Back to Journals » Drug Design, Development and Therapy » Volume 18
Outcome of Darunavir–Cobicistat-Based Regimens in HIV-Infected People Who Have Experienced Virological Failure
Authors Alberton F, Galli L , Lolatto R, Candela C, Gianotti N , Chiurlo M , Ranzenigo M, Strano M, Uglietti A, Castagna A
Received 9 October 2023
Accepted for publication 9 March 2024
Published 10 April 2024 Volume 2024:18 Pages 1153—1163
DOI https://doi.org/10.2147/DDDT.S443775
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Anastasios Lymperopoulos
Francesca Alberton,1 Laura Galli,2 Riccardo Lolatto,2 Caterina Candela,1 Nicola Gianotti,2 Matteo Chiurlo,2 Martina Ranzenigo,2 Martina Strano,2 Alessia Uglietti,3 Antonella Castagna1,2
1Infectious Diseases Unit, Vita Salute San Raffaele University, Milan, Italy; 2Infectious Diseases Unit, San Raffaele Scientific Institute, Milan, Italy; 3Medical Affairs Department, Infectious Diseases and Vaccines & Rare Diseases, Johnson&Johnson, Milan, Italy
Correspondence: Alessia Uglietti, Medical Affairs Department, Infectious Disease and Vaccines & Rare Diseases, Johnson&Johnson, viale Fulvio Testi 280/6, Milan, 20126, Italy, Tel +39-344 2665502, Email [email protected]
Objective: To evaluate the virological outcome of darunavir–cobicistat (DRVc)‐based regimens in adults living with HIV who had experienced virological failure (VF) on any previous drug combination.
Methods: This was a retrospective cohort study (CSLHIV Cohort) of adults living with HIV who started a DRVc‐based regimen with HIV‐RNA > 50 copies/mL after VF on any previous drug combination. Data on demographics, antiretroviral treatment since HIV diagnosis, and immunological and metabolic parameters from baseline (start of DRVc) to 48 weeks were analyzed in order to assess the cumulative proportion of those who achieved virological success (VS), defined as at least one instance of HIV‐RNA < 50 copies/mL within 12 months from baseline. Follow-up lasted from the start of the DRVc-based regimen (baseline) to the first instance of HIV-RNA < 50 copies/mL, last available visit, or loss to follow‐up or death, whichever occurred first. Univariate and multivariate Cox proportional-hazard regression models were used to identify baseline factors associated with VS.
Results: A total of 176 individuals were included, and 120 (68.2%) achieved < 50 HIV‐RNA copies/mL within 12 months since baseline. On multivariate analysis, baseline HDL cholesterol was independently associated with the occurrence of VS (adjusted HR 1.021, 95% CI 1.004– 1.038; p=0.014). Among the 120 subjects with VS, 27 (22.5%) had had VF during a median follow-up of 20.8 months since the first undetectable HIV-RNA. Resistance testing after VF was available in two cases, which harboured the HIV variant–bearing protease inhibitor–resistance mutations D30N, I50V, and N88D. During a median follow-up of 38.4 months, 65 of 176 (36.9%) individuals discontinued DRVc for any reason (37 of 120, 30.8%) and achieved VS vs. 28 of 56 (50%) without VS (p=0.019). Time to discontinuation was longer in people with VS (41.5 vs. 23.0 months, p=0.0007). No statistically significant changes were observed in immunological or lipid profiles during follow-up.
Conclusion: Most individuals in this study achieved VS within 12 months from the beginning of a DRVc-based regimen; therefore, this treatment represent a viable option for people who have experienced VF on other regimens.
