospitals that provide emergency care. Ann Emerg Med. 2018;71(3):314–25. e1. doi:10.1016/j.annemergmed.2017.05.021
27. Roberts JR, Reigart JR. Recognition and management of pesticide poisonings. 2013.
28. Amare F, Nigussie S, Getachew M. Treatment outcome and associated factors among patients admitted with acute poisoning in a tertiary hospital in Eastern Ethiopia: a cross-sectional study. SAGE Open Med. 2022;10.
29. Reddy BS, Skaria TG, Polepalli S, et al. Factors associated with outcomes in organophosphate and carbamate poisoning: a retrospective study. Toxicol Res. 2020;36(3):257–266. doi:10.1007/s43188-019-00029-x
30. Chatterjee S, Verma VK, Hazra A, Pal J. An observational study on acute poisoning in a tertiary care hospital in West Bengal, India. Perspect Clin Res. 2020;11(2):75. doi:10.4103/picr.PICR_181_18
31. Bhadade R, deSouza R, Gangawane S. Analysis of Poisoning in Urban Setting: a Single Centre Study. J Assoc Physicians India. 2019;67(4):57–61.
32. Ahuja H, Mathai AS, Pannu A, Arora R. Acute Poisonings Admitted to a Tertiary Level Intensive Care Unit in Northern India: patient Profile and Outcomes. J Clin Diagn Res. 2015;9(10):Uc01–4. doi:10.7860/JCDR/2015/16008.6632
33. Zaghary MMS, Radwan RA, Elsayed RM. Validity of Vital Signs, Coma Scales and Modified APACHE Score in Prediction of Prognosis and Outcome of Acutely Poisoned Patients. Egyptian J Hospital Med. 2021;85(1):2758–2766. doi:10.21608/ejhm.2021.189851
34. J-H Y, Weng Y-M, Chen K-F, Chen S-Y, Lin -C-C. Triage vital signs predict in-hospital mortality among emergency department patients with acute poisoning: a case control study. BMC Health Serv Res. 2012;12(1):1–8. doi:10.1186/1472-6963-12-1
35. Goldhill D, McNarry A. Physiological abnormalities in early warning scores are related to mortality in adult inpatients. Br J Anaesth. 2004;92(6):882–884. doi:10.1093/bja/aeh113
36. Satar S, Seydaoglu G, Akpinar A, et al. Trends in acute adult poisoning in a ten-year period in Turkey: factors affecting the hazardous outcome. Bratisl Lek Listy. 2009;110(7):404–411.
37. Forsberg S, Höjer J, Ludwigs U. Hospital mortality among poisoned patients presenting unconscious. Clin Toxicol. 2012;50(4):254–257. doi:10.3109/15563650.2012.670245
38. Vold ML, Aasebø U, Wilsgaard T, Melbye H. Low oxygen saturation and mortality in an adult cohort: the Tromsø study. BMC Pulm Med. 2015;15(1):1–12. doi:10.1186/s12890-015-0003-5
39. Mejía F, Medina C, Cornejo E, et al. Oxygen saturation as a predictor of mortality in hospitalized adult patients with COVID-19 in a public hospital in Lima. Peru PLoS One. 2020;15(12):e0244171. doi:10.1371/journal.pone.0244171
40. Mohammad YM. Mode of arrival to the emergency department of stroke patients in the United States. J Vasc Interv Neurol. 2008;1(3):83–86.
41. Jobé J, Ghuysen A, D’Orio V. Advanced nurse triage for emergency department. Rev Med Liege. 2018;73(5–6):229–236.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.