Back to Journals » Open Access Emergency Medicine » Volume 8
Objective triage in the disaster setting: will children and expecting mothers be treated like others?
Authors Kouliev T
Received 23 September 2015
Accepted for publication 8 March 2016
Published 27 October 2016 Volume 2016:8 Pages 77—86
DOI https://doi.org/10.2147/OAEM.S96913
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Hans-Christoph Pape
Timur Kouliev
Beijing United Family Hospital, Beijing, People's Republic of China
Abstract: The study of disaster triage is made difficult by the complex emotional response of potentially lifesaving intervention that a triage officer must make basing decisions on a succinct and efficient algorithm. A survey of triage professionals in international settings was designed to identify possible emotionally led bias that affects objective decision making in identifying victims most likely to benefit from immediate life support intervention. This survey suggests a lack of correlation between triage priority and predictable clinical outcomes as predicted by the Revised Trauma Score tool. Among the subjects, it was observed that a pediatric victim is uniformly overtriaged when compared to less injured victims.
Keywords: triage, disaster triage, emotional bias, pediatric trauma, obstetric trauma, People's Republic of China
Introduction
The study of triage has been at the core of disaster medicine since its roots in wartime necessity and has been transferred to general population tools when resources are limited in challenging times.1 Despite considerable uncertainty and academic interest, practical investigations into the field of disaster triage have been limited and have yielded few clear conclusions, and at present, the validated framework for prioritizing treatment and transport of injured patients remains the focus of theory and speculation (a good overview of the triage types is presented by Ireson and Moskop2). A typical framework describes a five-stage triage process:
- Stage 1. Sort, can the patient walk, move, or are they unconscious?
- Stage 2. Assess spontaneous breathing? Start lifesaving interventions.
- Stage 3. Assess respiration rate.
- Stage 4. Assess perfusion.
- Stage 5. Assess mental status.
At the end of this assessment, patients can be categorized as minor (green tagged), delayed (yellow tagged), immediate (medical care required, red tagged), or expectant (death expected, black tagged).3
Among the key challenges is that the adopted triage system must be robust to render decision making more objective and less prone to emotion and bias. It is reasonable to seek objectivity in triage decisions to maximize individual and public health benefit in the acute chaotic setting, thus optimizing health care resource allocation and delivery to the greatest number of affected individuals.
Although a large body of literature has now been published on disaster triage, the practical reliability of prehospital triage has been studied infrequently. Most of the research addressing the Futility and success of triage has been done using tabletop scenarios rather than being done in the field and has generally noted a poor correlation with clinical outcomes with an accuracy of only 45%–55%.4 In trying to identify and validate a triage tool, various algorithms have been utilized. Simple Treatment and Rapid Transport (START), Jump START, Care Flight Triage, Triage Sieve, Sacco Triage Method, Secondary Assessment of Victim Endpoint (SAVE), and Pediatric Triage Tape1 are among the more accepted techniques; however, no one method has gained substantial evidence to prove its superiority over the others.5
START triage has emerged as the most frequently used system worldwide due to its simplicity, its intuitive and easily adaptable nature, and in part its capacity to be taught to providers quickly.6 In one of the initial studies to quantify the effectiveness and reliability of START triage in a real disaster scenario, Kahn et al7 were successful in demonstrating a relatively poor correlation of START triage and outcomes. When discussing a gold standard for disaster triage, Cone and Koenig8 concluded that START is far from convincing as a framework. With its effectiveness unproven, it is presently unclear to what extent and how reliably START can be used in a real disaster setting or in training exercises.7
The failure of disaster triage algorithms may be attributed to the complex decision-making process that needs to fit into a concrete and objective set of guidelines. Individuals performing triage have the ability and responsibility to make lifesaving decisions within 2–5 minutes,5 based on limited information. If much of triage is then done on emotional or other subjective grounds, personal interpretation rather than adherence to the objective criteria may likely become the guiding impulse and thus the source of error and failure of proper allocation of resources.
