Back to Journals » Therapeutics and Clinical Risk Management » Volume 12
Open-label trial on efficacy of artemether/lumefantrine against the uncomplicated Plasmodium falciparum malaria in Metema district, Northwestern Ethiopia
Authors Wudneh F , Assefa AB, Nega D, Mohammed H , Solomon H, Kebede T, Woyessa A, Assefa Y, Kebede A, Kassa M
Received 26 May 2016
Accepted for publication 24 June 2016
Published 24 August 2016 Volume 2016:12 Pages 1293—1300
DOI https://doi.org/10.2147/TCRM.S113603
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Garry Walsh
Feven Wudneh,1,2 Ashenafi Assefa,3 Desalegn Nega,3 Hussien Mohammed,3 Hiwot Solomon,4 Tadesse Kebede,2 Adugna Woyessa,3 Yibeltal Assefa,3 Amha Kebede,3 Moges Kassa3
1Department of Microbiology, Immunology and Parasitology, School of Medicine, College of Health Sciences, Addis Ababa University, Addis Ababa, 2Biomedical Department, College of Health Sciences and Medicine, Dilla University, Dilla, 3Malaria and Other Parasitological and Entomological Research Team, Bacterial, Parasitic and Zoonotic Diseases Research Directorate, Ethiopian Public Health Institute, 4Malaria Research Team, Disease Prevention and Control Directorate, Federal Ministry of Health, Addis Ababa, Ethiopia
Purpose: Following the increased Plasmodium falciparum resistance to chloroquine and sulfadoxine/pyrimethamine, Ethiopia adopted artemether/lumefantrine (AL) as the first-line treatment for uncomplicated P. falciparum in 2004. According to the recommendation of the World Health Organization, this study was carried out for regular monitoring of the efficacy of AL in treating the uncomplicated P. falciparum malaria in Metema district, Gondar Zone, Northwest Ethiopia.
Patients and methods: This is a one-arm prospective 28-day in vivo therapeutic efficacy study among the uncomplicated P. falciparum malaria patients aged 6 months and older. The study was conducted from October 2014 to January 2015, based on the revised World Health Organization protocol of 2009 for surveillance of antimalarial drug therapeutic efficacy study. Standard six-dose regimen of AL was given twice daily for 3 days, and then the treatment outcomes were assessed on days 0, 1, 2, 3, 7, 14, 21, 28, and any other unscheduled day for emergency cases.
Results: There were 91 study subjects enrolled in this study, of whom 80 study subjects completed the full follow-up schedules and showed adequate clinical and parasitological responses on day 28, with no major adverse event. Per protocol analysis, the unadjusted cure rate of Coartem® was 98.8% (95% confidence interval: 93.3%–100%) in the study area. Recurrence of one P. falciparum case was detected on day 28, with a late parasitological failure rate of 1.2%. No early treatment failure occurred. Complete parasite and fever clearance was observed on day 3. Gametocyte carriage was 4.4% at enrollment that cleared on day 21. Although the difference is statistically not significant, a slight increase in the level of mean hemoglobin from baseline to day 28 was observed.
Conclusion: The study showed high efficacy and tolerability of Coartem® against uncomplicated P. falciparum malaria, suggesting the continuation as a first-line drug in the study district. However, regular monitoring of the therapeutic efficacy of the drug, possibly with plasma drug-level measurement, is critical among the mobile border population.