Keywords: HIV infection, antiretroviral therapy, ART, darunavir–cobicistat, DRVc, virological failure, VF
Introduction
Boosted darunavir (bDRV) is included in international guidelines for HIV1-infection therapy, both for treatment-naïve and treatment-experienced people, and in cases of virological failure (VF) with single- or multiclass resistance, as long as it proves to be fully active and in combination with at least another active drug.1 Ritonavir-boosted DRV (DRVr) 600/100 mg twice daily has proved to be highly effective in HIV-infected, treatment-experienced individuals showing VF and primary protease inhibitor (PI)-resistance mutations.2,3
It was later demonstrated that once-daily DRVr 800/100 mg was as effective as DRVr 600/100 mg twice daily in treatment-experienced patients with no DRV resistance-associated mutations, with a lower incidence of lipid profile worsening.4 A fixed-dose formulation of DRV–cobicistat (DRVc) was next developed and a once-daily single-tablet formulation of DRVc–emtricitabine (FTC)–tenofovir alafenamide (TAF) showed efficacy, a high barrier to resistance, tolerability, and bone and renal function safety benefits in treatment-naïve HIV1 patients.5
For these reasons, DRVc currently represents a natural choice for people living with HIV (PLWH) developing VF under non–nucleoside reverse-transcriptase inhibitor (NNRTI)-based regimens, integrase strand-transfer inhibitor (InSTI)-based regimens, or most PI-based regimens, thanks to the absence of cross-resistance. However, data on the efficacy of DRVc as a rescue drug are very scarce,6,7 as most of the data (even recent) come from clinical studies where DRV was boosted with ritonavir.8
Therefore, reviewing the efficacy of once-daily DRVc in a representative number of PLWH experiencing VF may provide important and useful clinical information. The primary aim of this 48-week analysis was to describe the virological outcome of DRVc‐based regimens in an adult HIV‐infected cohort who had experienced VF on any previous drug combination.
Methods
This was a retrospective cohort study carried on adult male and female outpatients attending the San Raffaele Infectious Diseases Department (HIVCSL Cohort). The analysis included treatment‐experienced PLWH aged ≥18 years at the start of a DRVc‐based regimen who had shown VF (>50 copies/mL) on any previous drug combination. Individuals were excluded in cases of documented resistance to DRV (according to the Stanford algorithm [HIVdb Program, version 9.0, last updated February 22, 2021]).
The primary endpoint of this analysis was the 48-week cumulative proportion of individuals who achieved virological success (VS), defined as at least one instance of HIV‐RNA <50 copies/mL, within 12 months since the start of the DRVc‐based regimen. Secondary endpoints were: time to VS, including estimates of cumulative probabilities of VS by Kaplan–Meier curves; factors associated with achievement of VS; proportion of subjects who lost VS after achievement and underwent VF, defined as those who had two consecutive HIV‐RNA values >50 copies/mL or a single HIV‐RNA value >1000 copies/mL after reaching undetectable viral load; proportion of subjects who discontinued the DRVc‐based regimen for any reason; reasons for discontinuation of the DRVc‐based regimen; time to DRVc‐based regimen discontinuation for any reason; and mean changes in main immunological and metabolic laboratory parameters during the DRVc‐based regimen.
Follow-up accrued began from the start of a DRVc-based regimen (baseline). In the primary analysis on the primary endpoint (time to VS achievement), follow‐up was censored to the date of first instance of HIV-RNA <50 copies/mL, last available visit, loss to follow‐up, or death, whichever occurred first within 12 months since baseline. For the secondary analyses on some secondary endpoints, follow‐up was censored to the date of last available visit under the DRVc-based regimen treatment, loss to follow‐up, or death, as appropriate.
Subjects’ characteristics are presented as medians (quartile 1 to quartile 3) or frequency (%) and compared by the Mann–Whitney or χ2/Fisher’s exact tests, as appropriate. The cumulative probabilities of VS and discontinuation for any reason were estimated using Kaplan–Meier curves. A multivariate Cox proportional hazard regression model was generated to identify baseline factors associated with the achievement of VS hazard ratios with corresponding 95% confidence intervals. The model comprised the covariates (p<0.15 on univariate analyses) calendar year of DRVc-based regimen start, type of antiretroviral therapy (ART) regimen previously failed, number of previous VFs, number of antiretroviral drugs never previously used with DRVc, and baseline HDL cholesterol. If necessary, variables were omitted in order to avoid collinearity.
The number of antiretroviral drugs previously used (r=0.499, p<0.0001), the number of NRTIs previously used (r=0.461, p<0.0001), and the number of PIs previously used (r=0.479, p<0.0001) were not included in the final model because of collinearity with the number of previous VFs. The number of NRTIs previously used (r=−0.217, p=0.004) and the number of PIs previously used (r=−0.153, p=0.043) were also excluded from the final model because of collinearity with the number of antiretroviral drugs never previously used with DRVc). We checked the proportional hazard assumption for the Cox model by adding time-dependent variables to the original final model (ie, the product of each factor significantly associated with VS and logarithm of time), As no statistically significant results were observed, the assumption of proportional hazards was satisfied for all the covariates considered.
