Back to Journals » International Journal of General Medicine » Volume 15
Operator’s Influence on Contrast Agent Intravasation During Hysterosalpingo-Contrast Sonography: Explanation Based on a Physics Model
Authors Jin BB , Ma Y, Zhao XH, Teng YL, Zhu SY
Received 8 July 2022
Accepted for publication 26 August 2022
Published 7 October 2022 Volume 2022:15 Pages 7709—7718
DOI https://doi.org/10.2147/IJGM.S380917
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Bin-Bin Jin, Yan Ma, Xiu-Hua Zhao, Yi-Ling Teng, Shang-Yong Zhu
Department of Medical Ultrasound, The First Affiliated Hospital of Guangxi Medical University, Nanning, People’s Republic of China
Correspondence: Shang-Yong Zhu, Department of Medical Ultrasound, The First Affiliated Hospital of Guangxi Medical University, No. 6 Shuangyong Road, Nanning, Guangxi, 530021, People’s Republic of China, Email [email protected]
Objective: To analyze the risk factors of the operators on contrast agent intravasation during hysterosalpingo-contrast sonography (HyCoSy).
Methods: We retrospectively collected 399 infertile women who underwent HyCoSy by the same sonographer. These patients were divided into two groups according to the way how the assistants connected the syringe to the uterus radiography catheter to inject the contrast agent. We analyzed whether the use of different contrast bolus injection methods had any influence on the incidence of intravasation during HyCoSy.
Results: There was no significant difference between the two groups with different cross-sectional areas of the syringe outflow tract in the risk variables for intravasation, but the intravasation rates of the two groups were different, 26.4% in group A and 17.1% in group B, P < 0.05. The primary manifestation was that when both fallopian tubes were unobstructed, the intravasation rate of group B with smaller cross-sectional area of the outflow tract of the syringe was lower, and the difference was statistically significant. The inferences drawn from our physics model were also in line with the clinical results.
Conclusion: The influence of different operators on the contrast agent intravasation rate of HyCoSy cannot be ignored. The assistants of HyCoSy examination should inject the contrast agent slowly and steady, and a needle can be used as a flow restrictor to control the flow into the uterine cavity per unit time, slow down the rising speed of intrauterine pressure, and avoid the accumulation of contrast agent in the uterine cavity, so as to reduce the intravasation caused by operator factors.
Keywords: intravasation, hysterosalpingo-contrast sonography, ultrasonography, contrast agent, fallopian tube patency, infertility
Introduction
At present, hysterosalpingo-contrast sonography (HyCoSy) which is one of the effective methods to check the patency of the fallopian tube, is easily accepted by infertility patients due to its advantages of non-radiation and non-invasiveness.1–3 There were many options of contrast agent used by HyCoSy and sulfur hexafluoride microbubbles were currently recommended.4,5 Sulfur hexafluoride microbubbles were safe contrast agent with few adverse effects,6 but a very disturbing adverse reaction when applied to HyCoSy was intravasation, which occurred in about 13.0%~27.9%.7–9 Namely, sulfur hexafluoride microbubbles injected into the uterine cavity passed through the open small veins of the uterine cavity mucosa and entered the myometrium or pelvic venous plexus.8 If intravasation of the contrast agent occurred during the HyCoSy operation, the ultrasound image would become complicated, which presented as “dendritic” “mesh-like” or “mist-cloudy” with an irregular strong echo and would jeopardize the doctor’s identifying the real fallopian tube even led to misdiagnosis.7,10
Most scholars believed that many risk factors might contribute to contrast agent intravasation in patients, such as the patient’s older age, secondary infertility, thin endometrial thickness, history of intrauterine surgery, history of pelvic surgery, poor bilateral fallopian tube patency, etc.7–9 These studies reported the risk factors from the patient’s perspective and rarely considered the possible influencing factors from the operator’s perspective. Therefore, to bridge this gap in knowledge, we conducted a retrospective study to analyze the operator’s influence on potential intravasation during HyCoSy so as to explore and establish better practices and reduce the incidence of contrast agent intravasation.
