Back to Journals » HIV/AIDS - Research and Palliative Care » Volume 15
Nutritional Treatment Outcomes of Therapeutic Feeding Program and Its Predictors Among HIV Patients at Hawassa University Comprehensive Specialized Hospital, Hawassa City, Sidama, Southern Ethiopia: A Retrospective Cohort Study
Received 2 December 2022
Accepted for publication 24 February 2023
Published 8 March 2023 Volume 2023:15 Pages 83—93
DOI https://doi.org/10.2147/HIV.S395936
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Olubunmi Akindele Ogunrin
Helen Tadesse,1 Alemayehu Toma2
1Department of Human Nutrition, College of Agriculture, Hawassa University, Hawassa, Sidama, Ethiopia; 2School of Pharmacy, College of Medicine and Health Sciences, Hawassa University, Hawassa, Sidama, Ethiopia
Correspondence: Alemayehu Toma, School of Pharmacy, Hawassa University, Sidama, Ethiopia, Tel +251913259141, Email [email protected]
Background: HIV-induced malnutrition is highly prevalent in different parts of the world particularly in sub-Saharan Africa. The food intervention package is one of the strategies that targets malnutrition among HIV-infected people through nutritional evaluation, counseling and care. However, little is known concerning the outcomes of intervention in such patients in treatment program. Therefore, this study aimed to assess nutritional treatment outcomes and its predictors among adult HIV-positive undernourished individuals in Ethiopia.
Methods: Facility based retrospective cohort study was deployed in Adult Antiretroviral therapy clinic of Hawassa University Comprehensive Specialized Hospital. Data of 419 patients were extracted from the food by prescription registration book and patient cards using structured questionnaires. Statistical significance was assessed using Cox-proportional Hazard model by determining hazard ratios and 95% confidence interval.
Results: The proportion of adult HIV patients who recovered from malnutrition after they were enrolled in the food by prescription therapy was 53.0%. The variables found to have an association with good nutritional treatment outcomes of food by prescription in the final model are being female (Adjusted Hazard Ratio (AHR) = 3.38, 95% CI: 2.15, 5.32), secondary education (AHR = 2.16, 95% CI: 1.11, 4.18), tertiary education (AHR = 3.75, 95% CI: 1.66, 8.48), SAM (AHR = 0.20; 95% CI: 0.12, 0.35), and HAART (AHR = 2.70, 95% CI: 1.50, 4.86). Having Severe Acute Malnutrition (SAM) at baseline nutritional assessment (AHR = 3.42, 95% CI; 2.81, 5.15), taking ART for more than 12 months (AHR = 0.26, 95% CI: 0.13, 0.84) and starting HAART immediately after testing positive (AHR = 0.26, 95% CI: 0.13, 0.84) are significantly associated with nutritional treatment failure.
Conclusion: Fifty-three percent of HIV patients recovered from malnutrition after they were enrolled in the food by prescription therapy.
Keywords: HIV patients, under nutrition, food by prescription, treatment outcomes, Ethiopia
Background
Human immunodeficiency virus (HIV) is a retro-virus that targets and modifies the immune function, and aggravates the risk and influence of opportunistic conditions. Depending on time of treatment intervention, the infection might progress to an advanced disease stage called acquired immune deficiency syndrome (AIDS).1
Among affected individuals, malnutrition is common in advanced stages of disease. HIV, immune manifestation, and nutrition interactions are related to each other. HIV/AIDS is associated with physiological and psychosocial factors that affect an individual’s ability to utilize nutrients. It also causes immune weakening leading to malnutrition which leads to further immune insufficiency, and allows rapid development of HIV infection to AIDS.2,3
The African region remains most severely affected, with nearly one in 25 adults living with HIV and accounting for more than two-thirds of the people living with HIV globally. AIDS and malnutrition have a high occurrence in many parts of the globe especially in sub-Saharan Africa.4
In Ethiopia about 40.4–87.4% people living with HIV struggle to have access to “safe, sufficient and nutritious food” for themselves and for their household. The high prevalence of malnutrition worsens the effect of HIV and poses substantial problems to HIV care and treatment programs in Ethiopia.5
The food intervention program is one of the approaches that targets malnutrition among HIV-infected individuals and their exposed family members through nutritional screening, counseling and care.6
Food by prescription is a program which provides food and nutritional care to malnourished HIV-positive individuals as therapeutic and supplementary feeding package at the health facilities. The objective of the program is to offer energy-rich and nutrient-dense food products along with nutrition evaluation, counseling and care to people living with HIV (PLHIV) who are malnourished or at threat of malnutrition.7 However, little is known concerning the outcomes of intervention in such patients in the treatment program. Therefore, this study aimed to assess nutritional treatment outcomes and their predictors among adult HIV-positive undernourished individuals in Ethiopia.
