Back to Journals » Risk Management and Healthcare Policy » Volume 9
Occupational management in the workplace and impact on injury claims, duration, and cost: a prospective longitudinal cohort
Received 3 March 2016
Accepted for publication 5 May 2016
Published 27 July 2016 Volume 2016:9 Pages 185—191
DOI https://doi.org/10.2147/RMHP.S107721
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Frank Papatheofanis
Mark E Lemstra
Alliance Health Medical Clinic, Moose Jaw, SK, Canada
Abstract: Few workplaces have prospectively reviewed workplace and worker issues simultaneously and assessed their impact on Workers’ Compensation Board (WCB) claims. In January of 2014, each worker in a large workplace in Saskatchewan, Canada, was prospectively followed for 1 year to determine factors that impact injury claim incidence, recovery, and costs. In total, 207 out of 245 workers agreed to complete the baseline survey (84.5%). In 2014, 82.5% of workers had self-reported pain, but only 35.5% submitted a WCB claim. Binary logistic regression was used to compare those with pain who did not submit a WCB injury claim to those with pain who did initiate a WCB claim. Independent risk factors associated with WCB claim incidence included depressed mood (odds ratio [OR] =2.75, 95% confidence interval [CI] 1.44–9.78) and lower job satisfaction (OR =1.70, 95% CI 1.08–10.68). Higher disability duration was independently associated with higher depressed mood (OR =1.60, 95% CI 1.05–4.11) and poor recovery expectation (OR =1.31, 95% CI 1.01–5.78). Higher cost disability claims were independently associated with higher depressed mood (OR =1.51, 95% CI 1.07–6.87) and pain catastrophizing (OR =1.11, 95% CI 1.02–8.11). Self-reported pain, physically assessed injury severity, and measured ergonomic risk of workstation did not significantly predict injury claim incidence, duration, or costs. In January 2015, the workplace implemented a new occupational prevention and management program. The injury incidence rate ratio reduced by 58% from 2014 to 2015 (IRR =1.58, 95% CI =1.28–1.94). The ratio for disability duration reduced by 139% from 2014 to 2015 (RR =2.39, 95% CI =2.16–2.63). Costs reduced from $114,149.07 to $56,528.14 per year. In summary, WCB claims are complex. Recognizing that nonphysical factors, such as depressed mood, influence injury claim incidence, recovery, and costs, can be helpful to claims management.
Keywords: workplace, Workers Compensation Board, injury claim, depressed mood, return-to-work program, job satisfaction
Introduction
Workers Compensation Board (WCB) injuries are complex. As such, treatment-focused programs in isolation have not reduced injury claim incidence, duration, or cost in the workplace.1–3
For example, the Institute for Work and Health (IWH) systematically reviewed injury prevention and loss control. The only intervention to demonstrate a strong level of evidence was proactive return-to-work programs, which included on-site education and offered return to work with modified duties. A moderate level of evidence was found for employee support and daily exercise.4
The IWH also performed a second systematic literature review on workplace return-to-work programs. No intervention had high levels of evidence for reducing claim incidence, duration, or costs. A moderate level of evidence was found for seven interventions, including 1) immediate contact with the worker and job accommodation; 2) independent ergonomic assessments with the goal of return-to-work coordination; 3) on-site education with supervisors and managers on how to facilitate early return to work; 4) active participation from workers in the return-to-work process; 5) creating conditions of goodwill; 6) avoiding miscommunication; and 7) allowing on-site, independent occupational health professionals to bridge communication between management, workers, and external health care practitioners.5
The IWH also performed a third systematic literature review on prognostic factors that negatively influence worker (not workplace) disability time. Strong evidence was found for five prognostic factors, including 1) worker’s poor recovery expectations; 2) passive (not active) rehabilitation; 3) worker’s self-report high pain intensity; 4) radiating pain; and 5) poor job satisfaction.6
Aside from IWH, four systematic literature reviews have also been conducted by the Cochrane Collaboration. One review found that exercise for the treatment of back pain reduces the number of recurrences of back pain.7 Similarly, a second review found that advice to stay active after a low back injury was more effective in pain relief and ability to perform work in comparison to bed rest.8 A third review found that back education in occupational settings reduced pain, increased function, and improved return-to-work status.9 A fourth review found that off-site work hardening programs had no effect on disability duration.10
There are five additional systematic literature reviews that were not published by either the IWH or Cochrane. One found evidence to support exercise in the prevention of occupational back pain.11 Similarly, another review concluded that there was strong evidence to support exercise for both treatment and prevention of back pain in the workplace.12 A third review found that advice to keep active was sufficient for acute work injuries, but specific exercises were required for subchronic and chronic occupational back injuries.13 A fourth review concluded that the best overall intervention to promote early return to work after an occupational injury was combining clinical interventions with occupational interventions, including modified work duties.14 Finally, the fifth review concluded that the most effective interventions at promoting return to-work were those that combined employers, employees, and health practitioners working together to implement work modifications.15