Materials and Methods
Clinical Data
In this research, we assessed 399 infertile patients (average age: 31.4 ±4.6 years; age range: 20–45 years) who underwent HyCoSy from September 1, 2019 to March 31, 2021 at the First Affiliated Hospital of the Guangxi Medical University. This research complies with the Declaration of Helsinki and was approved by the Ethics Committee of the First Affiliated Hospital of Guangxi Medical University. All patients were informed of the surgical risks in detail and all of them provided their signed informed consent. The patient inclusion criteria: (1) No vaginal bleeding, acute sexually transmitted diseases, and inflammation of the reproductive system or tumors; (2) Abstinence was required from the first day of menstruation to the moment of HyCoSy; (3) The timing of examination was 3–7 days after the menstrual vaginal bleeding was clean.
Operators
The ultrasound machine was operated by a sonographer with standardized training and >10 years of professional HyCoSy experience. Contrast agent was injected by sonography assistants who had undergone standardized training. A total of 12 assistants, who were all resident physicians, were rotated in the ultrasound department for this task. The rotation time in the ultrasound department ranged from 1 month to 6 months (average 3.8±2.1 months). None of the enrolled assistants had prior work experience with HyCoSy before.
Instruments and Method
The GE Voluson E8/E10 ultrasound system (GE Healthcare, Zipf, Austria) and the RIC 5-9-D probe were used for all inspections. SonoVue (membrane phospholipids filled with sulfur hexafluoride, Bracco, Milan, Italy)—an ultrasound contrast agent—and 5 mL of 0.9% saline solution were injected and shaken to prepare the suspension before use. We routinely disinfected the patient’s vulva and vagina, inserted the 12B uterus radiography catheter (Zhanjiang Star Enterprise Co., Ltd., Guangdong, China) into the uterine cavity, and injected 1.0–2.5 mL of 0.9% saline solution into the balloon to block internal ostium of the uterus. Then, with a 20-mL syringe (Lingyang Medical Instruments Co., Ltd., Zhejiang, China), 18 mL of the 0.9% saline solution and 2 mL of the contrast agent suspension were withdrawn and mixed for later use.
We drew out 18mL of 0.9% saline solution and 2mL of contrast agent suspension and mixed them for later use. Before injection of the contrast agent, routine transvaginal ultrasonography was performed to check the uterine and adnexa for organic diseases. Then we performed a three-dimensional pre-scan according to the conditions of the tubal angiography. When the region of interest (ROI) was within the volume box, the contrast button and the 4D button were activated and the contrast agent was injected simultaneously through the uterus radiography catheter. We observed the flow of contrast agents in the uterine cavity and the fallopian tube and was observed to flow out of the fallopian tube fimbriae. Meanwhile, whether the contrast agent had infiltrated the myometrium and the venous plexus of the pelvis were recorded, and the dynamic contrast data were stored. Then, we started the 3D key to store the static data of the pelvic cavity in order to analyze the dispersion of the contrast agent in the pelvic cavity. Finally, on returning to the 2D state, we observed and analyzed while injecting the contrast agent. Two standardized-trained ultrasound doctors with more than 5 years of professional experience operated the ultrasound machine, analyzed and reconstructed the image, and discussed mutually to reach a unified opinion.
The method of injection of contrast agent in group A was such that the outlet of the syringe barrel was directly connected to the uterus radiography catheter (Figure 1A), while that in group B was such that the syringe barrel was first connected to the needle and then inserted into the uterus radiography catheter (Figure 1B). The inner diameter of the outlet of the syringe was about 2 mm. The needles were the standard 12# needle of the 20-mL syringe used in the HyCoSy operation.
Image Analysis
In this research, three methods, 2D-HyCoSy, 3D-HyCoSy, and 4D-HyCoSy, were applied to evaluate the tubal patency, and all revealed similar diagnostic performance.11 The evaluation of the fallopian tube conditions was performed as follows:3,5,12,13 1. Unobstructed fallopian tube: The fallopian tube could be displayed throughout the entire process, indicating continuous band-like high enhancement. The contrast agent’s continuous and rapid flow could be observed in the lumen. The contrast agent overflew at the umbrella end, its ring enhancement was around the ovary, and the liquid contrast agent was in the Douglas pouch. The pelvic contrast agent was uniformly dispersed. 2. Fallopian tube obstruction: The fallopian tube could not be displayed throughout the processor or only the proximal end of the fallopian tube could be displayed but the distal end could not be or the distal end expanded into a “cystic or beaded” shape. No contrast agent overflew at the umbrella end, and there was no free liquid contrast agent present around the ovarian or pelvic cavity on the side of the fallopian tube blocked.