In identifying risks of emotional bias, triage priority allocation may be particularly problematic for specific patient groups and interfere with effective triage.9 This is especially notable for children, where distinct disaster triage strategies have been proposed. For any disaster patient, it has been observed how difficult it is for disaster medicine students to assign an adult victim a black card (too sick to resuscitate) next to others projected to survive (tagged red, yellow, or green) in simulated case scenarios.10 Assigning a black card to a child is still more difficult, as supported by the longer duration of code times when comparing pediatric resuscitation times to those of adults in nondisaster settings.11 The researchers suspect this to be partly due to a powerful emotional response toward children and partly due to a lack of training and experience triaging children in settings that may be overwhelming.
Methodology
This study examined the correlation between predicted quantifiable outcomes of disaster trauma patients, both adults and children, and the willingness of triage providers to assign them limited health care resources. Experienced emergency room (ER) nursing triage providers with similar training and backgrounds were surveyed in three metropolitan hospitals, although no nurses surveyed had appreciable or specific disaster medicine triage experience. A separate questionnaire was designed with six victims of a significant road traffic accident, which overwhelmed the resources of a local health care delivery system. The adult and pediatric disaster triage was examined; the extent of the problem was addressed by comparing the two populations; and guidelines were proposed to account for this problem in future research and clinical practice.
Chicago, Philadelphia, and Beijing were selected as the sites of study because they were the principal investigator’s primary places of work. The hospitals included a private urban, private suburban, and private Western-style hospital in these respective cities. The surveys were distributed in the course of clinical shifts and collected on the same workday at the end of the shift. A total of 63 subjects were enrolled in this study, 31 in Chicago, 18 in Philadelphia, and 14 in Beijing.
The training of nurses in the hospital in Beijing is designed to closely reflect nursing training in the US. The hospital is Joint Commission Accredited with standardized required procedures for infection control and error prevention. All emergency nurses are required to be Basic Life Support (BLS), Advanced Cardiovascular Life Support (ACLS), and Pediatric Advanced Life Support (PALS) certified. There is also basic obstetric training as the hospital is an obstetrics referral hospital. There are two yearly disaster drills at the hospital, one of which is a full-scale drill, where nurses are required to participate. Overall, nursing training is closely reflective and modeled after training received in US hospitals. Although some nurses receive specialized trauma training in both countries, trauma certification is not a requirement to work in either of the listed emergency departments. The ages and years of clinical experience of the nurses in the three sites were comparable.
All three centers care for children in the emergency departments, and nurses have specific training and experiences in triaging and managing for pediatric patients. The volume of pediatric patients differs slightly and represents 20%–30% of the total in the US hospitals and close to 50% of the ER volume in Beijing, possibly reflecting the contemporary characteristics of family and private health care in the People’s Republic of China.
Although there are appreciable and important fundamental differences between disaster triage and ER triage, ER nurses were selected for this study as they had the most experience for triage among any health care providers, physicians included, in the specific hospital settings where the work was conducted. In an attempt to address the gap in familiarity with disaster-specific triage experience for many of the emergency nurses, a standard verbal introduction of the START triage tool was taught by the investigator, followed by the distribution of a START triage reference sheet that was available to each of them during the completion of the survey (Figure 1). The nurses had the reference sheet as a reference, but as with any tool, it was not possible to ensure that they used the triage tool exclusively for the making of triage decisions. The surveys were unmarked and anonymous, and the results were hidden and folded prior to being returned to the primary investigator. Nurses were specifically asked to complete the surveys without consulting with their colleagues. The study’s subjects were blinded to the premise of the study, which was to examine the effect that emotional response to childhood and pregnancy may have in the selection of victims of a mass casualty incident (MCI).
  | Figure 1 START: Simple Triage and Rapid Treatment algorithm. |
The surveys, specially designed for the purposes of this study, consisted of two scenarios where a bus collided with a train and resulted in six victims between 4 years and 55 years of age being critically injured. In the first of the two scenarios, unlimited resources were available to transport the six patients to a trauma center, while in the second scenario, only two ambulances/teams were available for transporting victims to care. Therefore, triage nurses were asked to triage only two patients as “Red” and the remaining four victims had to be automatically triaged as “Black” (Table 2). The first scenario was used to create a control and ensure that all the patients were triaged as red in the setting of unlimited resources. Only one responder between the three hospitals marked a victim in the first scenario as black. That responder’s reply was not used in the final results. All other victims were triaged as red.
