Back to Journals » Clinical Ophthalmology » Volume 17
Optic Nerve Avulsion: Pattern and Etiologies at a Tertiary Eye Care Center in Saudi Arabia: An 8-Year Retrospective Study
Authors Al Amry M, AlHijji L, Elkhamary SM, Mousa A , AlGaeed A, AlGhadeer H
Received 18 June 2023
Accepted for publication 29 August 2023
Published 6 September 2023 Volume 2023:17 Pages 2633—2641
DOI https://doi.org/10.2147/OPTH.S426493
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Mohammad Al Amry,1 Lamia AlHijji,2 Sahar M Elkhamary,3 Ahmed Mousa,4 Abdulrahman AlGaeed,3 Huda AlGhadeer1
1Emergency Department, King Khaled Eye Specialist Hospital, Riyadh, Saudi Arabia; 2Ophthalmology Department, King Khaled Eye Specialist Hospital, Riyadh, Saudi Arabia; 3Radiology Department, King Khaled Eye Specialist Hospital, Riyadh, Saudi Arabia; 4Research Department, King Khaled Eye Specialist Hospital, Riyadh, Saudi Arabia
Correspondence: Huda AlGhadeer, Emergency Department, King Khaled Eye Specialist Hospital, PO Box 7191, Riyadh, 11462, Saudi Arabia, Tel +966 1 4821234 extension 2500, Email [email protected]
Purpose: Optic nerve avulsion (ONA) is a rare but serious presentation of ocular trauma. This study investigates the presenting characteristics and etiologies of all cases of ONA over an 8-year-period at a tertiary eye care center in the Middle East.
Methods: The medical records of patients diagnosed with ONA at an Ophthalmic Emergency Department between November 2014 and November 2022 were analyzed in this retrospective cohort study. Data were collected on patient age, sex, affected eye, cause of injury and imaging studies. The best-corrected visual acuity (BCVA) at presentation and at the last follow-up visit, and the duration of follow-up were documented.
Results: The study sample was comprised of 44 eyes of 43 patients with ONA with median age of 16.5 (9.3– 26.8) years ranging from 2 years old to 70 years old. There were (35;79.5%) males and (9; 20.5%) females. Most cases presented with an affected left eye (27; 61.4%) followed by the right eye (16; 36.4%) and only one patient (2.3%) had bilateral ONA. The most common cause of trauma resulting in ONA was a metallic object (8;18.2%). This study demonstrates the value of multi-sequence Magnetic resonance imaging (MRI) in the setting of unexplained vision loss when other modalities are inadequate or inconclusive.
Conclusion: Ophthalmic morbidity resulting from ONA can be devastating. Metallic object injuries were the most prevalent cause of ONA. The presence of associated media opacities challenges the initial diagnosis of ONA. In the vast majority of cases, the vision ended as no light perception (NLP), indicating permanent vision impairment.
Keywords: avulsion, ocular, optic nerve, trauma
Introduction
ONA is the traumatic separation of the optic nerve fibers at the level of the lamina cribrosa with preservation of the nerve sheath and surrounding sclera.1 It is a rare but visually devastating form of anterior traumatic optic neuropathy.2 The word “avulsion” comes from the Latin verb “vellere”, which means “to pluck”, and the prefix a, which means “out”. It has been used alternatively with the phrase “evulsion”, which means “to pluck out”.3,4 ONA can be either partial (only the optic nerve is torn) or complete (both the extraocular muscles and the optic nerve are torn, causing total luxation of the ocular bulb).4–7 In cases of complete ONA, the optic sheath, which is more elastic than the optic nerve, usually remains attached to the globe, and the optic nerve may appear normal.8 A complete avulsion causes profound vision impairment, whereas a partial (incomplete) avulsion might result in varying degrees of impairment.9 Various hypotheses of ONA have been proposed, including severe forced rotation of the globe, which avulses the optic nerve from a weakened scleral region, and a sudden elevation in intraocular pressure induced by compression of the globe or by abrupt forward propulsion of the globe as a result of increased intraorbital pressure, producing rupture at the weaker lamina cribrosa.8,10,11 There are several potential causes of ONA including blunt trauma, road traffic accident (RTA), or autoenucleation in psychiatric patients.12–14 ONA has been observed from sports injuries in children, falls, and door handle trauma.13 Breazzano et al15 described ONA in 110 children due to child abuse or (abusive head trauma). ONA has been reported after a finger poke to the globe16 and after an animal kick.17 The prognosis for these injuries is often poor, and they may be debilitating. Many individuals with ONA are referred to our facility for treatment or follow-up. This study presents our experience with ONA patients at a Saudi Arabian tertiary eye care hospital. To the best of our knowledge data on the presenting features of ONA in Saudi Arabia is sparse. In this study, we discuss the pattern and etiologies of ONA patients presenting to a tertiary eye hospital in central Saudi Arabia over the course of 8 years.