Evaluation of the intravasation was performed as follows:7–9 1. No contrast agent intravasation: the contour of the uterine cavity was smooth, there was no hyperechoic of contrast agent in the myometrium, and the contrast agent only flew inside the lumen of the fallopian tube, with no contrast agent flowing in the veins on both the sides of the uterus (Figure 2A–C); 2. With contrast agent intravasation: the contrast agent entered the myometrium/pelvic plexus/interstitial space, and the two-dimensional ultrasound image revealed a “spot-like” or “patchy-like” hyperechoic in the myometrium and on both the sides of the pelvic cavity (Figure 2D and E), three-dimensional/four-dimensional ultrasound images demonstrating irregularly shaped “dendrite-like” and “cloud-like” hyperechoic protruding beyond the contours of the uterine cavity, or “string-like” “branches-like” hyperechoic on both the sides of the uterus except for the fallopian tubes (Figure 2F).
Statistics
SPSS 26.0 for Windows statistical software was used to perform statistical analysis on the data. The measured data were expressed as mean ± standard deviation, and using t-test. The enumeration data were expressed as percentage and analyzed by the Chi-square test. P < 0.05 was considered to indicate statistical significance.
Results
Comparison of the Basic Situation of operators Between the Two Groups
All 399 patients in the present study were examined by the same sonographer with standardized training and >10 years of work experience, accompanied by assistants, for HyCoSy examinations. There was a total of 12 assistants (average age: 24.8 ±1.5 years; age range: 23–27 years). All assistants were resident training physicians at the ultrasound department, all held a bachelor’s degree, and none had prior work experience with HyCoSy. Their rotation time in the ultrasound department was an average of 3.2±1.9 months (range: 1–6 months). The assistants were divided into two groups, group A (n=6) and group B (n=6), according to the different connection methods used between the syringe and the uterus radiography catheter. All sonographers and assistants were female. Table 1 shows the comparison of the basic conditions of the two groups of operators. No significant difference was noted in the age of assistants and the average rotation time (P >0.05).
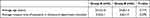 |
Table 1 Comparison of the Basic Situation Between the Two Groups of Assistants |
Comparison of the Basic Conditions and Intravasation Rate of Two Groups of Patients
The 399 patients who received HyCoSy in this study were divided into groups A and B according to the way how the assistants connected the syringe to the uterus radiography catheter. Table 2 compared the risk variables for intravasation between the two groups of patients, and the P-value was all >0.05. There was no significant difference between the two groups in the composition ratios of age, infertility time, endometrial thickness, balloon length, infertility type, gynecological surgical history, and tubal patency. However, the intravasation rate differed between the two groups was different, 26.4% in group A and 17.1% in group B, and the P-value was <0.05.
 |
Table 2 Comparison of the Risk Factors of Intravasation and Contrast Intravasation Rate Between the Two Groups of Patients |
Comparison of the Intravasation Rates Between the Two Groups of Patients with Different Degrees of Tubal Patency
We compared the intravasation rate of patients with different tubal patency situations between the two groups (Table 3), and discovered that the difference was primarily reflected in bilateral fallopian tubes patency patients (P <0.05), with group B having a lower rate of intravasation, while there was no statistically significant difference in the rate of intravasation between the two groups of patients with unilateral patency and bilateral obstruction.
 |
Table 3 Comparisons of Tubal Patency and Intravasation Between the Two Groups (Cases) |
Construction of HyCoSy Physical Model and the Analysis of Fluid Dynamics
Considering the difference on the connection between the syringe and the uterus radiography catheter between groups A and B with the different cross-sectional area of the outflow tract of the syringe, we established a physical model to analyze whether the cross-sectional area of the outflow tract of the syringe had an effect on the intrauterine pressure during HyCoSy (Figure 3).
Suppose F denotes the injection force, S1 the area of the piston of the syringe, v1 the speed of pushing the piston, P1 the pressure at the piston, S2 the cross-sectional area at the outlet of the syringe, v2 the outflow speed of the contrast agent at the outlet of the syringe, P2 the pressure at the outlet, S3 the total cross-sectional area of the unobstructed fallopian tube, v3 the average flow rate of contrast agent in the fallopian tube, P0 the atmospheric pressure, we can obtain the following:
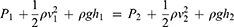
Considering that the contrast agent was close to an ideal fluid, according to Bernoulli’s equation, we obtained the following:
ρ is the density of the contrast agent, h1 the height of the syringe plunger from the horizontal plane, and h2 is the height of the syringe exit from the horizontal plane.
