Back to Journals » Journal of Multidisciplinary Healthcare » Volume 14
Optimal Nutritional Factors Influencing the Duration of Mechanical Ventilation Among Adult Patients with Critical Illnesses in an Intensive Care Unit
Authors Koontalay A , Suksatan W , Sadang JM, Prabsangob K
Received 10 May 2021
Accepted for publication 25 May 2021
Published 10 June 2021 Volume 2021:14 Pages 1385—1393
DOI https://doi.org/10.2147/JMDH.S319553
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Apinya Koontalay,1 Wanich Suksatan,2 Jonaid M Sadang,3 Kantapong Prabsangob4
1Independent Researcher, Melbourne, VIC, Australia; 2Faculty of Nursing, HRH Princess Chulabhorn College of Medical Science, Chulabhorn Royal Academy, Bangkok, Thailand; 3College of Health Sciences, Mindanao State University, Marawi, Philippines; 4College of Allied Health Sciences, Suan Sunandha Rajabhat University, Samut Songkram, Thailand
Correspondence: Wanich Suksatan
Faculty of Nursing, HRH Princess Chulabhorn College of Medical Science, Chulabhorn Royal Academy, Bangkok, Thailand
Tel +66827550027
Email [email protected]
Kantapong Prabsangob
College of Allied Health Sciences, Suan Sunandha Rajabhat University, Samut Songkram, Thailand
Tel +66840412068
Email [email protected]
Objective: This study aims to identify the impact of nutritional factors on mechanical ventilation duration for critical patients.
Patients and Methods: The current study was a single-center, prospective observational design which enrolled one-hundred critically ill patients who were admitted to an intensive care unit (ICU). It demonstrates purposive sampling and also performs the descriptive nutritional factors influencing the mechanical ventilation duration. Daily calories target requirement scale (DCRS), subjective global assessment form (SGA), dyspnea assessment form, and APACHE II have been used as methods in the study along with time to initial enteral nutrition (EN) after 24-hour admission and daily calories target requirement over 7 days to assess patients. Data is analyzed using the multiple regressions.
Results: As a result, nutritional status monitoring, time to initial EN, calories and target requirements are statistically positive significance associated with the mechanical ventilation duration respectively (R = 0.54, R = 0.30, R= 0.40, p < 0.05). However, age, illness severity, and dyspnea scales are not associated with the mechanical ventilation duration (p> 0.05). Therefore, the nutritional status, malnutrition scores and calorie target requirements can be used to significantly predict the mechanical ventilation duration. The predictive power is 58 and 28.0% of variance. The most proper influencer to predict the mechanical ventilation duration is nutritional status or malnutrition scores.
Conclusion: The research findings show that the nutritional status, time to initial EN, and calorie target requirement within 7 days of admission are associated with the mechanical ventilation duration in the critical patients. Therefore, it can be used to develop guidelines reducing the mechanical ventilation duration and to promote the ventilator halting for critical patients.
