Back to Journals » Neuropsychiatric Disease and Treatment » Volume 13
Once-monthly paliperidone palmitate in early stage schizophrenia – a retrospective, non-interventional 1-year study of patients with newly diagnosed schizophrenia
Authors Emsley R, Hargarter L, Bergmans P, Uglešić B, Sengül AC, Petralia A, Khannanova A, Cherubin P, Schreiner A
Received 26 May 2017
Accepted for publication 7 July 2017
Published 29 August 2017 Volume 2017:13 Pages 2261—2269
DOI https://doi.org/10.2147/NDT.S142634
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Roger Pinder
Robin Emsley,1 Ludger Hargarter,2 Paul Bergmans,3 Boran Uglešić,4 Abdullah Cem Sengül,5 Antonino Petralia,6 Angelina Khannanova,7 Pierre Cherubin,8 Andreas Schreiner2
1Stellenbosch University, Tygerberg Campus, Cape Town, South Africa; 2Janssen Cilag EMEA, Neuss, Germany, 3Janssen Cilag, Clinical Biostatistics, Breda, Netherlands; 4Department of Psychiatry, University Hospital Centre Split, Split, Croatia; 5Özel Antalya Likya Hastanesi, Antalya, Turkey; 6Department of Clinical and Experimental Medicine, School of Medicine, University of Catania, Catania, Italy; 7State Budgetary Healthcare Institution, Psychiatrc Clinical Hospital N3 named after VA Giliarovskiy, Moscow, Russia; 8Janssen Cilag EMEA, Issy-les-Moulineaux, France
Background: Long-acting antipsychotic therapy may be best suited for patients in the early stage of schizophrenia, when the most can be done before disease progression associated with poor adherence occurs. We explored the patterns of use of once-monthly paliperidone palmitate (PP1M), concomitant medication use, hospitalization, and clinical outcomes of adult, newly diagnosed patients with schizophrenia receiving continuous treatment with PP1M for at least 12 months.
Methods: This was an international, multicenter, exploratory, retrospective chart review of medical records of adult patients who were newly diagnosed (not more than 1 year before initiation of PP1M treatment) with schizophrenia and who had received continuous treatment with PP1M for ≥12 months in naturalistic clinical settings.
Results: A total of 84 (93.3%) patients were included in the analysis. All but one patient (98.8%, n=83) had received oral antipsychotic medication at least during the last month before the first PP1M administration. Three patients (3.6%) were newly hospitalized during the 12-month documentation period. The reason for hospitalization for all three was management of episode/relapse. A total of 79.2% of patients had a ≥20% improvement and 47.2% had a ≥50% improvement in Positive and Negative Syndrome Scale total score from baseline to endpoint. Half of patients (53.3%) showed a significant improvement, as reflected by an increase in Personal and Social Performance (PSP) total score of at least 7 points from baseline to endpoint (mean [SD] 11.9 [15.0] points; P<0.001). One quarter of patients (24.4%, n=11) moved from a PSP score of 31–70 (ie, moderate to marked functional impairment) at baseline to a PSP score of mild to no functional impairment (PSP score ≥71) at endpoint. Most adverse drug reactions were mild or moderate in severity.
Conclusion: Continuous treatment with PP1M over 12 months was associated with statistically significant and clinically meaningful improvements in psychotic symptoms, disease severity, and functional outcomes in patients with schizophrenia.
