Back to Journals » Clinical Ophthalmology » Volume 9
Ocular leech infestation
Received 22 December 2014
Accepted for publication 20 January 2015
Published 27 February 2015 Volume 2015:9 Pages 419—421
DOI https://doi.org/10.2147/OPTH.S79735
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Yueh-Chang Lee, Cheng-Jen Chiu
Department of Ophthalmology, Buddhist Tzu-Chi General Hospital, Hualien, Taiwan, ROC
Abstract: This case report describes a female toddler with manifestations of ocular leech infestation. A 2-year-old girl was brought to our outpatient clinic with a complaint of irritable crying after being taken to a stream in Hualien 1 day previous, where she played in the water. The parents noticed that she rubbed her right eye a lot. Upon examination, the girl had good fix and follow in either eye. Slit-lamp examination showed conjunctival injection with a moving dark black–brown foreign body partly attached in the lower conjunctiva. After applying topical anesthetics, the leech, measuring 1 cm in length, was extracted under a microscope. The patient began using topical antibiotic and corticosteroid agents. By 1 week after extraction, the patient had no obvious symptoms or signs, except for a limited subconjunctival hemorrhage, and no corneal/scleral involvement was observed.
Keywords: leech, ocular foreign body, conjunctival reaction, pediatric ophthalmology
Introduction
Ocular foreign bodies account for a significant number of emergency room visits. It is estimated that in 47% of the reported injuries in the United States Eye Injury Registry, the mechanism of injury increased the risk for an ocular foreign body,1 however, the presence of a leech as an ocular foreign body was seldom reported. Herein, we report the youngest case of conjunctival leech infestation in English literature, which was removed carefully without long-term complication.
Case report
A 2-year-old girl was brought to our outpatient clinic with a complaint of irritable crying after being taken to a stream in Hualien 1 day previous, where she played in the water. The parents noticed that she rubbed her right eye a lot. There was no history of trauma to the eye or any other chronic eye disorders.
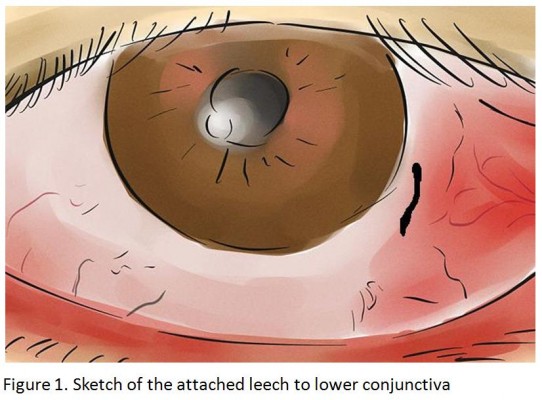
Upon examination, the girl had good fix and follow in either eye. Slit-lamp examination showed conjunctival injection with a moving dark black–brown foreign body partly attached in the lower conjunctiva near the limbus, resembling uveal prolapse. The dark black–brown foreign body was partially movable, with tail hanging. It was then identified as a live leech grasping the bulbar conjunctiva (Figure 1). After applying topical anesthetics, the leech was extracted under microscope with forceps, and it measured 1 cm in length (Figure 2). The patient began using topical antibiotic and corticosteroid agents afterward.
  | Figure 1 Sketch of the leech attached to the lower conjunctiva. |
  | Figure 2 The removed leech. |
By 1 week after extraction, the patient had no obvious symptoms or signs, except for a mild congestion and patchy subconjunctival hemorrhage. There was no evidence of scleral perforation, corneal injury, uveal prolapse, or uveitis.
Discussion
Therapeutic use of leeches has been documented over the past 2,500 years. Before the medical and pharmacological advances that followed World War II, bloodletting by leeches was even reported to be an effective way of treating acute congestive glaucoma.2 In modern plastic surgery, they have been used as decongestants for draining periorbital and scrotal hematomas.3,4 In a hospital emergency setting, there have been cases of ocular leech infestation described in publication, eg, a 32-year-old man in People’s Republic of China,5 a 4-year-old girl in Ethiopia,6 a 67-year-old man in Iran,7 a 66-year-old woman in Australia,7 a 38-year-old woman in Japan,8 a 28-year-old man in the UK,9 a 4-year-old girl in Germany,10 and a 7-year-old boy in Turkey.11 Herein, we report the youngest case of conjunctival leech infestation in English literature.
In previous literature, five ocular leeches were removed directly with forceps after instillation of local anesthetic.5,8,10–12 Other preparing methods before leech removal included irrigation with normal saline in combination with injection of suxamethonium into the worm,6 application of 3% hypertonic saline drops,7 or even direct application of cooking salt to the leech.9 None of the articles reported long-term complications. The method of extraction we used involved instilling topical anesthetic drops and removing the leech with forceps using precaution to ensure that the leech’s suckers and midbody were detached from the eyeball completely. We advocate that leech removal with forceps after instillation of local anesthetic is a safe method and should be attempted first. In refractory cases when the leech is firmly attached, additional preparing methods could be used, taking possible undesired eye irritation into consideration.
Although most human leech infestations have been found by otolaryngologists in the nasopharynx, ocular leech infestation should be considered in the differential diagnosis of patients presenting with ocular complaints, especially in those with a history of swimming or any type of exposure to water in streams and lakes. With proper management, it is feasible to preserve optimal ocular function, minimize morbidity, and reduce discomfort in the patient.
Disclosure
The authors report no conflicts of interest in this work.
References
Upshaw JE, Brenkert TE, Losek JD. Ocular foreign bodies in children. Pediatr Emerg Care. 2008;24:409–414. [quiz 415-7]. | ||
Lowe RF. Acute glaucoma – 1941. Aust N Z J Ophthalmol. 1995;23:213–215. | ||
Menage MJ, Wright G. Use of leeches in a case of severe periorbital haematoma. Br J Ophthalmol. 1991;75:755–756. | ||
Bunker TD. The contemporary use of the medicinal leech. Injury. 1981;12:430–432. | ||
Li WW, Shen T, Jiang J. Ocular leech infestation initially misdiagnosed as conjunctival pigmented nevus. Int J Ophthalmol. 2013;6:557–558. | ||
Tenkir A, Tibebu T. Leech on the eye in a child. Ethiop Med J. 2010;48:177–180. | ||
Partyka C, Fogg T. Leech on the eye: a novel use for hypertonic saline. Emerg Med Australas. 2009;21:84–85. | ||
Nawa Y, Hatanaka O, Hara Y, Ishizaka S. A case of conjunctival leech infestation. Jpn J Ophthalmol. 2006;50:64–65. | ||
Lewis G, Coombes A. Adult ocular leech infestation. Eye (London). 2006;20:391–392. | ||
Auw-Haedrich C, Keim A, Kist M. Conjunctival infestation of a child with Theromyzon tessulatum. Br J Ophthalmol. 1998;82:1093–1094. | ||
Alcelik T, Cekic O, Totan Y. Ocular leech infestation in a child. Am J Ophthalmol. 1997;124:110–112. | ||
Dey R, Dey S. Ocular leech infestation. Arch Iran Med. 2010;13:440–442. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