Methods and Materials
Study Area
The study was employed in the adult ART clinic of Hawassa University Comprehensive Specialized Hospital located in Hawassa city, Ethiopia. Hawassa is the capital of Sidama region, located about 275 kilometers south of the capital city of Ethiopia, Addis Ababa, having an approximate population of 350,000 populations. Hawassa has four public hospitals and 12 health centers. Among them, the two hospitals (Hawassa University Comprehensive Specialized Hospital, Adare General Hospital) and three health centers (Bushulo, Millennium and Tulla) provide ART services. From those ART service providing facilities Hawassa University Comprehensive Specialized Hospital is the largest facility with a food by prescription service without program interruption. The hospital was established in 2005 to provide different types of service for the community including ART service. The hospital was providing ART service for 2850 people living with HIV during the study period.
Study Design and Period
A facility based retrospective cohort study design was employed in Hawassa University Comprehensive Specialized Hospital’s adult ART clinic. The actual data collection (records review, i.e., patients’ cards and registration books reviewing) was conducted from March 1–30, 2021.
Source Population
The source population was all adult HIV-positive patients who had follow up for anti-retroviral therapy (ART) in Hawassa University Comprehensive Specialized Hospital ART clinic from March 1, 2015 to February 30, 2021.
Study Population
The study population was adult HIV-positive patients who had nutritional intervention with food by prescription program at Hawassa University Comprehensive Specialized Hospital’s adult ART clinic.
Eligibility Criteria
Inclusion Criteria
All adult HIV-positive patients aged 18 and above years and those who received nutritional intervention as registered in the food by prescription registration book from March 1, 2015 to February 30, 2021 were included.
Exclusion Criteria
Those who were transferred to other health institutions before the outcome were not evaluated.
Sample Size and Sampling Procedure
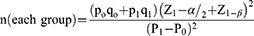
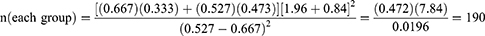
The necessary sample size was calculated using formula for cohort study in order to randomly take from each exposed and non-exposed group with the following assumptions: all explanatory variables were considered as exposure factors.
Z1-α/2 = 1.96; value of the standard normal distribution corresponding to 95% confidence interval for a 2-sided test.
Z1-β = 0.84; value of the standard normal distribution corresponding to the desired level of power of 80%.
n (each group) = equal sample sizes (n1 = n2) 1:1 exposed to non-exposed ratio.
WHO stage was taken as an exposure variable because it yields the largest sample size and the percentage of recovery in the exposed group (patients with WHO stage III or IV) is 52.7% from a recent study performed at Finote Selam Hospital, Northern Ethiopia. 5
P0 = proportion of patients with WHO stage I or II who were recovered = 0.667
P1 = proportion of patients with WHO stage III or IV who were recovered = 0.527
q0 = (1-P0) = 1.0–0.667 = 0.333
q1 = (1-P1) = 1.0–0.527 = 0.473
Therefore: 190 exposed (and 190 non-exposed) = 380,
Therefore, the final sample size included in this study was 419.
Adult HIV-positive patients with known WHO clinical stage and who are undernourished and received food by prescription therapy and fulfilled the inclusion criteria were selected from the available list of the food by prescription registration book from March 1, 2015 to February 30, 2021 (sampling frame, 746 clients were on food by prescription therapy) and then the study participants were selected using a simple random sampling by employing lottery method.
Variables of the Study
The dependent outcome variables are recovered, non-response, loss to follow-up and dead, while independent variables include socio-demographic factors (Sex, Age, Residence, Educational status, Religion, Occupation, Marital status) as well as clinical factors including baseline nutritional status [(BMI < 16 kg/m2) Severe acute malnutrition and (BMI 16–18.4 kg/ m2) Moderate Acute malnutrition], ARV Treatment Status [On pre-ART and on HAART, CD4 count at admission (200 cells/m³, 200–350 cells/m³ and > 350 cells/m³), Opportunistic Infections Presence (Tuberculosis (TB) and other OIs including diarrhea, mouth ulcer/oral thrush, pneumonia, meningitis, CNS toxoplasmosis), WHO clinical stages, Duration of ART treatment, ARV treatment regimens and Prophylaxis given].
