Back to Journals » Drug, Healthcare and Patient Safety » Volume 14
Obstacles and Opportunities in Information Transfer Regarding Medications at Discharge – A Focus Group Study with Hospital Physicians
Authors Glans M , Midlöv P , Kragh Ekstam A , Bondesson Å, Brorsson A
Received 15 February 2022
Accepted for publication 31 March 2022
Published 17 May 2022 Volume 2022:14 Pages 61—73
DOI https://doi.org/10.2147/DHPS.S362189
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Hemalkumar B Mehta
Maria Glans,1,2 Patrik Midlöv,1 Annika Kragh Ekstam,3 Åsa Bondesson,1,4 Annika Brorsson1
1Center for Primary Health Care Research, Department of Clinical Sciences Malmö, Lund University, Clinical Research Center, Malmö, 20213, Sweden; 2Department of Medications, Kristianstad-Hässleholm Hospitals, Kristianstad, Sweden; 3Department of Orthopedics, Kristianstad-Hässleholm Hospitals, Kristianstad, Sweden; 4Department of Medicines Management and Informatics in Skåne County, Region Skåne, Kristianstad, Sweden
Correspondence: Maria Glans, Center for Primary Health Care Research, Department of Clinical Sciences Malmö, Lund University, Clinical Research Center, Box 50332, Malmö, 20213, Sweden, Tel +46-44-3092971, Email [email protected]
Purpose: This qualitative study aimed to investigate experiences and perceptions of hospital physicians regarding the discharging process, focusing on information transfer regarding medications.
Methods: By purposive sampling three focus groups were formed. To facilitate discussions and maintain consistency, a semi-structured interview guide was used. Discussions were audio recorded and transcribed verbatim. Qualitative content analysis was used to analyze the anonymized data. A confirmatory analysis concluded that the main findings were supported by data.
Results: Identified obstacles were divided into three categories with two sub-categories each: Infrastructure; IT-systems currently used are suboptimal and complex. Hospital and primary care use different electronic medical records, complicating matters. The work organization is not helping with time scarcity and lack of continuity. Distinct routines could help create continuity but are not always in place, known, and/or followed. Physician: knowledge and education in the systems is not always provided nor prioritized. Understanding the consequences of not following routines and taking responsibility regarding the medications list is important. Not everyone has the self-reliance or willingness to do so. Patient/next of kin: For patients to provide information on medications used is not always easy when hospitalized. Understanding information provided can be hard, especially when medical jargon is used and there is no one available to provide support. A central theme, “We’re only human”, encompasses how physicians do their best despite difficult conditions.
Conclusion: There are several obstacles in transferring information regarding medications at discharge. Issues regarding infrastructure are seldom possible for the individual physician to influence. However, several issues raised by the participating physicians are possible to act upon. In doing so medication errors in care transitions might decrease and information transfer at discharge might improve.
Keywords: focus groups, medication reconciliation, medication errors, health information exchange, patient discharge summaries, patient discharge
Introduction
Medication discrepancies and medication errors are common in care transitions, including admission to,1,2 and discharge from hospital,2,3 as well as transfer between hospital units.4 These discrepancies and medication errors put patients at risk of adverse events4,5 which may increase the risk of medication-related readmission to hospital.6,7 In 2017, the risk associated with medication safety in care transitions was globally highlighted when the World Health Organization (WHO) initiated its third global patient safety challenge; Medication Without Harm, where care transitions featured as one of three priorities for action.8
On this note, the Swedish National Board of Health and Welfare states the need for medication review among the elderly as well as medication reconciliation and information transfer of medications and medication changes in care transitions.9 The purpose is to ensure fast and accurate updates on drug changes made during a hospital stay as well as adequate follow-up after discharge.
In southern Sweden, where this study took place, the current regional guidelines state that medication reconciliation should be performed in all patients upon admission to hospital.10 A discharge summary with a medication report, which should be comprehensible to a lay person, should be handed to the patient upon discharge.11,12 Its purpose is to inform patients of events occurring during the hospital stay as well as changes made to medications, why these changes were made and the plan for follow-up.11 The discharge summary should also be transferred to the next caregiver along with a medical case history.12 Also included in the discharge summary is a medications list, automatically derived from the electronic medical record.11 This list should be updated before handing the information to the patient and/or sending it to the next caregiver.
It has been shown that writing a discharge summary with medication report, according to these guidelines, and handing it to the patient and next caregiver at discharge can significantly decrease the number of discrepancies between medications lists after discharge.13 Better still, it has also been shown to decrease health care consumption after transition from hospital to primary care.5 Unfortunately, studies show that discharge summaries are often inadequately written and transferred.3,14–16 Even though general practitioners agree that the discharge summary and medication report could be of great value,15 they tend to distrust the information given, especially the medications list.14,15 Similar experiences have been reported in other studies.17–19
Understanding what underlies these problems of suboptimal information transfer regarding medications at discharge could lead to the understanding of how to improve the process. There are some previous studies exploring physicians’ perceptions on the discharging process,17,20–23 however, none including Swedish hospital physicians.
Hence, the aim of this study was to investigate the experiences and perceptions of Swedish hospital physicians regarding the discharging process. The focus was documentation and information transfer of medications and medication changes at discharge.