Keywords: long-acting antipsychotic, early diagnosis, schizophrenia, paliperidone palmitate
Introduction
Schizophrenia is a chronic, progressive disease characterized by one or more psychotic episodes.1,2 A large proportion of patients with schizophrenia fail to achieve remission or to recover – at least to the same level as before the prior episode. The process of relapse and incomplete remission often leads to the chronicity of the illness, which is associated with persistent symptoms and lasting deficits in functioning and cognition.1 Patient response to antipsychotic medication is reduced as the illness progresses, and evidence suggests that relapse events are a critical factor in the emergence of treatment refractoriness.3,4 Although there are a number of factors that may contribute to an increased risk of relapse, treatment discontinuation is a very common and important factor in clinical settings, particularly in the early stages of the disease.3,5 However, if patients commit to treatment early in the course of the illness, there is a substantial reduction in number of relapses and a higher rate of remission of psychotic symptoms following the initial episode.1,4,6
Long-acting antipsychotic therapy (LAT) may help to effectively manage the disease in the critical early years by optimizing adherence, improving treatment response, reducing the risk of relapse, and improving long-term outcomes.7,8 LATs already have an established role in the maintenance treatment of chronic, poorly adherent, and/or severely ill patients in the later stages of schizophrenia. However, LAT may perhaps be best suited for patients in the early stage of illness after an initial diagnosis of schizophrenia, when the most can be done for patients before disease progression associated with poor adherence occurs.7,8 Therefore, LATs should be considered as an early and even first-line option in treating schizophrenia, with some guidelines already reflecting this position.2,9 However, partly because of the paucity of evidence for the use of LATs early in the course of schizophrenia, these agents are not often recommended to this patient population.7
The comparative effectiveness of LAT and oral antipsychotics may largely depend on study designs;10,11 although some recent randomized controlled trials have shown no major differences in efficacy, a large set of prospective, retrospective, and mirror-image observational studies conducted in more naturalistic and realistic settings have shown significantly favorable outcomes.10,12–14 Here, we report the findings of an international, multicenter, non-interventional, retrospective chart review that explored the patterns of use of once-monthly paliperidone palmitate (PP1M), concomitant medication use, hospitalization, and clinical outcomes of adult, newly diagnosed patients with schizophrenia receiving continuous treatment with PP1M for at least 12 months in naturalistic clinical settings.
Methods
Study design
This was an international, multicenter, exploratory, retrospective chart review of medical records of adult patients who were newly diagnosed (not more than 1 year before initiation of PP1M treatment) with schizophrenia and who had received continuous treatment with PP1M for ≥12 months. The chart review was conducted at centers in Croatia, Italy, Russia, and Turkey, in which PP1M was approved and available. Our study was specifically designed to select a young patient population at a very early stage of schizophrenia. In accordance with the non-interventional, retrospective study design, patients did not receive any study-specific treatments or any study-specific assessments or evaluations in addition to the treatment they were prescribed by their treating physician. The retrospective documentation period started from the date of the first PP1M administration (baseline) and ended after the first 12 months (365±31 days) of continuous treatment with PP1M (endpoint). Endpoint data were the latest data collected within the 12-month documentation period. Informed written consent was provided by all patients for retrospective data collection and analysis. Ethics approval was provided by the appropriate institutions in the participating countries: Turkey (Pamukkale University Medical Faculty Non-Interventional Clinical Trials Ethics Committee), Italy (Comitato Etico dell’Azienda Sanitaria, dell’Alto Adige c/o Comprensorio, Sanitario di Bolzano, and Comitato Etico A.O. Universitaria Vittorio Emanuele II di Catania), Russia (Independent Ethics Committee at OOO “Arte Med Assistance”, Independent Ethics Committee at Sankt-Peterburgskiy Nauchno-issledovatelskiy institut im. V.M. Bekhterev, and Local Ethics Committee at Gosudarstvennoye Kazennoye Uchrezhdeniye Zdravookhraneniya of Moscow Region “Tsentralnaya Klinicheskaya Psikhiatricheskaya Bolnitsa”), and Croatia (Central Ethics Committee, Zagreb).
Patient selection criteria
Eligible patients
Patients aged 18–29 years at the time of first PP1M administration, with a documented diagnosis of schizophrenia (either according to International Classification of Diseases [ICD]-10 or to Diagnostic and Statistical Manual of Mental Disorders, fourth edition [DSM-IV]) were included. First psychotic episode suggestive of schizophrenia must have been clinically evident not longer than 1 year before the first PP1M administration. Documentation of continuous treatment (defined as regular consecutive administration, as prescribed by the treating clinician, with not more than one missed administration within the 12-month documentation period) with PP1M for at least 12 months (365±31 days) administered for the first time as part of routine clinical practice was required.