Methods
The medical records of patients who reported ocular injuries to the Ophthalmic Emergency Department between November 2014 and November 2022 were analyzed. The Hospital Institutional Review Board of the King Khaled Eye Specialist Hospital approved this study. All participants gave their written informed consent to participate in this study. For participants below 16 years of age, Informed consent to participate was obtained from their parents/legal guardians. Exclusion criteria were presentations that were, not due to an eye injury, resulted from an intentional injury, or were treated elsewhere. Data were collected on patient age, sex, affected eye and cause of injury. BCVA at presentation, at the last follow-up visit, and the duration of follow-up were recorded from the medical records. All of the patients underwent a comprehensive eye examination including measurement of distance BCVA at 6 meters using a Snellen chart. Finger counting, hand motion, and light perception from all cardinal directions were tested if the biggest optotype could not be read. In cases of closed globe injury, intraocular pressure was measured using a Tonopen (Medtronic plc., Minneapolis, MN, USA). Pupillary reflexes were assessed with a well-focused torchlight. A slit lamp biomicroscope was used to evaluate the anterior segment (Topcon Corp., Tokyo, Japan). For uncooperative children, ophthalmic loupes with a light source (Keeler Ltd., Windsor, USA) were used. Indirect ophthalmoscopy (Heine Optotechnik, Ammersee, Bavaria, Germany) was used to examine the posterior segment. B-scan ultrasonography was conducted when necessary and when posterior segment inspection is impossible. Computed tomography (CT) studies were requested to check for intraocular foreign bodies, orbital injuries, and possible bone fractures. MRI was ordered if the optic nerve head region was difficult to visualize due to opaque media, extensive vitreous hemorrhage, subretinal hemorrhage, or if CT was inconclusive. Imaging is critical in the treatment of ONA caused by foreign bodies. MRI is not recommended as first-line imaging after trauma and is not recommended for evaluating intra-orbital metallic foreign bodies since they may cause additional tissue damage.
CT is regarded as the imaging technique of choice for determining foreign body location and topographic relationships with adjacent structures (e.g. eyeball and optic nerve) using 3-dimensional CT images. In the majority of cases, the metallic foreign body is in or near orbit but away from the globe.
ONA was diagnosed when the patient had decreased vision and a relative afferent pupillary defect. Patients have a history of trauma and complain of or are found to have significant visual loss, decreased color vision, visual field deficit, afferent pupillary defect. Dilated fundus exam is often unremarkable initially. Other possible diagnoses (optic neuritis, ischemic optic neuropathies, optic nerve inflammations, optic nerve infections, hereditary optic neuropathies, optic nerve tumors, and compressive optic neuropathy; retinal causes, e.g. ischemic retinal disease, intraocular tumors, and retinal infections) were ruled out.
Since the institution where this study was carried out is a specialist ophthalmology facility, all patients with significant non-ophthalmic injuries were treated at general hospitals.
Statistical Analysis
Data were collected in Microsoft Excel 365 (Microsoft Corporation, Redmond, WA, USA). Excel was used to check data and for coding purposes. SPSS version 26 (IBM Inc., Armonk, NY, USA) was used for statistical analysis. Continuous variables are reported as the median and interquartile range while categorical data are reported as frequencies and percentages. Inferential analysis was conducted using Chi2 to detect the change in vision at presentation and at the post-intervention assessments. The confidence level was set to 95%, and a P value less than 0.05 is considered statistically significant.