Operational Definitions
Adult: Age equal to or greater than 18 years old.
Recovered: Patients who had a BMI of 18.5 kg/m² for two consecutive visits within three months for MAM and within six months for SAM.7
Non-response: Participants who were unable reach a BMI of 18.5 kg/m² for two consecutive visits within three months for MAM and within six months for SAM.7
Loss to follow-up: Participant who did not attend for more than three consecutive months from visit for the nutritional support package.7
Died: Participant died during course of package intervention, and death was documented by clinic staff in the register book.7
Food by prescription: The ready to use therapeutic food prescribed to HIV-positive patients based on their nutritional status (MAM or SAM) as the strategy to address malnutrition among PLHIV through nutritional assessment, counseling, and support.
Treatment outcomes: Outcome of the treatment with food by prescription for 3–6 months among HIV-positive patients recovered, unrecovered, defaulted or died.
Data Collection Procedures and Tool
Data were extracted from the food by prescription registration book and patient cards form by the help of 2 supervisors and 4 nurses who have experience in HIV/AIDS care from March 1–30, 2021. The data were collected using a data extraction tool (checklist) from client chart and food by prescription register. The tool was developed from literature, clients’ intake form cards and food by prescription register. The checklist included data related to socio-demographic, ART, clinical status and outcomes.
Data Processing and Analysis
After collection of data, all questionnaires were checked for completeness and consistency by the principal investigator. All data were cleaned, edited, coded and entered into Epi-Data version 3.1 and exported to SPSS version 25. Frequencies and proportions were used to describe the characteristics of the cohort. The outcome measures of food by prescription were recovered, failure to respond, default, and death. Kaplan–Meier survival curve together with log rank test was used to estimate median time and to compare the overall survival experience of two or more groups. Cox proportional hazards model was fitted after checking the reasonability of assumptions through the Schoenfeld residuals test and graphically. The bivariate analysis was done to identify variables that could be a candidate for multivariate analysis. Variables with P ≤ 0.25 levels in the bi-variable analysis were further analyzed through multivariable analysis. The backward variable selection procedure was applied to get a list of best predictors and adjusted hazard ratio, 95% CI and P-value were used to assess the strength of association and statistical significance. Level of statistical significance was declared at P-value < 0.05.
Data Quality Management
The data gathering format was checked for clarity and completeness and the whole method was pre-tested on randomly selected patients before the actual data collection was deployed. Possible modifications were carried out on the data collection format based on available data and review of previous literature. Data collectors were two BSc nurses from the hospital’s ART clinic and one supervisor was also from the clinic and he was pharmacy head of the ART clinic. Two days training was given for both data collectors and supervisor in order to make them familiar with the data collection tool. Filled data-gathering tools were being checked regularly for completeness of information.
Ethical Considerations
The Institutional ethical review committee of Hawassa University College of Medicine and Health Sciences approved the study and study design and objectives were explained to concerned administrative officials of Hawassa Comprehensive Specialized Hospital through an official letter. Permission to conduct the study was obtained from the Clinical and Academic Director of the facility. The nature of the study was fully explained to the head of department of the ART clinic to obtain the permission for extracting data from FBP registration books and patient cards. The study used the routine existing patient record data. The gathered data were kept safe throughout the whole process of the research work to limit data accessibility to a third party. Since the study was retrospective, informed consent was waived by the institutional review board. The privacy of the participants was maintained as data were anonymized or maintained with confidentiality. We confirm that the study complies with the Declaration of Helsinki.
Results
Socio-Demographic Characteristics
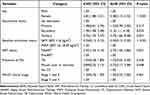
A total of 419 study participants were included in this study. More than half of participants were females (59.2%) and median age was 35 years (IQR 29–42). Around 37.7% of participants had secondary level education, and 62.8% were self-employed. Around (44.4%) were in union, 90.7% were come from an urban area (Table 1).
 |
Table 1 Socio-Demographic Characteristics of Malnourished Adult HIV-Infected Patients at Admission by Outcome in Hawassa University Comprehensive Specialized Hospital, Southern Ethiopia, 2021 |
Clinical Characteristics of HIV-Infected Adult Patients at Admission
From the total 419 study participants, one-fourth (25%) were treated as SAM cases while almost 30% participants received food by prescription as they had MAM (BMI 16–18.49 kg/m2). Only 22.2% adult HIV-infected patients had CD4 level of < 200 cells/m3. More than three-fourths (77.8%) of participants had WHO clinical stage 1 and 2 at baseline and 11.9% had tuberculosis as opportunistic infection. The median BMI was 16.9 kg/m2 (IQR 16.0–17.5) at baseline and 18.6 kg/m2 (IQR 17.2–19.5) at the end of the study (Table 2).