Non-eligible patients
Patients with an ICD-10 or DSM-IV axis 1 diagnosis other than schizophrenia were excluded, along with patients diagnosed with alcohol or drug dependence (except for nicotine and caffeine dependence) within 1 month before the initiation of PP1M treatment or during the 12-month documentation period. Patients treated with any LAT before PP1M initiation or with an LAT other than PP1M during the 12-month documentation period were not eligible.
Outcome measures
Primary outcome
Hospitalization – encompassing the number of psychiatric hospitalizations, the number of psychiatric hospitalization days, and the reasons for hospitalizations during the 12-month documentation period.
Other outcomes of interest
Patterns of PP1M treatment within the 12-month documentation period, treatment response (measures of clinical illness, symptom severity), psychosocial functioning, medical resource utilization, psychiatric hospitalizations during the year preceding the first PP1M administration, and safety results were as reported and documented by the clinicians in the medical records.
Assessment of clinical and functional treatment response
The following measures were reported as they were available in the patient records.
Symptom severity – Positive and Negative Syndrome Scale (PANSS) or Brief Psychiatric Rating Scale (BPRS): clinically relevant improvement, defined as a ≥20% decrease in mean PANSS or BPRS total score from baseline to endpoint; or Clinical Global Impression-(CGI) Severity (CGI-S) and/or CGI-Change (CGI-C): clinically relevant improvement will be defined as an improvement in CGI-S of at least 2 points from baseline to endpoint and/or a CGI-C score of ≤2 (much or very much improved) at endpoint, and no PANSS, BPRS, CGI-S or CGI-C score indicating disease worsening; decrease in CGI-S score of ≤2 points or a CGI-C score of ≤3 (1= very much improved; 2= much improved; 3= minimally improved) at endpoint and with no PANSS, BPRS, CGI-S or CGI-C score indicating disease worsening.
Functioning – Personal and Social Performance (PSP), Global Assessment of Functioning (GAF) or Social and Occupational Functioning Assessment Scale (SOFAS): clinically relevant functional improvement, defined as an increase in PSP total score of ≥7 points, or an increase in GAF total score of ≥20 points or an increase in SOFAS total score of ≥30% from baseline to endpoint and with no PSP, GAF, or SOFAS score indicating worsening of the disease.
Statistics
Descriptive statistics were used for all outcomes. Within-group changes from baseline to endpoint were tested using the two-sided Wilcoxon signed-rank test with type I error fixed at 0.05. The last observation carried forward method was used for the endpoint in the analyses of clinical and functional response parameters.
Results
Demographics and baseline characteristics
A total of 90 patients provided written informed consent for this study; of these, 84 (93.3%) patients were eligible for analysis and were included in the full analysis set, and 88 (97.8%) patients received at least one dose of PP1M and were included in the safety analysis set. Two thirds of the patients (69.0%) were male, and the mean age was 24.1(SD 2.7), range 19–29 years. The mean (SD) age at first psychotic episode was 23.8(2.6) years and the mean (SD) time between first onset of psychotic symptoms and the first PP1M administration was 5.5(3.3) months (Table 1). All but one patient (98.8%, n=83) had received oral antipsychotic medication at least during the last month before the first PP1M administration.
PP1M dosing
Overall, 69.0% (n=58) of patients received PP1M according to the initiation regimen as recommended in the summary of product characteristics (150 mg, Day 1; 100 mg, Day 8±4 days, both in deltoid muscle).15 The main reasons for PP1M initiation as documented by the treating clinician were relapse prevention (56.0%), partial/non-adherence to previous medication (20.2%), and convenience (15.5%). From Month 1 after first PP1M administration onwards, 67.9% (n=57) of patients did not change their dose, 6.0% (n=5) of patients had a dose increase, and 28.6% (n=24) of patients had a dose decrease. Overall, 7.1% (n=6) of patients had a dose decrease because of tolerability reasons and 21.4% (n=18) of patients had a decrease to minimize exposure. However, efficacy and/or tolerability were within expectation according to the treating clinician.