In addition, according to the continuity equation, we could also can obtain the following:
Where, Q denotes the flow of the contrast agent, namely, the volume of the contrast agent flowing into the uterine cavity per unit time.
Since the patients are generally supine during the examination, the height of the syringe, connecting tube, and fallopian tube from the horizontal plane was essentially the same. In other words, the tilt height of the syringe showed little effect on the overall pressure difference, hence the following could be considered:
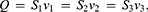
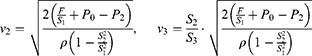
Using the simultaneous equations (1)-(4), one could obtain the following:
According to Poiseuille’s law, the intrauterine pressure ∆P was proportional to the flow Q and the flow resistance Rf, which could be expressed as follows:
Assuming that, for the course of a single injection, the injection force F and flow rate remained constant. According to the volume formula,
Where, t stands for the duration of the injection, and V is the volume of contrast agent injected into the uterine cavity.
In the above equations, S1 and P0 are constants. As a consequence of the preceding equations, if we set the desired outcome as preventing the intrauterine pressure from rising too quickly by slowing down the injection rate in order to develop techniques for improving the injection design we may draw the following inferences:
(1) When the injection force F was constant, and the cross-sectional area of the syringe’s outflow channel was reduced (ie, reduced S2), although P2 increases accordingly, owing to the high order of v2,v2 decrease accordingly when S2 is reduced. Since  , the volume of contrast agent injected into the uterine cavity per unit time Q decreased. On the other hand, for the patients, the total cross-sectional area of the fallopian tube that could be unobstructed S3 and the average flow rate of the contrast agent in the fallopian tube v3 both had an upper limit, which could not be infinite. Therefore, reducing S2 would result in a decrease in Q. According to
, the volume of contrast agent injected into the uterine cavity per unit time Q decreased. On the other hand, for the patients, the total cross-sectional area of the fallopian tube that could be unobstructed S3 and the average flow rate of the contrast agent in the fallopian tube v3 both had an upper limit, which could not be infinite. Therefore, reducing S2 would result in a decrease in Q. According to  , if S3 had reached the upper limit, v3 would correspondingly decrease. As long as the upper limit of the flow rate was not reached, the intrauterine fluid volume would not grow, increasing intrauterine pressure. If it did not reach the upper limit, it meant that the fallopian tube might still possess the ability to extend and would not induce fluid collection in the uterine cavity. It can also be seen
, if S3 had reached the upper limit, v3 would correspondingly decrease. As long as the upper limit of the flow rate was not reached, the intrauterine fluid volume would not grow, increasing intrauterine pressure. If it did not reach the upper limit, it meant that the fallopian tube might still possess the ability to extend and would not induce fluid collection in the uterine cavity. It can also be seen  , that if Q was reduced, the continuous evolution time of the same dose of contrast agent would be prolonged, or less contrast agent may be used in the same evolution time.
, that if Q was reduced, the continuous evolution time of the same dose of contrast agent would be prolonged, or less contrast agent may be used in the same evolution time.
(2) When S2 and S3 are constants, by appropriately reducing the injection force F, v2 would also decrease. The flow of the contrast agent in the fallopian tube Q would not easily exceed its maximum flow at this time, resulting in fluid accumulation and an increase in the intrauterine pressure ∆P.
(3) When the injection force F and cross-sectional area S2 are constant, the total cross-sectional area of the oviduct that could be unobstructed S3 also influenced on the intrauterine pressure. The larger S3 is, the less fluid and pressure are accumulated in the uterine cavity. If both the fallopian tubes are completely blocked, S3=0, the intrauterine pressure increases as the number of intrauterine fluid increases, peaking when the intrauterine fluid reaches the maximum volume of the uterine cavity.