Keywords: artemether/lumefantrine, cure rate, parasite clearance, fever clearance, uncomplicated malaria
Introduction
The global malaria burden has decreased in recent years with the scale-up of control interventions; however, malaria still remains among the most important communicable diseases in Ethiopia.1,2 Among the total 84.2 million Ethiopian population in 2014, >50 million (60%) live in malaria risk areas, at altitudes <2,000 m above sea level. The Federal Ministry of Health reported in 2011/2012 that malaria was the leading cause of outpatient visits (17% of all outpatient visits) and 8% of health facility admissions among all age groups. Malaria was also one of the top ten causes of inpatient deaths among <5-year-old children and adults based on Health Management Information System data in 2012/2013.2
Early diagnosis and prompt treatment of cases is the most important strategy in the control and prevention of malaria. As a result of Plasmodium falciparum resistance to chloroquine and sulfadoxine/pyrimethamine, Ethiopia shifted the national treatment policy for the first-line treatment of uncomplicated P. falciparum malaria to artemisinin-based combination therapy (ACT), artemether/lumefantrine (AL; Coartem®), in 2004.3,4 Adoption of AL together with the mass distribution of insecticide-treated bed nets and indoor residual spraying has contributed much for the substantial declines in malaria-related deaths in Ethiopia.2,5,6 Currently, AL is working highly effectively, with rapid parasite and fever clearance rates, showing mild adverse effects in almost all areas. Unlike the Greater Mekong Subregion of Southeast Asia where delayed response to ACTs has been reported,7,8 AL has shown cure rates of >95% in adult and pediatric populations with a good safety in sub-Saharan Africa,9,10 including Ethiopia.11–15
As a strategy to handle early the changing malaria trends and the threat of emerging artemisinin resistance by Plasmodium parasite in malaria-endemic countries, particularly in sub-Saharan Africa,16 the World Health Organization (WHO) recommends the routine monitoring of the therapeutic efficacy of the first-line and second-line ACTs every 2 years.17 There could be a change in the national antimalarial treatment policy for a treatment failure >10% in an in vivo open-label trial therapeutic efficacy study (TES). Accordingly, this TES was conducted to assess the efficacy of AL (Coartem®) for the treatment of uncomplicated P. falciparum malaria among the border population of Metema district, Northwestern Ethiopia.
Patients and methods
Study area and period
The study was conducted in Gendewuha Health Center, during the peak malaria transmission season from October 2014 to January 2015. The health center is located in Metema district in Northern Gondar Zone, Amhara Region. The area is lying between latitudes of 12°45′–12°58′ N and longitudes of 36°11′–36°25′ E.18 The area is 925 km northwest of Addis Ababa, Ethiopia’s capital, and 180 km west of Gondar town. The district has an international boundary of >60 km long distance between Ethiopia and Sudan. The mean annual temperature ranges from 22°C to 28°C, and daily temperature reaches as high as 43°C during the months of March–May. The mean annual rainfall ranges from 850 mm to 1,100 mm and has a unimodal pattern. The altitudes range from 550 m to 1,608 m above sea level. Malaria is endemic in the area, with a higher proportion of P. falciparum followed by Plasmodium vivax according to the report of the district in 2014.19
Study design
The study is a one-arm open-label 28-day in vivo trial TES on efficacy of AL among the uncomplicated P. falciparum malaria patients aged 6 months and older. This TES was conducted based on the revised WHO protocol of 2009 for the assessment of antimalarial drug efficacy. The patients were included in the study according to the inclusion criteria set by the WHO in 2009 as described elsewhere.17 Treatment with a standard six-dose regimen of AL was given twice daily for 3 days, and the clinical and parasitological responses were measured on days 1, 2, 3, 7, 14, 21, and 28 and at any unscheduled day when the disease occurred.17
Sample size
The revised WHO protocol of 200917 was used to calculate the required sample size. Sample size calculation assumed 95% cure rate of AL on day 28. With a desired precision of 5% and 95% confidence interval (CI), an initial sample size of 73 was calculated. Assuming an additional 20% for loss to follow-up, at least 88 patients were to be recruited.
Microscopic blood examination
Thick and thin blood smears were prepared on a single slide, respectively, for parasite detection and species identification. Two smears were prepared in each case. The first was stained rapidly with 10% Giemsa for 10–15 minutes for initial screening. The next stained slowly with 3% Giemsa for 45–60 minutes was used to provide standard parasite count and speciation based on the WHO criteria described elsewhere.17 All collected slides were crosschecked by expert microscopists at the Adama Malaria Center, Ethiopia, and the discordant slides were reread by a third senior microscopist at the Ethiopian Public Health Institute (EPHI).