Switching and concomitant antipsychotics
A total of 90.5% (n=76/84) of patients were switched from a daily oral antipsychotic to PP1M. Most patients (77.4%, n=65) were switched to PP1M from antipsychotic monotherapy and 13.1% (n=11) of patients were switched from antipsychotic polytherapy. The main antipsychotic from which patients were switched was risperidone (n=58 [69.0%]), followed by paliperidone extended release (n=8 [9.5%]), and olanzapine (n=7 [8.3%]). In the 65 patients who switched from oral monotherapy, 17.9% (n=15) stopped their pre-switch antipsychotic the day before or at the day of the first PP1M administration: for 45.2% (n=38) of patients, the pre-switch antipsychotic monotherapy was tapered off within 4 weeks after the first dose of PP1M; 14.3% of patients (n=12) continued their pre-switch medication for >4 weeks. The most common antipsychotics used concomitantly with PP1M among the full analysis set during the documentation period were oral risperidone (45.2%), olanzapine (7.1%), clozapine (6.0%), and haloperidol (6.0%) (Table 1).
Hospitalizations
Hospitalizations are summarized in Table 2. Of 84 patients in the full analysis set, three (3.6%) were newly hospitalized during the 12-month documentation period. The reason for hospitalization for all three was management of episode/relapse; the mean number of hospitalization days was 15.7 (mean of 10, 12 and 25) days (Figure 1).
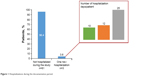  | Figure 1 Hospitalizations during the documentation period. |
None of the hospitalizations were reported to be a result of a serious adverse drug reaction (ADR). Almost half of patients (42.9%) were in hospital at the time they received the first PP1M administration (index hospitalizations – hospitalizations that started before the first PP1M administration and ended after the first PP1M administration), and the mean number of days spent in this index hospital stay (SD) was 52.1(40.6) days. The main reason for the index hospitalization was management of episode/relapse with the previous oral antipsychotic medication (35 of 36 patients were receiving oral antipsychotic treatment when admitted for the index hospitalization).
Other outcomes of interest
PANSS and CGI-S
Seventy-two patients had a PANSS assessment documented at baseline and at least one additional time point during the 12-month period. Most patients (n=65/72) had a PANSS assessment at or around the study endpoint. A total of 79.2% of these patients had a ≥20% improvement and a total of 47.2% had a ≥50% improvement in PANSS total score from baseline to endpoint (Figure 2A). Overall, there was a statistically significant (P<0.001) and clinically relevant improvement in mean (SD) PANSS total score of −31.6(21.1) from baseline to endpoint (Figure 2B). Sixty-eight patients had a CGI-S score documented at baseline and at least one additional time point during the 12-month period. A total of 82.4% of patients were minimally, much, or very much improved at endpoint (defined as CGI-S score decrease of ≥2 points). There was a significant mean (SD) change in CGI-S score from baseline to endpoint of −2.5 (1.1); P<0.001 (Figure 2B). Sixty-eight patients had a CGI-C score documented at baseline and at least one additional time point during the 12-month period. At endpoint, a total of 70.6% of patients had a CGI-C score of ≤2 (were either much, or very much improved) at endpoint.
PSP and GAF
Forty-five patients had a PSP assessment documented at baseline and at least at one additional time point during the 12-month documentation period. Most patients (n=38/45) had a PSP assessment at or around endpoint. The mean PSP total score at baseline was 52.1 (range 23–80); only 11.1% (n=5) of patients were rated as having good functioning or mild functioning difficulties at baseline (PSP score ≥71). A total of 53.3% of patients showed a significant improvement, as reflected by an increase in PSP total score of at least 7 points from baseline to endpoint (mean [SD] 11.9 [15.0] points; P<0.001) (Figure 3). One quarter of patients (24.4%, n=11) moved from a PSP score of 31–70 (ie, moderate to marked functional impairment) at baseline to a PSP score of mild to no functional impairment (PSP score ≥71) at endpoint. Of the 47 patients with documented GAF scores, 72.3% (n=34) showed a significant improvement in GAF score as reflected by an increase of at least 20 points from baseline to endpoint (mean [SD] change 26.1 [12.3] points; P<0.001) (Figure 3).