Methods
Qualitative Approach and Research Paradigm
The goal of the study was to understand the physicians’ experiences of the discharging process, rather than to identify the “true nature” of it. A qualitative design with focus group discussions was used since this is an appropriate method to use when studying experiences.24 In a focus group people who share similar experiences are gathered and discuss their feelings, thoughts, and perceptions on these experiences.25 In addition, focus group participants interact with each other, which can elicit associations and imagination. Thus, the group dynamics contribute to creating stories and adding richness to the material.24,25 The interaction between participants is facilitated by the moderator and the interview guide used and the participants’ thoughts and perceptions are collected and further analyzed to describe the phenomenon under study.25 Qualitative content analysis is suitable for analyzing data from focus groups.24,25
In reporting this study, the Standards for Reporting Qualitative Research (SRQR) were used.26
Researcher Characteristics and Reflexivity
The first author and moderator of the focus group discussions (MG) is a clinical pharmacist with extensive experience in working towards decreasing medication related harm in a hospital environment. MG had not worked regularly with any of the participants before the study but had met some of them briefly in the role of clinical pharmacist and/or educator. MG had no authority over the participants.
Observing the discussions was AB, a general practitioner who has the perspective of the receiving end of information transferred from the hospital at discharge. AB has extensive experience in qualitative research and has been involved in several qualitative studies involving focus group discussions and qualitative content analysis. AB had not previously met any of the participants in the study and had no authority over them.
Reflexivity was maintained throughout the study by the researchers continuously discussing and challenging established assumptions. In addition, both researchers kept reflective notes throughout the study.
Context
The study was conducted at two hospitals in a region in southern Sweden. Hospital 1 is a larger emergency hospital whereas Hospital 2 is a smaller, local hospital.
Electronic Medical Records
The electronic medical records in the regional hospitals are currently separate from those in primary care, which can complicate information transfer at transitions of care. To complicate matters further, nursing care for the elderly, in their homes or nursing homes, is provided by the local municipality using yet another electronic medical record. In elderly patients, especially those in need of home care or living in a nursing home, multi-dose drug dispensing is quite common. This is a system involving machine-packaging of the medications the patient should take at any particular time of day. For these patients, all prescriptions are collected in the Pascal system where changes to prescriptions (initiating medication, changing doses, and discontinuing medication) should also be performed. This system is used by both hospital and primary care physicians, but it is neither connected to the hospital nor the primary care electronic medical record, thus further increasing the risk of medication discrepancies in transitions of care.
Physicians
Graduates from medical school in Sweden do not immediately receive a doctor’s license. This is earned through a supervised internship of 1.5 years during which the intern physicians are stationed at different departments at the hospital as well as in primary, and psychiatric care. Before starting the internship, it is common to work for some time as an unlicensed physician. After earning the doctor’s license, physicians can start their specialist training as a resident physician. The current duration of the specialty training is a minimum of five years.
In this study, resident, and intern physicians (including unlicensed physicians) were selected as participants as they are the ones mainly involved in the discharging process on the healthcare wards.
Sampling
Three focus groups with 4–6 participants per occasion were planned with a fourth to be held in case data saturation was not reached after three.
Initially, interns and residents in both surgery and internal medicine were intended to be included in the study. However, due to the Covid-19 pandemic of 2020, the surgical interns and residents could not attend. Since the focus of the study was documentation and information transfer regarding medication and medication changes, the research team decided that physicians from internal medicine were sufficient as participants.
The sampling strategy was purposive aiming at a mix of male and female interns and residents from the two included hospitals. Resident and intern physicians at the hospitals were informed about the study and invited to participate. The goal was to form focus groups with participants familiar with each other and comfortable with sharing their experiences and perceptions. Hence, the first focus group (FG 1) was formed from those interested and available at Hospital 1 whereas a department secretary in Hospital 2 helped with recruiting and scheduling participants to the second and third groups (FG 2 and 3).
In total 15 physicians, distributed as shown in Table 1, participated in the three focus group discussions. There were 4–6 participants per group. In total 10 female and five male physicians participated.
 |
Table 1 Distribution of Participants in the Focus Group Discussions |
Data Collection
The three focus groups were convened from September through November 2020. The first focus group discussion was held face-to-face in a meeting room at Hospital 1, which was conveniently located for all participants. Due to Covid-19 restrictions physical meetings were not allowed in late 2020 and the remaining two focus groups were held as digital conferences. All the discussions were audio recorded.
The first focus group discussion lasted approximately 90 minutes whereas the second and third lasted approximately 60 minutes. A semi-structured interview guide in Swedish was used to facilitate the discussions and to maintain consistency throughout the focus groups. The guide was based on previous knowledge of problems in the discharging process and started off with the trigger question:
Studies show that primary care physicians do not always trust the information in the discharge summary, especially the medications list. What are your perceptions on the discharging process in general and the documentation of medications and medication changes in particular? What are the obstacles and opportunities as you see it?
The guide included general areas of interest as well as a checklist of specific points and probes to bring up as needed, to ensure that relevant issues were touched upon. Between discussions, the guide was adjusted according to information provided by the participants. However, the general areas of interest were maintained throughout the study. Hence, the development mostly included specifications in the checklist and addition of probes, rather than changes to and/or additions of questions.