Hemoglobin measurement
Hemoglobin was measured from finger prick blood samples using a portable spectrophotometer (HemoCue, Ängelholm, Sweden) on days 0, 14, and 28.
Statistical analysis
All data were imported into and analyzed by WHO-designed excel spreadsheet and SPSS 20 (IBM Corporation, Armonk, NY, USA) for Windows.
Ethical considerations
The study was ethically cleared and approved by the Scientific and Ethical Review Office of the EPHI and the Ethical Clearance Committee of the Department of Microbiology, Immunology and Parasitology, Addis Ababa University. Written and oral informed consent was obtained from adults and caregivers of children in their local language.
Results
Patient screening and enrolling
Clinically suspected 2,469 febrile cases were screened for malaria, and 42.8% (1,056/2,469) cases were diagnosed to be positive. Out of the positives, 49.8% (526/1,056) were P. falciparum mono-infections, 32.5% (343/1,056) were P. vivax infections, and 17.7% (187/1,056) were mixed infections. Among the 526 P. falciparum mono-infections, 435 were excluded for not fulfilling the inclusion criteria. Of which, 36.8% (160/435) had parasite load <1,000 parasites/μL of blood, 32% (139/435) were out of the catchment area, 12.4% (54/435) had severe and complicated malaria, 10.6% (46/435) were late attendees in the afternoon, 4.6% (20/435) had refused the consent, 2.5% (11/435) were pregnant and breast feeding mothers, and the remaining 1.1% (5/435) had taken antimalaria drugs within 15 days before the start of the study (Figure 1).
  | Figure 1 Recruitment and follow-up in Coartem efficacy study at Gendewuha Health Center, Metema, Ethiopia. |
Based on the inclusion criteria, 91 patients (before noon diagnosed) qualified and participated in the study. However, 11% (10/91) were withdrawn during follow-up, ie, 7.7% (7/91) were lost to follow-up, 2.2% (2/91) had mixed infections enrolled by mistake at screening on day 0, and 1.1% (1/91) were found to have P. vivax infections on day 28. One person was diagnosed to be positive for P. falciparum on day 28 and classified as late parasitological failure (LPF). Thus, 80 study participants successfully completed the 28-day follow-up of Coartem® efficacy monitoring (Figure 1).
Baseline characteristics of the study participants
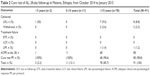
Among the study participants, 17.6% (16/91) were females and 82.4% (75/91) were males. The age group of <5 years consisted of 2.2% (2/91) participants, 5–14 years 12.1% (11/91), and ≥15 years 85.7% (78/91). The mean age was 13 years (range 2–24 years), and the average body weight was 41.5 kg (range 13–70 kg) among all study participants. The baseline mean body temperature, parasite count, and hemoglobin level were 37.9°C, 13,441.6/μL, and 13.7 g/dL, respectively (Table 1).
  | Table 1 The baseline characteristics of the participants in the 28-day Coartem® efficacy study in Metema, Ethiopia, from October 2014 to January 2015 |
From 91 study participants, 65.9% (60/91) had insecticide-treated bed net, whereas 34.1% (31/91) had no bed nets and 84.6% (77/91) had previous malaria attack. Of the net users, 46.7% (28/60) used always, 48.3% (29/60) used sometimes, and the rest 5% (3/60) were not using it.
Cure rate of Coartem®
There were 91 study subjects enrolled in this study, of whom 80 participants completely attended all the follow-up schedules and showed an adequate clinical and parasitological responses to the treatment on day 28. Per protocol analysis showed the polymerase chain reaction (PCR)-unadjusted cure rate of Coartem® as 98.8% (95% CI: 93.3%–100%) in the study area. P. falciparum recurrent case was detected in one individual late on day 28 and classified as LPF, giving the uncorrected total failure rate of 1.2% (1/81; Table 2).