Keywords: critical care, enteral feeding, mechanical ventilation, nutritional status
Introduction
The critical patients usually have dysfunctional respiratory or circulation systems failure.1,2 In serious conditions, their bodies respond to inflammatory stimulating systems due to hypermetabolic and hypercatabolic and determine the malnutrition.3,4 Their energy and protein have been decreased because hypercatabolic significantly leading to infection complications, delayed recovery, constant hospitalization, or mechanical ventilation.5 The malnutrition prevalence is associated with chronic diseases, particularly in 40% to 60% of patients resulting from changes in systematic functions,6 such as loss of body mass, respiratory function impairment, diaphragm muscle weakness, fat or protein depletion and admission time, leading to morbidity and mortality.7,8
The critical illness steadily increases hypermetabolism as protein and fats in muscle tend to decrease, especially the diaphragm resulting in muscle atrophy, fatigue movement, difficult breathing and extended mechanical ventilation.3,4 The American Society of Parenteral and Enteral Nutrition (ASPEN)4 recommended that ICU patients should start enteral nutrition (EN) support within 24 to 48 hours of admission or after resuscitation4 in order to maintain systemic immune functions and structure of major organs.9 Accordingly, the American Society of Parenteral and Enteral Nutrition (ASPEN) recommended that 75.6% of patients receive adequate protein and 61.2% meet energy requirements within the first 7 days of admission. It can improve their respiratory function, structure, increase weaning ability10 and reduce mechanical ventilator duration.11
It has been discovered that nutrition importantly supports critical patient recovery by affecting treatment outcome and mechanical ventilator duration.12 Factors correlated with nutritional conditions for critical patients using ventilator have been studied, however, it is not applied. Therefore, this study purposedly focuses on factors influencing the mechanical ventilators duration for critical patients.1–6 The selected factors include malnutrition, age, disease severity, dyspnea scale, initial EN time, and targeted calorie requirement.6,10–13 It could be defined as a guideline in mechanical ventilation for critical patients13 leading to ventilator availability and reduced admission duration. Therefore, the purpose of the current study was to examine nutritional factors and predict the effect that those variables have on the duration of mechanical ventilation among patients with a critical illness.
Patients and Methods
Research Design and Sampling
This study is a prospective cohort study conducted in the Tertiary Hospital in Thailand between January and October 2019. A sample is derived from a medical-surgical intensive care unit (ICU) includes 8 beds and 360 critically ill patients per year. They are conscious and understand the research purpose and procedure. The purposive samplings include patients age over 18 years who received EN and invasive mechanical ventilator after hemodynamic stable within 6 hours. The study excludes patients who are transferred to another unit or changed to another hospital during treatment as well as who terminated the EN or palliative care. This study uses G*Power program (version 3.1)17 to calculate sample size, test power is examined at 0.80, statistically significant level is 0.05 (α=0.05) and effect size level is 0.25. The sample size is increased by 15% to compensate potential dropout rate. The total eligible participants are 140 persons, 40 participants are dropped out because 37 persons stopping enteral feeding (thirty-seven persons) and 3 persons required a palliative care. They involve in unstable hemodynamic due to their physiological characteristics, so, the final participants are 100 persons (Figure 1).
 |
Figure 1 Study participant’s flow chart in hospitals. |
The researchers selected samples from medical records and collected data by assessing demographic data, disease severity, and nutrition status with malnutrition screening form within 24 hours after admitting to ICU. Additionally, the researchers assessed dyspnea scores within the first 24 hours and after or at least 4 hours after inserting the ventilator. Energy consumption that the patients receive every day and mechanical ventilation duration form are recorded by the researchers, start when the patients are inserted ventilator until they wean off. It includes receiving T-piece 10 LPM and extubated endotracheal tube or ventilator at least 48 hours.
Research Instrument
Daily Calories Target Requirement Scale (DCRS)
DCRS uses Harris Benedict equation x 1.0–1.3 and 1.0–2.0 gram per kilogram of bodyweight to calculate targeted calorie requirement in the first 24 hours after ICU admission and assesses every 7 days. The Cronbach’s alpha coefficient was 0.84 for the pilot and 0.86 for the main study.
Disease Severity Assessment Form (DSAF)
DSAF uses the APACHE II adopted by Knaus et al14 to determine initial 24 hour requirement after ICU admission. It consists of 12 potential physiologic measures with a score range 0 to 7. If the total APACHE II score is 25 or over, it indicates a greater than 50% risk of mortality. The Cronbach’s alpha coefficient was 0.86 for the pilot and 0.93 for the main study.
Dyspnea Scales Form
Dyspnea Scales form uses Dyspnea Visual Analogue Scale (DVAS)15 for dyspnea scales within 24 hours after using an invasive mechanical ventilator and hemodynamic stable. The score is 0 to 100, higher scores determining severe dyspnea. The Cronbach’s alpha coefficient was 0.82 for the pilot and 0.84 for the main study.