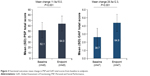  | Figure 3 Functional outcomes: mean change in PSP and GAF total scores from baseline to endpoint. |
BPRS assessments were found to be documented in only one patient’s medical record, and there were no SOFAS assessments available in any medical records.
Safety
Overall, for 14.8% (n=13) of 88 patients in the safety analysis set, ≥1 ADR was reported, which was defined as an adverse event that was at least possibly causally related to PP1M treatment. ADRs occurring in ≥2% of patients are summarized in Table 3. Most ADRs were mild or moderate in severity. For three patients (3.4%), a severe ADR related to hyperprolactinemia was reported. Seven (8%) patients had an ADR that led to a dose change at the discretion of the treating physician. Median body weight (SD) increase from baseline to last PP1M administration was 1.2 (3.9) kg; P<0.001 (n=85).
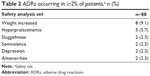  | Table 3 ADRs occurring in ≥2% of patients,a n (%) |
Medical resource utilization/living-housing status/employment and education
The most common type of outpatient consultation during the 12-month documentation period was consultation with a psychiatrist or neurologist (23.8%, n=20 patients with ≥1 consultation). Only one (1.2%) patient had an emergency room visit. Almost all patients (97.6%, n=82) were living at home (alone or with family/friends) at baseline, and no change in living status was observed at endpoint. For those patients who were employed (n=19), the mean number of working days lost as a result of their illness or treatment during the last 3 months of the 12-month documentation period was 0.9 days (range 0–14 days), which was different from the mean number of working days lost during the 3 months before starting PP1M (n=13; 34.5 days [range 0–90 days]). For the 13 patients who were students, no educational days were reported lost during the last 3 months of the documentation period (n=11), compared with a mean of 38.5 days lost (n=10) during the 3 months before starting PP1M.
Discussion
Using a pragmatic, retrospective approach, the present study explored the efficacy of continuous treatment with an atypical once-monthly LAT by exploring “real-world” treatment characteristics and outcomes in young, newly diagnosed adults with schizophrenia who received long-term treatment with PP1M over 12 months. The retrospective and therefore non-interventional design enabled the evaluation of patients who had been diagnosed with schizophrenia around 5 months before treatment with PP1M and who had a low prior lifetime exposure to antipsychotic medication, in a naturalistic setting, without study-related influences on routine clinical practice.
