Back to Journals » Clinical Ophthalmology » Volume 17
One-Year and 18-Month Outcomes in nAMD Patient Eyes Switched to Brolucizumab Alone versus to Brolucizumab Alternating with Other Anti-VEGF Agents
Authors Coney JM , McCoy JE, Buxy Sinha S, Sonbolian N, Zhou L, Hull TP, Lewis SA, Miller DG, Novak MA, Pendergast SD, Pham H, Platt SM, Rao LJ, Schartman JP, Singerman LJ, Donkor R , Fink M, Zubricky R, Karcher H
Received 27 September 2023
Accepted for publication 15 November 2023
Published 23 November 2023 Volume 2023:17 Pages 3601—3611
DOI https://doi.org/10.2147/OPTH.S432957
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Joseph M Coney,1 Jasmyne E McCoy,1 Samriddhi Buxy Sinha,2 Nina Sonbolian,2 Lujia Zhou,3 Thomas P Hull,1 Shawn A Lewis,1 David G Miller,1 Michael A Novak,1 Scott D Pendergast,1 Hang Pham,1 Sean M Platt,1 Llewelyn J Rao,1 Jerome P Schartman,1 Lawrence J Singerman,1 Richard Donkor,1 Margaret Fink,1 Ryan Zubricky,4 Helene Karcher2
1Retina Associates of Cleveland Inc, Beachwood, OH, USA; 2Novartis Pharma AG, Basel, Switzerland; 3KMK Consulting, Morristown, NJ, USA; 4Geisinger Eye Institute, Danville, PA, USA
Correspondence: Joseph M Coney, Retina Associates of Cleveland Inc, 24075 Commerce Park, Beachwood, OH, 44122, USA, Tel +1 (216) 831-5700, Email [email protected]
Objective: Retrospective, real-world study to evaluate visual acuity (VA), anti-vascular endothelial growth factor (anti-VEGF) injection intervals, and central macular thickness (CMT) in neovascular age-related macular degeneration (nAMD) eyes switched to brolucizumab only or to brolucizumab alternating with another anti-VEGF.
Methods: The overall study population comprised eyes that were given ≥ 1 brolucizumab injection between 1 October 2019 and 30 November 2021. The brolucizumab-only (BRO) cohort consisted of prior anti-VEGF-treated eyes treated exclusively with ≥ 3 brolucizumab injections over ≥ 12 or ≥ 18 months; the alternating brolucizumab (ALT) cohort comprised prior anti-VEGF-treated eyes treated with ≥ 2 brolucizumab injections and ≥ 1 other anti-VEGF over ≥ 12 or ≥ 18 months.
Results: A total of 482 eyes received ≥ 1 brolucizumab injection during the study period. Mean VA changes from baseline were − 1.1± 15.1 letters (BRO cohort; n = 174) and 1.3± 13.0 letters (ALT cohort; n = 47) at Month 12, and 0.0± 13.5 letters (BRO cohort; n = 95) and − 7.3± 17.2 letters (ALT cohort; n = 29) at Month 18. Mean changes in injection intervals were +26.9± 48.1 days (BRO cohort) and +11.1± 17.3 days (ALT cohort) at Month 12 and +36.3± 52.3 days (BRO cohort) and +14.0± 19.9 days (ALT cohort) at Month 18. Mean changes in CMT were − 35.2± 108.1 μm (BRO cohort) and − 31.5± 91.2 μm (ALT cohort) at Month 12 and − 38.9± 75.0 μm (BRO cohort) and − 9.0± 59.9 μm (ALT cohort) at Month 18. Intraocular inflammation-related adverse events were recorded in 22/482 (4.6%) eyes.
Conclusion: Treatment with either brolucizumab alone or brolucizumab alternating with another anti-VEGF can preserve vision, reduce CMT, and extend anti-VEGF injection intervals in patients with nAMD.