Nutritional Status Scale (NSS)
NSS uses Subjective Global Assessment (SGA)16 to assess patients’ nutritional status. The scale consists of 1) good nourish, 2) moderately malnourish (3) severe malnourish as well as a score from 0 to 11. The Cronbach’s alpha coefficient was 0.84 for the pilot and 0.86 for the main study.
Demographic Data
Demographic data consists of three items with multiple choice and open-ended questions, including sex, age, and diagnosis of the patients.
Ethical Considerations
Ethical clearance is obtained from the Research Ethics Committee on Human, Suan Sunandha Rajabhat University (IRB No. 59–043-1-3), Bangkok, Thailand. The current study is conducted in accordance with the Declaration of Helsinki having written consents obtained from the patients after explaining purpose of the study.
Data Collection
The following data is collected:
- Demographic data: over 18 years old, gender, underlying disease and diagnosed to admit in ICU, date of initial invasive mechanical ventilation, mechanical ventilation duration in days, initiation EN in hours, and calorie target requirement in a day.
- Data assessment for the first 24 hours and every 7 days after admission to ICU: disease severity, dyspnea scales, nutrition status, and calorie target requirement in hours.
Study Outcome
The main outcome of this study is mechanical ventilation duration in days.
Statistical Analysis
All data are analyzed using SPSS, version 22.0 (IBM SPSS, Chicago, USA). Descriptive statistics is used to analyze demographics eg, number, percentage, mean, and standard deviation (SD). This study can be categorized as a predictive correlational research to study nutritional factors influencing mechanical ventilator duration. The samples are critical patients using ventilators admitted in an intensive medicine unit. The research instruments include demographic data, nutrition status screening, disease severity assessments, dyspnea scale assessments and calorie target requirement. Data analysis is done by a distribution of frequency, percentage, average, standard deviation, and relationships by finding Pearson correlation coefficient. Pearson correlation coefficient and analyses can predict related factors by determining step-by-step multiplication regression coefficient. Stepwise multiple regression analysis is used to summarize findings and discuss association between nutrition factors and mechanical ventilation duration. The multiple regression analysis with the stepwise method is used to assess nutrition variables as a predictor on mechanical ventilation duration, p < 0.05 is considered significant.
Results
Characteristics of the Study Population
A total number of critical patients admitted in ICU between January to October 2019 was 360 and eligible participants is 140. However, 220 persons are excluded because of non-invasive ventilator (n= 65), start EN longer than 48 hours (n=100), and unstable after resuscitating (n=55), 10 participants are dropped out by discontinuing EN caused by therapeutic procedures (n=7) and palliative care (n=3). Finally, 100 participants are enrolled.
The demographic data and clinical characteristics of the participants consist of 76% men with a mean age of 61.79 (min-max = 20–94 years, SD = 16.99). 40% of the participants are admitted for a medical illness, particularly a cardiovascular system. 52% are severe malnutrition (mean=7.81, SD = 1.61), 67% are severe illness (mean = 43.24, SD= 20.20), 69% are severe dyspnea (min-max = 70–100, mean = 95.0, SD = 9.10), 57% are started EN within 6 h (min-max = 1–24 h, mean = 7.40, SD = 5.40), 89% have daily calories target requirement within 24–48 h of admission in ICU (min-max= 14–72 h, mean = 31.15, SD = 7.20) and 86% have mechanical ventilation duration days, most participants have mechanical ventilation 5 to 20 days (min-max= 1–40 days, mean = 7.70, SD= 5.80) (Table 1).
 |
Table 1 Demographic Characteristics of the Participants |
The Relationship Between Nutritional Factors and the Duration of a Mechanical Ventilator
This single-center study investigates the association between nutritional status and mechanical ventilation duration (MV) among critical patients. It found that nutrition status, time to initial enteral nutrition (EN), and calories target requirements are positively moderate statistic significance associated with MV duration (R = 0.54, R = 0.30, R= 0.40, p < 0.05) (Table 2). From variables, the greatest predictor to influence MV duration is nutrition status or malnutrition scores. Therefore, this study highlights the importance of nutrition support for critical patients and also provides the association between nutritional status and MV duration (Figure 2).