The characteristics of the patient population in the present study reflect those of patients in naturalistic clinical settings in that baseline scores indicated significant levels of symptom severity and functional impairment associated with an acute first episode of illness. Most patients in this population maintained their dose or had a dose decrease of PP1M, in line with the observation that first-episode patients, in general, may require normal or lower doses of medication.16 The patients in this study had likely been acutely psychotic for a limited period of time as indicated by the short mean time between first psychotic symptoms and enrollment; the significant clinical improvement observed in this population is consistent with favorable outcomes observed in young, first-episode patients in other studies, in which continuous treatment was provided by use of an atypical long-acting antipsychotic formulation.17 In a previous study of flexibly dosed PP1M in acutely ill patients with schizophrenia who were unsuccessfully treated with oral antipsychotics, transition to PP1M treatment resulted in significant improvement of symptoms as early as 1 week after the first PP1M administration, and these improvements were further sustained over the following 6 months of treatment.18
In the present study, almost half of the patients achieved a robust treatment response (ie, ≥50% decrease in PANSS total score) by the end of the documentation period. Although there is no set cut-off in patients with first-episode schizophrenia,19 it has been suggested that the most appropriate definition of response in schizophrenia research is a ≥50% improvement in PANSS total score,20,21 given the generally favorable response to antipsychotic treatment in these patients. One analysis that was conducted to explore the predictive validity of early response in first-episode schizophrenia found that the best PANSS score cut-off to predict maintenance of response was 51.6%.22
The low rates of rehospitalization during the treatment period are consistent with results of a randomized controlled 2-year study in recently diagnosed patients with schizophrenia (within 1–5 years). In this study, PP1M was better in preventing relapse compared with physician’s choice of oral antipsychotics,13 an important implication given the evidence that relapse events may be one critical factor in treatment-emergent refractoriness.3 Compared with multi-episode patients, those with first-episode schizophrenia are more likely to achieve remission, as they are more likely to respond favorably to antipsychotic treatment.17,23
The safety results in the present study suggest that the treatment for those patients receiving PP1M for 12 months or longer was well tolerated and ADRs were consistent with the known safety profile of PP1M.13,18,24,25 This is noteworthy given that patients with newly diagnosed schizophrenia may be particularly susceptible to antipsychotic side effects, such as weight gain, metabolic abnormalities, and extrapyramidal symptom (EPS) side effects.26,27 The mean changes in body weight and body mass index observed in the current study did not differ from those changes observed in other studies with PP1M in patients with more chronic schizophrenia.24,28 The incidence of EPS-related ADRs and the use of anticholinergic medication was low; these results are in line with observations that young patients in remission received lower doses of a long-acting antipsychotic and had fewer EPS side effects.17
Limitations
This was a retrospective chart review, designed to explore treatment outcomes with PP1M in newly diagnosed patients with schizophrenia over a long-term period (at least 12 months) by use of efficacy measures as they were routinely documented in patients’ medical records. Sites were eligible for participation if standard efficacy measures were documented at least at the beginning of treatment with PP1M and at the end of the observation period (at least 12 months later). Furthermore, sites were requested to capture these measures if available from the medical records at any time point in between, but it was expected that such measures may not be frequently assessed in routine clinical settings, or that the frequency of such assessments may vary considerably between sites and patients. Although the inclusion of patients with more than two documented assessments may have further strengthened the results, it would have required a highly complex selection process and considerable efforts to select sites and patients’ records with similar and/or comparable assessment dates. These criteria may have biased the study-site selection. Inclusion criteria required patients to have been receiving PP1M for at least 12 months, thereby selecting a group that continued and responded well on PP1M. Therefore, the present results cannot be generalized to patients who were treated with PP1M for a shorter or longer period of time or a broader schizophrenia population, because of the specific patient group assessed (young, adult, recently diagnosed patients with schizophrenia who had been treated with PP1M for at least 12 months). The objective of this pragmatic and naturalistic study was not to compare different treatments; therefore, no active treatment control group was included in the design. Nevertheless, this limits the generalizability of the conclusions drawn. However, the outcomes of this study can be indirectly compared with outcomes from other similar open-label studies conducted in similar populations of patients with schizophrenia.17
Conclusion
The present study aimed to address the paucity of naturalistic data in young patients with schizophrenia treated with an atypical LAT at an early stage of the illness and over a longer period of time. In this study, continuous treatment with PP1M over 12 months was associated with statistically significant and clinically meaningful improvements in psychotic symptoms, disease severity, and functional outcomes in patients with schizophrenia. More importantly, the rate of hospitalization over the 12 months of treatment was low, which is consistent with evidence demonstrating that treatment of schizophrenia with LAT can improve relapse rates.6,8,12–14 The importance of these findings rests in the clinical imperative of managing first-episode patients to prevent further relapses and to minimize the burden and distress that these relapses may have in derailing hard-won progress in psychosocial recovery; and in reducing both the risk of persistent psychosis after each new episode and the added economic burden of treating relapse.7 Results of this study suggest that PP1M is efficacious and well tolerated when used as an early option in treating schizophrenia. Continuous antipsychotic treatment during the early years of the disease may be critical, as this is when the illness is at its most aggressive, and when relapses and illness progression are most likely to occur.29,30
Acknowledgments
The study was sponsored by Janssen Pharmaceutica NV. Medical writing assistance was provided by ApotheCom Ltd, London, and funded by Janssen Pharmaceutica NV.