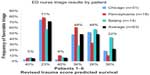
The victims were designed especially for the survey, and their predicted calculated probability of survival was devised using the Revised Trauma Score (RTS), a validated clinical outcome prediction tool.12,13 The victims were designed to have a predicted survival to be in the range of 36%–40%, based on the criteria described by RTS. This is illustrated in Figure 2. In contrast, the pediatric victim’s chance of survival was specially designed to be just over 20%, while the pregnant patient’s survival was calculated at 25%. Triage nurses were not aware of the chance of survival of each patient or of the criteria for the design of each victim.
  | Figure 2 Survival probability by revised trauma scale. |
Prior to the survey being administered, bias in the formulation of clinical vignettes was considered, and the survey was submitted to a panel of the specialty’s top disaster medicine experts. Their opinions were incorporated into the phrasing and presentation of the vignettes.
Using the methodology upon which this study was designed, there was no interaction with real patients while the study was being administered, and Institutional Review Board approval was not formally sought, although this would change with future expansion of the study. Written approval for the study was received from the nursing leadership and the ER directors of all three practice settings in Chicago, Philadelphia and Beijing.
Although the START triage algorithm was recommended and introduced, triage professionals used it at their discretion, the result being not a study of START triage but of MCI triage in general. For this reason, the following study results could be considered appropriate in whichever triage system may be used, although it should be noted that firm conclusions await a larger sample size than were able to be returned by this study.
Results
A lack of correlation was demonstrated between the assigned triage card and the predicted outcome, which was particularly notable for the pediatric victim.
The study results are summarized in Table 1 and Figure 3. Table 1 presents the chance of survival of six patients using the RTS prediction tool and how often the patient was selected to be resuscitated in preference over the other five with the results separated by city. The numbers add up to 200% as two patients were selected.
  | Table 1 Survival chance of six patients and frequency of preferable selection |
  | Figure 3 Frequency of preferable selection in triage by patient and center. |
The six columns in Table 1 demonstrate the relative selection of the six victims, which is further divided between the three sites. The chance of survival, calculated by the RTS, is listed at the base of the column for each patient. The results for the 4-year-old critically injured victim are in column 2, and those for the critically injured pregnant patient are in column 4.
High response rates were achieved as each distributed survey was followed up personally and collected prior to completion of the clinical shift. No subject refused to participate in the survey. The response rates were 100% in Philadelphia and Beijing and 97% in Chicago, due to one survey being filled in incorrectly.
Overall, in this small sample, there appears to be little between triage severity and the predicted survival rate, as has been observed in previous studies.7 Particularly noticeable is the fact that the child was selected by 71% of responders despite having the lowest chance of survival by RTS (~20%). Patients #4 (OB) and #5 had similar overall chances of selection, despite the probability of survival by RTS being significantly lower for patient #4 (~25%). A greater number of patients, followed by a statistical analysis, would be required to see if such a trend is indeed statistically significant.
Although the study was not designed or powered to account for the different geographic and cultural practice environments, it is interesting to note a trend toward disagreement on appropriate triage of patients #4–6. Based on the case description, patient #6 is the only patient with penetrating injuries, while #5 had predominantly upper airway compromise. Patient #6 was selected far more frequently in Beijing (43% vs 22%/11%), while patient #5 was most often transported in Philadelphia (61% vs 48%/28%). The implication of these results merits further investigation in studies dedicated to cross-cultural perception of disaster injury severity and triage.
Discussion
Disaster management of pediatric victims has been identified as a component of planning and training that is missing from many protocols and education programs.14 It is suggested that up to a third of all MCIs have at least one pediatric victim.15 The results highlight the difficulty in comparing and weighing the relative values of resuscitation in adults and children, especially when these two patient groups compete head-to-head for resources.