Characteristics of Recovered Patients from Under-Nutrition
The median follow-up time of the study participants was 6 months (IQR 3.7–9.0 months) during which 53% of adult HIV patients recovered from their malnutrition after they were enrolled in the food by prescription therapy. Of those who experienced poor outcome, 197 out of 419 (47.0%), 155 (37.0%) did not respond to the food by prescription therapy, 7 (1.7%) died and 35 (8.4%) were defaulters. The median recovery time for participants with moderate acute malnutrition was 5.0 months (IQR 3.6–8.6 months) and 6.0 months (IQR 3.7–9.7 months) for those with severe acute malnutrition.
Factors Associated with Recovery as Treatment Outcomes
Using bivariate Cox regression analyses, six variables with P-value of < 0.25 were recruited to be included in the final model. Thus, in the multivariable analysis, the variables found to have an association with recovery from under-nutrition of food by prescription in the final model are sex, education status, baseline nutritional status, and ART status.
Therefore, this study found that female adult HIV patients had 3.4 times higher odds of recovery from malnutrition after being enrolled in food by prescription therapy compared with male patients (AHR = 3.38; 95% CI: 2.15, 5.32). Participants who completed secondary (AHR = 2.16; 95% CI: 1.11, 4.18) or tertiary level of education (AHR = 3.75; 95% CI: 1.66, 8.48) had higher probability of recovery compared with participants with no education. The probability of nutritional recovery was 80% lower for participants with severe acute malnutrition (AHR = 0.20; 95% CI: 0.12, 0.35) compared with those adult HIV patients who had moderate acute malnutrition when enrolled in the food by prescription therapy. Moreover, those adult HIV patients who were using highly active anti-retroviral therapy at baseline were 2.7 times more likely to recover from their malnutrition compared with those who were pre-ART at admission (AHR = 2.70; 95% CI: 1.50, 4.86). Having opportunistic infections such as diagnosed TB at admission or during follow-up, presence of diarrheal disease or extensive candidiasis, or any of the WHO clinical stages were unrelated to the probability of nutritional recovery (Table 3, Figure 1).
 |
Figure 1 Kaplan–Meier estimate curve for median nutritional recovery time. |
Factors Associated with Non-Response/Treatment Failure
During bivariate analyses, 6 variables were found to be candidates for multivariable analysis with P-value of < 0.25. These variables are Baseline nutritional status, ART treatment duration, and Baseline CD4 level, and Educational status, CD4 after ART treatment started ART status and WHO stage. After multivariate analysis Baseline nutritional status was found to be significant (AHR = 3.42, 95% CI = 2.81–5.15), P-value = 0.001 (Table 4).
Factors Associated with Defaulting from Under-Nutrition in Food by Prescription Therapy
During bivariate analyses, 4 variables were found to be candidates for multivariable analysis with P-value of < 0.25. These variables are Residence, ART treatment duration, Baseline CD4 level, and WHO stage. After multivariate analysis only ART treatment duration was found to be significant (AHR = 0.2, 95% CI = 0.06–0.54), P-value = 0.002.
Factors Associated with Death from Under-Nutrition in Food by Prescription Therapy
During bivariate analyses, 6 variables were found to be candidates for multivariable analysis with P-value of < 0.25. These variables are Age, Baseline BMI, Baseline CD4 level, Educational status, CD4 after ART treatment started and WHO stage. After multivariate analysis only ART treatment duration was found to be significant (AHR = 0.2, 95% CI = 0.06–0.54), P-value = 0.002 (Table 5).
Discussion
The current study demonstrated that from the total adult HIV patients enrolled in the food by prescription therapy, more than half of patients (53.0%) were recovered from under-nutrition. This level of recovery was higher than the finding from a study carried out in Ethiopia on impacts of food by prescription which demonstrated that the percentage of recovery was 42%,7 but lower than the finding of a retrospective cohort study conducted in Mekelle which stated 62.2% of patients were recovered from malnutrition after ready-to-use food therapy initiation.8 These differences of recovery rate might indicate the success of the nutritional therapy program center to effectively follow patients thus decreasing default from the program. In our study 8.4% of participants defaulted from the program.