Keywords: alternating anti-VEGF treatments, brolucizumab, neovascular age-related macular degeneration, wet age-related macular degeneration, 12-month outcomes, 18-month outcomes
Introduction
Neovascular age-related macular degeneration (nAMD), characterized by choroidal neovascularization resulting in the accumulation of retinal fluid, is a leading cause of vision loss in the older population worldwide.1,2 Following pivotal trials with ranibizumab in 20063,4 and aflibercept in 2012,5 intravitreal anti-vascular endothelial growth factor (anti-VEGF) therapies have become the standard of care for the treatment of nAMD and since then, there has been a substantial decrease in the incidence of visual impairment due to nAMD in the US and Europe.3–10
Despite the functional and morphological gains achieved with anti-VEGF therapies, the maintenance of these gains requires frequent re-treatment, thus imposing a burden on both patients and health care systems. The initial studies were performed with anti-VEGF agents administered monthly and although less burdensome treatment regimens, such as pro re nata and treat and extend, have been developed, the maintenance of visual gains requires long-term treatment,11 with a frequency <8 weeks in over half of nAMD patients.12 Delays in administering anti-VEGF agents and treatment avoidance by patient non-compliance increases the risk of avoidable vision loss.13–15 In addition, some patients with nAMD have a sub-optimal response despite frequent injections and may require switching to another anti-VEGF therapy to improve treatment outcomes.16 Therefore, an optimal treatment regimen needs to be identified for patients with nAMD that can improve and stabilize their vision while minimizing treatment burden.
Brolucizumab is a single-chain antibody fragment that, following the pivotal Phase III HAWK and HARRIER studies, was approved by the US Food and Drug Administration (FDA) in 2019 for the treatment of patients with nAMD.9,10 In these clinical trials, brolucizumab provided similar vision gains and superior fluid resolution compared with aflibercept, with more than 50% of brolucizumab-treated patients on a 12-week dosing interval at Week 48, which was maintained to Week 96.9,10 Additionally, real-world studies have reported on the outcomes of anti-VEGF therapies in nAMD, including on nAMD patients who were switched to treatment with brolucizumab.17–25 Following the Phase III MERLIN study, which assessed the efficacy and safety of brolucizumab administered every 4 weeks in eyes with nAMD and persistent retinal fluid, brolucizumab is not indicated for injection intervals <8 weeks beyond the loading phase.26–28 As a consequence, patients on injection intervals <8 weeks who switch to brolucizumab, to further control their fluid and/or to prolong their injection intervals, may therefore opt to alternate brolucizumab with another anti-VEGF to ensure brolucizumab is not injected more frequently than every 8 weeks.
However, to date, no studies have reported on the outcomes of patients switched to brolucizumab that alternate brolucizumab with other anti-VEGF agents. The aim of this study was to evaluate visual acuity (VA), anti-VEGF injection intervals, and central macular thickness (CMT) in real-world nAMD patients switching to brolucizumab from other anti-VEGF agents in patients treated with either brolucizumab alone or with brolucizumab alternating with other anti-VEGF agents.
Methods
Study Design
This was a retrospective, non-interventional cohort study of patients with nAMD carried out at a large retina practice located in Cleveland, OH, USA, between 1 October 2019 and 30 November 2021. Part of the data in this study was analyzed for another, recently published study by the same authors.29 Data collected are stored in the patients’ charts in the practice’s office. The Sterling Institutional Review Board granted a waiver of authorization for this study. Anonymized patient data were extracted on 1 December 2021 and were used to create the different study cohorts. The brolucizumab cohort included all patient eyes who received ≥1 brolucizumab injection during the study period. Two efficacy cohorts were derived from the brolucizumab cohort: the 12-month BRO cohort, which consisted of patient eyes who switched from a previous anti-VEGF and had ≥3 brolucizumab injections with no other anti-VEGF in the first 12 months (360 days) of follow-up and was already analyzed for another, recently published study by the same authors;29 and the 12-month ALT cohort, which consisted of patient eyes who switched from a previous anti-VEGF to brolucizumab and had ≥2 brolucizumab injections and ≥1 injection of another anti-VEGF in the first 12 months of follow-up and was not analyzed before. Eyes with at least 18 months (540 days) of follow-up from the first brolucizumab injection were included in two cohorts. Eyes in the 18-month BRO cohort received no anti-VEGF other than brolucizumab up to Month 18, whereas there were no restrictions on the anti-VEGF agent used after Month 12 in eyes included in the 18-month ALT cohort (Figure 1). Optical coherence tomography (OCT) data initially missing from the electronic charts were manually extracted from OCT machines at the various Retina Associates of Cleveland clinic sites.