Since no new analytical information had emerged after the third focus group discussion, the researchers MG, AB, and PM found that the study provided enough information on the subject, hence sampling saturation was reached.
Data Processing and Analysis
Data from the discussions were transcribed verbatim by a neutral professional transcriber. The transcripts were reviewed by the first author (MG) to ensure that they were accurate and reflected the totality of the discussions, including pauses, punctuations, and non-verbal data. Anonymized transcribed data was used for data analysis. Only the researchers involved in analyzing the data (MG, AB, PM, AKE and ÅB) had access to the raw data.
MG and AB met regularly (via video conference and face-to-face meetings) to review, discuss, and come to a consensus on the material. Through an iterative process of reading, discussing, and rereading the material, preliminary themes were identified and consensually validated. The material was analyzed in order to identify self-standing meaning units relating to the aim of the study. The units or segments were coded and organized into categories throughout the analysis. Furthermore, exemplar quotes illustrating each category were chosen and categories were further explored. Finally, a theme covering the findings of the study was defined. PM, AKE, and ÅB performed a confirmatory analysis which concluded that the main findings were supported by data. Reflective notes were maintained to track the team’s developing thoughts. Examples of the analytical process are shown in Table 2.
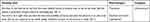 |
Table 2 Examples of the Analytical Process |
Results
The hospital physicians described various obstacles in the course of updating and transferring information on medications at discharge. These obstacles constituted three categories and six sub-categories as shown in Figure 1. Categories and sub-categories are described below with representative quotations.
A central theme emerged during analysis. This theme encompasses how physicians do their best despite difficult conditions. As one physician put it: “I think we need to be humble to the fact that we're only human.” (FG 1)
Infrastructure
IT-Systems
Different Systems
The transfer of a correct medications list at discharge from hospital requires an updated medications list at admission. Participants reported that the fact that hospital and primary care use different electronic medical records makes medication reconciliation at admission difficult. Participants expressed frustration at not being able to easily access the medical records in primary care, or to know if the medications list in the hospital medical record had been updated.
… and then it’s just that we do not have the same medical record as primary care, so we do not know why the patient is prescribed ramipril instead of something else … (FG 1)
The participants expressed the belief that a common electronic medical record would increase patient safety and decrease the risk of medication discrepancies in care transitions. This information would then be immediately available to the primary care physician instead of it being printed, signed, posted and, ultimately, delivered. This procedure can take weeks, according to the participants’ experience.
In patients with multi-dose drug dispensing, hospital and primary care do, in fact, use the same system (Pascal) for prescribing which was considered positive by the participants.
The basis that you are in the same system as the colleagues in primary care facilitates tremendously. You instantly see what they have done, and they instantly see what we have done, and I think this is the main reason why it feels like mistakes are rarer (in these patients). (FG 1)
Complicated Software and Dysfunctional Hardware
There is, in fact, a national system in which one can access primary care medical records from a hospital computer (and vice versa). Similarly, there is a national system in which one can find out the prescriptions patients have filled in the last 15 months. Using these systems requires patient consent and a computer that is available and functions. Hence, doing so was considered complicated and time-consuming by the participants.
It can be tricky … often you try to log in and it does not work, and you have to start over … and that’s annoying. So, I tend to only log in if there is really something … I think it would have been used a lot more if the information had been more organized and readily available. (FG 2)
Physicians expressed hope for future IT-systems to be more accessible and user friendly.
I hope that the goal is to make it as simple as possible. You can incorporate lots of fancy functions but if no one understands how to use them they will not be used. And that’s not why you become a physician; to be able to use computer systems in a flexible way. (FG 2)
Work Organization and Routines
Time and Continuity
Medication reconciliation is not limited to finding out what medications the patient is prescribed. It also includes determining what the patient is actually taking. This requires talking to the patient and systematically going through the medications list, finding out what medications they are taking and how. In the participants’ experience this takes time, which is scarce in the emergency room, leading to medication reconciliation being down prioritized.
… it becomes a matter of medical priority. Sometimes there is a larger medical risk for the patient to wait to be admitted than to state that “I tried to perform a medication reconciliation, but I didn’t have the information needed and I have not been able to access it, this needs more time, and I don’t have that time”. (FG1)
If medication reconciliation is not completed in the emergency room the ward physician should complete it the next day. Unfortunately, the participants’ reported that the ward physicians are also under pressure and have a lot of tasks to perform in a limited amount of time. There is also a lack of physician continuity that complicates things further and makes the daily tasks even more time consuming.
If you had had continuity things would have gone a lot faster and every patient conversation during rounds would have gone faster since you would both know that this was discussed yesterday and there is no need to go through it in detail again today. (FG 2)
In some wards clinical pharmacists help with medication reconciliation. To have another professional, with a different competency and approach, who can thoroughly investigate the patient’s use of medications, was greatly appreciated by the participating physicians.
Imagine having that help in the emergency room, someone with only that task (to perform medication reconciliation). That would be great … (FG 1)
One of the major problems identified by the participants was, in fact, that the medications list used during the hospital stay has discrepancies regarding what the patient was using before admission. Participants expressed concern that this leaves patients at risk of medication related problems.