It has been previously highlighted that disaster triage in adults and children was like comparing two completely different groups of patients, and differing triage systems for the two populations have been proposed.16 Although these tools have attempted to account for differences that are intrinsic to pediatric triage needs, none of these tools have been found to have adequate sensitivity or specificity to justify their use, and additional complexities have arisen when administering two algorithms simultaneously. Among the best known tools, Romig proposed Jump START as a modification of the previously accepted START triage,17 but despite the triage tool being incorporated into practice by several centers and providers in the last decade, it has thus far not been validated. Moreover, its use has at times been shown to be inferior to others pediatric triage tools available.1 Still, in the case of a large number of pediatric victims, or a combination of many pediatric and adult patients, these strategies may have merit, and disaster experts continue to use Jump START awaiting better studies aimed at validating or disproving its use.
In the cases where one or a few children are involved, a unified triage strategy can often be more practical and easier to use in the field, as every additional protocol, used in an already unusual or stressful scenario, reduces the chance that any protocol would actually be used correctly. The team responsible for managing the July 7, 2005, London bombings expressed the opinion that a simplified P1–4, in some ways similar to START, contributed to the effective triage process and low critical mortality.19 Although START has not been shown to improve outcomes per se, it was shown to be as equally predictive in children as other tools in the pediatric populations,1 and it has, therefore, been chosen as the unifying triage strategy for the purposes of this study.
The 4-year-old victim, despite having a far lower chance of survival, was selected by the vast majority of triage professionals, who were blinded to the study’s intent. This result gives some support for failure of objective triage criteria when confronted with an unusual or potentially emotional scenario. Although the survey environment is but an imitation of the decision-making environment in a real disaster setting, the results of the study call attention to triage professionals’ need to be more aware and self-critical of their decisions, even when working under a triage protocol.
There are several potential reasons for failure of triage professionals to select the individuals with the highest probability of survival.2 First is the possibility that prioritizing the individuals by probability of survival is fundamentally different from the way that health care providers really assess treatment priority. Instead, it is possible that years of life gained and/or quality of life may be perceived to be a better and more appropriate reflection of triage priority than the chance and time to loss of life or limb. Not surprisingly, it shows that it is particularly difficult to discern what goes into the triage decision-making process in severely injured patients.20 According to Chang et al21 and Scheetz et al,22 there is evidence that undertriaging of the elderly takes place in disaster scenarios, and it may not be overly surprising that there would be a natural tendency of decisions of triage professionals to benefit young patients.
The second probable reason that triage benefits children is the lack of providers’ experience and comfort with pediatric disaster triage.9 Invariably, health care professionals will have had less experience with children than with adults when mixed disaster settings arise, and this may, in turn, result in decisions being more subjective and less based on physiological parameters or survival prediction scores.
The third and potentially major explanation is that triage is inherently an emotional decision, and even the most rigorous attempts to standardize it will fail on some level.23 When faced with a sick child and in the absence of specific and clear triage guidelines for every setting, individuals have every impulse to “save” the child, rather than choose between the adult patients who might each have an objectively higher chance of survival.23 Even with proper validating triage tools, it would be impossible to protect fully against this tendency, although the creators of pediatric disaster triage have on some level recognized it and addressed ways that aimed to reduce it. Different health care providers may have different tendencies for emotional bias. Notably in this study, all subjects are nurses, and >90% are female. Although the study was not designed to identify triage differences between men and women, doctors or nurses, or between single and married individuals with children, such differences can potentially affect the subjective component of the decision and merit further research in order to design effective triage strategies.
Whether children should receive special resuscitative efforts in lieu of an adult who may have a higher chance of survival may be a valid conclusion and recommendation. That is especially true if survival is weighed against quality or life and/or years of life gained. At the same time, overtriaging, whether in pediatric or adult medicine, has been associated with increased mortality among critical patients.24 A greater number of pediatric victims may be expected to lead to massive overtriage and further strain the limited resources. However, outcomes of disaster events based on pediatric overtriage have not yet been investigated.25
Importantly, although the START triage model was given to the subjects, they were not required to use this protocol in their decision-making process. The subjects could have merely selected which two patients would receive care and which four would not, and the bias demonstrated in this study calls attention to disaster triage as a whole process with its inherent limitations.