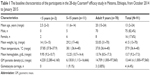
Parasite and fever clearance rate
Parasitemia was cleared from 23.6% (21/89) of patients on day 1, 91% (81/89) of patients on day 2, and 100% on day 3. Forty-six patients had fever (T0≥37.5°C), and the remaining thirty-five patients had a history of fever during study enrollment. Fever was cleared in 69.6% (32/46), 97.8% (45/46), and 100% (1/46) of patients on days 1, 2, and 3, respectively. Gametocyte was detected in 4.4% (4/91) patients at enrollment, with blood density from 16/μL to 5,680/μL. However, two patients finished the follow-up, and the other two were lost during the follow up. One patient cleared gametocyte on day 2 and the other on day 21 (Table 3 and Figure 2).
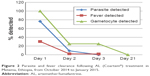  | Figure 2 Parasite and fever clearance following AL (Coartem®) treatment in Metema, Ethiopia, from October 2014 to January 2015. |
Hemoglobin recovery
A slight increase in the mean hemoglobin level was observed from baseline to day 28 among the study participants. The mean hemoglobin level was 13.7 g/dL (range 8.5–17.3 g/dL) and 13.6 g/dL (range 8.8–17 g/dL) at enrollment and on day 14, respectively. After 28 days of follow-up, the level of mean hemoglobin was slightly increased to 13.9 g/dL (range 9.6–17.4 g/dL). However, the mean difference in the level of hemoglobin among days 0, 14, and 28 was statistically not significant (P-value: 0.07; data not shown).
Adverse events following Coartem® treatment
Most of the adverse events observed were similar to common symptoms of malaria, which included headache, fever, joint pain, weakness, anorexia, cough, dizziness, abdominal pain and diarrhea, and mouth ulcer. Most of the side effects observed in the assessment were related to the symptoms of malaria itself, and all disappeared spontaneously following the resolution of parasitemia and fever. The dominant adverse effects observed in this study were headache and joint pain in most patients, followed by dry and unproductive cough in all patients and ulceration of oral area in children (Table 4).
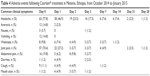  | Table 4 Adverse events following Coartem® treatment in Metema, Ethiopia, from October 2014 to January 2015 |
Discussion
These are preliminary data on the efficacy of AL in the study locality after >9 years of its use as a first-line treatment in the area. This study is part of the national regular TES, for monitoring of the therapeutic efficacy of AL (Coartem®) against the uncomplicated P. falciparum malaria in four eco-epidemiologic sentinel sites of Ethiopia. The primary aim of this study was to assess the therapeutic efficacy of Coartem® for uncomplicated P. falciparum malaria in Metema district, North Gondar Zone, Ethiopia (nearby the country’s border to Sudan). The adequate clinical and parasitological responses observed within the 28 days of follow-up had demonstrated the high efficacy and well tolerability of Coartem® for the treatment of uncomplicated P. falciparum malaria in the study locality.
