Back to Journals » Risk Management and Healthcare Policy » Volume 16
Nutrition and Physical Activity Counseling by General Practitioners in China
Received 28 July 2023
Accepted for publication 10 October 2023
Published 16 October 2023 Volume 2023:16 Pages 2151—2162
DOI https://doi.org/10.2147/RMHP.S427481
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jongwha Chang
Xian Tan,1,2 Hebin Xie,3 Danling Wang1– 3
1Hengyang Medical School, University of South China, Hengyang, Hunan, People’s Republic of China; 2Institute for Future Sciences, University of South China, Changsha, Hunan, People’s Republic of China; 3The Affiliated Changsha Central Hospital, Hengyang Medical School, University of South China, Changsha, Hunan, People’s Republic of China
Correspondence: Danling Wang, Hengyang Medical School, University of South China, 28 West Changsheng Road, Hengyang, Hunan, 421001, People’s Republic of China, Email [email protected]
Introduction: To reduce unhealthy lifestyles in China, it is critical to implement effective strategies. Counseling provided by physicians is important for assisting patients in improving their lifestyles, and general practitioners (GPs) are the main providers of lifestyle counseling to patients. However, few studies have focused on the lifestyle counseling practices by GPs in China, particularly in regard to nutrition and physical activity.
Objective: The aims of this study are: (i) to examine the current practice of Chinese GPs in counseling patients regarding nutrition and physical activity; (ii) to understand the common barriers to such counseling by Chinese GPs; and (iii) to study the association between GPs’ personal lifestyle choices and their practices in lifestyle counseling.
Methods: A cross-sectional, self-reported online questionnaire was conducted among GPs in Hunan province, China. A total of 198 GPs completed the questionnaire.
Results: The majority of GPs provide nutrition and physical activity counseling to less than 40% of their patients, spending less than three minutes per counseling session. The main reported barriers to counseling on nutrition and physical activity are inadequate time and a lack of knowledge or experience. GPs primarily acquire knowledge through medical books and journals, followed by science popularization. Furthermore, GPs who maintain healthier lifestyle habits, possess a better understanding of lifestyle guidelines, conduct longer office visits, and exhibit higher self-efficacy are more likely to provide counseling to patients.
Conclusion: This study highlights the need for improvement in nutrition and physical activity counseling among Chinese GPs. GPs’ personal nutrition and physical activity habits may measurably influence their counseling practice. We recommend that GPs themselves adopt healthier lifestyle habits to potentially improve their counseling practice. Moreover, proactive measures should be taken to assist GPs in overcoming barriers encountered with lifestyle counseling.
Keywords: nutrition counseling, physical activity counseling, lifestyle counseling, general practitioner, China
Introduction
Noncommunicable diseases (NCDs), such as cardiovascular disease (CVD), cancer, respiratory disease, and diabetes, are the biggest threats to global health, responsible for 74% of all deaths worldwide.1 In China, NCDs account for approximately 89% of deaths and contribute to 82% of the country’s total disease burden, and the incidence of NCDs is expected to rise further due to China’s rapid population aging.2,3 Modifiable behaviors like physical inactivity and unhealthy diet are the leading risk factors for NCDs.4,5 In China, physical inactivity contributes 12–19% of the risks associated with five major NCDs, imposing a substantial economic burden.6 Additionally, research in China suggests that excessive energy intake contributes to the high incidence of stroke and hypertension, with high consumption of edible salt being the major cause of these conditions in northern China.7,8 Given that most NCDs are chronic and reversible, an efficient way to control NCDs is educating individuals on healthy lifestyles, such as eating well-balanced diet and exercising regularly.9,10
The World Health Organization (WHO) currently recommends that adults carry out at least 150 minutes of moderate-intensity aerobic exercise or 75 minutes of vigorous aerobic exercise each week.11 In addition, the WHO advocates for a healthy, well-balanced diet comprising less than 30% of fat energy, less than 10% saturated fats energy, and less than 10% free sugars energy that is in line with energy expenditure.12 In alignment with the WHO recommendations, the Chinese government has developed the Chinese Food Guide Pagoda (CFGP) and the Chinese National Fitness Guidance (CNFG) to promote healthy lifestyles within the Chinese population.13 The CFGP is a graphic representation illustrating the recommended quantity and proportion of various food intake for adequate nutrition to adults, and the CNFG provides guidelines to promote physical fitness and healthy lifestyle through various exercise activities.14
Despite all these efforts, the rate of obesity among Chinese people has been steadily rising.15 Moreover, there has been a concerning upward trend in China in adult population (17.9% being physical inactive in 2010 and 22.3%, in 2018).16 The total physical activity of children aged 6–17 years in China has also exhibited a trend of decreasing from 2004 to 2015.17 In addition, a recent report published in BioMed Central Public Health reported that healthy lifestyle interventions were ineffective in rural China, for less than 50% of the population participating in salt intake control and less than 9% engaging in at least mild-intensity physical exercise.18 Thus, there is an urgent need to implement strategies aimed at reducing unhealthy lifestyles in China.