Results
A total of 44 eyes of 43 patients were recruited for the current study. The median age of the study sample was 16.5 (9.3–26.8) years, ranging from 2 to 70 years old. The study sample was comprised of (35; 79.5%) males and (9; 20.5%) females. Most of the cases presented with an affected left eye (27; 61.4%) followed by (16; 36.4%) right eyes. One (2.3%) patient had bilaterally ONA Table 1. The most common causes of trauma resulting in ONA were metallic objects (18.2%), followed by RTA (16%) and door handles (11.4%). Knives were also listed as a major cause (4; 9.1%), whereas fireworks, stones, and wood items were all listed as a source of trauma in the same order (3;6.8%). Table 2 outlines the details of all causes. Disaggregation of visual acuity at presentation revealed significant impairment, with the majority of patients in the NLP (34; 77.3%) category, followed by >20/200 (10; 22.7%). When comparing visual acuity at presentation to the final visual acuity, no statistically significant difference was found, with a slight improvement. Table 3 presents visual acuity at presentation and final visual acuity. In terms of intervention, 77% of eyes had surgery. The majority of interventions (13;38.2%), were primary repairs, followed by retinal detachment repairs (9;26.5%) and orbital wall fracture repairs (4;11.7%). The remaining surgical cases involved the treatment of ocular comorbidity complications. Details of surgical intervention procedures are demonstrated in Table 4.
 |
Table 1 Demographic Data of Patients with Optic Nerve Avulsion (ONA) |
 |
Table 2 Causes of Trauma of Optic Nerve Avulsion (N = 44) |
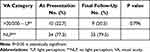 |
Table 3 Visual Acuity of Patients with Optic Nerve Avulsion (ONA) at Presentation and at Final Follow-Up |
 |
Table 4 Surgical Interventions of Patients with Optic Nerve Avulsions (ONA) |
Figure 1. Presents the ultrasound features of ONA; widened pattern of the optic nerve, funnel-shaped vitreous hemorrhage extending from the optic nerve head towards the vitreous. Figure 2. Indicating vitreous hemorrhage, optic nerve avulsion and inferior retinal detachment. Figure 3. CT and MRI studies of the orbit showing traumatic optic nerve avulsion in a 21-year-old male. Axial and coronal T2 fat saturation images revealed a widened optic nerve pattern with loss of the optic nerve sheath around the proximal optic nerve.
Discussion
In the study of ONA patients, we found that the age ranged from 2 to 70 years and the majority (79%) were male. Additionally, we observed that almost all cases were unilateral, and the left eye was more commonly affected. This observation could have occurred as a result of the patients’ recruitment using their dominant eye. Our findings were consistent with the literature that ONA is often unilateral.14 There was one patient with bilateral ONA. A bilateral traumatic globe avulsion was reported in a young woman due to RTA.14 In our study, the most common causes of ONA were metal object injuries (18%) and RTA (16%). Our study reported a high rate of ONA caused by RTA. The majority of patients, especially those involved in RTA, suffer orbital fractures.12,13 In a small number of cases, ONA was caused by falls and stone-related injuries. ONA is associated with globe luxation, which can occur from facial and orbital fractures that compresses the optic nerve following severe trauma. Despite the fact that the lamina cribrosa is the weakest area of attachment of the optic nerve to the globe, optic nerve shearing can occur more than 25 mm behind the globe14,15,18 and at the orbital apex due to the tethering effect of the optic nerve at the attachment of the dura and periosteum of the optic canal.19 Our series’ findings should be viewed from a localization perspective, as the regionally specific cause may produce a completely different pattern than the global or even regional pattern. In isolated ocular trauma, the examination is simple and immediate, but if the patient has sustained a generalized injury, the evaluation of the globe and, consequently, the posterior segment injury will result in delayed examination and difficult prognosis unless the patient receives urgent treatment.1,4–6,20,21
In the majority of cases, the vision ended as (NLP) indicating permanent vision impairment. In our series, even with cases that enrolled in this cohort with relatively better vision, such as >20/200, the improvement was not statistically significant. We observed that the final visual acuity was NLP in approximately 79% percent of the cases. In prior research from the same facility, the presenting visual acuity (VA) of 5 patients was light perception (LP), while 9 patients had NLP. The ultimate VA of LP was maintained in only one patient, while VA in the remaining 13 cases ended as NLP.19
An afferent pupillary defect is vital and the only indicator of vision in many cases; the optic nerve head will initially be normal despite severe and sudden visual loss with a slight visual field defect.