Management of HIV/AIDS-related malnutrition has been successfully improved after nutrition intervention packages. Both body weight and general health condition of many patients with HIV/AIDS have markedly improved after being enrolled into such programs.9 In the current study, there was weight increment from mean weight at admission of 44.4 kg (± 4.8 SD) to 49.2 kg (± 5.6 SD) and mean CD4 level was increased from 442.6 cells/m3 at admission to 490.6 cells/m3 after nutritional treatment.7,8
This study found that female adult HIV-patients had 3.4 times higher odds of recovery from malnutrition after being enrolled in food by prescription therapy compared with male patients. Males tend to access HIV care at a higher viral load level as well as clinically and/or immunologically advanced stage of disease than women,5–8 a higher probability of nutritional recovery therefore exists in females. Sex variances in patient adherence to nutritional management and/or ART could also explain our outcomes.
In our study, participants who completed secondary or tertiary level of education had higher probability of recovery from under-nutrition after being enrolled in food by prescription therapy compared with participants with no education. Our finding is in line with the finding of a study carried out at Finote-Selam General Hospital, Northwest Ethiopia that revealed those who did not attend any formal education had a decreased probability of recovery from under-nutrition.5 Educated clients may better understand the benefits of using food by prescription and adhere to the therapy, consequently could have better probability of recovery from their under-nutrition.
The likelihood of nutritional recovery was 80% lower for participants with severe acute malnutrition compared with those adult HIV patients who had moderate acute malnutrition when enrolled in the food by prescription therapy. Our finding was comparable with a study conducted in another part of Ethiopia on impacts of food by prescription which showed that being moderately rather than severely malnourished increased the chances of recovery from malnutrition.7–9 Nutritional care with ready to use therapeutic foods (RUTF) may be more effective when provided to patients at earlier stages of malnutrition. A study carried on effects and affordability of food by prescription on retrieval from under-nutrition in Ethiopia revealed that close follow-up of the nutritional status of HIV patients and treating malnutrition at an early stage is important to achieve optimal retrieval from under-nutrition.7 A study carried out in Tanzania indicated 3.0% of underweight and 2.8% of wasting among RUTF receivers, whereas in non-RUTF receivers there were 12.4% of underweight and 16.5% of wasting. Provision of RUTF for at least four consecutive months was linked with less probability of low nutritional status.10
Moreover, those adult HIV patients who were using highly active anti-retroviral therapy at admission were 2.7 times more likely to recover from their malnutrition compared with those who were pre-ART at admission. This finding was comparable with a study carried out in Ethiopia on effects of food by prescription and another study employed in sub-Saharan African countries demonstrated that recent launching of ART increased chance of recovery from malnutrition.7,10 This might be explained by the fact that not using ART depletes immunity (CD4) and surges the rate of opportunistic infections. Nutrition-based interventions can play a complementary role in overall weight improvement and HAART’s action in improving the life of the patient. This finding is backed by confirmation from a prospective cohort study assessing acceptability and success of a locally produced RUTF in HIV-infected, regularly ill adult patients in Malawi,11 where HIV patients beginning ART prior to or while on nutritional therapy developed greater weight gains.
This study has found that patients who are severely undernourished in baseline nutritional status are 3.42 times at risk of failing to respond compared with those with mild under-nutrition at baseline assessment. This finding is supported by a similar study done in Mekelle.12,13
Patients who started HAART immediately after being found positive for HIV and those who have taken ART therapy for a longer period are 74% and 78% less likely to non-respond to treatment, respectively. This finding may be explained by patients who started their HIV treatment immediately after being found positive have good progress in clinical stages of the disease which may boost the recovery from under-nutrition. Patients who are on HIV treatment for longer periods may have good awareness about their clinical status and may adhere better to nutritional therapy.