A powerful solution to promoting healthy lifestyles is through medical counseling provided by physicians of primary care, ie, general practitioners (GPs). Benefiting from the trust patients place in them and the continuity of care they can provide, GPs hold a unique and influential position in educating and guiding patients towards healthy lifestyles.19,20 As a result of the ongoing nationwide healthcare reform, China has been rapidly expanding its GP workforce in recent years. In 2012, there were merely 100,000 GPs in China, but by 2030, the goal is to have 700,000 GPs, aiming for an average of five GPs per 10,000 residents.21,22 Consequently, China has established various career development programs pathways for individuals to becoming and practicing as a GP, including rural service tracks (3–5 year program), GP-oriented pathways (3–5 year program), and transitioning from other medical specialties to the GP track (1–2 year program).23 Due to this swift expansion, the population of Chinese GPs could be relative younger and less experienced compared to those in Western countries where health systems have long been built based on the GP system.
Many previous studies have explored how GPs in Western countries provide lifestyle counseling in their clinical practices. For example, in the United States, exercise counseling occurred in 22.3% of clinic visits, with an average counseling duration of 0.78 minute, ranging from 0.33 to 6.00 minutes.24 Nutrition counseling was provided by six percent of family physicians in the United States during the majority of patient visits. The average duration for nutrition counseling was 55 seconds, ranging from less than 20 seconds to more than 6 minutes.25 However, there have been limited studies assessing the pattern of lifestyle counseling among GPs in China, particularly in terms of nutrition and physical activity counseling. This study aimed to examine the current practice of lifestyle counseling on nutrition and physical activity among GPs in Hunan province, China. In addition, this study evaluated the common barriers faced by GPs when providing such counseling to patients and whether GPs’ personal lifestyle habits could predict their counseling practices.
Materials and Methods
Study Sample
According to the Hunan Province Statistical Communiqué for the 2021 National Economic and Social Development and the Hunan Province Statistical Communiqué for the 2021 Health Care Development, by the end of 2021, there were estimated 18,000 GPs in Hunan Province, equating to an average of 2.71 GPs per 10,000 residents. In this study, the sample was recruited from the Hunan GP Educational network, which is organized and managed by Hengyang Medical School at the University of South China. The network is estimated to encompass about 15% of all GPs from various geographical areas in Hunan province.
This study adopted a convenient sampling method within GPs who were actively practicing in Hunan province. The survey was conducted using Questionnaire Star, an internet-based survey tool. Eligible GPs from this network were invited to participate through both email and WeChat (a social media platform requires real identity authentication). A total of 204 GPs returned the questionnaire. With an estimated total number of GPs in this network being 2700 (18,000 x 15% = 2700), the questionnaire return rate was about 8% (204/2700 = 7.56%). After excluding 6 incomplete questionnaire responses, the final sample size was 198. To determine the required sample size for this study, G-Power 3.1 statistical software was chosen to use. Using two-tailed tests, an effect size of 0.30, a power value of 0.80, and α value of 0.05, the minimal sample size needed for this study was calculated to be 143.26
Measures
The questionnaire was designed based on previously published surveys used in other countries, with meticulous adapting to draw questions from guidelines widely used in China such as CFGP, and CNFG.27–29 To enhance the comprehensiveness of the questionnaire, we revised the questionnaire for multiple rounds with the insights and feedback received from a group of three experienced senior GPs after analyzing the question items and a group of twenty GPs after running a pre-survey test. The final refined version of the questionnaire was used for the survey.
The questionnaire designed for this research was aimed to obtain comprehensive information including the demographic, nutritional, and physical activity profiles of GPs, as well as their engagement in nutrition and physical activity counseling. Demographic information includes gender, age, and body mass index (BMI).