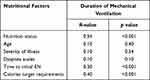 |
Table 2 Associated Factors Between the Nutrition Factors and the Length of Mechanical Ventilation |
 |
Figure 2 Association between mechanical ventilation and nutritional status. |
Nutritional Factors Influencing Mechanical Ventilator Duration
This study found that nutrition status and calories target requirements can be defined by mechanical ventilator duration (p<0.01). Therefore, the result using statistical significance with risk of malnutrition is the best predictor in terms of having impact on duration of a mechanical ventilator for critical patients. The second best predictor is calories target requirement. Additionally, when considering the standard coefficient (Beta), nutrition status has the greatest predictive power and the second is calories target requirements (Beta = 0.58, 0.26 respectively) (Table 3).
 |
Table 3 The Result of Sequential Multiple Regression for Predicting the Length of Mechanical Ventilation |
Discussion
This research studied predictability of nutrition factors on mechanical ventilation duration with objectives discussed below.
The results, nutrition status, time to initial enteral nutrition (EN), and calories target requirements are positively correlated factor, nutrition status is the best predictor on mechanical ventilator duration for critical patients (r = 0.283, p < 0.001). Most critical patients have moderate risk of malnutrition of 52% (mean= 7.81, SD = 1.61). It can be explained that patients have a high risk of malnutrition with statistically significant effect on mechanical ventilation duration (Beta = 0.54, p < 0.001). The study states that most critical patients are invasive ventilator to eat orally, and they have previous malnutrition before admitted to the hospital. The study also shows a significant association between nutrition status, time to initial EN, and calories target requirements on mechanical ventilation duration. High risk malnutrition and calories target requirements can be defined by mechanical ventilation duration. As a result of this study, patients with high risk malnutrition may require longer duration, about 50.34 days for mechanical ventilation. However, if adequate calories target requirement is quicker than 1 hour, it can decrease mechanical ventilation duration used by 8 days. This study delivers initial EN within 6 hours and average daily amounts of full energy enteral nutrition within 7 days following the recommended ASPEN guidelines. In addition, malnutrition is an indirect factor effecting on mechanical ventilation duration. If the critical patients have been promoted nutritional support within 24–48 hours, it could improve to recover main organ function and reduce inflammation process from producing hypermetabolism and hypercatabolic.17 This study confirms that patients started EN within 24–48 hours can reduce mechanical ventilation duration.
Moreover, most patients received calories target in this study may relate to the fact that adequate energy could reduce mechanical ventilation duration.18–20 This study shows that starting EN as soon as possible or within 24–48 hours after hospitalization or resuscitation and promoting adequate energy may affect mechanical ventilation duration. The reasons are to promote intestinal absorption, to prevent intestinal atrophy, as well as to increase blood circulation in gastrointestinal tract and to reduce incidence of organ failure and immune system.6–10 When body has critical illness then begins to adapt flowing phase, it increases hypermetabolic rate such as lipids and proteins which dissolved into energy. Losing of muscle mass directly affects diaphragm muscle causing muscle weakness, especially chest wall muscles which has a direct impact on breathing and difficult to wean off mechanical ventilation.18–21 Therefore, time to initial EN should begin as soon as possible or within 48 hours to recover immune systems (immunosuppressive-inflammatory response), produce proteins, restore organs to work normally,2–4 provide daily calories target or adequate energy requirements. These factors are important for critical patients using mechanical ventilation as they need more energy and protein. Critical patients have higher metabolic process to respond in crisis stages despite consuming energy about 25–35 kcal/kg per day6 and 1.2–1.5 g/kg/BW/day protein.3 Critical patients should receive adequate energy according to their targets within 5 days.22–26 Those who receive targeted energy within 3 days have better clinical outcome as it reduces the duration of a ventilator (p < 0.05).