The major problem, when I am at the ward discharging a patient, is the information from admission. That’s where you find these problems with a previously doubled dose of ACE inhibitor and, at admission, we thought we doubled it. But we have actually just prescribed the same dose as the one they had before admission. (FG 1)
These discrepancies have been there throughout the entire hospital stay leading to further problems at discharge. If this is the medication the patient has received during the hospital stay, should it be continued or changed at discharge? If changed it should be evaluated, and the patient would benefit from staying at the hospital for a few more days. Unfortunately, this is rarely a possibility. Physicians expressed feeling frustrated and crestfallen as they find that there is no real solution to the problems they face regularly.
There is no ground to build on when you sit there with the patient thinking “you are ready to go home”, no genuine ground to build on, and that makes me really sad. (FG 1)
The participants reported that discharge and all that it entails in form of documentation and information transfer is often rushed. This is mainly due to municipal care demanding patients to be discharged at a certain time or a shortage of hospital beds. The participants further reported that many other urgent tasks need to be executed in the wards before lunchtime, leaving them in a position where they must prioritize. They need to choose between taking care of patients in the ward or thoroughly going through documentation to compose a correct discharge summary and medication report.
… you want to do it right when you have the time and possibility, of course, but when the pressure is on, even if we know that we are supposed to do certain things, deviations increase as the pressure is rising. (FG 1)
Documentation and Information Transfer
If medication reconciliation is not completed in the emergency room the admitting physician should make clear to the physician at the ward that the medications list needs reviewing. The routine is that this should be documented in a special note, stating if medication reconciliation is completed – yes/no, in the electronic medical record. However, participants pointed out that this is not always sufficiently done, nor is this note adequately read by the ward physician.
I write yes or no depending on whether I have done it, but my gut feeling is that this note gets lost in the whizz of everything else and that quite a large proportion of my colleagues do not give a da … ignores it, to rephrase … (FG 1)
Participants further conveyed that since this note is not accurately used many physicians report the need for completing the medication reconciliation at the ward in the patient assessment note instead, thus hoping that the ward physician reads it and acts upon it.
To be able to clearly inform patients of changes made to their medications at discharge these changes need to be adequately documented in the medical record throughout the hospital stay. This is especially important since physician continuity is scarce in the wards. Participants reported that it is quite common that patients are discharged by a new attending physician who has never met them. To assemble a discharge information with medication report under those circumstances takes time, especially without distinct documentation of changes made.
The problem as I see it with documenting in the medical record is that the information is hard to find and even if you find it there is nothing confirming that this is the only medication adjustment made. (FG 1)
Hence, participants conveyed that they preferred to use the medications list in the electronic medical record as a source of information when assembling the medication report. Even if this, too, is hard to overview, due to generic changes and long hospital stays, they considered it to provide a clearer picture of medication changes made than notes in the medical record itself.
Many times, follow-up after discharge is needed. If this is the case a referral should be sent to the next caregiver. Unfortunately, participants reported that this is not always sufficiently done, thus risking that the issue is not properly taken care of. Further, they pointed out that it is not always clear to the discharging physician what should be followed-up or by whom.
There is no straight definition regarding what should be taken over by primary care and what you should handle yourself, and the thoughts on this matter differs between colleagues. (FG 1)
Physician
Knowledge and Education
Participants expressed that some of the problems identified regarding documentation and information transfer could be resolved by improving physicians’ education in the IT-systems used. Such education has been incorporated in the internship for some time, but participants expressed concern that education is not always provided for unlicensed physicians, working before their internship. Further, updating knowledge in the IT-systems used is rarely prioritized for more experienced physicians.
In my experience senior colleagues do not get the same continuous education in these administrative tasks, as us newly graduated. Many times, I have experienced that if I am in need of help, with Pascal or adjusting medications, it’s been hard to get that help from a senior colleague. (FG 3)
Failure to provide education is not the only cause for not learning the IT-systems. Participants expressed that lack of motivation is another factor. This is often caused by a sense that there are too many technical tasks to handle.
… but others shut that door in their mind and think that this is not part of my job, and it adds up to there being too many technical tasks to handle … (FG 1)
Further, participants reported that they have experienced a feeling of aversion towards the IT-systems used among fellow physicians. One participant expressed concern that such aversion towards the IT-systems could decrease the motivation to learn how to use them properly, thus jeopardizing medication safety.
Understanding and Responsibility
Since physician continuity is not always possible, information continuity in medical records is vital. To achieve information continuity, it is important that physicians understand the consequences of not following routines concerning documentation. Hence, insight regarding the situation and routines of the next caregiver was considered important by the participants. They believed that if the emergency room physicians were familiar with the routines in the ward, they might be more thorough in going through the medications list before admission. This could decrease the risk of patients receiving medications that, for example, should not be given under the current circumstances.
It’s important to know that when you activate the medications list you prescribe these medications. It’s not an administrative task without a purpose, but rather an important part of the patients’ care for the next 24 hours. And I am afraid our opinions differ on this matter. (FG 1)
Similarly, participants expressed the belief that if the discharging physicians were familiar with the situation and routines in primary care, their documentation and transfer of information regarding medication changes made and follow-up needed might improve.