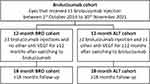 |
Figure 1 Definition of the brolucizumab, BRO and ALT cohorts. Abbreviations: ALT, brolucizumab alternating with another anti-VEGF; BRO, brolucizumab only; VEGF, vascular endothelial growth factor. |
Ethics
This study complied with the tenets of the Declaration of Helsinki. It is based on a medical records database built using medical records from nAMD patients who visited one of the 13 clinic sites and provided consent to have their deidentified data used for research purposes. All patient data was deidentified before being entered in the database and personal data was never shared. This study is based on a retrospective analysis of deidentified data obtained as part of routine clinical practice. As a result, no ethics approval was required.
Study Endpoints
Study endpoints included VA, anti-VEGF injection intervals, and CMT at Month 12 and Month 18, changes in these outcomes from baseline, and safety. Baseline VA and CMT measurements were collected on the day of the first brolucizumab injection, and VA and CMT values at Month 12 and at Month 18, respectively, were defined as the measurements collected closest (±90 days) to the Month 12 and Month 18 injections, respectively. The baseline injection interval was defined as the time between the last pre-switch anti-VEGF injection and the first brolucizumab injection. The injection intervals at Month 12 and Month 18 were defined as the time between the anti-VEGF injection closest to Month 12 or Month 18, respectively, and the corresponding preceding injection. Safety data collected included all intraocular inflammation (IOI) events, retinal vasculitis (RV), retinal vascular occlusion (RO) in the presence or absence of IOI and secondary to brolucizumab use.
Statistical Methods
Changes in injection interval, VA and CMT from baseline to Month 12 or Month 18, respectively, were calculated by subtracting the corresponding baseline measurement from the Month 12 or Month 18 measurements and were reported as mean ± standard deviation (SD) or mean (95% confidence intervals [CI]). Statistical significance was evaluated by paired t-test analysis, and P-values below 0.05 were considered statistically significant. P-values and 95% CIs of the mean differences between respective baseline and Month 12 or Month 18 measurements were reported and displayed in figures using the statistical software R. VA was converted from Snellen numerators, denominators and logMAR values to Early Treatment Diabetic Retinopathy Study (ETDRS) letters as described by Gregori et al.30 Missing value analyses were performed by calculating the percentage of missing values at baseline and at Month 12 and Month 18, respectively.
Results
Study Population
Of the 414 patients, a total of 482 eyes received ≥1 brolucizumab injection during the study period. Coney et al found that the 12-month BRO cohort consisted of 174 eyes from 154 patients.29 This study found the 12-month ALT cohort consisted of 47 eyes from 41 patients. Mean ± SD patient age was 80.5±7.7 years and 77.4±9.2 years; 55.8% and 58.5%; baseline VA: 60.8±17.1 and: 61.4±16.0 ETDRS letters and; baseline CMT: 292.2±113.3 and 288.0±89.6 μm; pre-switch injection interval: 47.8±25.1 days and pre-switch injection interval: 32.0±10.5 days respectively. Mean age and pre-switch injection interval were statistically significant between the 12-month BRO and ALT cohorts. The 18-month BRO and ALT cohorts comprised 95 eyes from 85 patients and 29 eyes from 24 patients, respectively (Table 1).
 |
Table 1 Clinical and Baseline Characteristics of Patients and Eyes in the BRO and ALT Cohorts |
Baseline demographics and clinical characteristics of the brolucizumab cohort (N = 482 eyes from 414 patients) were similar to those of the 12-month BRO cohort. CMT data were missing for 12/174 (6.9%) eyes in the 12-month BRO cohort29 and from 6/95 (6.3%) in the 18-month BRO cohort. In the 12-month BRO cohort, 2/174 (1.1%) eyes were excluded from the quantitative VA analysis as they only had light perception VA. In the 12-month ALT cohort, 2/47 (4.3%) eyes had missing VA measurements.