This study shows nutrition status and calories target requirements to define mechanical ventilation duration. Therefore, assessed nutrition status of critical patients within 24 hours of admission in ICU to evaluate malnutrition risk and to monitor every 7 days is important to integrate nutrition support strategy for patients.27 Moreover, the study also states that daily calories target requirement is significantly associated with mechanical ventilation duration and predictor. Critical patients with mechanical ventilation >72 hours may need 1000 kcal per day or 30-gram protein/day or 1.2–1.5 gram/kg/BW/day or 25-kc/kg/day to decrease mechanical ventilation duration and mortality.28–30 Likewise, Koontalay et al30 reported critical patients with early EN can accrue significantly decreased mechanical ventilation duration in comparison with those who receive standard care. Khalid et al31 also stated that beneficial effect of early EN is associated with a decreased duration of mechanical ventilation and hospital mortality. Additionally, Stewart et al2 suggested that EN can support intestinal structure and function, prevent improved permeability, and bacteria translocation, and also utilize consequent systemic inflammation with gut obstructed. Early EN is widely accepted to decrease infection, complications, hospitalization, and mortality.4
Therefore, physiologically critical patients have been altered as a result of hormonal system and immune system changes, which are a dynamic response to illness crisis by changing metabolic stages rapidly.3–6 It occurs in a crisis stage when the body has energy process breakdown. In order to maintain condition, the body demands more energy and oxygen to increase muscle mass. This directly affects the diaphragm muscle used to breathe. As a result, if the body does not receive proper nutrition care, it probably causes malnutrition and extends mechanical ventilator duration.6 Malnutrition screening for critical patients using ventilators is a key to relieving nutrition process in each patient. It also used to calculate how much energy the patient should receive appropriately. Higgins et al,18 found that nutrition assessment affects ventilator duration, and it should be evaluated within the first 24 hours admitted to a critical care ward by following-up with malnutrition every 7 days. Finally, age, illness severity, dyspnea scales, and time to initial EN cannot be used as a main predictor as nutrition factors. To predict mechanical ventilation duration in critical patients is associated with other several factors such as residual gastric volume, interrupted feeding, and feeding formulas.28
There are several limitations found in the study. First, the research is conducted in a medical surgical critical care unit in a Tertiary Hospital in Thailand; thus, the results might not be generalizable to other settings. Second, the sample size is 100 critical patients, therefore these results might not be applied to other patient groups. Additionally, the factors used to predict selection are not extensive and lack of outcome assessment such as patient morbidity or mortality. However, further research should study on other nutrition factors that may affect critical patients and extend ventilators, for example, feeding obstacles in long term nutrition care, implementing enteral nutrition protocol to achieve energy and protein requirements to reduce ventilator duration.
Conclusion
Our findings show that nutrition status, time to initial EN and calories target requirements are statistically significantly associated with mechanical ventilation duration. The results also state that the assessment of nutrition status is an important procedure for critical patients. Patients who receive enteral nutrition (EN) should have daily calories target requirement monitoring every 7 days in order to provide a nutrition support strategy to reduce mechanical ventilation duration in intensive care units (ICU). Nutrition support with guidelines can reduce mechanical ventilation duration for critical patients by providing appropriate nutritional care support assessment of nutritional status and proportion of enteral nutrition. It should be performed at the start of EN after deriving stable hemodynamic or as soon as possible.
Abbreviations
ICU, intensive care unit; DCRS, daily calories target requirement scale, SGA, subjective global assessment form; EN, enteral nutrition; DSAF, disease severity assessment form; NSS, nutritional status scale; LPM, liter per minutes; NPO, nothing per oral.