The overall PCR-uncorrected cure rate per protocol was 98.8% (95% CI: 93.3%–100%). One P. falciparum recurrent case was observed on day 28, which gave the LPF rate of 1.2% among the whole study participants. This finding was consistent with previous findings of efficacy of 96%–100% in different geographies of Ethiopia12,14,15,20–23 and a cure rate of 98.1% in Tanzania.24 In the combination therapy of AL, artemether has a short half-life of ~1 hour. Lumefantrine has a half-life of 3–6 days and clears the long-lasting parasites and thus is expected to avoid the occurrence of recurrent parasitemia.10 Therefore, this study still shows the high efficacy and good safety of AL as already reported in sub-Saharan Africa.9
The current study showed the complete clearance of parasite and fever on day 3. The ACTs have already been demonstrated to be capable of rapid reduction in parasite biomass to result in rapid fever resolution.25 The drug has antipyretic property and is fast acting to clear the different stages of the parasite, which in turn makes fever clearance time short.20 Parasite clearance was rapid on the first 3 days following the treatment, and complete clearance was observed on day 3. Fever was cleared in 69.6% of patients on day 1 and in 97.8% of patients on day 2, and complete clearance was observed on day 3. This fast action of AL was already reported in studies conducted elsewhere in Ethiopia11,12,20 and Tanzania.24 The emerging resistance to artemisinins on the Thailand–Cambodian border26,27 has been characterized by the slow parasite clearance in vivo and the increased day 3 positive cases.9,12,28,29 The day 3 parasitemia on blood smear is a good predictor of the forthcoming failure in Coartem® therapy in the areas of low and moderate transmission.9 Fortunately, the current study showed no day 3 parasitemia; indicating that AL (Coartem®) was highly effective for clearance of parasites in the study area.
In the present study, complete gametocyte clearance was observed on day 21. This is similar to other findings12,30 where complete clearance of gametocyte occurred on day 21. It differs from some of other findings where gametocyte clearance was observed on day 3,15 day 7,20 and day 14.11 Prompt treatment of P. falciparum malaria infections with effective drugs is often associated with low gametocyte carriage and may invariably reduce transmission of gametocytes to mosquitoes.25 It has been reported that the drugs have schizonticidal action to reduce the development of gametocytes. Therefore, AL would not only reduce the problem of resistant malaria but also lessen the chances that an infected person might transmit the infections to mosquitoes and to other members of the community.
The overall incidence of adverse reaction was very low; the tolerability to AL treatment was good in the current study. Most of the adverse reactions observed were related to the symptoms of malaria itself and all disappeared spontaneously following the resolution of parasitemia and fever as reported elsewhere.9 The predominant side effects observed in this study were headache and joint pain, followed by dry and unproductive cough in all participants and ulceration of oral area in children after intake of the medication. This finding was in agreement with other reports in home country.11,15,30 The current finding was also related to the results reported in Uganda,31 where 37% of cough was observed before and 40% after the initiation of treatment.
The study result showed that 30.9%, 32.1%, and 27.2% of participants were anemic, respectively, during inclusion, at day 14, and at day 28. The main reason for the fluctuation in hemoglobin level might be due to the frequent attack of individuals by malaria in the study area.30 A slight increase in the level of hemoglobin was observed on day 28; however, the difference from baseline is statistically not significant. Similar 28-day studies reported that there was a significant recovery in hemoglobin level after medication with AL.11,15,23 The difference in the findings concerning recovery of hemoglobin level might have been due to the associated confounding factors in the study environments, such as helminth infections and feeding habit of the study community.
One of the major limitations concerning this study was inability to measure the level of the drug absorption post treatment. AL absorption is dependent on fatty foods; however, the patients were provided only peanuts when doses were taken in the health center. The first dose during inclusion and the morning doses of days 1 and 2 were taken at direct observation in the health center. The patients were advised to take the rest of night doses in their home, possibly after a fatty meal; however, the night intake was not directly controlled. Another limitation was the inability to genotype the recurrent case to differentiate between recrudescence and reinfection by PCR. Despite the limitations, the study approach is almost close to a real life situation.
Conclusion
This is a preliminary study in Metema district, which showed a high efficacy and good tolerability of AL (Coartem®) in the treatment of uncomplicated P. falciparum malaria, suggesting the safe continuation of the treatment in the locality. However, regular monitoring of efficacy of the drug is considered crucial to handle early the emerging drug resistance among the highly mobile border populations. Furthermore, controlled studies measuring the levels of drugs absorbed and providing the drug intake under direct observation should be conducted for better outcome assessment.