Compared to overtriage of the pediatric victim, the choice to transporting the obstetric victim was much less uniform. This patient was still overall transported more frequently than would be expected from her chance of survival alone; nevertheless, several of the other adult victims were treated comparably. The decision to design this patient to be ~32 weeks of gestation was made due to the realistically visible gravid in the field, while still perhaps viewing the patient as one victim rather than two. The decision whether to view her as one victim or two, however, is taken individually by the triage provider. The emotional and objective decision in treating a mother and fetus together or separately was not examined further in the scope of this study. Due to probable personal and cultural differences in perception, the results suggest that this decision is far from uniform among the triage subjects and geographic sites in this study.
Some other geographical differences are notable and require further culture-specific research before conclusion can be made. For instance, in Beijing, there was a far higher selection of patient #6 (graph), who suffered hemodynamic and respiratory compromise due to penetrating injury, the only victim having this profile. This finding may reflect the relative rarity of penetrating injury in Beijing due to the very low rates of penetrating violent knife and gun crime resulting in differences in emotional perception and/or less experience in judging the chance of survival and suffering.
Limitations
The limitations of the study relate to a significant extent to the use of the RTS, survey design and administration, and the intrinsic aspects of the START protocol.
RTS consists of a weighted score combining patients’ vital signs parameters. It does not address mechanism of injury, circumstances, or preexisting conditions.12 It may be argued whether RTS, an “adult” trauma score, is appropriate for predicting outcomes in pediatric patients, especially in a disaster setting.22 Several models have been used to predict outcomes in pediatric trauma patients, but few have been used in both adults and children as they were not designed to compare the survival. For this reason, RTS was chosen as the ideal method for this study, so it could be used for comparison. The results of the research by Nayduch et al26 demonstrate that RTS, in fact, is a useful method of predicting outcome in pediatric trauma. Nonetheless, the limitations of this method need to be recognized.
As there is only one child in this study, the selection of this child may not reflect the selection across a group of pediatric victims. Although the child in the study has multiple failing systems, the neurological injury appears particularly severe. However, survival after severe head trauma has been shown to be significantly better in children than in adults with equivalent findings.27 Feickert et al24 demonstrated a mortality rate as low as 22% with severe head injury in children, although the survivors generally had severe neurological damage on discharge. The child in this scenario had a Glasgow Coma Scale of 3, and much of the decrease in the RTS calculated score was due to neurological impairment, making his survival arguably better than the 20% predicted by RTS. However, for the worst head injuries, the work by Pillai et al28 demonstrated that a Glasgow Coma Scale of 3–5 remains a predictor of poor clinical outcome in the setting of trauma, regardless of the age.
It is concluded that despite these limitations, RTS remains one of the few available options to compare survival of pediatric and adult patients in surveys and tabletop disaster scenarios. Although small differences in predicted survival probability may not be apparent in triage, a markedly decreased RTS is not consistent with marked pediatric overtriage that was demonstrated in this study.
The results of this study are susceptible to bias inherent to observational study design. There were a limited number of victims, created as part of the survey. Although every effort was made to compare chances of survival head-to-head, the study’s simplicity depended on there being only one child and one gravid victim. The wording of the vignettes was created by medical doctors and may not necessarily reflect the wording that nurses undertaking triage would use in similar circumstances. Nonetheless, every effort was made to be objective in the design and wording of the vignette, which emphasized factual and where possible quantitative data. Still, when dealing with complex disaster decision-making scenarios, bias inherent to observational study design cannot be avoided despite a rigorous methodology and expert reviews.
Subject selection was chosen for competency and facility of survey administration, even though ER triage nurses differ from prehospital providers in disaster settings. The study was not designed to differentiate decisions of prehospital providers, field physicians, paramedics, or hospital emergency physicians. By limiting the subjects to triage nurses, the surveyed population was largely dominated by female full-time staff. Men or women were not specifically chosen for the study, but their numbers reflected the staff working in the ER, the large majority of whom were females at all three sites.