The first objective of the current study was to determine which factors prospectively determined WCB injury claim incidence, higher duration, and higher costs. The second objective was to determine if a new, comprehensive occupational program reduced injury claim incidence, duration of disability time, and costs. This program included on-site education, ergonomic evaluations, advice to stay active, immediate contact with workers, support from managers and union, enhanced communication, proactive offer of return to work with modified duties, and independent on-site physical and occupational therapists
Methods
In January of 2014, each worker at a large company (meat company with kill floor, processing area, and shipping) in Saskatchewan, Canada, was asked to complete a confidential survey that was voluntary. There was no inclusion or exclusion criteria. Because intervention was requested by both management and the union, the survey was voluntary, results were placed in a sealed envelope with confidentiality and privacy assured by the independent researchers, and the results were stored in the confidential file area of a medical clinic with experience in privacy and health information protection. Because the intervention was jointly requested by the union and its workers as part of a broad proactive health initiative, external ethics review was not required.
Measurement
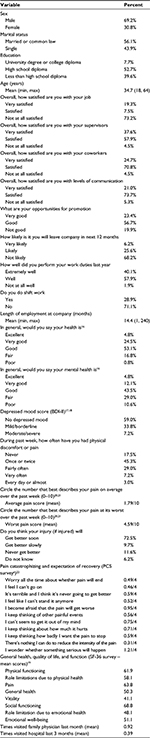
Based on the literature review, the survey was designed to collect information on demographics, job satisfaction, self-report health, depressed mood, general health status, and pain. Questions addressing drug use, alcohol use, and suicide ideation were prohibited by the union.
Questions on demographics, job satisfaction, and self-report health came from the Canadian Community Health Survey conducted by Statistics Canada.16 The Beck Depression Inventory II (BDI-II) was used to measure depressed mood.17 This survey has good internal scale reliability for community-dwelling adults (Cronbach’s α =0.86–0.92).18 Those who scored 11 or higher on the BDI-II were considered to have depressed mood. The Short Form-36 (SF-36) was used to measure general health status.19 The SF-36 is a commonly used instrument that measures eight dimensions of self-report health, quality of life, and function.
Participants also completed a pain scale and a visual analog scale measuring pain from 0 (no pain) to 10 (as bad as it can be) for 1) average pain and for 2) pain at its worst over the past week.20,21 Coping with pain and expectation of recovery was measured with the Pain Catastrophizing Scale. The Pain Catastrophizing Scale is well known, with established reliability (r=0.75) and validity (scale explains 59% of variance in pain).22
Ergonomic risk of injury included direct measurement of each workstation by an occupational therapist. The occupational therapist used the WorkSmart Ergonomic Systems Specialist program to code all workstations into either low, medium, or high risk of injury. Low risk was defined as only one significant exposure to musculoskeletal injury, moderate risk was two significant exposures, and high risk was three or more significant exposures to musculoskeletal injury.23
Intervention
In 2014, each worker was asked to present to an on-site occupational therapist for musculoskeletal screening. If the worker had pain, the injury was coded as 1 (pain, stiffness, or tenderness without physical signs), 2 (pain and musculoskeletal signs), 3 (pain and neurological signs), or 4 (pain and fracture or dislocation). The classifications came from the Quebec Task Force for neck and back pain.24
Binary logistic regression was used to compare those with pain who did not submit a WCB injury claim to those with pain who did initiate a WCB claim in 2014. Regression was used to compare higher duration claims (top 50%) to lower duration WCB injury claims (lower 50%) and higher cost claims (top 50%) to lower cost WCB injury claims (lower 50%) in 2014. In total, 24 self-report survey variables, ergonomic workstation risk variables, and direct physical evaluation variables were included for analysis. The unadjusted effect of each covariate was determined and then entered one step at a time based on changes in the −2 log likelihood and the Wald test. The final results are presented as adjusted odds ratios (ORs) with 95% confidence intervals (CIs).25
The management (January 5, 2015) and the union (January 15, 2015) signed a contract for an on-site occupational management program. Any worker with pain or stiffness was encouraged to see the on-site independent occupational therapist or physical therapist for education (ie, stretches), advice to stay active, enhanced communication between the worker and supervisor, and proactive offer of return to work with modified duties. The program did not provide on-site treatment. If a worker had a serious injury, they were advised to go to their family physician. The occupational management intervention was 1 hour a day, 5 days a week, for 1 year. The program was based on an evidence-based review of the literature described previously.5–15
Ergonomic evaluations and recommendations on 77 workstations took 154 hours, whereas physical assessments of 207 workers took 69 hours. The WCB results were analyzed on February 3, 2016 to allow sufficient time for claims adjudication.