Effects on Vision by Switching to Brolucizumab
At Month 12, average VA changed relative to baseline by −1.1±15.1 ETDRS letters in the BRO cohort and by 1.3±13.0 ETDRS letters in the ALT cohort. At Month 18, VA changed by 0.0±13.5 ETDRS letters in the BRO cohort and by −7.3±17.2 letters in the ALT cohort (Table 2).
 |
Table 2 Visual Acuity Change from Baseline at Months 12 and 18 |
Characterization of Anti-VEGF Agents
Eyes in the 12- and 18-month BRO cohorts received only brolucizumab injections (Figure 2A and Supplementary Figure S1A, respectively). In contrast, eyes in the 12-month ALT cohort received a mean of 7.1±1.6 injections with brolucizumab and 3.2±2.6 injections with other anti-VEGF agents (82.7% aflibercept, 14.0% bevacizumab, and 3.3% ranibizumab) within 12 months after switching to brolucizumab (Figure 2B). Eyes in the 18-month ALT cohort received a mean of 10.3±1.3 brolucizumab injections and 3.7±2.9 other anti-VEGF agent injections (82.2% aflibercept, 10.3% bevacizumab, and 7.5% ranibizumab) within the first 18 months after switching to brolucizumab (Supplementary Figure S1B).
Effects on Injection Intervals by Switching to Brolucizumab
The mean baseline (ie, pre-switch) injection intervals were longer in the BRO cohort (47.8±25.1 days [=6.8 weeks]) than in the ALT cohort (32.0±10.5 days [=4.6 weeks]). At Month 12, injection intervals were extended by 26.9±48.1 days (=3.8 weeks) in the BRO cohort compared with 11.1±17.3 days (=1.6 weeks) in the ALT cohort (Figure 3A). Similarly, injection intervals were extended by a mean of 36.3±52.3 days (=5.2 weeks) in the 18-month BRO cohort compared with 14.0±19.9 days (=2.0 weeks) in the 18-month ALT cohort (Supplementary Figure S2A).
Effects of Switching to Brolucizumab on CMT
From baseline to Month 12, mean CMT changed by −35.2±108.1 μm in the BRO cohort29 and by −31.5±91.2 μm in the ALT cohort (Figure 3B). At Month 18, CMT reductions were −38.9±75.0 μm in the BRO cohort29 and −9.0±59.9 μm in the ALT cohort (Supplementary Figure S2B).
Safety Outcomes
As described in the recently published study by the same authors,29 22/482 brolucizumab cohort eyes (21 patients) experienced IOI-related AEs. This included 4/482 (0.8%) eyes with concomitant RV. Two of these 4 eyes (2/482; 0.4%) had IOI, RV and RO. Two eyes (2/482 eyes; 0.4%) with IOI with RV experienced ≥15 letters vision loss, one of which had concomitant RO. Neither of the 2 patients with IOI, RV and RO experienced vision loss of ≥30 letters. Inflammation events occurred most commonly with in the first 6 months (82%), less presented between 6 and 12 months (14%) and few between 12 and 18 months (5%).
Discussion
This study of real-world outcomes in nAMD patients switching to either brolucizumab alone, or brolucizumab alternating with another anti-VEGF agent, demonstrates that VA was maintained, CMT was reduced, and injection intervals were extended with both anti-VEGF treatment regimens after 12 and 18 months, respectively. At Month 12, mean injection intervals were extended by 3.8 weeks vs 1.6 weeks in eyes treated with only brolucizumab vs eyes treated with brolucizumab in combination with another anti-VEGF agent, and at Month 18, the injection interval length extensions were 5.2 weeks and 2.0 weeks, respectively.