Discussion
Contrast agent intravasation during HyCoSy was caused by a variety of causes. Most scholars believed that it was related to the patency of the fallopian tubes and the pressure in the uterine cavity.7–9 In this research, it could be seen that the intravasation rate was related to the patency of the fallopian tube, the intravasation rate in both groups were that bilateral unobstructed fallopian tube <unilateral unobstructed fallopian tube <bilateral obstructed fallopian tube, which was consistent with the research conclusions of other scholars. The different degrees of patency of the fallopian tubes directly affected the pressure in the uterine cavity. Some researchers used a pressure tester to measure the injection pressure in real-time, and discovered that as the degree of fallopian tube obstruction grew, so did the peak of the contrast medium pressure, ie, pressure in the uterine cavity.14 When the intrauterine pressure rose, the uterine cavity expanded, increasing the strain and permeability of the blood vessels in the basal layer and resulting in contrast agent intravasation. If the contrast agent was injected too quickly, the intrauterine pressure would too quickly, causing the patient’s uterine tubal spasm and discomfort.15,16 Therefore, a slow low-pressure bolus injection of contrast agent could avoid excessive accumulation of the contrast agent in the uterine cavity, which helped reduced reducing the possibility of intravasation.
In this study, no significant difference was noted between the two groups of assistants in terms of age, gender, education, operating experience, and rotation time at the ultrasound department. However, certain differences were noted in the association between the two groups of syringes and uterus radiography catheter. The lower rate of intravasation in group B may be related to the fact that the assistants all used needles as flow restrictors, which reduced the cross-sectional area of the syringe outflow tract.
According to the inferences (1) and (2) of our physical model, it can be seen that the rate of intrauterine pressure rise can be slowed down by many ways, such as reduce the cross-sectional area of the outflow tract of the syringe, reduce the hole diameter at the exit of the uterine radiography catheter, or reduce thrust. These ways can simultaneously reduce the amount of contrast agent injected into the uterus per unit time. In the unobstructed group of both the fallopian tubes, as long as the fluid flow volume was kept lower than the upper limit of the fluid flow rate in both the fallopian tubes, the fluid in the uterine cavity could be adequately drained, and the uterine cavity could maintain a small pressure to avoid development of intravasation.
This operation method reduced the amount of contrast agent flowing into the uterine cavity per unit time Q, according to the formula  , there were two additional and significant advantages: First, under the same injection force, if a needle is used as a baffle, the same dose of contrast agent had a significantly longer injection time than those without a baffle, allowing sonographers to have sufficient observation time to achieve correct diagnosis; Second, within the observation time required for correct diagnosis, doctors could use less contrast agent to complete the diagnosis, which not only reduced costs, but also alleviated some patients’ discomfort like pelvic swelling caused by excessive injection of contrast agent.
, there were two additional and significant advantages: First, under the same injection force, if a needle is used as a baffle, the same dose of contrast agent had a significantly longer injection time than those without a baffle, allowing sonographers to have sufficient observation time to achieve correct diagnosis; Second, within the observation time required for correct diagnosis, doctors could use less contrast agent to complete the diagnosis, which not only reduced costs, but also alleviated some patients’ discomfort like pelvic swelling caused by excessive injection of contrast agent.
According to the inference (2) in our physics model, the thrust of the syringe plunger by the assistant could directly affect the pressure in the uterine cavity, and the pressure in the uterine cavity could rise too quickly, which could induce adverse reactions such as intravasation and pain. Some scholars recommended using a constant pressure automatic injection device,8 but its’ high cost and installation complications put most medical institutions off and the corresponding manual operation was mostly adopted. The manual operation could adjust the injection plan based on real-time patient feedback and was more patient-friendly; nevertheless, maintaining a steady and slow enough injection speed during the related manual operation is challenging. Therefore, sonographers in the training of assistants will emphasize the importance of maintaining a uniform and slow bolus of contrast agent. According to Poiseuille’s law, under a given pressure gradient, the flow resistance of the liquid Rf is inversely proportional to the fourth power of the pipe radius. The outflow tract of group A was the inner diameter of the nipple of a 20-mL syringe with a width of approximately 2 mm, while the outflow tract of group B was the inner diameter of the needle (the inner diameter of the 12# needle was 0.98mm), while the radius of the outflow tract of the syringe of group B was significantly smaller than that of group A. Therefore, the assistants in group B could feel greater flow resistance when injecting contrast agent, which was beneficial to control the initial injection speed and achieve low flow rate injection, thereby maintaining a lower pressure in the uterine cavity. Moreover, the syringe with a needle was easier to connect with the uterine radiography catheter’s tube head via puncture, and it was difficult to slip off the uterus radiography catheter after the connection, which was easier to master by the operating assistants in the group B.