You know who has never set foot in primary care before working in the hospital. They can easily send referrals phrased “grateful for follow-up”, without a specific question and not including specific information. And that will not be greatly appreciated! (FG 1)
Participants further claimed that physicians need to take responsibility for the medications list and take charge of it. This includes terminating prescriptions that are no longer valid as well as clearing out doublets and generics. Further, indications and instructions about medications should be clarified so that the patients understand them. Making these adjustments would facilitate for the patient as well as for the next caregiver.
The perspective needs to improve so that every physician feels more responsible for the medications list while the patient is hospitalized, preferably already at admission. (FG 1)
However, participants reported that this is not always done, especially by insecure, unlicensed physicians and interns who may not have the self-reliance to make such changes to prescriptions made by others. Further, participants expressed concerns that these inexperienced physicians may sometimes feel reluctant to ask for help from their attending physician.
As a specialist you do not always think to ask “can you handle prescribing medications in the electronic medical record” because then you feel obliged to ask “do you know how to dictate, do you know how to … ” and so on. You presume that they tell you if they do not know, but everyone may not have the courage to do so. (FG 1)
Writing the discharge summary, letting the patient know about changes made to medications and why, was considered important by the participants. However, they expressed concerns that the information given is often inadequate and that some physicians are having trouble using everyday language. They feared that this may cause compliance issues in patients who do not understand why the medications prescribed are important for them to take.
Sometimes I find that we use too much medical jargon so that the patient does not understand, and, at home, they dismiss the information and stop taking the medicine … (FG 3)
Patient/Next of Kin
Providing Information
In compiling information on medications, the patient is often the key source. Unfortunately, in the hospital, patients are not always in a state where they can provide this information in a coherent way. Often, they have low cognitive margins to begin with but even if this is not the case, they are ill and in a stressful situation. The physicians reported difficulties in retrieving correct information on medications from patients under such circumstances.
The patient is not quite there cognitively and that goes for the young who are ill as well as the old. They are in shock, have a fever, feel sick … (FG 1)
Physicians further expressed that, in some cases, the retrieval of a correct medications list is hindered by other factors. Some patients are so reluctant to disturb the staff that they do not tell, even if they receive the wrong medications. Also, some patients are unwilling to admit to bad compliance, risking that important medical decisions are based on false information. Further, according to the participants, some patients simply cannot remember their medications and do not have a next of kin present to assist.
… sure, we have our task in the beginning of the hospital stay, to reconcile the medications list, but sometimes it’s the patient … We need to eliminate this as best we can, but I think we need to be humble to the fact that we're only human. (FG 1)
Understanding Information
In the participants’ experience, even if the discharge summary, medication report, and medications list are correct and informative, the patient does not always understand. Sometimes next of kin can help. However, during the Covid-19 pandemic next of kin were not allowed in the wards, making it harder for the frailer patients.
Before Corona next of kin were sometimes there when I talked to the patient regarding the discharge information, and I think that’s important. Patients are tired, and they can miss information. (FG 3)
The participating physicians pointed out that even if they try hard to simplify information for the patients there are limits to what can be done. Even if multiple generic names are listed on the discharge summary and it is clearly stated on new prescriptions that this medication is to replace another, one cannot control patients’ medication intake after discharge.
It’s a different world out there and prescriptions you fill at the pharmacy can be different from those in the cupboard. That makes it extra important that they get an updated medications list and understand that this is the list to follow. (FG 1)
Discussion
Several obstacles in transferring information regarding medications at discharge were identified. Issues regarding infrastructure are seldom possible for the individual physician to influence. However, several issues described in this qualitative study are possible to act upon. In doing so medication errors in care transitions might decrease and information transfer at discharge, regarding medications and medication changes, might improve.
There are previous studies investigating physicians’ perceptions on the discharging process,17,20–23 some of which report results similar to ours. In 2017 Pinelli et al20 identified five primary barriers in a qualitative study including providers as well as patients. These barriers included system insufficiencies, lack of understanding each other’s roles, information-communication breakdowns, patient-perspective issues, and poor collaboration processes. Similar barriers were identified by Manias et al21 in a qualitative study including patients and family members as well as physicians, nurses, and pharmacists.
Also, in the current study, one of the major obstacles identified was the infrastructure and system insufficiencies. As reported by Pinelli et al,20 system insufficiencies and obstacles related to infrastructure are often out of the physicians’ immediate control. These obstacles can be IT-related, such as poor usability, time-consuming data entry, or inability to exchange health information between electronic medical records.22 They can also be related to routines and work organization, such as inadequate documentation, time scarcity, lack of continuity, and instructions not being understandable to patients.20,21 All these obstacles were also identified by the participants in the current study.