Due to the media opacities, such as vitreous hemorrhage, the initial diagnosis might be difficult.22 Multimodal imaging can be utilized for the diagnosis and evaluation of eye injuries.23 Ultrasound is the initial imaging modality, with classic examinations revealing a dilated, funnel-shaped vitreous hemorrhage extending from the optic nerve head to the vitreous. A wide optic nerve pattern with retrobulbar echolucent areas indicates a retrobulbar hemorrhage. Classic ocular wall thickening surrounding the optic nerve head insertion is also present on ultrasound examination. Echolucent areas indicate hemorrhage in retrobulbar space and are a typical observation with traumatic ONA (partial or total).24
Talwar et al22 reported a defect in the posterior ocular coat surrounding the optic nerve. This echo-free defect spreads irregularly posteriorly along the nerve and the authors22 suggested that these echographic observations coincide with the existence of a partially avulsed nerve with irregular nerve fiber retraction within a dural sheath, which is intact.
In a case of complete avulsion, B-scan ultrasonography indicates a retrodisplacement of the lamina cribrosa and a separation of the optic nerve shadow from the scleral canal, allowing for the early diagnosis of avulsion despite dense vitreous hemorrhage. Singh et al25 observed an anterior “blunting” of the normally acute nerve angle. Ultrasound detected this loss of the normal “V” configuration of the optic nerve shortly after full nerve avulsion.3
Ultrasonography may help in identifying the location of the avulsion of the optic nerve from the sclera and retina by showing the “step sign”, which is a step-like ridge separating the edematous retina from the bare sclera.1 However, the diagnosis of traumatic optic nerve head avulsion is frequently masked by the presence of concomitant vitreous hemorrhage; hence, any investigation leading to an early identification of this entity would be beneficial.
A CT scan is necessary in trauma to diagnose ONA, intra-sheath hemomatoma, optic nerve compression, and concomitant orbital fractures and/or hematomas.12 However, the role of CT for identifying an avulsion may be limited by media opacity, such as vitreous hemorrhage.15 However, CT imaging is vital if intracranial damage is suspected.15 Previous research19,26–28 has demonstrated the utility of MRI in cases of unexplained post-traumatic vision loss when other diagnostic methods are inadequate, impossible, or inconclusive. MRI detection of ONA is uncommon because optic nerve dural sheaths typically remain attached to the globe, making detection difficult. Barnard and Ajlan29 described the significance of MRI in identifying ONA after Ball Bearing (BB) gun trauma. They demonstrated that MRI is essential when there is no obvious cause for visual loss following trauma or when conventional ophthalmic diagnostic techniques, such as B-scan ultrasonography, are unable to detect ONA.
Treatment
The major objective of treatment in ONA is to prevent visual impairment. If the optic nerve is partly severed, it is possible to restore partial visual function.30 Nevertheless, in cases of entirely severed optic nerves devoid of visual function, only cosmetic concerns may become significant, and the therapy of such cases is controversial.31 Options for treatment include observation, steroid administration, and decompression of the optic canal.1,4–6 Observation is the rule with the exception of orbital hematoma, intra-sheath hematoma, and optical canal fracture fragments.12–15 Surgical intervention attempts to decompress the optic nerve sheath. However, according to the International Optic Nerve Trauma Study, only 30% of patients improved from surgery, 52% improved from steroid therapy, and 57% improved with observation.12 Even though surgical intervention was not superior to observation; it was able to preserve vision in cases with orbital and posterior ethmoid hematomas accompanied by hematomas of the optic sheath.20,23
Vaitheeswaran et al23 described a unique method for optic canal decompression employing a transcaruncular route under regional anesthesia. The incision was made into the caruncle, and the dissection extended to the periosteum and orbital apex, where the optic nerve was observed leaving through the optic canal posterior to the posterior ethmoidal artery. The optic nerve was decompressed with adequate visualization. Fibrin glue was used to create hemostasis and wound closure. This patient’s vision improved from hand motion to 20/32 within 6 months of surgery.23
Several reports have documented cases of an avulsed globe that was replaced into the orbit without the need for subsequent enucleation, whereas others required enucleation due to pain, prolonged ocular inflammation, and poor cosmesis. However, no signs of sympathetic ophthalmia were observed in these cases.32
Limitations
This study has several limitations, including its retrospective nature and a small sample size. These cases are referred from our institution to a general hospital with Neurosurgery and Faciomaxillary surgery services and follow-up is nearly impossible. Hence, the patient may have been lost to follow-up as a result. Therefore, long-term outcomes are not readily accessible for these patients.