In terms of GPs’ nutrition choices, the daily consumption of essential food items like cereals, vegetables, and meat was evaluated among GPs and compared with the CFGP. The deviations from the Pagoda, either with higher or lower consumption of certain food, was considered as not meeting the recommendations by the Pagoda. The number of days with a well-balanced diet refers to the weekly frequency of appropriately matched food types to achieve balanced nutrition, categorized as “< 3” or “≥ 3” days.
To understand GPs’ physical activity profiles, GPs were queried about the frequency and duration of each session of moderate and heavy physical activity, along with their daily step count. Physical activity per week was classified by the number of engaged days, as “0”, “1–2”, “3–4” or “5–7” days. Duration of moderate physical activity was categorized as “< 30 min” or “≥ 30 min;” duration of heavy physical activity was categorized as “< 20 min” or “≥ 20 min;” and average daily step count was categorized as “< 6000” or “≥ 6000”.
To evaluate GPs’ practices regarding nutrition and physical activity counseling, GPs were queried to estimate the percentage of patients they counseled and the time spent per counseling session. Percentage of patients received counseling on nutrition and physical activity during their clinic visits was categorized as “< 40%” or “≥ 40%”. Duration of each counseling session was categorized as “< 1 min”, “1–3 min” or “> 3 min”. Last, the average duration of a routine visit was classified as “< 10 min” or “≥ 10 min”.
To evaluate GPs’ confidence on nutrition and physical activity counseling, the self-efficacy of the counseling was also inquired via self-reporting method. The self-efficacy of improving a patient’s nutrition and physical activity was categorized as “Not/Slightly effective” or “Effective/Very effective”. GPs’ familiarity with key guidance tools like the CFGP and the CNFG was also assessed, categorized as “Not/Slightly familiar” or “Familiar/Very familiar”.
Furthermore, data were collected on the perceived barriers to counseling patients on nutrition and physical activity, with options including “not enough time”, “I don’t think it’s necessary”, “lack of knowledge and experience”, and “others”. Additionally, the sources from which GPs derived their knowledge for counseling, including categories such as “Family & friends”, “Advertisement”, “Science popularization”, “Training”, and “Medical books/Journals” was also surveyed in the questionnaire.
Statistical Analysis
Exploratory data analysis was conducted to understand the characteristics of the dataset, and Shapiro–Wilk tests were performed to determine the normality of the data distribution. Continuous variables are presented as means or medians along with interquartile ranges, and categorical variables are described using counts and percentages. The χ2 test was performed to compare categorical variables between groups at the baseline. The level of significance was set by 2-sided P value, and statistical significance is defined as P < 0.05. All statistical analyses were carried out using IBM SPSS Statistics 25.0 (IBM, New York, USA).
Results
A total of 198 GPs completed the survey, of whom 88 (44%) were male and 110 (56%) were female. The majority of respondents (53%) fell within the age range of 26 to 35 years (Table 1 and Table 2).
 |
Table 1 Personal Profile of and the Nutrition Counseling Practice by General Practitioners in Hunan, China (N = 198) |
 |
Table 2 Personal Profile of and the Physical Activity Counseling Practice by General Practitioners in Hunan, China (N = 198) |
Nutrition and Physical Activity Counseling Provided by GPs
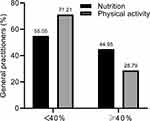
We observed no significant differences in the duration of nutrition and physical activity counseling or the percentage of patients counseled based on the gender or age of the GPs (Table 1 and Table 2). During routine office visits, more than half of the responded GPs reported that they offer nutrition and physical activity counseling (55.05% for nutrition and 71.21% for physical activity) to less than 40% of their office-visiting patients (Figure 1). Majority of GPs stated spending 3 minutes or less on nutrition and physical activity counseling (77.78% for nutrition and 87.88% for physical activity, Figure 2). Between nutrition and physical activity counseling, there were some differences in the duration of counseling and the percentage of patients counseled. As shown in Table 3, GPs were more likely to spend more than 3 minutes on nutrition counseling (P < 0.001), and the percentage of patients counseled on nutrition was more likely to exceed 40% (P < 0.001).
 |
Table 3 Comparing Nutrition Counseling and Physical Activity Counseling by General Practitioners in Hunan, China |
 |
Figure 2 Duration for Nutrition and Physical Activity Counseling Sessions. The majority of GPs stated spending 3 minutes or less on nutrition and physical activity counseling. |
Perceived Barriers to the Nutrition and Physical Activity Counseling
As shown in Figure 3, among the main perceived barriers to nutrition and physical activity counseling, inadequate time was reported as the primary obstacle by a significant portion of GPs (56.06% for nutrition counseling and 54.04% for physical activity counseling). A majority of GPs (68%) stated generally spending less than 10 minutes with patients per office visit. GPs who had longer consultation time with patients were more likely to counsel on nutrition for more than three minutes (P = 0.004) and counsel more than 40% of patients (P = 0.027, Table 1). Similarly, these GPs were more likely to counsel more than 40% of patients on physical activity (P = 0.004, Table 2).