Acknowledgments
EPHI and Addis Ababa University were collaborators of the study in the success of the research. Funding was obtained from the Federal Ministry of Health through the support of the Global Fund. Our heartfelt appreciation goes to the study participants and staff of Metema Health Center and health extension workers for their participation in the study.
Author contributions
MK, AA, and HM conceived and designed the study. FW, DN, HM, and MK collected the data. FW, TK, and AA statistically analyzed and interpreted the data. AW, YA, AK, and HS supervised the general study. DN drafted the article. FW, TK, HS, AA, AW, YA, AK, and MK critically reviewed the manuscript. All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
World Health Organization. World malaria report 2015. Geneva: World Health Organization; 2015. Available from: http://apps.who.int/iris/bitstream/10665/200018/1/9789241565158_eng.pdf. Accessed July 26, 2016. | ||
PMI. Malaria Operational Plan FY. PMI; USA: 2015. | ||
Federal Democratic Republic of Ethiopia, Ministry of Health. Malaria Diagnosis and Treatment Guidelines for Health Workers in Ethiopia. 2nd ed. Addis Ababa: Ministry of Health; 2004. | ||
The Earth Institute at Columbia University. Centre for National Health Development in Ethiopia [webpage on the Internet]. Malaria Treatment. Available from: http://cnhde.ei.columbia.edu/programs/malaria/treatment.html. Accessed on May 22, 2015. | ||
Charles M. Vector Control & Entomology Scoping Report – Ethiopia. Integrated Vector Management (IVM) Task Order 2. Current Status of Entomological Monitoring and Surveillance for an Effective Delivery of Vector Control Interventions in Ethiopia. RTI International; USA: 2006. | ||
PMI. Africa Indoor Residual Spraying Project. Ethiopia PMI Country Profile. PMI; USA: 2015. | ||
World Health Organization. Global Plan for Artemisinin Resistance Containment (GPARC). Global Partnership to Roll Back Malaria. Geneva: World Health Organization; 2011. | ||
WHO. Update on Artemisinin Resistance – January 2014. Geneva: World Health Organization; 2014. | ||
Makanga M, Falade C, Bassat Q, et al. Efficacy and safety of artemether lumefantrine in the treatment of acute uncomplicated Plasmodium falciparum malaria: a pooled analysis. Am J Trop Med Hyg. 2011;85:793–804. | ||
Kibwika P, Lamorde M, Kizza H, Merry C, Colebunders B, Geertruyden J. Update on the efficacy, effectiveness and safety of artemether–lumefantrine combination therapy for treatment of uncomplicated malaria. Ther Clin Risk Manag. 2010;6:11–12. | ||
Assefa A, Kassa M, Tadese G, Mohamed H, Animut A, Mengesha T. Therapeutic efficacy of artemether/lumefantrine (Coartem®) against Plasmodium falciparum in Kersa, South West Ethiopia. Parasit Vectors. 2010;3:1. | ||
Hwang J, Alemayehu B, Hoos D, et al. In vivo efficacy of artemether-lumefantrine against uncomplicated Plasmodium falciparum malaria in Central Ethiopia. Malar J. 2011;10(1):209. | ||
Eshetu T, Abdo N, Bedru KH, et al. Open-label trial with artemether-lumefantrine against uncomplicated Plasmodium falciparum malaria three years after its broad introduction in Jimma Zone, Ethiopia. Malar J. 2012;11:240. | ||
Mekonnen SK, Medhin G, Berhe N, Clouse RM, Aseffa A. Efficacy of artemether-lumefantrine therapy for the treatment of uncomplicated Plasmodium falciparum malaria in Southwestern Ethiopia. Malar J. 2015;14:317. | ||