Using different electronic medical records in hospital and primary care was considered a major obstacle by the participants in this study and similar results have been previously identified.15,23 Discrepancies between medications lists in the hospital and those in the primary care electronic medical records are common.3,20,21,23 This calls for performing medication reconciliation at admission to hospital but since time is scarce in the emergency room as well as in the wards, this is not always prioritized.21 Further, as physician continuity is not always possible, and discharges are often rushed, medication reconciliation during the hospital stay or at discharge is not always possible either, as stated by the participants in this study. The fact that discharge, with all that it entails, is often performed by the least experienced physicians is not helping this matter. Hence, discrepancies are often present throughout the entire hospital stay and included in the discharge information27 as experienced by the participants in this study. This poses a risk to patient safety after discharge. Not being able to deliver high-quality care has been previously identified to cause professional dissatisfaction among physicians.22 Similarly, participants in this study expressed feelings of frustration and resignation towards their situation.
General practitioners in the region where this study took place have previously expressed distrust in the discharge summary, especially the medications list.15 They have further reported that their trust would increase if it was stated in the discharge summary that a clinical pharmacist had been involved in medication reconciliation and review during the hospital stay.15
Involving clinical pharmacists in medication reconciliation has been previously identified as an appreciated strategy to improve the discharging process.20,28 Clinical pharmacists are viewed as critical partners to facilitate safe and effective medication management as well as to decrease medication errors and medication related problems.29,30 Participants in the current study similarly expressed appreciation towards clinical pharmacists helping with medication reconciliation and review in the wards. They further wished for expansion of the service presently provided in the included hospitals.
In order to fully reconcile a patient’s medications list, it is important to know what the patient is actually taking.28 Unfortunately, patients are not always well enough to answer questions, not willing to admit to deficient compliance, and not able to remember medications used.20,21 Seeing that the staff is stressed can also render patients unwilling to initiate conversation leading to them not telling, even if they have received the wrong medications.21 Next of kin can sometimes be of assistance but are not always readily available.21 This issue was also reported by participants in the present study. Involving clinical pharmacists in this process could help as patients are often more prone to admit non-adherence to someone other than the physician.28
It has been previously shown that patients often have poor recall of discharge instructions.31 Further, patients have expressed that information given at discharge is often inadequate and hard to understand.17,21,27 This can cause uncertainty and anxiety as well as compliance issues,17,21,27 a concern similarly reported by participants in the present study.
Unintentional, as well as intentional, non-adherence is common after discharge.27 To avoid this, improved communication at discharge is important.27 Again, involving clinical pharmacists could help.16,27,32 In 2016 Daliri et al32 showed that a pharmacist-led transitional care program decreased the amount of medication related problems after discharge. Apart from medication reconciliation at admission and discharge, the program included clinical pharmacists informing patients of medications and medication changes at discharge.32
In the present study, participating physicians raised concerns about not being able to influence what patients are actually taking post discharge. Telephone follow-up or home visits a few days after discharge have been previously identified as ways to bridge the transition from hospital to home.33 Such follow-up appointments, carried out by physicians, nurses, or clinical pharmacists, provides a chance to attend to any patient questions regarding medications or medication changes. This can decrease the risk of adverse events33 and medication related problems.32
It has been previously stated that poor usability of electronic medical records is a prominent source of dissatisfaction among physicians.22 Similarly, participants in this study expressed concerns that the motivation to learn new systems is lacking, especially among the more experienced physicians. Hence, even if the IT-systems in this region improve it is important that physicians’ attitudes toward them also improve and that they learn to use them as best they can. Education needs to be prioritized and continuously updated to achieve better use of the IT-systems used.
Similar to the results of Pinelli et al20 participants in this study identified lack of routines and ineffective communication as obstacles in the discharging process. Routines regarding documentation need to be distinct, known and, ultimately, followed by all. Further, physicians must be aware of and understand consequences that result from them not following these routines.
As identified by the participants in this study, not understanding each other’s roles or work situations can lead to duplication of work or failure to complete pertinent tasks.20 Hence, being able to put yourself in the next caregivers’ shoes and see the next step in the patient’s continuous care is essential if wanting to improve the discharging process. In doing so information continuity could be improved and the risk of adverse events in transitions of care might decrease.
Strengths and Weaknesses
We used several techniques to enhance trustworthiness in this study:
Prolonged engagement was applied as we (MG and AB) used a semi-structured interview guide based on previous knowledge of problems in the discharging process. Using this guide, we asked the participants several distinct questions regarding topics related to discharge. We also asked follow-up questions and encouraged participants to support their statements with examples.
Persistent observation was secured as we (MG and AB) initially read and reread the data and analyzed the focus group discussions independently after which we compared interpretations. If interpretations differed, they were discussed until the most suitable interpretation was found, which best represented the meaning of the data. We (MG and AB) met regularly throughout the process of the study and minutes from these meetings were reflected upon as was the development of the study.
Investigator triangulation was applied by including researchers with differing research backgrounds and data triangulation was secured as the various datasets that emerged throughout the analysis process, i e, the raw material, preliminary themes and codes, and reflective notes, were all used for analysis.
Another strength in this study was including participants with recent experience from working with admission and discharge of patients. With the processes and perceived obstacles fresh in their minds, the participating physicians were well suited to contribute to a rich material.
The fact that the first focus group consisted of residents only whereas the other two groups included interns as well could be considered a strength as well as a weakness. The overall sense was that the first focus group resulted in a thicker material, which could be due to the participants in the first focus group being more experienced. However, it could also be because the first discussion was conducted face-to-face whereas the second and third focus groups were conducted as digital conferences. The digital conference environment can be inhibiting but was, unfortunately, a must due to the Covid-19 pandemic.