The second major reported barrier was inadequate knowledge or experience, with 26.26% reporting this barrier for nutrition counseling and 30.30% for physical activity counseling (Figure 3). When asked about their sources of knowledge for providing lifestyle counseling, GPs frequently cited medical books and journals (52.53% for nutrition counseling and 43.43% for physical activity counseling), as well as science popularization (37.37% for nutrition counseling and 43.94% for physical activity counseling). Only a small percentage of GPs (7.58% for nutrition counseling and 6.57% for physical activity counseling) stated that they gained knowledge of lifestyle counseling through professional training (Figure 4).
In terms of beliefs and attitudes, more than half of the GPs reported low perceived confidence in effectively counseling to improve patients’ nutrition choices (54%, Table 1). A similar high percentage with low perceived confidence was observed in physical activity counseling (58%, Table 2). GPs who reported high self-efficacy for counseling on nutrition were more likely to counsel for more than 3 minutes (P = 0.001) and more than 40% of patients (P < 0.001, Table 1). Surprisingly, a notable percentage of GPs (10.10% for nutrition counseling and 11.62% for physical activity counseling) indicated that they considered providing nutrition and physical activity counseling unnecessary (Figure 3).
General Practitioners’ Lifestyle Choices and Their Lifestyle Counseling
We also investigated the association between GPs’ lifestyle choices and their nutrition and physical activity counseling practices at the clinic. As shown in Table 1, GPs who reported healthier dietary habits, such as adhering to the recommended vegetables consumption according to the CFGP, were more likely to counsel for over 3 minutes (P = 0.002) and discuss nutrition with more than 40% of patients (P = 0.009). In addition, GPs who adopted well-balanced diet for more than 3 days per week were more inclined to counsel more than 40% of their patients (P = 0.008) about nutrition. Furthermore, GPs who exhibited better familiarity with the CFGP were more likely to counsel more than 40% of their patients (P = 0.006) about nutrition and for a duration longer than 3 minutes (P = 0.008).
Table 2 shows that GPs with more days of moderate physical activity per week were more likely to counsel on physical activity for longer than 3 minutes (P = 0.007). Moreover, GPs who have a step count of more than 6000 steps per day were more likely to counsel more than 40% of patients about physical activity (P = 0.042). Conversely, GPs who reported being overweight (BMI ≥ 24) were associated with a shorter duration of physical activity counseling (P = 0.037, Table 2).
Discussion
In recent years, China has experienced a surge in the GP workforce due to the ongoing healthcare reform throughout the country, part of which aims to develop a robust primary care foundation to support a hierarchical diagnosis and treatment system.23 This rapid expansion has led to an inrush of young professionals, therefore raising an important question that how Chinese GPs provide lifestyle counseling, particularly regarding nutrition and physical activity, to their patients. Until now, there are very limited amount of studies have been published to address this question. To bridge this gap, we conducted a cross-sectional self-reported online questionnaire among GPs in Hunan province, China.
We observed several key findings that align well with those reported with GPs’ practices in other countries. First, our results showed that more than half of the GPs reported providing nutrition and physical activity counseling to less than 40% of their patients, consistent with previous studies that also reported that less than 40% of patients received such counseling.27,30 Second, a majority of our GPs reported spending less than three minutes on nutrition or physical activity counseling during a routine office visit, in line with studies conducted in the United States, where 57.7% of GPs spend 3 minutes or less counseling their patient about diet,29 and 53% of GPs provide physical activity counseling for no more than 3 minutes.27
Similar to studies in the other countries, we identified common barriers to nutrition and physical activity counseling among our GPs are inadequate time and lack of knowledge. A previous systematic literature review on the perceptions of medical providers has also identified lack of time as the most common barrier to physical activity counseling, followed by lack of knowledge or training.31 Similar barriers have been indicated in the practice of nutrition counseling—a Danish study has reported that lack of time and knowledge are the main obstacles that prevent Danish GPs providing nutrition counseling to their patients;32 and time constraint was concluded as the most common barrier to providing nutrition counseling in the United States.30
To further understand the time constraints faced by our GPs, we assessed the overall duration of GP office visits. A majority of our GPs reported spending less than 10 minutes per patient during office visits, contrasting with the longer durations typically seen in other countries.25,33 Consistently, we found that GPs with longer office-visit durations were more likely to provide lifestyle counseling to their patients. Therefore, it could be crucial to implement a system that allows for longer physician office visits to enhance the lifestyle counseling in China.