Significant changes in laboratory parameters were explored using univariate mixed linear models (with random slope, random intercept, and unstructured variance–covariance matrix), as there were more than two available determinations per individual for all the laboratory parameters during treatment with a DRVc-based regimen. Analyses were conducted using two‐sided tests at α=0.05 with SAS 9.4 (SAS Institute Inc, Cary, NC).
Results
Baseline Characteristics
Overall, 176 individuals who met the aforementioned inclusion criteria were included in the analysis. At the beginning of DRVc treatment (baseline), males represented 77.3% (136/176) of the study population, with a median (quartile 1 to quartile 3) age of 52.3 (44.4–57.3) years. Subjects had had a known HIV infection lasting 17.1 (9.6–27.5) years and had been on ART for 15.2 (5.7–21.4) years. Nadir CD4+ lymphocyte count was 190 (66–307) cells/µL, with 52.3% of population <200 cells/µL, while their current CD4+ count was 470 (281–722) cells/µL with 16.2% <200 cells/µL. At baseline, median HIV-RNA load was 209 (96–2682) copies/mL. An AIDS diagnosis was present in 59 subjects (33.5%) and a history of HBV and HCV coinfection in 14 (8%) and 46 (26.1%) (with positive HCV-RNA in 19/46 [42.2%]) individuals, respectively.
Among 130 subjects who had previous reverse-transcriptase and protease HIV1 genotype-resistance test (GRT) and 115 InSTI GRT data available, the presence of at least one NRTI-, NNRTI-, PI-, or InSTI-resistance mutation was identified in 51 (39.2%), 35 (26.9%), 8 (6.2%), and 17 (14.8%) individuals, respectively. At the time of inclusion-qualifying VF, 106 individuals (60.2%) were on a three-drug regimen (InSTI-based [n=49, 27.8%], PI-based [n=57, 32.4%]), 24 (13.6%) were on a two-drug regimen (2DR): bDRV + dolutegravir (DTG) in eight cases, bDRV + rilpivirine in one case and bDRV + lamivudine (3TC) in one case), six (3.4%) on boosted PI monotherapy, and 40 (22.7%) on other regimens, eg, FTC–TAF + bDRV + DTG in 11 cases, bDRV + DTG + maraviroc in three cases, and 3TC + bDRV + DTG in two cases. The most frequent failing regimens were FTC–TAF–bictegravir (BIC) in 15 cases (8.5%), FTC–tenofovir disoproxil fumarate (TDF)–DRVr in 12 cases (6.8%), FTC–TAF–DTG in 11 cases (6.3%), and 3TC–abacavir–DTG in nine cases (5.1%). NNRTI-based regimens failed in 28 individuals (15.9%).
The main DRVc-based regimens chosen after VF occurrence were FTC–TAF–DRVc (n=76, 43.2%), FTC–TAF–DRVc + DTG (n=27, 15.3%), FTC–TDF + DRVc (n=25, 14.2%), and DRVc + DTG (n=14, 8%). Overall, 61.4% (n=108) of these regimens were made up of DRVc + two NRTIs and 11.9% (n=21) DRVc + one drug from a different class combined in a 2DR. Furthermore, 89.2% (n=157) of regimens included at least one NRTI (usually two), only 4% (n=7) included an NNRTI, and 31.3% (n=55) included an InSTI combined with DRVc. Finally, in six subjects (3.4%), a fusion inhibitor was part of the DRVc-based treatment. Further details on the baseline characteristics of the individuals included in the analysis are shown in Table 1.