Although eyes in the BRO and ALT cohorts had similar VA and CMT at baseline, the pre-switch injection intervals were 2.2 weeks shorter in the ALT cohort compared to the BRO cohort, and IRF was more frequent (ALT: 31.9% IRF; BRO: 23.0% IRF), which may suggest that eyes in the ALT cohort had a higher degree of baseline disease activity than eyes in the BRO cohort. It is therefore not surprising that improvements in VA, injection intervals, and CMT were less pronounced in the ALT cohort compared with the BRO cohort. However, even though the injection interval for eyes in the ALT cohort were not able to extend their injection interval as much as eyes in the BRO cohort, this treatment option should not be discounted, as it may allow for additional flexibility for eyes treated with brolucizumab that require short-term reduction in injection intervals due to high nAMD disease activity. It is also possible that some of the ALT cohort eyes may have been treated with a combination of anti-VEGFs because of the brolucizumab urgent safety measure introduced following the results of the MERLIN study in June 2021.28 Due to the higher IOI rates in patients treated with monthly brolucizumab injections in this study, the recommendation was made that brolucizumab should not be administered more frequently than every 8 weeks after the 3 monthly loading doses.26,27 However, this study has demonstrated that alternating treatment between brolucizumab and other anti-VEGF agents when injection intervals shorter than 8 weeks are required allows physicians more flexibility to balance optimal disease activity management and minimization of the anti-VEGF injection burden by resuming brolucizumab injections once the patient no longer requires injections more frequent than every 8 weeks.
To avoid bias in favor of eyes that tolerate ≥3 brolucizumab injections over the 12-month follow-up, adverse events (AEs) were evaluated in a larger brolucizumab cohort that included all eyes treated with at least one brolucizumab injection during the study period (482 eyes). A total of 4.6% of brolucizumab-treated eyes experienced IOI-related AEs, and 82% of these events took place within 6 months after initiating treatment with brolucizumab. These rates are similar to those observed in a post hoc analysis of the Phase 3 HAWK and HARRIER studies of anti-VEGF-treatment-naive eyes with nAMD, where 50/1088 brolucizumab-treated eyes (4.6%) developed IOI, most frequently (74%) within 6 months after the first administration of brolucizumab
Several real-world studies have also evaluated the real-world safety profile of brolucizumab. A small study from Japan reported IOI occurring in 16/68 (22.1%) treatment-naive nAMD eyes within 12 months of brolucizumab-treatment,31 and the large IRIS Registry and Komodo Healthcare Map (n = 10,654 and 11,161 eyes, respectively) reported an IOI rate of 2.4% in real-world patients, the majority of which were brolucizumab switch patients.32
The strength of this study, with 174 eyes treated with brolucizumab alone and 47 with brolucizumab and another anti-VEGF, is that it has one of the largest, real-world, brolucizumab-treated study cohorts with follow-up to 12 months and the only one studying the alternating regimen of brolucizumab and other anti-VEGFs. Other brolucizumab real-world studies include the REBA study of 105 eyes with nAMD and a mean follow-up of 10.4 months18 and a Japanese study of 45 treatment-naive eyes with 1 year of follow-up.31 Data collected in this study found the eyes also have differing lengths of treatment history prior to starting brolucizumab. The extent of missing data was low in this study for all variables allowed for in-depth analyses.
It should be noted that factors include that the data was collected during the 2020 COVID-19 pandemic and that timely patient follow-up visits might have been impacted. A recent publication at this practice has shown this effect was limited to a mean 5% reduction in clinic visits over a 10-week period during the COVID-19 pandemic (16 March to 31 May 2020) compared to a corresponding pre-pandemic 10-week period (1 January to 15 March 2020), and that the negative impact of COVID-19 measures on clinic visits disappeared by the end of the 10-week study period.33 It is therefore unlikely that the COVID-19 pandemic had meaningful impact on the overall results of this 26-month study. Other limitations of this study are linked to its observational nature: eyes were not randomly assigned to the BRO or ALT regimens, meaning that harder-to-treat patients may have been channeled to the ALT cohort. Additionally, a potential limited external validity cannot be excluded since the data were collected from only one private specialty retina clinic. However, despite this limitation, agreement with other real-world studies on the injection interval extension and VA maintenance results in the BRO cohort are striking.18,19,31,34,35
Conculsion
In conclusion, this real-world study of nAMD patients switching to either brolucizumab alone, or to brolucizumab alternating with another anti-VEGF agent, reveals that injection intervals could be extended more than twice as much in eyes treated with brolucizumab alone compared to eyes treated with brolucizumab alternating with another anti-VEGF, which may help reduce the injection burden in nAMD. Our data suggest that both anti-VEGF treatment regimens can preserve vision, reduce CMT, and extend anti-VEGF injection intervals in patients with nAMD, which increases the treatment options for patients with nAMD.