Our study also emphasized an imperfection in knowledge acquisition among our GPs. Although about one-third of GPs reported a lack of knowledge and experience in providing nutrition and physical activity counseling, the percentage of GPs who obtained knowledge through professional training was notably low. Other studies have demonstrated that physicians with specific training in nutrition and physical activity counseling are more likely to provide relevant counseling compared to those physicians without such training.34,35 Furthermore, there is a demonstrated desire among Canadian physicians for lifestyle medicine curriculum to be included in their medical training.36 Therefore, enhancing lifestyle medical trainings might significantly improve Chinese GPs’ ability to provide such counseling to their patients.
In addition, our results highlighted that role of self-efficacy in counseling effectiveness. GPs with higher self-efficacy for counseling on nutrition were more likely to counsel for longer durations and to more of their patients. However, more than half of our GPs reported low perceived confidence for being able to provide effective counseling to improve their patients’ nutrition and physical activity styles. Professional training has been shown to be effective in improving physician’s self-efficacy in lifestyle counseling.35 Physicians with adequate training in lifestyle counseling exhibit greater confident in their ability to counsel effectively and are more likely to initiate counseling.28 Thus, our observation promotes the idea that measures should be taken to offer more comprehensive lifestyle medical trainings to our GPs.
Consistent with numerous previous reports, our study demonstrated that GPs’ personal nutrition and physical activity habits are associated with their patient counseling.37,38 GPs who reported healthier personal nutrition and physical activity habits were more inclined to provide counseling. Thus, to enhance the effectiveness of lifestyle counseling to patients, it is important for GPs to first improve their own lifestyle choices.27
One notable finding in this study is that a significant portion of GPs (10.10% for nutrition counseling and 11.62% for physical activity counseling) who believe that it is unnecessary to provide nutrition and physical activity counseling to patients. Given the strong association between NCDs and unhealthy lifestyle behaviors, one would expect a stronger belief in the value of lifestyle counseling among GPs. The disbelief among some of our GPs may be attributed to the assumption that patients with NCDs, such as CVDs, would consult specialists and dietitians, leading to a misconception that lifestyle counseling is the role to be fulfilled by other healthcare professionals in the healthcare process.
Despite these interesting findings, this study has certain limitations. The survey relies on GP’s self-reports, which may not be entirely reliable. The sample size of this study is relatively small, potentially impacting the study’s power. The response rate of the survey is also relatively low, which could be due to factors like the questionnaire being not mandatory and some GPs lacking interest in participating. The study’s sample is restricted to GPs from a single province, limiting the generalizability of the findings to the whole population of GPs in China. Future research using a direct observation approach and involving a larger sample across various regions in the country would be helpful to provide a more comprehensive understanding of the lifestyle counseling practices among GPs in China.
Conclusion
Despite the limitations mentioned, the study offers valuable insights into nutrition and physical activity counseling among GPs in Hunan Province, China. The findings from this study underscore the need for improvement in nutrition and physical activity counseling practice among Chinese GPs. Specific measures should be taken to assist Chinese GPs in overcoming barriers faced with lifestyle counseling. GPs’ personal nutrition and physical activity habits may influence their counseling practice; therefore, we advocate for GPs to adopt healthier lifestyles to enhance their lifestyle counseling to patients.
Ethics Statement
The human participation of this study has been reviewed and approved by the Ethics Committees of the Affiliated Changsha Central Hospital, Hengyang Medical School, University of South China. Informed consent was obtained from all participants involved in the study. This research was conducted in full compliance with the principles set out in the Declaration of Helsinki.
Acknowledgments
We express our sincere gratitude to Professor Zhihan Tang from Hengyang Medical School, University of South China, for his valuable assistance in connecting us with GPs in the Hunan GP Educational network and providing insightful discussions throughout the whole study.