 |
Table 1 Main baseline characteristics of the 176 individuals starting a DRVc-based regimen after a virological failure on any previous drug combination |
Virological Responses
During 1389 person-months of follow-up (median 3.8 [1.6–9.1) months]), 120 of 176 (68.2%, 95% CI 61%–74.6%) achieved VS within 12 months since the start of the DRVc‐based regimen, for an overall incidence of VS of 8.6 per 100 person-months of follow-up (95% CI 7.1–10.2). The 12-month cumulative probability of VS was 76.1% (95% CI 68.9%–82.7%), and the corresponding Kaplan–Meier curve is shown in Figure 1. At last visit, HIV-RNA value distribution was 58.8% >50 copies/mL and 29.1% ≥50 copies/mL, with 17.6% missing. Among those 56 individuals who did not achieve VS within 12 months, median HIV-RNA was 81 (52–207) copies/mL. Among the 120 who achieved VS, 27 (22.5%, 95% CI 15.9%–30.8%) experienced VF during a median follow-up of 20.8 (IQR 9.1–46.4) months since first undetectable HIV-RNA. Figure 2 shows the cumulative probability of VF on the DRVc-based regimen in those who achieved HIV-RNA <50 copies/mL within 12 months since the start of this ART regimen. Resistance testing at VF was available for two people. In one, the drug-resistance mutations D30N, I50V, N88D were detected, conferring potential low-level resistance to DRV. In the second case, no PI-resistance mutations were detected. On multivariate analysis, baseline HDL cholesterol was independently associated with the risk of VS (adjusted HR 1.021, 95% CI 1.004–1.038, p=0.014; Table 2).
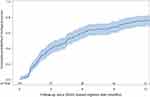 |
Figure 1 Cumulative probability of virological success since the start of the DRVc‐based regimen (baseline). |
 |
Figure 2 Cumulative probability of virological failure of the DRVc-based regimen in those who achieved HIV-RNA <50 copies/mL within 12 months since the start of the regimen. |
 |
Table 2 Multivariate Cox proportional-hazard model on risk of virological success among people treated with a DRVc-based regimen |
Treatment Discontinuation
Overall, during a median follow-up of 24.1 (IQR 11.7–46.9) months, 86 of 176 (48.9%, 95% CI 41.6–56.2%) individuals discontinued at least one drug of the DRVc-based regimen for any reason. Median time to discontinuation was longer in subjects with VS: 29.06 (IQR 16.84–48.9) vs. 14.18 (IQR 3.6–38.36) months (p<0.0001). During a median follow-up of 38.4 (IQR 16.4–50.5) months, 65 of 176 (36.9%, 95% CI 30.2%–44.3%) subjects specifically discontinued DRVc for any reason. Median time to discontinuation was longer in subjects with VS: 41.5 (IQR 20–60.6) vs. 23 (IQR 7.2–44.5) months (p=0.0007). The cumulative probability of DRVc discontinuation for any reason following achievement of VS is shown in Figure 3. Overall, the main reasons for discontinuation were represented by patient decision/noncompliance in 11 of 65 (16.9%; two of 37 [5.4%] among those who achieved VS and nine of 28 [32.2%] among those who did not), recurrent viral blips (without VF) in eight of 65 (12.3%; three of 37 [8.1%] vs. five of 28 [17.9%]), simpler or more convenient regimen in eight of 65 (12.3%; six of 37 [16.2%] vs. two of 28 [8%]), dyslipidemia in six of 65 (9.2%; five of 37 [13.5%] vs. 1/28 [3.6%]), concerns about cardiovascular disease in four of 65 (6.2%; three of 37 [8.1%] vs. 1/28 [3.6%]), drug interactions in four of 65 (6.2%; four of 37 [10.8%] vs. none of 28), and toxicity/side effects in seven of 65 (10.7%; three of 37 [8.1%] vs. four of 28 [14.3%]): one case each of hypersensitivity, abnormal fat redistribution, and nervous system toxicity and two cases each of of kidney toxicity and osteopenia/osteoporosis Details are reported in Table 3.