Abbreviations
AE, adverse event; ALT, alternating cohort; BRO, brolucizumab; CI, confidence interval; CMT, central macular thickness; ETDRS, Early Treatment Diabetic Retinopathy Study; IOI, intraocular inflammation; logMAR, logarithm of the minimum angle of resolution; nAMD, neovascular age-related macular degeneration; OCT, optical coherence tomography; RO, retinal vascular occlusion; RV, retinal vasculitis; SD, standard deviation; VA, visual acuity; VEGF, vascular endothelial growth factor.
Data Sharing Statement
Novartis is committed to sharing with qualified external researchers, access to patient-level data and supporting clinical documents from eligible studies. These requests are reviewed and approved by an independent review panel on the basis of scientific merit. All data provided is anonymized to respect the privacy of patients who have participated in the program in line with applicable laws and regulations.
Ethics Statement
This study was granted a Waiver Of Authorization by Sterling IRB (IRB ID 9558).
Acknowledgments
The authors wish to thank the following from Retina Associates of Cleveland Inc.: Dr Arnold F. Nothnagel and Dr Thomas J Tsai, as well as Tia Drugan for retrieving CMT data from RACI locations. Support was also provided by Novartis Ireland Ltd. employees Ver Bilano, PhD (analytical support), Andrew Heaney, PhD (double programming). Medical writing assistance, under the guidance of the authors, was provided by Stefan Amisten, PhD and Susan Simpson, PhD (both Novartis Ireland Ltd.), in accordance with Good Publication Practice (GPP3) guidelines (http://www.ismpp.org/gpp3). Medical writing support was funded by Novartis Pharma AG.
The Association for Research in Vision and Ophthalmology (ARVO) May 1–4, 2022, Denver, CO, USA.
Funding
Financial support was provided by Novartis Pharma AG (Basel, Switzerland). The sponsor or funding organization participated in the design of the study; management, analysis, and interpretation of the data; preparation, review, and approval of the manuscript.
Disclosure
NS and HK are Novartis employees and HK is a Novartis shareholder. SBS was a Novartis employee at the time of this study and is a current employee of the Novartis Sandoz division. LZ is an employee of KMK Consulting, which was paid by Novartis to conduct the statistical analysis of the study. JMC has received grants from Aerpio, Alcon Laboratories, Alimera Sciences, Allergan/AbbVie, Apellis, Genentech, Hoffman La Roche, MacTel, National Eye Institute, Novartis, Regeneron and RegenexBio, consulting fees from Alimera Sciences, Apellis and RegenexBio, honoraria from Alimera Sciences, Allergan/AbbVie, Apellis, Genentech, Iveric Bio, Novartis, Regeneron and RegenexBio. DM reports consultancy fees and Speakers’ Bureau honoraria from Regeneron Pharmaceuticals. LS has received grants from Alkeus, Apellis, Genentech, Ionis Pharm, NGM, Biopharmaceuticals, Graybug Vision and Kodiak Sciences. The authors report no other conflicts of interest in this work.