Data Sharing Statement
There are no additional data used to support the findings of this study can be made available from the corresponding author upon request. All the data other than which are mentioned in the article already. The obtained data and materials were used only for the present study and are available only to the researchers who participated in the study project.
Acknowledgment
The author (s) acknowledge the ICU staff for their support during this study and the patients and families for their collaboration.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding
This research received no external funding.
Disclosure
The authors declare no conflicts of interest for this work, nor with respect to the research, authorship, and/or publication of this article.
References
1. Mueller C, Compher C, Ellen DM, Parenteral ASf, Directors ENBo. ASPEN clinical guidelines: nutrition screening, assessment, and intervention in adults. J Parenteral Enteral Nutri. 2011;35(1):16–24. doi:10.1177/0148607110389335
2. Stewart ML. Interruptions in enteral nutrition delivery in critically ill patients and recommendations for clinical practice. Crit Care Nurse. 2014;34(4):14–22. doi:10.4037/ccn2014243
3. Doig GS, Heighes PT, Simpson F, Sweetman EA. Early enteral nutrition reduces mortality in trauma patients requiring intensive care: a meta-analysis of randomised controlled trials. Injury. 2011;42(1):50–56. doi:10.1016/j.injury.2010.06.008
4. Elamin EM, Camporesi E. Evidence-based nutritional support in the intensive care unit. Int Anesthesiol Clin. 2009;47(1). https://journals.lww.com/anesthesiaclinics/Fulltext/2009/04710/Evidence_based_Nutritional_Support_in_the.10.aspx.
5. Honda CKY, Freitas FGR, Stanich P, et al. Nurse to bed ratio and nutrition support in critically ill patients. Am J Crit Care. 2013;22(6):e71–e78. doi:10.4037/ajcc2013610
6. O’Leary-Kelley C, Bawel-Brinkley K. Nutrition support protocols: enhancing delivery of enteral nutrition. Crit Care Nurse. 2017;37(2):e15–e23. doi:10.4037/ccn2017650
7. Puthucheary ZA, Rawal J, McPhail M, et al. Acute skeletal muscle wasting in critical illness. JAMA. 2013;310(15):1591–1600. doi:10.1001/jama.2013.278481
8. VanBlarcom A, McCoy MA. New nutrition guidelines: promoting enteral nutrition via a nutrition bundle. Crit Care Nurse. 2018;38(3):46–52. doi:10.4037/ccn2018617
9. Klaude M, Mori M, Tjäder I, Gustafsson T, Wernerman J, Rooyackers O. Protein metabolism and gene expression in skeletal muscle of critically ill patients with sepsis. Clin Sci. 2011;122(3):133–142. doi:10.1042/cs20110233
10. Sungur G, Sahin H, Tasci S. The effects of implementing a nutritional support algorithm in critically ill medical patients. J Pak Med Assoc. 2015;65(8):810–814.
11. Santos H, Araújo I. Impact of protein intake and nutritional status on the clinical outcome of critically ill patients. Revista Brasileira De Terapia Intensiva. 2019;31(2):210–216. doi:10.5935/0103-507X.20190035
12. Sharada M, Vadivelan M. Nutrition in critically ill patients. J Ind Acad Clin Med. 2014;15(3&4):205–209.
13. Kahraman BB, Ozdemir L. The impact of abdominal massage administered to intubated and enterally fed patients on the development of ventilator-associated pneumonia: a randomized controlled study. Int J Nurs Stud. 2015;52(2):519–524. doi:10.1016/j.ijnurstu.2014.11.001
14. Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13(10):818–829.