 |
Figure 3 Cumulative probability of DRVc discontinuation for any reason according to the following achievement of virological success. |
 |
Table 3 Reasons for DRVc discontinuation following achievement of virological success (no statistically significant differences observed between these two groups; p=0.058) |
Safety Parameters
A panel of immunological and metabolic laboratory parameters collected during the DRVc‐based regimen treatment period were analyzed. A slight increase in CD4+ cell count (VS: 5.37 [95% CI 2.36–8.39] cells/µL, p=0.0005; no VS: 2.76 [95% CI −1.93 to 7.46] cells/µL, p=0.249; VS vs. no VS: p=0.930) and CD4:CD8 ratio (VS: 0.009 [95% CI 0.003–0.015], p=0.005; no VS: 0.002 [95% CI −0.009 to 0.012], p=0.773; VS vs. no VS: p=0.096) was found. A statistically significant slope was observed for estimated glomerular filtration rate (eGFR; VS: −0.319 [95% CI −0.635 to −0.1] mL/min/1.73 m2, p=0.007; no VS: −0.158 [95% CI −0.618 to 0.301] mL/min/1.73 m2, p=0.499; VS vs. no VS: p=0.327) and Fibrosis 4 (FIB4) index for liver fibrosis (VS: −0.076 [95% CI −0.129 to −0.023], p=0.005; no VS: −0.705 [95% CI −1.092 to −0.319], p=0.0007; VS vs. no VS: p<0.0001). No statistically significant changes in lipid profile were observed, as shown in Table 4.
 |
Table 4 Immunovirological and safety parameters during treatment with DRVc-based regimen |
Discussion
DRVc-based regimens, such as those based on DRVr, are widely used and recommended by international guidelines in treatment-naïve PLWH, especially in situations where a rapid reduction in viral load is needed before resistance tests are available (eg, in acute infection) or in conditions of potentially poor adherence to therapy.1,9–11The usefulness of collecting efficacy data on DRVc-based regimens not extrapolated from studies on DRVr arises mainly from two peculiarities of such regimens. The first consists in the presence of cobicistat as a pharmacokinetic booster, endowed with greater selectivity of CYP3A inhibition than ritonavir and fewer side effects and drug–drug interactions.12–14 The second is the unicity of DRVc–FTC–TAF as fixed-dose and single-tablet regimens containing PI combined with an NRTI backbone, thus offering an advantage in terms of reduction in pill burden and medication errors.15 Both of these factors are relevant in constructing an effective therapy regimen after VF, as they contribute to limiting the risk of nonadherence to therapy.
In the analyzed cohort of 176 adult PLWH who had failed on a previous antiretroviral regimen, after 48 weeks of follow-up in a real-life setting, 68.2% achieved VS in a median time of 3.8 months, with a 12-month cumulative probability of VS of 76.1%. This result is consistent with those observed in the phase III, 48-week, open-label ODIN study, which proved noninferiority in virological response to once-daily DRVr 800/100 mg (72.1% HIV-RNA <50 copies/mL at week 48) to twice-daily 600/100 mg (70.9%) when combined with an optimized background regimen in treatment-experienced PLWH without DRV resistance–associated mutations.4
A multivariate Cox proportional hazard model was used to identify factors predicting virological success using the data of 144 subjects, 103 of whom achieved VS. Favorable response seemed not to be conditioned by past antiretroviral regimens or previous VF, and baseline HDL cholesterol was the only parameter independently associated with the probability of VS (p=0.014). These data, together with some observations of discontinuation causes, suggest a significant role of adherence in achieving VS compared with other factors, such as past drug exposure.
In fact, the beneficial effect of DRVc on the lipid profile and in particular on triglycerides and high-density lipoproteins is known in cases of switching from ritonavir,15,16 which represents only a fraction of the switches in our cohort. The association of VS with higher baseline HDL cholesterol cannot reveals the effect of initiating DRVc, but rather could work as a performance indicator (or a proxy variable) of overall adherence to therapies (eg, lipid-lowering drugs) of subjects who achieved VS compared with those who did not. A similar perception, which cannot be demonstrated since lipid-lowering therapies were not available for the subjects included, is also evident from the reasons for discontinuation (Table 3), where dyslipidemia had greater incidence in those who achieved VS, while such items as recurrent viral blips, noncompliance, and patient decision had higher incidence in patients who did not achieve VS, as an effect of more and less regular intake, respectively.