References
1. Wong WL, Su X, Li X, et al. Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: a systematic review and meta-analysis. Lancet Glob Health. 2014;2(2):e106–16. doi:10.1016/S2214-109X(13)70145-1
2. Ayoub T, Patel N. Age-related macular degeneration. J R Soc Med. 2009;102(2):56–61. doi:10.1258/jrsm.2009.080298
3. Brown DM, Kaiser PK, Michels M, et al. Ranibizumab versus verteporfin for neovascular age-related macular degeneration. N Engl J Med. 2006;355(14):1432–1444. doi:10.1056/NEJMoa062655
4. Rosenfeld PJ, Brown DM, Heier JS, et al. Ranibizumab for neovascular age-related macular degeneration. N Engl J Med. 2006;355(14):1419–1431. doi:10.1056/NEJMoa054481
5. Heier JS, Brown DM, Chong V, et al. Intravitreal aflibercept (VEGF trap-eye) in wet age-related macular degeneration. Ophthalmology. 2012;119(12):2537–2548. doi:10.1016/j.ophtha.2012.09.006
6. Gale RP, Mahmood S, Devonport H, et al. Action on neovascular age-related macular degeneration (nAMD): recommendations for management and service provision in the UK hospital eye service. Eye. 2019;33(Suppl 1):1–21. doi:10.1038/s41433-018-0300-3
7. Skelly A, Bezlyak V, Liew G, Kap E, Sagkriotis A. Treat and extend treatment interval patterns with anti-VEGF therapy in namd patients. Vision. 2019;3(3). doi:10.3390/vision3030041
8. Ricci F, Bandello F, Navarra P, Staurenghi G, Stumpp M, Zarbin Z. Neovascular age-related macular degeneration: therapeutic management and new-upcoming approaches. Int J Mol Sci. 2020;21(21). doi:10.3390/ijms21218242
9. Dugel PU, Koh A, Ogura Y, et al. HAWK and harrier: phase 3, multicenter, randomized, double-masked trials of Brolucizumab for Neovascular age-related macular degeneration. Ophthalmology. 2020;127(1):72–84. doi:10.1016/j.ophtha.2019.04.017
10. Dugel PU, Singh RP, Koh A, et al. HAWK and harrier: ninety-six-week outcomes from the phase 3 trials of brolucizumab for neovascular Age-related macular degeneration. Ophthalmology. 2021;128(1):89–99. doi:10.1016/j.ophtha.2020.06.028
11. Gillies MC, Campain A, Barthelmes D, et al. Long-term outcomes of treatment of neovascular age-related macular degeneration: data from an observational study. Ophthalmology. 2015;122(9):1837–1845. doi:10.1016/j.ophtha.2015.05.010
12. Bakri SJ, Karcher H, Andersen S, Souied EH. Anti-VEGF treatment discontinuation and interval in neovascular age-related macular degeneration in the US. Am J Ophthalmol. 2022;242:189–196. doi:10.1016/j.ajo.2022.06.005
13. Sobolewska B, Sabsabi M, Ziemssen F. Importance of treatment duration: unmasking barriers and discovering the reasons for undertreatment of anti-VEGF agents in neovascular age-related macular degeneration. Clin Ophthalmol. 2021;15:4317–4326. doi:10.2147/OPTH.S325763
14. Chakravarthy U, Harding SP, Rogers CA, et al. Alternative treatments to inhibit VEGF in age-related choroidal neovascularisation: 2-year findings of the IVAN randomised controlled trial. The Lancet. 2013;382(9900):1258–1267. doi:10.1016/S0140-6736(13)61501-9
15. Martin DF, Maguire MG, Fine SL, et al. Comparison of Age-related Macular Degeneration Treatments Trials Research Group. Ranibizumab and bevacizumab for treatment of neovascular age-related macular degeneration: two-year results. Ophthalmology. 2012;119(7):1388–1398. doi:10.1016/j.ophtha.2012.03.053
16. Yang S, Zhao J, Sun X. Resistance to anti-VEGF therapy in neovascular age-related macular degeneration: a comprehensive review. Drug Des Devel Ther. 2016;10:1857–1867. doi:10.2147/DDDT.S97653
17. Baumal CR, Sorensen TL, Karcher H, et al. Efficacy and safety of brolucizumab in age-related macular degeneration: a systematic review of real-world studies. Acta Ophthalmol. 2022;101(2):123–139. doi:10.1111/aos.15242