Physicians from surgical specialties did not participate in this study which may, perhaps, have influenced the results. However, since the processes of medication reconciliation and transfer of information in care transitions are the same regardless of specialty, we believe that the results of this study are transferable to all specialties as well as to similar contexts.
Conclusions
There are several obstacles in the course of transferring information regarding medications at discharge. Issues regarding infrastructure, such as suboptimal IT-systems, time scarcity, and lack of continuity, are seldom possible for the individual physician to influence. However, several issues raised by the physicians participating in this qualitative study are possible to act upon. Establishing routines and making sure they are known and followed by all could, possibly, help improve information continuity. Further, providing, and prioritizing education in IT-systems used and making sure physicians take responsibility for the medications list could, possibly, help decrease medication errors and improve information transfer at discharge. Involving clinical pharmacists could be of great value in these activities. Further studies are needed to verify these hypotheses.
Abbreviation
WHO, World Health Organization.
Data Sharing Statement
The data that support the findings of this study are available from the corresponding author on reasonable request. The data are not publicly available due to privacy or ethical restrictions.
Ethics Approval and Informed Consent
The study was performed in accordance with the Declaration of Helsinki.33
Ethical approval was applied for at the Swedish Ethics Review Authority. The Swedish Ethics Review Authority assessed that ethical approval was not required since the study did not include any intervention covered in the Swedish Ethics Review Act. The advisory remark from the Ethics Review Authority (Registry number 2020-01581) stated that there were no ethical objections to the study.
Informed consent, including consent for publication of anonymized responses, was obtained from all participants. To ensure that participants were fully aware of what their participation implied (i e the risks and benefits associated, the steps and precautions taken to minimize risks and the plan to use the data), they were asked to read an information letter describing these things before signing the informed consent form. Participation was voluntary and the collected data cannot be linked to the participants.
Acknowledgments
We would like to thank the physicians who chose to take part in the focus group discussions for their time and contribution. We are further indebted to Patrick Reilly for his expertise and advice in editing the manuscript, to Lena Lennartsson for transcription of the raw data, and to Jazmin Rosberg Tomasino for helping out with sampling and scheduling participants at Hospital 2.
Funding
This study was supported by a grant from the ALF funding from Region Skåne, awarded to PM. The study was further supported by grants from FoU Kryh and Södra Sjukvårdsregionen, awarded to MG. The funding body had no role in the design of the study, the collection, analysis, or interpretation of data or in writing the manuscript.
Disclosure
Mrs Maria Glans reports grants from FoU Kryh, grants from Södra sjukvårdsregionen, during the conduct of the study. The authors declare that they have no competing interests.
References
1. Tam VC, Knowles SR, Cornish PL, Fine N, Marchesano R, Etchells EE. Frequency, type and clinical importance of medication history errors at admission to hospital: a systematic review. CMAJ. 2005;173(5):510–515. doi:10.1503/cmaj.045311
2. Midlov P, Bergkvist A, Bondesson A, Eriksson T, Hoglund P. Medication errors when transferring elderly patients between primary health care and hospital care. Pharm World Sci. 2005;27(2):116–120. doi:10.1007/s11096-004-3705-y
3. Caleres G, Modig S, Midlöv P, Chalmers J, Bondesson Å. Medication discrepancies in discharge summaries and associated risk factors for elderly patients with many drugs. Drugs Real World Outcomes. 2020 Mar;7(1):53–62. doi:10.1007/s40801-019-00176-5
4. Lee JY, Leblanc K, Fernandes OA, et al. Medication reconciliation during internal hospital transfer and impact of computerized prescriber order entry. Ann Pharmacother. 2010;44(12):1887–1895. doi:10.1345/aph.1P314
5. Midlov P, Deierborg E, Holmdahl L, Hoglund P, Eriksson T. Clinical outcomes from the use of medication report when elderly patients are discharged from hospital. Pharm World Sci. 2008;30(6):840–845. doi:10.1007/s11096-008-9236-1
6. Witherington EM, Pirzada OM, Avery AJ. Communication gaps and readmissions to hospital for patients aged 75 years and older: observational study. Qual Saf Health Care. 2008;17(1):71–75. doi:10.1136/qshc.2006.020842
7. Ekerstad N, Bylin K, Karlson BW. Early rehospitalizations of frail elderly patients - the role of medications: a clinical, prospective, observational trial. Drug Healthc Patient Saf. 2017;9:77–88. doi:10.2147/DHPS.S139237
8. Donaldson LJ, Kelley ET, Dhingra-Kumar N, Kieny MP, Sheikh A. Medication without harm: WHO’s third global patient safety challenge. Lancet. 2017;389(10080):1680–1681. doi:10.1016/S0140-6736(17)31047-4
9. Swedish National Board of Health and Welfare. Directives and general advice on prescription and handling of medicines in health care. 2017.
10. Department of medicines management and informatics in Skåne county. Directions for medication reconciliation and review in Skåne County. Region Skåne; 2014.
11. Department of Medicines Management and Informatics in Skåne county. Discharge summary guidelines. Region Skåne; 2013.