Results
In 2014 and 2015, the company had 245 full-time workers. For data collection in 2014, 207 out of 245 workers agreed to complete the questionnaire (84.5% response rate). Job satisfaction was low, with 73.2% not at all satisfied with work. The prevalence of depressed mood was high, with 33.8% reporting mild depressed mood and another 7.2% reporting moderate-to-severe depressed mood (41% with depressed mood). In total, 82.5% of the workforce reported pain at least once per week. The complete results are listed in Table 1.
Ergonomic risk of injury included direct measurement of each of the 77 workstations by an occupational therapist. Low risk was detected at 22 workstations, moderate risk was detected at 46 workstations, and high risk was detected at 9 workstations. The results are listed in Table 2. Among those who completed the survey, the occupational therapist coded the injuries as Level 1 (93% with pain or stiffness or tenderness but without any physical signs) or Level 2 (7% with pain and musculoskeletal signs), with no Level 3 or Level 4 injuries found. Those with musculoskeletal signs were advised to consider seeing their family physician. Three workers with WCB claims refused to be physically assessed by the therapist. This was permitted due to the voluntary nature of the intervention.
  | Table 2 Ergonomic risk of workstations measured by occupational therapist Note: Data from Worksmart Ergonomics Ltd.23 |
For pain catastrophizing, the scores were relatively low, with means ranging from 0.46 to 1.21 out of a maximum score of 4.
Binary logistic regression was used to compare those with pain who did not submit a WCB injury claim to those with pain who did initiate a WCB claim in 2014. Completing a WCB injury claim, in comparison to not initiating a WCB claim, was independently associated with higher depressed mood (OR =2.75, 95% CI 1.44–9.78) and lower job satisfaction (OR =1.70, 95% CI 1.08–10.68).
Regression was used to compare higher duration claims (top 50%) to lower duration WCB injury claims (lower 50%) in 2014. Higher disability duration was independently associated with higher depressed mood (OR =1.60, 95% CI 1.05–4.11) and poor recovery expectation (OR =1.31, 95% CI 1.01–5.78).
Regression analysis was also used to compare higher cost claims (top 50%) to lower cost WCB injury claims (lower 50% of costs) in 2014. Higher cost disability claims were independently associated with higher depressed mood (OR =1.51, 95% CI 1.07–6.87) and pain catastrophizing (OR =1.11, 95% CI 1.02–8.11).
Through regression analysis, it was found that self-report pain, physically assessed injury severity, and measured ergonomic risk of workstation with an occupational therapist did not significantly predict injury claim incidence, duration, or costs.
The results for all three regression analyses can be found in Table 3. In 2014, there were 87 WCB injuries (28 time loss and 59 no time loss), a combined disability duration time of 403 days and a total cost of $114,149.07. In January 2015, the workplace implemented a new occupational program. In response, in 2015, there were 55 WCB injuries (15 time loss and 40 no time loss), a combined disability duration time of 169 days and a total cost of $56,528.14. Computing an injury incidence rate ratio from 2014 to 2015 resulted in a ratio of 1.58 (95% CI 1.28–1.94). Computing a ratio for disability duration from 2014 to 2015 resulted in a ratio of 2.39 (95% CI 2.16–2.63).
Discussion
Work-related injuries and subsequent WCB claims are complex. For that reason, treatment-focused programs working in isolation have not reduced injury claim incidence, duration, or cost in the workplace.1–3
The current study found that depressed mood was associated with injury claim incidence, longer disability duration, and higher costs. In a systematic literature review of predictors of failure to return to work, the authors concluded that recovery expectation and fear avoidance are predictive of outcome, but that depression, job satisfaction, and psychological strain are not.26 The first two conclusions are consistent with our study, whereas the others are inconsistent. A possible explanation could be that this systematic literature review included only nonchronic cases (less than 3 months), nonspecific back pain, and complete failure to return to work in its inclusion criteria.26 In comparison, our study included acute and chronic cases, specific and nonspecific back pain, as well as all other musculoskeletal injuries. We also included those who returned to work and those who did not.