Disclosure
In the past 3 years, Dr Emsley has participated in speakers/advisory boards and received honoraria from Janssen, Lundbeck, Servier and Otsuka. He has also received research funding from Janssen and Lundbeck.
Dr Hargarter, Dr Schreiner, and Mr Bergmans are full-time employees of Janssen Cilag and are shareholders of Johnson & Johnson. Mr Cherubin is a full-time employee of Janssen Cilag.
Drs Uglešić, Sengül, Petralia, and Khannanova have no conflicts of interest in this work.
References
Lieberman JA, Perkins D, Belger A, et al. The early stages of schizophrenia: Speculations on pathogenesis, pathophysiology, and therapeutic approaches. Biol Psychiatry. 2001;50(11):884–897. | ||
Hasan A, Falkai P, Wobrock T, et al. World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for biological treatment of schizophrenia, part 2: Update 2012 on the long-term treatment of schizophrenia and management of antipsychotic-induced side effects. World J Biol Psychiatry. 2013;14(1):2–44. | ||
Emsley R, Chiliza B, Asmal L, Harvey BH. The nature of relapse in schizophrenia. BMC Psychiatry. 2013;13:50. | ||
Wiersma D, Nienhuis FJ, Slooff CJ, Giel R. Natural course of schizophrenic disorders: A 15-year followup of a dutch incidence cohort. Schizophr Bull. 1998;24(1):75–85. | ||
Caseiro O, Pérez-Iglesias R, Mata I, et al. Predicting relapse after a first episode of non-affective psychosis: a three-year follow-up study. J Psychiatr Res. 2012;46(8):1099–1105. | ||
Emsley R, Medori R, Koen L, Oosthuizen PP, Niehaus DJ, Rabinowitz J. Long-acting injectable risperidone in the treatment of subjects with recent-onset psychosis: a preliminary study. J Clin Psychopharmacol. 2008;28(2):210–213. | ||
Emsley R, Chiliza B, Asmal L, Mashile M, Fusar-Poli P. Long-acting injectable antipsychotics in early psychosis: a literature review. Early Interv Psychiatry. 2013;7(3):247–254. | ||
Subotnik KL, Casaus LR, Ventura J, et al. Long-acting injectable risperidone for relapse prevention and control of breakthrough symptoms after a recent first episode of schizophrenia. A randomized clinical trial. JAMA Psychiatry. 2015;72(8):822–829. | ||
Malla A, Tibbo P, Chue P, et al. Long-acting injectable antipsychotics: recommendations for clinicians. Can J Psychiatry. 2013;58(5 Suppl 1):30S–35S. | ||
Kirson NY, Weiden PJ, Yermakov S, et al. Efficacy and effectiveness of depot versus oral antipsychotics in schizophrenia: synthesizing results across different research designs. J Clin Psychiatry. 2013;74(6):568–575. | ||
Alphs L, Schooler N, Lauriello J. How study designs influence comparative effectiveness outcomes: the case of oral versus long-acting injectable antipsychotic treatments for schizophrenia. Schizophr Res. 2014;156(2–3):228–232. | ||
Kishimoto T, Nitta M, Borenstein M, Kane JM, Correll CU. Long-acting injectable versus oral antipsychotics in schizophrenia: a systematic review and meta-analysis of mirror-image studies. J Clin Psychiatry. 2013;74(10):957–965. | ||
Schreiner A, Aadamsoo K, Altamura AC, et al. Paliperidone palmitate versus oral antipsychotics in recently diagnosed schizophrenia. Schizophr Res. 2015;169(1–3):393–399. | ||
Gaebel W, Schreiner A, Bergmans P, et al. Relapse prevention in schizophrenia and schizoaffective disorder with risperidone long-acting injectable vs quetiapine: results of a long-term, open-label, randomized clinical trial. Neuropsychopharmacology. 2010;35(12):2367–2377. | ||