As in several previous studies involving disaster triage, the effectiveness of START should be called into question, as the technique has yet to be validated.6 Most recently, Kahn et al7 failed to validate START triage in a real disaster scenario. His study demonstrated poor agreement between initial triage level and clinical outcome, especially true for critical patients who were the focus of this study. Therefore, using START is bound to have limitations, yet this study’s methodology was not designed to differentiate between failure of START and failure by personnel to apply it consistently or correctly. Designed as an intention-to-treat analysis, the study did not include a goal to determine the reasons or process for assignment of triage designations. Instead, the START framework was used as a recommendation, as it is frequently done in real disaster settings. The final decisions of the caregivers are based invariably on applying the framework in their own way, which would be the case with any guidelines used.
Having considered introducing a separate pediatric tool, a second triage protocol was not chosen for distribution in order to decrease complexity of administration, facilitate decision making, and decrease bias. Some researchers would indicate that START triage protocol is not intended to be applied to children,7 but START triage has been used in pediatric disaster settings and has not been demonstrated to be either more or less effective when compared to other tools for managing children in disaster settings.1 For the purposes of this study, use of START as just one of the acceptable frameworks is considered, one as legitimate as Jump START or an alternative pediatric tool that may serve as the framework of triage professionals’ consistent decision making (Figure 4). Moreover, it was judged that for the purposes of this survey, the distribution of the Jump START protocol would have added confusion to the survey responders due to the amount of information and possibly unblinded as to the purpose of the study. It should be noted that an equivalent to such a tool is not available to the best of the investigator’s knowledge for obstetric patients.
  | Figure 4 JumpSTART algorithm. |
Conclusion
In this study, triage professionals were surveyed regarding their disaster triage of patients, standardized by their probability of survival using validated clinical scores. The results suggest that despite a lower likelihood of survival, triage nurses in three international centers consistently distributed scarce health care resources to benefit the sole pediatric victim. Despite limitations of such a survey methodology, the trend for favorable triage of a more critically injured pediatric victim remains striking. A less consistent selection trend was also noted for an obstetric patient in her third trimester. Possible interpretations include limited experience in triaging dying children, prioritization of factors other than survival, or an emotional response on the part of triage professionals. If that is the case, in the absence of significant other mechanisms for the measurement of emotion in triage, increased allocation of resources despite objective evidence of futility may be a useful indirect measurement of emotional response. Although these findings will not immediately change clinical practice and do not comment on general effectiveness or reliability of disaster triage, the results call attention to triage’s inherent limitations in cases that are either emotionally difficult or value factors other than survival of injured patients. Additional outcome-based assessments are required to investigate effectiveness of field triage to compare outcomes in adults and children, the proper triage system to use in a mixed disaster scenario, the causes for such preferential triage, and the way to manage this inherent tendency in planning for disaster scenarios.
Disclosure
The authors report no conflicts of interest in this work.