Among immunological and metabolic markers monitored during the DRVc‐based regimen treatment period, the slight increase in CD4+ cell count and CD4:CD8 ratio is consistent with CD4+ cell recovery reported in treatment-experienced and -naïve PLWH.6,17 This tendency is confirmed in favor of those who achieved VS, though not significantly. A statistically significant slope for eGFR is attributable to cobicistat’s known mechanism of inhibition of the tubular secretion of creatinine while not affecting actual renal function.18
Of the 120 subjects who achieved VS, 52 (43.3%) discontinued at least one drug of the DRVc-based regimen after a median 29 months, and 37 of 52 discontinued DRVc after a median 41.5 months. In sum, 27 of 120 (22.5%) developed VF during a median follow-up of 20.8 months since first undetectability, and only in one case did GRT at VF highlight mutations (D30N, I50V, N88D) conferring potential low-level resistance to DRVr in a subject previously exposed to lopinavir–ritonavir, as recently described by Abdullahi et al.19
The main limitation of this analysis lies in its retrospective design, lack of a standardized evaluation of adherence to treatment, and relatively small sample that may not be representative of the national population. Further, there may be some missing data for some variables, despite individuals’ information being generally accurately recorded in the CSLHIV Cohort database by each referring physician during each visit. In addition, this was a single-center study. On the other hand, it contributes to evidence for therapeutic effectiveness in real-world practice settings.
Conclusion
Most PLWH who experienced VF in this study achieved virological success within 12 months from the beginning of a DRVc-based regimen. DRVc-based regimens represent a viable option in cases of loss of virological control and no DRV-resistance mutations, with no significant impact on lipid profile and with bone and renal safety benefits. Prospective observational studies designed to collect data on real-world treatment–experienced PLWH are crucial for further understanding of the role of adherence and other predicting factors on outcomes.
Ethics and Consent
Individuals provided written informed consent to the use of their data in scientific analyses and to be included in the Centro San Luigi (CSL) HIV Cohort. The CSL-HIV Cohort was approved by the Ethics Committee of the IRCCS San Raffaele Scientific Institute (Milan, Italy; date of approval 4th December 4, 2017, protocol 34). The study described in the manuscript was conducted in accordance with the principles of Good Clinical Practice and the Declaration of Helsinki.
Acknowledgments
The authors thank Diana Canetti for medical writing on behalf of the IRCCS San Raffaele Scientific Institute and Johnson & Johnson Italy.
Funding
This analysis was funded by Johnson & Johnson Italy.
Disclosure
AC has received personal fees for advisory boards, speaker panels, and educational materials from Gilead Sciences, ViiV Healthcare, Janssen-Cilag, Merck Sharp & Dohme, and Theratechnologies. NG has been an advisor for Gilead Sciences, Janssen-Cilag, ViiV Healthcare and Merck Sharp & Dohme and has received speakers’ honoraria from Gilead Sciences, ViiV Healthcare, Janssen-Cilag and Merck Sharp & Dohme. FA, LG, RL, CC, MC, MR, MS declare no competing interests. AU is an employee of Johnson & Johnson Italy.
References
1. EACS Guidelines version 11.1; 2022. Available from: https://eacs.sanfordguide.com/.
2. Clotet B, Bellos N, Molina J-M, et al. Efficacy and safety of darunavir-ritonavir at week 48 in treatment-experienced patients with HIV-1 infection in POWER 1 and 2: a pooled subgroup analysis of data from two randomised trials. Lancet. 2007;369(9568):1169–1178. doi:10.1016/S0140-6736(07)60497-8
3. Katlama C, Haubrich R, Lalezari J, et al. Efficacy and safety of etravirine in treatment-experienced, HIV-1 patients: pooled 48 week analysis of two randomized, controlled trials. AIDS. 2009;23(17):2289–2300. doi:10.1097/QAD.0b013e3283316a5e