Nega D, Assefa A, Mohamed H, et al. Therapeutic efficacy of artemether-lumefantrine (Coartem®) in treating uncomplicated P. falciparum malaria in Metehara, Eastern Ethiopia: regulatory clinical study. PLoS One. 2016;11(4):e0154618. | ||
WHO. WHO Guidelines for the Treatment of Malaria. Geneva, Switzerland: WHO; 2006. | ||
WHO. Methods for Surveillance of Antimalarial Drug Efficacy. Geneva: World Health Organization; 2009. | ||
Desalew T, Tegegne A, Nigatu L, Teka W. Rangeland Condition and Feed Resources in Metema District, North Gondar Zone, Amhara Region, Ethiopia. Vol. 4. Addis Ababa: IPMS; 2010:142. | ||
Tolessa M. Contradictions between rhetoric and practice: the case of intraregional resettlement programme in northern Ethiopia. J Sustain Dev Africa. 2012;14(2):1520–5509. | ||
Kinfu G, Gebre-selassie S, Fikrie N. Therapeutic efficacy of artemether-lumefantrine for the treatment of uncomplicated Plasmodium falciparum malaria in Northern Ethiopia. Malar Res Treat. 2012;2012:1–6. | ||
Getnet G, Fola AA, Alemu A, Getie S, Fuehrer HP, Noedl H. Therapeutic efficacy of artemether – lumefantrine for the treatment of uncomplicated Plasmodium falciparum malaria in Enfranze, north-west Ethiopia. Malar J. 2015;14:258. | ||
Ebstie YA, Zeynudin A, Belachew T, Desalegn Z, Suleman S. Assessment of therapeutic efficacy and safety of artemether-lumefantrine (Coartem®) in the treatment of uncomplicated Plasmodium falciparum malaria patients in Bahir Dar district, Northwest Ethiopia: an observational cohort study. Malar J. 2015;14:236. | ||
Kefyalew T, Animut A, Tamene T, Jima D, Hailemariam A, Legesse M. Efficacy of six-dose regimen of artemether-lumefantrine for the treatment of uncomplicated falciparum malaria, three years after its introduction into Ethiopia. Parasite. 2009;16(2):129–134. | ||
Ngasala B, Malmberg M, Carlsson A, Ferreira P, Petzold M, Blessborn D. Efficacy and effectiveness of artemether-lumefantrine after initial and repeated treatment in children <5 years of age with acute uncomplicated Plasmodium falciparum malaria in rural Tanzania: a randomized trial. Clin Infect Dis. 2011;52(7):873–882. | ||
Silamut K, Phu NH, Whitty C, et al. A quantitative analysis of the microvascular sequestration of malaria parasites in the human brain. Medicine National Institutes of Health. Am J Pathol. 1999;155(2):395–410. | ||
Noedl H, Se Y, Schaecher K, et al. Evidence of artemisinin-resistant malaria in western Cambodia. N Engl J Med. 2008;359(24):2629–2620. | ||
Rozendaal J. Fake antimalaria drugs in Cambodia. Lancet. 2001;1357:890. | ||
Worldwide Antimalarial Resistance Network (WWARN) AL Dose Impact Study Group. The effect of dose on the anti-malarial efficacy of artemether–lumefantrine: a systematic review and pooled analysis of individual patient data. Lancet Infect Dis. 2015;15:692–702. | ||
Anderson T, Nair S, Nkhoma S, et al. High heritability of malaria parasite clearance rate indicates a genetic basis for artemisinin resistance in western Cambodia. J Infect Dis. 2010;201(9):1326–1330. | ||
Mulu A, Geresu B, Beyene Y, Ademe M. Efficacy of artemether-lumefantrine for the treatment of uncomplicated Plasmodium falciparum malaria in Northeast Ethiopia. Int J Basic Clin Pharmacol. 2015;4:492–496. | ||
Fogg C, Bajunirwe F, Piola P, et al. Adherence to a six-dose regimen of artemether-lumefantrine for treatment of uncomplicated Plasmodium falciparum malaria In Uganda. Am J Trop Med Hyg. 2004;71:525–530. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.