However, there was no significant difference in the rate of intravasation between participants in groups A and B in patients with unilateral tubal patency and obstructed bilateral fallopian tubes, and the results were in line with the third inference of our physical model. Because the fluid injected into the uterus could not be drained, once the volume of the intrauterine fluid reached the maximum volume of the uterine cavity, it was difficult to continue injecting the contrast agent; or because the bolus of contrast agent was decelerated due to the gradual increase in intrauterine pressure, adding a needle as a baffle to slow down the rate of bolus injection could only postpone the peak time. If a patient has unobstructed fallopian tubes on one side, the operator may inject an additional contrast agent into the uterine cavity at a greater pressure to conform unilateral tubal obstruction, which is more difficult to diagnose than bilateral obstruction. As a result, in patients with unilateral tubal obstruction, the greater the pressure and volume of the contrast agent, the more severe the contrast agent intravasation. Another possible explanation is that the volume of fluid injected into the uterus per unit time in the group B was still more than the maximum amount that could be drained from the unilateral fallopian tube. In this study, we did not subdivide the level of tubal “unobstructed but not smooth”, because of a large subjective difference in the diagnosis of “unobstructed but not smooth”. The finer the grouping, smaller was the sample size in each group, which was not conducive to statistical analyses. However, in the unilateral patency group, some patients had one side of the fallopian tube blocked owing to chronic pelvic inflammation and other diseases. Although the remaining fallopian tube was unobstructed, the pelvic condition was affected by inflammatory factors and the patency of the fallopian tube was not good. For example, in 6 patients with unilateral fallopian tube obstruction, the contrast agent clearly flowed out in the form of filaments from the other side of the fallopian tube and the fluid in the uterine cavity could not be quickly drained, which resulted in the accumulation of the contrast agent in the fallopian tube cavity and swelling in the cystic shape. The fallopian tube condition was similar to that of patients with bilateral fallopian tube obstruction, and a high intrauterine pressure caused intravasation.
Group B initially used the connection method of the needle over the syringe because a new assistant found it difficult to connect the latex-made uterus radiography catheter to the syringe nipple, which requires a certain level of strength and skills that was not easy for a novice to master. In such cases, once the connection fails, it can result in the contamination of the contrast agent and related consumables. This particular assistance found that the syringe with a needle was easier to connect to the uterus radiography catheter than the syringe without a needle, and then gradually popularized its usage. Moreover, when the intrauterine pressure was high, the connection between the syringe nipple and the intrauterine fluid passage tube was prone to slip off during the injection of the contrast agent, especially when the catheter’s head was wet. Group A experienced multiple cases of slip off of the joint, but no such case was reported for group B. As the improved operation used a syringe with a needle, there was a problem that required special attention: the needle must be carefully operated when inserting into the uterus radiography catheter to prevent the assistant from being accidentally injured by the needle.
The limitation of this study was that, as a retrospective study, although assistants had undergone standardized training, there were unavoidable individual differences. The assistants who rotated for 1 month and those who rotated for 6 months showed certain differences in the proficiency and strength control of bolus injection, but there were only a few cases of assistants who rotated for only 1 month, and their patients were insufficient to analyze differences in individual skills in a group. We did not make further detailed pain scores for the two groups of patients undergoing examinations, and could not assess whether the two methods of injection of contrast media had any difference in patients’ subjective feelings. Our physical model for analyzing intrauterine pressure was based on an ideal uterus without intravasation. Once the contrast agent intravasate into the parauterine venous plexus, the situation will become complicated and difficult to analyze with simple physical models.
Conclusion
The influence of different operators on the contrast agent intravasation rate during HyCoSy cannot be ignored. Both the data from clinical studies and the physical models confirmed that contrast agent intravasation were related to the rate of intrauterine pressure rise. A needle can be used as a flow restrictor to slow down the rate of intrauterine pressure rise, thereby reducing the intravasation incidence in patients with unobstructed fallopian tubes, which benefits both the doctor and the patient. It is recommended that sonographers share their experience to better guide their assistants to control toward controlling the strength and speed of bolus injection of the contrast agent, as well as to reduce the accumulation of contrast agent in the uterine cavity to avoid potential intravasation.