The finding that job satisfaction impacts recovery has been found in other systematic literature reviews.6 In that review, poor job satisfaction was found to delay recovery by 35%.6 The impact of recovery expectation is also not new. In a prospective study of 1,566 injured workers looking specifically at the impact of recovery expectations, the authors found that this one variable explained one-sixth of the variation in duration of disability benefits received.27 This finding is consistent with a systematic literature review.6
The impact of depressed mood or depression has received less attention. As mentioned previously, one systematic literature review did not find that depression impacted return to work in those with very specific inclusion criteria: nonchronic cases, with nonspecific back pain who never returned to work.26 With more general inclusion criteria, the result may be different. For example, in a large study of 367,900 injured and noninjured workers, injured workers were much more likely (45%) to be suffering from depression than noninjured workers.27
In our study, 84.5% of the workplace had self-report pain, but only 35.5% submitted a WCB claim. In another study of 1,598 injured employees, only 25% of workers with a musculoskeletal injury filed a WCB claim. Factors that impacted the decision to file WCB claims, in comparison to not filing claims, despite the presence of an injury, included shorter employment duration with company, dissatisfaction with coworkers, and lower income.28
Consistent with the evidence, our study found that having an on-site, independent occupational therapist or physical therapist to provide education and advice to stay active, as well as offering return to work with modified duties resulted in a significant reduction in injury claim incidence, duration, and costs.5–15
A limitation to our study is that it only included information until February 3, 2016. Given WCB claims adjudication, it is possible that claims that were originally accepted or rejected could be reversed upon appeal in the following year. Second, although injury severity did not influence outcomes, it is possible that musculoskeletal screening had an influence on outcome through a Hawthorne effect (behavior changes as a result of observation). Third, although this was a prospective study, some information was collected at the same time. For example, we could not determine if job dissatisfaction led to depressed mood or if depressed mood led to job dissatisfaction and so on. Fourth, our study did not include a control group. Finally, only 84.5% of workers completed the voluntary survey.
Conclusion
Independent risk factors associated with WCB claim incidence included depressed mood (OR =2.75, 95% CI 1.44–9.78) and lower job satisfaction (OR =1.70, 95% CI 1.08–10.68). Higher disability duration was independently associated with higher depressed mood (OR =1.60, 95% CI 1.05–4.11) and poor recovery expectation (OR =1.31, 95% CI 1.01–5.78). Higher cost disability claims were independently associated with higher depressed mood (OR =1.51, 95% CI 1.07–6.87) and pain catastrophizing (OR =1.11, 95% CI 1.02–8.11).
In January of 2015, the workplace implemented a new occupational prevention and management program. The injury incidence rate ratio reduced by 58% from 2014 to 2015 (IRR =1.58, 95% CI =1.28–1.94). The ratio for disability duration reduced by 139% from 2014 to 2015 (RR =2.39, 95% CI =2.16–2.63).
In summary, WCB claims are complex. However, it appears that recognizing that nonphysical factors (ie, depressed mood, low job satisfaction, recovery expectations) influence injury claim incidence, recovery, and cost can be helpful to claims management. For example, one systematic literature review suggests that asking a worker about job satisfaction at the start of a WCB injury claim can help identify those at higher risk of delayed recovery and in need of extra attention.6 By accepting this finding, evidence-based occupational programming can have a positive impact on the workplace and its workers.
Disclosure
The author reports no conflicts of interest in this work.