References
Jenkins JL, McCarthy ML, Sauer LM, et al. Mass-casualty triage: time for an evidence based approach. Prehosp Disaster Med. 2008;23(1):3–8. | |
Ireson KV, Moskop JC. Triage in medicine, part I: concept, history, and types. Ann Emerg Med. 2007;49(3):275–281. | |
Aacharya RP, Gastmans C, Denier Y. Emergency department triage: an ethical analysis. BMC Emergency Medicine. 2011;11:16. | |
Chen K. The role tabletop exercise using START in improving triage ability in disaster medical assistance team. Ann Disaster Med. 2003;1(2):79–83. | |
Mace SE, Mayer TA. Triage. In: Baren JM, editor. Pediatric Emergency Care. Elsevier Health Sciences; Philadelphia. 2008:1087–1095. | |
Zoraster R. Disaster triage: is it time to stop START? Am J Disaster Med. 2006;1(1):7–9. | |
Kahn CA, Schultz CH, Miller KT, Anderson CL. Does START triage work? An outcomes assessment after a disaster. Ann Emerg Med. 2009;54(3):424–430. | |
Cone D, Koenig K. Mass casualty triage in the chemical, biological, radiological, or nuclear environment. Eur J Emerg Med. 2005;12(6):287–302. | |
Ranse J, Zeitz K. Disaster triage. In: Powers R, Daily E, editors. International Disaster Nursing. Cambs Uni Press; New York. 2010:57–80. | |
EMDM. Triage Exercise Tabletop Exercise. Universita del Piemonte Orientale. Novarra, Italy. 2009. | |
Cu J, Phan P, O’Leary FM. Knowledge and attitude towards paediatric cardiopulmonary resuscitation among the carers of patients attending the Emergency Department of the Children’s Hospital at Westmead. Emerg Med Australas. 2009;21(5):401–406. | |
Champion HR, Sacco WJ, Copes WS, Gann DS, Gennarelli TA, Flanagan ME. A revision of the trauma score. J Trauma. 1989;29(5):623–629. | |
Hong R, Sierzenski PR, Bollinger M, Durie CC, O’Connor RE. Does the simple triage and rapid treatment method appropriately triage patients based on trauma injury severity score? Am J Disaster Med. 2008;3(5):265–271. | |
Mace SE, Bern AI. Needs assessment: are Disaster Medical Assistance Teams up for the challenge of a pediatric disaster? Am J Emerg Med. 2007;25(7):762–769. | |
Gausche-Hill M. Pediatric disaster preparedness: are we really prepared? J Trauma. 2009;67(2 suppl):S73–S76. | |
Cross KP, Cicero MX. Head-to-head comparison of disaster triage methods in pediatric, adult, and geriatric patients. Ann Emerg Med. 2013;61(6):668–676. | |
Wallis LA, Carley S. Comparison of paediatric major incident primary triage tools. Emerg Med J. 2006;23(6):475–478. | |
Romig LE. Pediatric triage. A system to JumpSTART your triage of young patients at MCIs. JEMS. 2002;27(7):52–58. | |
Aylwin CJ, König TC, Brennan NW, et al. Reduction in critical mortality in urban mass casualty incidents: analysis of triage, surge, and resource use after the London bombings on July 7, 2005. Lancet. 2006;368(9554):2219–2225. | |
West JG, Murdock MA, Baldwin LC, Whalen E. A method for evaluating field triage criteria. J Trauma. 1986;26(7):655–659. | |
Chang DC, Bass RR, Cornwell EE, Mackenzie EJ. Undertriage of elderly trauma patients to state-designated trauma centers. Arch Surg. 2008;143(8):776–781. | |
Scheetz LJ, Zhang J, Kolassa JE. Using crash scene variables to predict the need for trauma center care in older persons. Res Nurs Health. 2007;30(4):399–412. | |
Koziel JR, Meckler G, Brown L, et al. Barriers to pediatric disaster triage: A qualitative investigation. Prehosp Emerg Care. 2015;19(2): 279–286. | |
Frykberg ER, Tepas JJ 3rd. Terrorist bombings: lessons learnt from Belfast to Beirut. Ann Surg. 1988;208(5):569–576. | |
van der Wulp I, Sturms LM, Schrijvers AJ, van Stel HF. An observational study of patients triaged in category 5 of the Emergency Severity Index. Eur J Emerg Med. 2010;17(4):208–213. | |
Nayduch DA, Moylan J, Rutledge R, et al. Comparison of the ability of adult and pediatric trauma scores to predict pediatric outcome following major trauma. J Trauma. 1991;31(4):452–457. | |
Feickert HJ, Drommer S, Heyer R. Severe head injury in children: impact of risk factors on outcome. J Trauma. 1999;47(1):33–38. | |
Pillai S, Praharaj SS, Mohanty A, Kolluri VR. Prognostic factors in children with severe diffuse brain injuries: a study of 74 patients. Pediatr Neurosurg. 2001;34(2):98–103. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