Acknowledgment
We are very grateful to Dr. De-Bei Pan for his critical contributions from the first manuscript onwards, additions, and suggestions for improvements. And we thank Mr. Chen Huang for drawing the schematic diagram.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Yu J, Cai M, Liang W, et al. Diagnostic efficacy of 3-D hysterosalpingo-contrast sonography in the detection of tubal occlusion: systematic meta-analysis. J Obstet Gynaecol Res. 2015;41(9):1418–1425. doi:10.1111/jog.12728
2. Wang Y, Qian L. Three- or four-dimensional hysterosalpingo contrast sonography for diagnosing tubal patency in infertile females: a systematic review with meta-analysis. Br J Radiol. 2016;89(1063):20151013. doi:10.1259/bjr.20151013
3. Chen S, Du X, Chen Q, et al. Combined real-time three-dimensional hysterosalpingo-contrast sonography with B mode hysterosalpingo-contrast sonography in the evaluation of fallopian tube patency in patients undergoing infertility investigations. Biomed Res Int. 2019;2019:1–7.
4. Committee on Gynecologic Practice American Society for Reproductive Medicine. Infertility workup for the women’s health specialist. Obstet Gynecol. 2019;133(6):e377–e384. doi:10.1097/AOG.0000000000003271
5. Obstetrics and Gynecology Group of Ultrasound Branch of Chinese Medical Doctor Association. Guidelines for clinical application of gynecological contrast ultrasound. Chin J Med Ultrasound. 2015;6:94–98.
6. Hu C, Feng Y, Huang P, et al. Adverse reactions after the use of SonoVue contrast agent: characteristics and nursing care experience. Medicine. 2019;98(44):e17745. doi:10.1097/MD.0000000000017745
7. Wang W, Zhou Q, Zhou X, et al. Influence factors on contrast agent venous intravasation during transvaginal 4-dimensional hysterosal pingo-contrast sonography. J Ultrasound Med. 2018;37(10):2379–2385. doi:10.1002/jum.14594
8. Shi J, Li S, Wu H, et al. The influencing factors of venous intravasation during transvaginal four-dimensional hysterosalpingo-contrast sonography with SonoVue. Ultrasound Med Biol. 2019;45(9):2273–2280. doi:10.1016/j.ultrasmedbio.2019.05.003
9. He Y, Wu H, Xiong R, et al. Intravasation affects the diagnostic image quality of transvaginal 4‐dimensional hysterosalpingo‐contrast sonography with SonoVue. J Ultrasound Med. 2018;38(8):2169–2180. doi:10.1002/jum.14914
10. Liang N, Wu -Q-Q, Li J-H, et al. Causes of misdiagnosis in assessing tubal patency by transvaginal real-time three-dimensional hysterosalpingo-contrast sonography. Revista da Associação Médica Brasileira. 2019;65(8):1055–1060. doi:10.1590/1806-9282.65.8.1055
11. Alázar JL, Martinez A, Duarte M, et al. Two-dimensional hysterosalpingo-contrast-sonography compared to three/four-dimensional hysterosalping o-contrast-sonography for the assessment of tubal occlusion in women with infertility/subfertility: a systematic review with meta-analysis. Hum Fertil. 2020;25:1–13.
12. Lanzani C, Savasi V, Leone FPG, et al. Two-dimensional HyCoSy with contrast tuned imaging technology and a second-generation contrast media for the assessment of tubal patency in an infertility program. Fertil Steril. 2009;92(3):1158–1161. doi:10.1016/j.fertnstert.2008.07.1746
13. He Y, Geng Q, Liu H, et al. First experience using 4-dimensional hysterosalpingo-contrast sonography with SonoVue for assessing f allopian tube patency. J Ultrasound Med. 2013;32(7):1233–1243. doi:10.7863/ultra.32.7.1233
14. Zhou Q, Wang W, Li Y, et al. The value of injection pressure measurement during real-time three-dimensional hysterosalpingo-contrast sonography for assessing fallopian tube patency. Chin J Ultrasonography. 2018;27(03):232–236.
15. Li H, Zhang M, Qiang Y, et al. Pain and side effects associated with 4-dimensional hysterosalpingo-contrast sonography for evaluating of the fallopian tubes patency. Comput Assisted Surg. 2017;22(sup1):93–99. doi:10.1080/24699322.2017.1379229
16. Zhang N, Liu Y, He Y, et al. Transvaginal four-dimensional hysterosalpingo-contrast sonography: pain perception and factors influencing pain severity. J Obstet Gynaecol Res. 2020;47(1):302–310. doi:10.1111/jog.14538
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.