12. Department of medicines management and informatics in Skåne county. Routine and guidance for collaboration at discharge from hospital care. Region Skåne; 2020.
13. Midlov P, Holmdahl L, Eriksson T, et al. Medication report reduces number of medication errors when elderly patients are discharged from hospital. Pharm World Sci. 2008;30(1):92–98. doi:10.1007/s11096-007-9149-4
14. Caleres G, Bondesson Å, Midlöv P, Modig S. Elderly at risk in care transitions When discharge summaries are poorly transferred and used –a descriptive study. BMC Health Serv Res. 2018;18(1):770. doi:10.1186/s12913-018-3581-0
15. Caleres G, Strandberg EL, Bondesson A, Midlov P, Modig S. Drugs, distrust and dialogue -A focus group study with Swedish GPs on discharge summary use in primary care. BMC Fam Pract. 2018;19(1):127. doi:10.1186/s12875-018-0804-8
16. Kogut SJ, Goldstein E, Charbonneau C, Jackson A, Patry G. Improving medication management after a hospitalization with pharmacist home visits and electronic personal health records: an observational study. Drug Healthc Patient Saf. 2014;6:1–6. doi:10.2147/DHPS.S56574
17. Hesselink G, Schoonhoven L, Plas M, Wollersheim H, Vernooij-Dassen M. Quality and safety of hospital discharge: a study on experiences and perceptions of patients, relatives and care providers. Int J Qual Health Care. 2013;25(1):66–74. doi:10.1093/intqhc/mzs066
18. Robelia PM, Kashiwagi DT, Jenkins SM, Newman JS, Sorita A. Information transfer and the hospital discharge summary: national primary care provider perspectives of challenges and opportunities. J Am Board Fam Med. 2017;30(6):758–765. doi:10.3122/jabfm.2017.06.170194
19. Kripalani S, LeFevre F, Phillips CO, Williams MV, Basaviah P, Baker DW. Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007;297(8):831–841. doi:10.1001/jama.297.8.831
20. Pinelli V, Stuckey HL, Gonzalo JD. Exploring challenges in the patient’s discharge process from the internal medicine service: a qualitative study of patients’ and providers’ perceptions. J Interprof Care. 2017;31(5):566–574. doi:10.1080/13561820.2017.1322562
21. Manias E, Gerdtz M, Williams A, Dooley M. Complexities of medicines safety: communicating about managing medicines at transition points of care across emergency departments and medical wards. J Clin Nurs. 2015;24(1–2):69–80. doi:10.1111/jocn.12685
22. Friedberg MW, Chen PG, Van Busum KR, et al. Factors affecting physician professional satisfaction and their implications for patient care, health systems, and health policy. Rand Health Q. 2014;3(4):1.
23. Jones CD, Vu MB, O’Donnell CM, et al. A failure to communicate: a qualitative exploration of care coordination between hospitalists and primary care providers around patient hospitalizations. J Gen Intern Med. 2015;30(4):417–424. doi:10.1007/s11606-014-3056-x
24. Malterud K. [Qualitative methods in medical research: An introduction]. Studentlitteratur; 2014. 3. Language: Swedish.
25. Moser A, Korstjens I. Series: practical guidance to qualitative research. Part 3: sampling, data collection and analysis. Eur J Gen Pract. 2018;24(1):9–18. doi:10.1080/13814788.2017.1375091
26. O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med. 2014;89(9):1245–1251. doi:10.1097/ACM.0000000000000388
27. Knight DA, Thompson D, Mathie E, Dickinson A. ‘Seamless care? Just a list would have helped!’ Older people and their carer’s experiences of support with medication on discharge home from hospital. Health Expect. 2013;16(3):277–291. doi:10.1111/j.1369-7625.2011.00714.x
28. Vogelsmeier A, Pepper GA, Oderda L, Weir C. Medication reconciliation: a qualitative analysis of clinicians’ perceptions. Res Social Adm Pharm. 2013;9(4):419–430. doi:10.1016/j.sapharm.2012.08.002
29. Gillespie U, Alassaad A, Henrohn D, et al. A comprehensive pharmacist intervention to reduce morbidity in patients 80 years or older: a randomized controlled trial. Arch Intern Med. 2009;169(9):894–900. doi:10.1001/archinternmed.2009.71
30. Schnipper JL, Kirwin JL, Cotugno MC, et al. Role of pharmacist counseling in preventing adverse drug events after hospitalization. Arch Intern Med. 2006;166(5):565–571. doi:10.1001/archinte.166.5.565
31. Foust JB, Vuckovic N, Henriquez E. Hospital to home health care transition: patient, caregiver, and clinician perspectives. West J Nurs Res. 2012;34(2):194–212. doi:10.1177/0193945911400448
32. Daliri S, Hugtenburg JG, Ter Riet G, et al. The effect of a pharmacy-led transitional care program on medication-related problems post-discharge: a before-after prospective study. PLoS One. 2019;14(3):e0213593. doi:10.1371/journal.pone.0213593
33. Kripalani S, Jackson AT, Schnipper JL, Coleman EA. Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists. J Hosp Med. 2007;2(5):314–323. doi:10.1002/jhm.228
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