Conclusion
Optic nerve avulsion is a devastating injury. Injuries caused by metallic objects were the leading cause of ONA. The presence of associated media opacities challenges the initial diagnosis of ONA. In the vast majority of cases, the vision ended as NLP, indicating permanent vision impairment.
Abbreviations
ONA, Optic nerve avulsion; BCVA, Best corrected visual acuity; MRI, Magnetic resonance imaging; NLP, No light perception; RTA, Road traffic accident; CT, Computed tomography; LP, Light perception; VA, Visual Acuity.
Ethical Statement
The study was authorized by the King Khaled Eye Specialist Hospital’s local ethical board and followed the Helsinki Declaration’s tenets. All participants have provided written informed consent to participate in this study.
Patient Consent
Written consent from the patient was obtained for publication of this report.
Acknowledgment
We would like to thank Gharam Al Zahrani, the Clinical Research Optometrist for her contribution to this Research.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This manuscript received no funding.
Disclosure
The researchers declared that they were not involved in any conflicts of interest. No further financial interests in the submitted work have been reported by any of the authors.
References
1. Foster BS, March GA, Lucarelli MJ, et al. Optic nerve avulsion. Arch Ophthalmol. 1997;115(5):623–630. doi:10.1001/archopht.1997.01100150625008
2. Mumcuoglu T, Durukan HA, Erdurman C, et al. Functional and structural analysis of partial optic nerve avulsion due to blunt trauma: case report. Indian J Ophthalmol. 2010;58(6):524–526. doi:10.4103/0301-4738.71705
3. Roberts SP, Schaumberg DA, Thompson PA. Traumatic avulsion of the optic nerve. Optomet Vision Sci. 1992;69(9):721–727. doi:10.1097/00006324-199209000-00010
4. Gupta R, Kent JS, Khan YA. Traumatic complete evulsion of the globe and optic nerve. Can J Ophthalmol. 2014;49(5):e108–e110. doi:10.1016/j.jcjo.2014.06.004
5. Moris WR, Osborn FD, Fleming JC. Traumatic evulsion of the globe. Ophthal Plast Reconstr Sur. 2002;18(4):261–267. doi:10.1097/00002341-200207000-00006
6. Kirath H, Tumer B, Bilgic S. Management of traumatic luxation of the globe. a case report. Act Ophthalmol Scand. 1999;77(3):340–342. doi:10.1034/j.1600-0420.1999.770319.x
7. Chia MA, Shah VH, Turner AW. Partial optic nerve avulsion: a diagnostic challenge. Clin Experiment Ophthalmol. 2020;48(5):701–702. doi:10.1111/ceo.13740
8. Pillai SA, Mahmood MA, Limaye SR. Complete evulsion of the globe and optic nerve. Br J Ophthalmol. 1987;71(1):69–72. doi:10.1136/bjo.71.1.69
9. Babitha V, Prasannakumary C, Ramesan E, et al. Optic nerve avulsion: a rare presentation of blunt trauma. Muller J Med Sci Res. 2017;8(2):97. doi:10.4103/mjmsr.mjmsr_23_17
10. Mahjoub A, Sellem I, Mahjoub A, et al. Optic nerve avulsion: case report. Ann Med Surg. 2021;68:102554. doi:10.1016/j.amsu.2021.102554
11. Patel TP, Archer EL, Trobe JD. Optic nerve avulsion after finger-poke injury. J Neuro Ophthalmol. 2018;38(1):57–59. doi:10.1097/WNO.0000000000000597
12. Reichstein D, Esmaili N, Wells T, et al. Attempted auto-enucleation in two incarcerated young men with psychosis. Saudi J Ophthalmol. 2015;29(2):172–174. doi:10.1016/j.sjopt.2014.09.006