Patients who are illiterate were 4.25 times more likely to fail or die than those educated. Similar study from other areas of Ethiopia had supportive confirmation for this finding that individuals who had no formal education is 1.8 CI (1.5–5.2) at risk of dying.7,12
The limitations of the study were lack of control group for comparison and the nature of the study design limits the ability to gather all primary relevant factors as data were collected by document review, and hence, the analysis and interpretation of the data were limited to only those parameters that were documented in the patient records. Information on household food availability and patient adherence to nutrition therapy were not obtainable and might have biased the results of our analysis. The other limitation was that, there could have been a data recruitment bias arising from the fact that the samples were limited only to individuals with documented nutritional outcomes.
Conclusion
In this study, 53% recovered from malnutrition after they were enrolled in the food by prescription therapy than any other treatment outcomes. Being female, secondary and tertiary level of education, and using HAART at admission increase probability of nutritional recovery while having SAM nutritional status decreased probability of nutritional recovery. Being undernourished in baseline nutritional status, patients who started HAART after being found positive and those who had taken ART therapy for a longer period are less likely to non-respond to treatment respectively. Patients with no education and low CD4 level had a lower survival on nutrition treatment.
Data Sharing Statement
The data utilized in this study are within the manuscript.
Ethics Approval and Consent to Participate
Ethical approval number IRB/070/2021 for this study was obtained from Institutional Ethical Review Committee of Hawassa University College of Medicine and Health Sciences.
Acknowledgment
We are grateful to the Hawassa University Comprehensive Specialized Hospital ART Clinic staff for providing the data.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was funded by Hawassa University Office of Vice President for research and Technology Transfer Grant Number 6114/2021.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Duggal S, Chugh TD, Duggal AK. HIV and malnutrition: effects on immune system. Clin Dev Immunol. 2012;2012:784740. doi:10.1155/2012/784740
2. Amlogu AM, Tewfik S, Wambebe C, Tewfik I. Innovative nutritional approach to attenuate the progression of HIV to AIDS among People Living with HIV (PLWH): a study based in Abuja, Nigeria. J Adv Res Med Health Sci. 2019;5(1):01–28.
3. Baez-Franceschi D, Morley JE. Pathophysiologie des Katabolismus* bei unterernährten alten Patienten; PATHOPHYSIOLOGIE DER MALNUTRITION [Pathophysiology of catabolism in undernurished elderly patients]. Z Gerontol Geriatr. 1999;32(Suppl 1):I12–I19. German. doi:10.1007/s003910050175
4. UNAIDS D. Update AE. Geneva: Joint United Nations Programme on HIV, AIDS; 2019.
5. Diress G, Moges NA. Nutritional recovery and its predictors among adult HIV patients on therapeutic feeding program at Finote-Selam general hospital, Northwest Ethiopia: a retrospective cohort study. AIDS Res Treat. 2020;2020:1–6.
6. Wieringa F. FANTA)/FHI 360; 2013.
7. Bontrager E, Sadler K. Early stages of a ‘food by prescription’programme for HIV infected adults. Field Exch. 2011;40:82.
8. Berhe M, Fisaha H, Ashenafi S. Outcome of ready to use food therapy among patients on HIV/AIDS care in Mekelle Hospital, Northern Ethiopia: retrospective cohort study. J AIDS Clin Res. 2014;5(1):268.
9. Koethe JR, Chi BH, Megazzini KM, Heimburger DC, Stringer JS. Macronutrient supplementation for malnourished HIV-infected adults: a review of the evidence in resource-adequate and resource-constrained settings. Clin Infect Dis. 2009;49(5):787–798. doi:10.1086/605285
10. Sunguya BF, Poudel KC, Mlunde LB, et al. Ready to Use Therapeutic Foods (RUTF) improves undernutrition among ART-treated, HIV-positive children in Dar es Salaam, Tanzania. Nutr J. 2012;11(1):60. doi:10.1186/1475-2891-11-60
11. Bahwere P, Sadler K, Collins S. Acceptability and effectiveness of chickpea sesame-based ready-to-use therapeutic food in malnourished HIV-positive adults. Patient Prefer Adherence. 2009;3:67. doi:10.2147/PPA.S4636
12. Maldey B, Haile F, Shumye A. Outcome of ready to use food therapy among patients on HIV. AIDS care in Mekelle Hospital, Northern Ethiopia: retrospective cohort study. AIDS Clin Res. 2014;5(1):
13. Ahoua L, Umutoni C, Huerga H, et al. Nutrition outcomes of HIV-infected malnourished adults treated with ready-to-use therapeutic food in sub-Saharan Africa: a longitudinal study. J Int AIDS Soc. 2011;14:2. doi:10.1186/1758-2652-14-2
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.