References
Lemstra M, Olszynski WP. The effectiveness of standard care, early intervention and occupational management in Workers’ Compensation claims: Part 2. Spine (Phila Pa 1976). 2004;29:1573–1579. | ||
Lemstra M, Olszysnki WP. The effectiveness of standard care, early intervention and occupational management in workers’ compensation claims. Spine (Phila Pa 1976). 2003;28:299–304. | ||
Frank JW, Brooker AS, DeMaio SE, et al. Disability resulting from occupational low back pain part 2: what do we know about secondary prevention? A review of the scientific evidence on prevention after disability begins. Spine (Phila Pa 1976). 1996;21:2918–2929. | ||
Brewer S, King E, Amick BC, et al. A Systematic Review of Injury/Illness Prevention and Loss Control Programs (IPC). Toronto, ON: Institute for Work and Health; 2008. | ||
Franche RL, Cullen K, Clarke J, et al. Workplace-Based Return to Work Interventions: A Systematic Review of the Quantitative and Qualitative Literature. Toronto, ON: Institute for Work and Health; 2004. | ||
Steenstra I, Irvin E, Heymans M, Mahood Q, Hogg-Johnson S. Systematic Review of Prognostic Factors for Worker’s Time Away from Work Due to Acute Low Back Pain. Toronto, ON: Institute for Work and Health; 2011. | ||
Choi BK, Verbeek JH, Tam WW, Jiang JY. Exercises for the prevention of recurrences of episodes of low back pain. Cochrane Database Syst Rev. 2011;(1):CD006555. | ||
Dahm KT, Bruberg KG, Jamtvedt G, Hagen KB. Advice to rest in bed versus advice to stay active for acute low back pain and sciatica. Cochrane Database Syst Rev. 2010;(6):CD007612. | ||
Heymans MW, van tulder MW, Easmail R, Bombardier C, Koes BW. Back schools for non-specific low back pain. Cochrane Database Syst Rev. 2004;(4):CD000261. | ||
Schaafsma FG, Whelan K, van der Beek AJ, van der Es-Lambeek LC, Ojajarvi A, Verbeek JH. Physical conditioning as part of a return to work strategy to reduce sickness absence for workers with back pain. Cochrane Database Syst Rev. 2013;(8):CD001822. | ||
van Poppel MN, Koes B, Smid T, Bouter LM. A systematic review of controlled clinic trials on the prevention of back pain in industry. Occup Environ Med. 1997;549(12):841–847. | ||
Bell JA, Burnett A. Exercise for the primary, secondary and tertiary prevention of low back pain in the workplace: a systematic review. J Occup Rehabil. 2009;19(1):8–24. | ||
Liddle SD, Gracey JH, Baxter GD. Advice for the management of low back pain: a systematic review of the randomized trials. Man Ther. 2007:12(4);310–327. | ||
Williams RM, Westmorland MG, Lin Ca, Schmuk G, Creen M. Effectiveness of workplace rehabilitation programs in the treatment of work-related back pain: a systematic review. Disabil Rehabil. 2007;29(8):607–624. | ||
Caroll C, Rick J, Pilgrim H, Cameron J, Hillage J. Workplace involvement improves return to work rates among employees with back pain on long term sick leave: a systematic review of the effectiveness and cost effectiveness of interventions. Disabil Rehabil. 2010;32(8):607–621. | ||
Béland Y. Canadian community health survey – methodological overview. Statistics Canada, Catalogue 82-003. Health Rep. 2002;13(3):9–14. | ||
Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. San Antonio, TX: Psychological Corporation; 1996. | ||
Segal DL, Coolidge FL, Cahill BS, O’Riley AA. Psychometric properties of the Beck Depression Inventory-II (BDI-II) among community-dwelling older adults. Behav Modif. 2008;32(1):3–20. | ||
Ware JE, Kosinski M, Keller, SD. SF-36 Physical and Mental Health Summary Scales: A Users’ Manual. Boston, MA: The Health Institute; 1994. | ||
Jensen MP, Karoly P, Braver S. The measurement of clinical pain intensity: a comparison of six methods. Pain. 1986;27:117–126. | ||
Margolis RB, Tait RC, Krause SJ. A rating system for use with patient pain drawings. Pain. 1986;24:57–65. | ||
Sullivan MJL, Bishop SR, Pivik J. The Pain Catastrophizing Scale: development and validation. Psychol Assess. 1995;7(4):524–532. | ||
Worksmart Ergonomics Ltd. Ergonomics Systems Specialist Certification USA. 2015. Available from: www.worksmart.ca | ||
Spitzer WO, Skovron ML, Salmi LR, et al. Scientific monograph of the Quebec Task Force on Whiplash-Associated Disorders: redefining “whiplash” and its management. Spine. 1995;20(8S):1–73. | ||
Rothman KJ, Greenland S. Modern Epidemiology. 2nd ed. Philadelphia PA: Lippincott Williams and Wilkins; 1998. | ||
Iles RA, Davidson M, Taylor NF. Psychosocial predictors of failure to return to work in non-chronic non-specific low back pain: a systematic review. Occup Environ Med. 2008;65:507–517. | ||
Cole DC, Mondloch MV, Hogg-Johnson S. Listening to injured workers: how recovery expectations predict outcomes – a prospective study. CMAJ. 2002;166(6):749–754. | ||
Rosenman KD, Gardiner JC, Wang J, et al. Why most workers with occupational repetitive trauma do not file for Workers’ Compensation. J Occup Environ Med. 2000;42:25. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.