Funding
This work is funded by the Education Department Program of Hunan Province, under grant number HNJG-2020-0440.
Disclosure
The authors declare that they have no competing interests in this work.
References
1. World Health Organization. World health statistics 2022: monitoring health for the SDGs, sustainable development goals; 2022. Available from: https://www.who.int/publications/i/item/9789240051157.
2. World Health Organization. Noncommunicable diseases country profiles; 2018. Available from: https://www.who.int/publications/i/item/ncd-country-profiles–2018.
3. Menhas R, Dai J, Ashraf MA, et al. Physical inactivity, non-communicable diseases and national fitness plan of China for physical activity. Risk Manag Healthc P. 2021;14:2319–2331. doi:10.2147/RMHP.S258660
4. Saqib ZA, Dai J, Menhas R, et al. Physical activity is a medicine for non-communicable diseases: a survey study regarding the perception of physical activity impact on health wellbeing. Risk Manag Healthc P. 2020;13:2949–2962. doi:10.2147/RMHP.S280339
5. Sisay T. Physical inactivity as a pandemic: daily activities and dietary practices. Risk Manag Healthc P. 2021;14:3287–3293. doi:10.2147/RMHP.S317440
6. Zhang J, Chaaban J. The economic cost of physical inactivity in China. Prev Med. 2013;56(1):75–78. doi:10.1016/j.ypmed.2012.11.010
7. Sun S, Li H, Liu G, Zhang J. A critical review of the association between nutrition and health in modern Chinese diet. J Food Nutr Res. 2020;8(7):337–346. doi:10.12691/jfnr-8-7-5
8. Li T, Guan L, Wang X, et al. Relationship between dietary patterns and chronic diseases in rural population: management plays an important role in the link. Front Nutr. 2022;9:866400. doi:10.3389/fnut.2022.866400
9. Talip WA, Steyn NP, Visser M, Charlton KE, Temple N. Development and validation of a knowledge test for health professionals regarding lifestyle modification. Nutrition. 2003;19(9):760–766. doi:10.1016/s0899-9007(03)00101-1
10. Tan XQ. The role of healthy lifestyles in preventing chronic disease among adults. Am J Med Sci. 2022;364(3):309–315. doi:10.1016/j.amjms.2022.04.007
11. World Health Organization. Physical activity; 2022. Available from: https://www.who.int/news-room/fact-sheets/detail/physical-activity.
12. World Health Organization. Healthy diet; 2020. Available from: https://www.who.int/news-room/fact-sheets/detail/healthy-diet.
13. China Daily. National fitness guidance. Available from: http://www.chinadaily.com.cn/a/201807/31/WS5b5fa5fba31031a351e91110.html.
14. Chinese Center for Disease Control and Prevention. Revision and explanation of Chinese Food Guide Pagoda and Plate; 2022. Available from: https://en.chinacdc.cn/health_topics/nutrition_health/202206/t20220622_259773.html.
15. Wu F, Zhang L, Guo W, et al. Evaluation of China healthy lifestyle for all interventions based on RE-AIM framework-China, 2007–2020. China CDC Wkly. 2022;4(19):403–406. doi:10.46234/ccdcw2022.091
16. Zhang M, Ma Y, Xie X, et al. Trends in insufficient physical activity among adults in China 2010–18: a population-based study. Int J Behav Nutr Phy. 2023;20:87. doi:10.1186/s12966-023-01470-w
17. Xi Y, Waiyi LA, Yi Z, Hua ZW. Recent trends in physical activity among Chinese children based on their demographic and social characteristics. Biomed Environ Sci. 2021;34(5):404–409. doi:10.3967/bes2021.054
18. Lyu J, Zhang W, Li W, Wang S, Zhang J. Epidemic of chronic diseases and the related healthy lifestyle interventions in rural areas of Shandong Province, China. BMC Public Health. 2020;20:606. doi:10.1186/s12889-020-08729-y
19. van Dillen SME, van Binsbergen JJ, Koelen MA, Hiddink GJ. Nutrition and physical activity guidance practices in general practice: a critical review. Patient Educ Couns. 2013;90(2):155–169. doi:10.1016/j.pec.2012.10.022