13. Arkin MS, Tubin AD, Bilyk JR, et al. Anterior chiasmal optic nerve avulsion. AJNR. 1996;17(9):1777–1781.
14. Tok L, Tok OY, Argun TC, et al. Bilateral traumatic globe luxation with optic nerve transection. Case Rep Ophthalmol. 2014;5(3):429–434. doi:10.1159/000370043
15. Breazzano MP, Unkrich KH, Barker-Griffith AE. Clinicopathological findings in abusive head trauma: analysis of 110 infant autopsy eyes. Am J Ophthalmol. 2014;158(6):1146–1154. doi:10.1016/j.ajo.2014.08.011
16. Anand S, Harvey R, Sandramouli S. Accidental self-inflicted optic nerve head avulsion. Eye. 2003;17(5):646–647. doi:10.1038/sj.eye.6700449
17. Al-Ghadeer H, Al-Amry M, Elkhamary SM, et al. Isolated traumatic optic nerve avulsion in a boy who suffered a horse kick. Saudi J Ophthalmol. 2020;34(2):134. doi:10.4103/1319-4534.305045
18. Tabatabaei SA, Soleimani M, Alizadeh M, et al. Predictive value of visual evoked potentials, relative afferent pupillary defect and orbital fractures in patients with traumatic optic neuropathy. Clin Ophthalmol. 2011;5:1021–1026. doi:10.2147/OPTH.S21409
19. Chaudry IA, Shamsi FA, Al-Sharif A, et al. Optic nerve avulsion from door-handle trauma in children. Br J Ophthalmol. 2006;90(7):844–846. doi:10.1136/bjo.2005.087544
20. Buchwarld HJ, Spraul CW, Wagner P, et al. Optic nerve evulsion: meta-analysis. Klin Monatsbl Augenheilkd. 2001;218(10):635–644. doi:10.1055/s-2001-18384
21. Simsek T, Simsek E, Ilhan B, et al. Traumatic optic nerve avulsion. J Pediatr Ophthalmol Strabismus. 2006;43:367–369.
22. Talwar D, Kumar A, Verma L, et al. Ultrasonography in optic nerve head avulsion. Acta Ophthalmol. 1991;69(1):121–123. doi:10.1111/j.1755-3768.1991.tb02008.x
23. Vaitheeswaran K, Kaur P, Garg S. Minimal invasive transcaruncular optic canal decompression for traumatic optic neuropathy. Orbit. 2014;33(6):456–458. doi:10.3109/01676830.2014.950282
24. Algaeed AH, Kozak I, editors. Clinical Atlas of Ophthalmic Ultrasound. Springer; 2019.
25. Singh J, Goyal JL, Garg SP. Optic nerve avulsion following tip-cat injury, fluorescein angiographic and echographic features. Afr Asian J Ophthalmol. 1987;6:71–73.
26. Sawhney R, Kochhar S, Gupta R, et al. Traumatic optic nerve avulsion: role of ultrasonography. Eye. 2003;17(5):667–670. doi:10.1038/sj.eye.6700411
27. Kline LB, McCluskey MM, Skalka HW. Imaging techniques in optic nerve evulsion. J Clin Neuroophthalmol. 1988;8(4):281–282.
28. Ohle R, McIsaac SM, Woo MY, et al. Sonography of the optic nerve sheath diameter for detection of raised intracranial pressure compared to computed tomography: a systemic review and meta analysis. J Ultrasound Med. 2015;34(7):1285–1294. doi:10.7863/ultra.34.7.1285
29. Barnard L, Ajlan R. MRI visualization of optic nerve avulsion due to ocular perforation from BB gun projectile. Am J Ophthalmol Case Rep. 2018;11:121–123. doi:10.1016/j.ajoc.2018.06.016
30. Shneck M, Oshry T, Marcus M, et al. Attempted bilateral manual enucleation (gouging) during a physical assault. Ophthalmology. 2003;110(3):575–577. doi:10.1016/S0161-6420(02)01768-2
31. Meena S, Rakheja V, Sahu S, et al. Traumatic avulsion of the globe with optic nerve transection: an unusual presentation. BMJ Case Rep CP. 2020;13(10):e233148. doi:10.1136/bcr-2019-233148
32. Razmjua H, Masjedi M. Traumatic bilateral globe avulsion (case report). J Res Med Sci. 2009;14(4):259–260.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