Janssen Cilag. Paliperidone palmitate summary of product characteristics. Janssen Cilag; 2016. Available from: http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/002105/WC500103317.pdf. Accessed July 12, 2017. | ||
Alvarez-Jimenez M, O’Donoghue B, Thompson A, et al. Beyond clinical remission in first episode psychosis: thoughts on antipsychotic maintenance vs. guided discontinuation in the functional recovery era. CNS Drugs. 2016;30(5):357–368. | ||
Emsley R, Oosthuizen P, Koen L, Niehaus DJ, Medori R, Rabinowitz J. Remission in patients with first-episode schizophrenia receiving assured antipsychotic medication: a study with risperidone long-acting injection. Int Clin Psychopharmacol. 2008;23(6):325–331. | ||
Hargarter L, Cherubin P, Bergmans P, et al. Intramuscular long-acting paliperidone palmitate in acute patients with schizophrenia unsuccessfully treated with oral antipsychotics. Prog Neuropsychopharmacol Biol Psychiatry. 2015;58:1–7. | ||
Kinon BJ, Chen L, Ascher-Svanum H, et al. Early response to antipsychotic drug therapy as a clinical marker of subsequent response in the treatment of schizophrenia. Neuropsychopharmacology. 2010;35(2):581–590. | ||
Schennach R, Riedel M, Musil R, Möller HJ. Treatment response in first-episode schizophrenia. Clin Psychopharmacol Neurosci. 2012;10(2):78–87. | ||
Leucht S. Measurements of response, remission, and recovery in schizophrenia and examples for their clinical application. J Clin Psychiatry. 2014;75 Suppl 1:8–14. | ||
Schennach R, Riesbeck M, Mayr A, et al. Should early improvement be re-defined to better predict the maintenance of response in first-episode schizophrenia patients? Acta Psychiatr Scand. 2013;127(6):474–481. | ||
Agid O, Schulze L, Arenovich T, et al. Antipsychotic response in first-episode schizophrenia: efficacy of high doses and switching. Eur Neuropsychopharmacol. 2013;23(9):1017–1022. | ||
Schreiner A, Bergmans P, Cherubin P, et al. Paliperidone palmitate in non-acute patients with schizophrenia previously unsuccessfully treated with risperidone long-acting therapy or frequently used conventional depot antipsychotics. J Psychopharmacol. 2015;29(8):910–922. | ||
Schreiner A, Bergmans P, Cherubin P, et al. A prospective flexible-dose study of paliperidone palmitate in nonacute but symptomatic patients with schizophrenia previously unsuccessfully treated with oral antipsychotic agents. Clin Ther. 2014;36(10):1372–1388.e1. | ||
McEvoy JP, Lieberman JA, Perkins DO, et al. Efficacy and tolerability of olanzapine, quetiapine, and risperidone in the treatment of early psychosis: a randomized, double-blind 52-week comparison. Am J Psychiatry. 2007;164(7):1050–1060. | ||
Maayan L, Correll CU. Management of antipsychotic-related weight gain. Expert Rev Neurother. 2010;10(7):1175–1200. | ||
Hargarter L, Bergmans P, Cherubin P, et al. Once-monthly paliperidone palmitate in recently diagnosed and chronic non-acute patients with schizophrenia. Expert Opin Pharmacother. 2016;17(8):1043–1053. | ||
Birchwood M, Todd P, Jackson C. Early intervention in psychosis. The critical period hypothesis. Br J Psychiatry Suppl. 1998;172(33):53–59. | ||
Andreasen NC, Liu D, Ziebell S, Vora A, Ho BC. Relapse duration, treatment intensity, and brain tissue loss in schizophrenia: a prospective longitudinal mri study. Am J Psychiatry. 2013;170(6):609–615. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