4. Cahn P, Fourie J, Grinsztejn B, et al. Week 48 analysis of once-daily vs. twice-daily darunavir/ritonavir in treatment experienced HIV-1-infected patients. AIDS. 2011;25(7):929–939. doi:10.1097/QAD.0b013e328345ee95
5. Orkin C, Eron JJ, Rockstroh J, et al. Week 96 results of a Phase 3 trial of darunavir/cobicistat/emtricitabine/tenofovir alafenamide in treatment-naive HIV-1 patients. AIDS. 2020;34(5):707–718. doi:10.1097/QAD.0000000000002463
6. Tashima K, Crofoot G, Tomaka FL, et al. Cobicistat-boosted darunavir in HIV-1-infected adults: week 48 results of a Phase IIIb, open-label single-arm trial. AIDS Res Ther. 2014;11(1):39. doi:10.1186/1742-6405-11-39
7. Lee SA, Kim S-W, Chang H-H, et al. Effectiveness, safety, and tolerability of a switch to dual therapy with dolutegravir plus cobicistat-boosted darunavir in treatment-experienced patients with human immunodeficiency virus. Infect Chemother. 2018;50(3):252–262. doi:10.3947/ic.2018.50.3.252
8. Paton NI, Musaazi J, Kityo C, et al. Dolutegravir or darunavir in combination with zidovudine or tenofovir to treat HIV. N Engl J Med. 2021;385(4):330–341. PMID: 34289276. doi:10.1056/NEJMoa2101609
9. Eron JJ, Orkin C, Gallant J, et al. A week-48 randomized phase-3 trial of darunavir/cobicistat/emtricitabine/tenofovir alafenamide in treatment-naive HIV-1 patients. AIDS. 2018;32(11):1431–1442. doi:10.1097/QAD.0000000000001817
10. Huhn GD, Crofoot G, Ramgopal M, et al. Darunavir/cobicistat/emtricitabine/tenofovir alafenamide in a rapid-initiation model of care for human immunodeficiency virus type 1 infection: primary analysis of the diamond study. Clin Infect Dis. 2020;71(12):3110–3117. doi:10.1093/cid/ciz1213
11. Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in adults and adolescents with HIV. Department of Health and Human Services; 2023. Available from: https://clinicalinfo.hiv.gov/en/guidelines/adult-and-adolescent-arv.
12. Xu L, Liu H, Murray BP, et al. Cobicistat (GS-9350): a potent and selective inhibitor of human CYP 3A as a novel pharmacoenhancer. ACS Med Chem Lett. 2010;1(5):209–213. doi:10.1021/ml1000257
13. Gallant JE, Koenig E, Andrade-Villanueva J, et al. Cobicistat versus ritonavir as a pharmacoenhancer of atazanavir plus emtricitabine/tenofovir disoproxil fumarate in treatment-naive HIV type 1-infected patients: week 48 results. J Infect Dis. 2013;208(1):32–39. doi:10.1093/infdis/jit122
14. Bangalore S, Kamalakkannan G, Parkar S, et al. Fixed dose combinations improve medication compliance: a meta-analysis. Am J Med. 2007;120(8):713–719. doi:10.1016/j.amjmed.2006.08.033
15. Gori A, Antinori A, Vergori A, et al. Effectiveness of switching to darunavir/cobicistat in virologically suppressed HIV-positive patients receiving ritonavir-boosted protease inhibitor-based regimen: the ”STORE” Study. Study J Acquir Immune Defic Syndr. 2020;84(3):290–294. PMID: 32101882; PMCID: PMC7289135. doi:10.1097/QAI.0000000000002331
16. Echeverría P, Bonjoch A, Puig J, et al. Significant improvement in triglyceride levels after switching from ritonavir to cobicistat in suppressed HIV-1-infected subjects with dyslipidaemia. HIV Med. 2017;18(10):782–786. PMID: 28671337. doi:10.1111/hiv.12530
17. Taiwo B, Zheng L, Gallien S, et al.; ACTG A5262 Team. Efficacy of a nucleoside-sparing regimen of darunavir/ritonavir plus raltegravir in treatment-naive HIV-1-infected patients (ACTG A5262). AIDS. 2011;25(17):2113–2122. PMID: 21857490; PMCID: PMC3515052. doi:10.1097/QAD.0b013e32834bbaa9
18. German P, Liu HC, Szwarcberg J, et al. Effect of cobicistat on glomerular filtration rate in subjects with normal and impaired renal function. J Acquir Immune Defic Syndr. 2012;61(1):32–40. doi:10.1097/QAI.0b013e3182645648
19. Abdullahi A, Diaz AG, Fopoussi OM, et al. A detailed characterization of drug resistance during darunavir/ritonavir monotherapy highlights a high barrier to the emergence of resistance mutations in protease but identifies alternative pathways of resistance. J Antimicrob Chemother. 2024;79(2):339–348. doi:10.1093/jac/dkad386
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