20. Muharib NS, Afifi A, Hakami M. Personal physical activity and physical activity counseling habits among primary care physicians of Prince Sultan Military Medical City, Riyadh city, Saudi Arabia, 2018. Saudi J Sports Med. 2021;21(3):115–126. doi:10.4103/sjsm.sjsm_18_21
21. Fu Y, Wang J, Sun J, Zhang S, Huang D. Equity in the allocation of general practitioner resources in mainland China from 2012 to 2019. Healthc. 2023;11(3):398. doi:10.3390/healthcare11030398
22. Lian S, Chen Q, Yao M, Chi C, Fetters MD. Training pathways to working as a general practitioner in China. Fam Med. 2019;51(3):262–270. doi:10.22454/FamMed.2019.329090
23. Chen S, Sam XH, Soong A, Car LT, Lian S, Smith HE. Recruitment of general practitioners in China: a scoping review of strategies and challenges. BMC Primary Care. 2022;23:249. doi:10.1186/s12875-022-01854-0
24. Podl TR, Goodwin MA, Kikano GE, Stange KC. Direct observation of exercise counseling in community family practice. Am J Prev Med. 1999;17(3):207–210. doi:10.1016/s0749-3797(99)00074-4
25. Eaton CB, Goodwin MA, Stange KC. Direct observation of nutrition counseling in community family practice. Am J Prev Med. 2002;23(3):174–179. doi:10.1016/s0749-3797(02)00494-4
26. Lin X, Li X, Bai Y, Liu Q, Xiang W. Death-coping self-efficacy and its influencing factors among Chinese nurses: a cross-sectional study. PLoS One. 2022;17(9):e0274540. doi:10.1371/journal.pone.0274540
27. Abramson S, Stein J, Schaufele M, Frates E, Rogan S. Personal exercise habits and counseling practices of primary care physicians: a national survey. Clin J Sport Med. 2000;10(1):40–48. doi:10.1097/00042752-200001000-00008
28. Livaudais JC, Kaplan CP, Haas JS, Pérez-Stable EJ, Stewart S, Jarlais GD. Lifestyle behavior counseling for women patients among a sample of California physicians. J Womens Health. 2005;14(6):485–495. doi:10.1089/jwh.2005.14.485
29. Harkin N, Johnston E, Mathews T, et al. Physicians’ dietary knowledge, attitudes, and counseling practices: the experience of a single health care center at changing the landscape for dietary education. Am J Lifestyle Med. 2019;13(3):292–300. doi:10.1177/1559827618809934
30. Kushner RF. Barriers to providing nutrition counseling by physicians: a survey of primary care practitioners. Prev Med. 1995;24(6):546–552. doi:10.1006/pmed.1995.1087
31. Hébert ET, Caughy MO, Shuval K. Primary care providers’ perceptions of physical activity counselling in a clinical setting: a systematic review. Br J Sports Med. 2012;46:625–631. doi:10.1136/bjsports-2011-090734
32. Hølund U, Boysen G, Charles P, et al. Attitude of general practitioners to the importance of gender and diet in disease prevention. Ugeskr Laeg. 1999;161(1):40–43. PMID:9922687.
33. Mechanic D, McAlpine DD, Rosenthal M. Are patients’ office visits with physicians getting shorter? N Engl J Med. 2001;344:198–204. doi:10.1056/nejm200101183440307
34. Tsui JI, Dodson K, Jacobson TA. Cardiovascular disease prevention counseling in residency: resident and attending physician attitudes and practices. J Natl Med Assoc. 2004;96(8):
35. Kolasa KM, Rickett K. Barriers to providing nutrition counseling cited by physicians. Nutr Clin Pract. 2010;25(5):502–509. doi:10.1177/0884533610380057
36. Solmundson K, Koehle M, McKenzie D. Are we adequately preparing the next generation of physicians to prescribe exercise as prevention and treatment? Residents express the desire for more training in exercise prescription. Can Med Educ J. 2016;7(2):e79–e96. PMID:28344695. doi:10.36834/cmej.36702
37. Howe M, Leidel A, Krishnan SM, Weber A, Rubenfire M, Jackson EA. Patient-related diet and exercise counseling: do providers’ own lifestyle habits matter? Prev Cardiol. 2010;13(4):180–185. doi:10.1111/j.1751-7141.2010.00079.x
38. Lobelo F, de Quevedo IG. The evidence in support of physicians and health care providers as physical activity role models. Am J Lifestyle Med. 2016;10(1):36–52. doi:10.1177/1559827613520120
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.