18. Bilgic A, Kodjikian L, March de Ribot F, et al. Real-world experience with brolucizumab in wet age-related macular degeneration: the REBA study. J Clin Med. 2021;10(13):2758. doi:10.3390/jcm10132758
19. Bulirsch LM, Sassmannshausen M, Nadal J, Leigl R, Thiele S, Holz FG. Short-term real-world outcomes following intravitreal brolucizumab for neovascular AMD: SHIFT study. Br J Ophthalmol. 2022;106(9):1288–1294. doi:10.1136/bjophthalmol-2020-318672
20. Chakravarthy U, Havilio M, Syntosi A, et al. Impact of macular fluid volume fluctuations on visual acuity during anti-VEGF therapy in eyes with nAMD. Eye. 2021;35(11):2983–2990. doi:10.1038/s41433-020-01354-4
21. Chakravarthy U, Pillai N, Syntosi A, Barclay L, Best C, Sagkriotis A. Association between visual acuity, lesion activity markers and retreatment decisions in neovascular age-related macular degeneration. Eye. 2020;34(12):2249–2256. doi:10.1038/s41433-020-0799-y
22. Granstam E, Aurell S, Sjovall K, Paul A. Switching anti-VEGF agent for wet AMD: evaluation of impact on visual acuity, treatment frequency and retinal morphology in a real-world clinical setting. Graefes Arch Clin Exp Ophthalmol. 2021;259(8):2085–2093. doi:10.1007/s00417-020-05059-y
23. MacCumber MW, Yu JS, Sagkriotis A, et al. Antivascular endothelial growth factor agents for wet age-related macular degeneration: an IRIS registry analysis. Can J Ophthalmol. 2021;58(3):252–261. doi:10.1016/j.jcjo.2021.10.008
24. Rave V, Sharma K, Wagner A, Kapoor K. Real-world analysis of brolucizumab in neovascular AMD. Investig Ophthalmol Vis Sci. 2021;62(8):431.
25. Walter SD, Saba NJ. Real-world efficacy and safety of brolucizumab. Investig Ophthalmol Vis Sci. 2021;62(8):456.
26. European Medicines Agency. Brolucizumab SmPC; 2022. Available from: https://www.ema.europa.eu/en/medicines/human/EPAR/beovu.
27. US Food and Drug Administration. Beovu USPI. FDA; 2022. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/761125s000lbl.pdf.
28. Khanani AM, Brown DM, Jaffe GJ, et al. MERLIN: phase 3a, multicenter, randomized, double-masked trial of brolucizumab in participants with nAMD and persistent retinal fluid. Ophthalmology. 2022;129(9):974–985. doi:10.1016/j.ophtha.2022.04.028
29. Coney JM, Zubricky R, Sinha SB, et al. Switching to brolucizumab: injection intervals and visual, anatomical and safety outcomes at 12 and 18 months in real-world eyes with neovascular age-related macular degeneration. Int J Retin Vitr. 2023;9(8). doi:10.1186/s40942-023-00445-0
30. Gregori NZ, Feuer W, Rosenfeld PJ. Novel method for analyzing Snellen visual acuity measurements. Retina. 2010;30(7):1046–1050. doi:10.1097/IAE.0b013e3181d87e04
31. Matsumoto H, Hoshino J, Mukai R, Nakamura K, Akiyama H. One-year results of treat-and-extend regimen with intravitreal brolucizumab for treatment-naive neovascular age-related macular degeneration with type 1 macular neovascularization. Sci Rep. 2022;12(1):8195. doi:10.1038/s41598-022-10578-1
32. Khanani AM, Zarbin MA, Barakat MR, et al. Safety outcomes of brolucizumab in neovascular age-related macular degeneration: results from the IRIS registry and komodo healthcare map. JAMA Ophthalmol. 2022;140(1):20–28. doi:10.1001/jamaophthalmol.2021.4585
33. Robertson JA, Abdulaal M, Moore MT, et al. Risk and assessment of covid-19 in a retina ophthalmologic setting. Investig Ophthalmol Vis Sci. 2021;62(8):1989.
34. Kishimoto MM, Miki A, Chubachi A, et al. One-year results of switching to brolucizumab in exudative age related macular degeneration. Investig Ophthalmol Vis Sci. 2022;63:323–F0154.
35. Liegl RG, Karcher H, Chetty-Mhlanga S, Igwe F, Freitas R. The treatment patterns with brolucizumab in Germany (realize) study: a retrospective cohort study based on longitudinal prescription data. Ophthalmol Ther. 2022;12(1):195–208. doi:10.1007/s40123-022-00596-7
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