15. Gift AG. Validation of a vertical visual analogue scale as a measure of clinical dyspnea. Rehabil Nurs. 1989;14(6):323–325. doi:10.1002/j.2048-7940.1989.tb01129.x
16. Detsky AS, McLaughlin JR, Baker JP, et al. What is subjective global assessment of nutritional status? J Parenteral Enteral Nutri. 1987;11(1):8–13. doi:10.1177/014860718701100108
17. Faul F, Erdfelder E, Buchner A, Lang A-G. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods. 2009;41(4):1149–1160. doi:10.3758/BRM.41.4.1149
18. Higgins PA, Daly BJ, Lipson AR, Guo S-E. Assessing nutritional status in chronically critically ill adult patients. Am J Crit Care. 2006;15(2):166–176. doi:10.4037/ajcc2006.15.2.166
19. Moisey LL, Mourtzakis M, Cotton BA, et al. Skeletal muscle predicts ventilator-free days, ICU-free days, and mortality in elderly ICU patients. Crit Care. 2013;17(5):R206. doi:10.1186/cc12901
20. McKendry J, Thomas ACQ, Phillips SM. Muscle mass loss in the older critically ill population: potential therapeutic strategies. Nutri Clin Pract. 2020;35(4):607–616. doi:10.1002/ncp.10540
21. Kim S-H, Park C-M, Seo J-M, et al. The impact of implementation of an enteral feeding protocol on the improvement of enteral nutrition in critically ill adults. Asia Pac J Clin Nutr. 2017;26(1):27. doi:10.6133/apjcn.122015.01
22. Reignier J, Mercier E, Le Gouge A, et al. Effect of not monitoring residual gastric volume on risk of ventilator-associated pneumonia in adults receiving mechanical ventilation and early enteral feeding: a randomized controlled trial. JAMA. 2013;309(3):249–256. doi:10.1001/jama.2012.196377
23. McClave SA, Taylor BE, Martindale RG, et al. Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient: society of critical care medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.). JPEN J Parenter Enteral Nutr. 2016;40(2):159–211. doi:10.1177/0148607115621863
24. Rice TW, Mogan S, Hays MA, Bernard GR, Jensen GL, Wheeler AP. Randomized trial of initial trophic versus full-energy enteral nutrition in mechanically ventilated patients with acute respiratory failure. Crit Care Med. 2011;39(5):967–974. doi:10.1097/CCM.0b013e31820a905a
25. Shen Y, Cheng X, Ying M, Zhang W, Jiang X, Du K. Early low-energy versus high-energy enteral nutrition support in patients with traumatic intracerebral haemorrhage: protocol for a randomised controlled trial. BMJ Open. 2017;7(11):e019199. doi:10.1136/bmjopen-2017-019199
26. Li Q, Zhang Z, Xie B, et al. Effectiveness of enteral feeding protocol on clinical outcomes in critically ill patients: a before and after study. PLoS One. 2017;12(8):e0182393. doi:10.1371/journal.pone.0182393
27. Padar M, Uusvel G, Starkopf L, Starkopf J, Reintam Blaser A. Implementation of enteral feeding protocol in an intensive care unit: before-and-after study. World J Crit Care Med. 2017;6(1):56–64. doi:10.5492/wjccm.v6.i1.56
28. Weijs PJM, Stapel SN, de Groot SDW, et al. Optimal protein and energy nutrition decreases mortality in mechanically ventilated, critically ill patients. J Parenteral Enteral Nutri. 2012;36(1):60–68. doi:10.1177/0148607111415109
29. Perman MI, Ciapponi A, Franco JV, et al. Prescribed hypocaloric nutrition support for critically‐ill adults. Cochrane Database Syst Rev. 2018;6. doi:10.1002/14651858.CD007867.pub2
30. Koontalay A, Sangsaikaew A, Khamrassame A. Effect of a clinical nursing practice guideline of enteral nutrition care on the duration of mechanical ventilator for critically ill patients. Asian Nurs Res. 2020;14(1):17–23. doi:10.1016/j.anr.2019.12.001
31. Khalid I, Doshi P, DiGiovine B. Early enteral nutrition and outcomes of critically ill patients treated with vasopressors and mechanical ventilation. Am J Crit Care. 2010;19(3):261–268. doi:10.4037/ajcc2010197
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
