Back to Journals » Risk Management and Healthcare Policy » Volume 16
Nosocomial Omicron Outbreak in a Medical Ward During the Coronavirus Disease 2019 Pandemic
Authors Lu TL, Chuang Y, Huang C
Received 7 December 2022
Accepted for publication 18 February 2023
Published 28 February 2023 Volume 2023:16 Pages 309—315
DOI https://doi.org/10.2147/RMHP.S398668
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jongwha Chang
Tsung-Lung Lu,1 Yiling Chuang,1 Chienhsiu Huang2
1Department of Nursing, Dalin Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, Chiayi County, Taiwan; 2Department of Internal Medicine, Dalin Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, Chiayi County, Taiwan
Correspondence: Chienhsiu Huang, Department of Internal Medicine, Dalin Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, NO. 2, Min-Sheng Road, Dalin Town, Chiayi County, Taiwan, Email [email protected]; [email protected]
Background: The Omicron variant of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is 2 to 3 times more contagious than the Delta variant and poses a new challenge in containing transmission in community and health care settings. Transmission in hospitals can cause nosocomial outbreak infections and affect patients and health care workers. This study describes a coronavirus disease 2019 (COVID-19) outbreak in a medical ward. The purpose of the investigation was to determine the transmission source of the outbreak, as well as the measures implemented to prevent and control it.
Methods: A cluster of SARS-CoV-2 infections that affected health care workers, inpatients, and caregivers was thoroughly researched in a medical ward. There were several strict outbreak measures implemented in our hospital, and these measures controlled the nosocomial COVID-19 outbreak in this study.
Results: Seven cases of SARS-CoV-2 infection were diagnosed within 2 days in the medical ward. The infection control team declared a nosocomial outbreak of the COVID-19 Omicron variant. Several strict outbreak measures were implemented as follows: 1. The medical ward was closed and cleaning and disinfection were performed. 2. All patients and caregivers with negative test results were transferred to a spare COVID-19 isolation ward. 3. Relatives’ visits were not allowed, and no new patient was admitted during the outbreak period. 4. Health care workers were retrained on wearing personal protective equipment and enhanced techniques and practices of hand hygiene, social distancing, and self-monitoring of fever and respiratory symptoms.
Conclusion: This outbreak occurred in a non-COVID-19 ward during the COVID-19 Omicron variant phase of the pandemic. Our strict outbreak measures halted and contained the nosocomial COVID-19 outbreak in 10 days. Future studies are needed to establish a standard policy of COVID-19 outbreak measure implementation.
Keywords: SARS-CoV-2, COVID-19, nosocomial outbreak, medical ward, Omicron variant
Introduction
Since the first coronavirus disease 2019 (COVID-19) cases were reported in China in 2019, there have been 630 million COVID-19 cases and 6.59 million deaths worldwide as of October 2022, and the overall mortality is approximately 1%.1 The clinical characteristics of the COVID-19 pandemic are being impacted by the emergence of SARS-CoV-2 variants with spike protein mutations. These variants could make it easier for viruses to spread and reduce the protection afforded by neutralizing monoclonal antibodies and vaccination. In comparison to the SARS-CoV-2 alpha strain, the delta variant, designated B.1.617.2, includes 23 mutations. The T19R, L452R, T478K, D614G, P681R, and d960N mutations in the spike gene, along with deletions at locations 157 and 158, are present in this B.1.617.2 variation.2 Three SARS-CoV-2 Omicron Subvariants BQ.1.1, BA.5, and BF.7 each have a unique neutralizing antibody escape as follows: 1.BQ.1.1 subvariants are primarily driven by the N460K mutation, with R346T and K444T mutations playing a less significant role; 2.BA.5 reverse two mutations back to the original virus, Orf6 D61 and NSP4 L438, which replicate the virus by negative regulation of proteins, enzymes and various other signals; 3.BF.7 underwent by its signature F486S mutation. and a reduction by the D1199N mutation to its fusogenicity and S processing, resulting in minimal overall change.3,4 In November 2021, the Omicron variant was first detected in South Africa; this variant is highly transmissible and rapidly spread worldwide. However, the Omicron variant is 2 to 3 times more contagious than the Delta variant and has reduced clinical severity.
In January 2022, the first domestic Omicron case in Taiwan was confirmed. Then, the Central Epidemic Command Center (CECC) adjusted the management measures for visitation control and screening strategies for patients, caregivers, and health care workers (HCWs), which was a new challenge in containing transmission in community and health care settings.5 Furthermore, transmission in hospitals can cause nosocomial outbreak infections, affect vulnerable patients, and suspend the HCW workforce.
In Taiwan, there were 547,054 new confirmed cases from May 15, 2022, to May 21, 2022, and 561,194 new confirmed cases from May 22, 2022, to May 28, 2022. The variant was mostly an Omicron variant. During the period from May 19 to May 28, 2022, we experienced a nosocomial outbreak among patients, caregivers and HCWs caused by the COVID-19 Omicron variant in a medical ward of a tertiary teaching hospital in Taiwan. Hospital policies intended to prevent nosocomial transmission episodes must take into account infection dynamics. This study describes a COVID-19 outbreak, and the purpose of the investigation was to determine the transmission source of the outbreak, as well as the measures implemented to prevent and control it.
Methods
Hospital Overview and Study Setting
This study was conducted from May 19 to May 28, 2022, at Dalin Tzu Chi Hospital in Taiwan. A cluster of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infections that affected HCWs, inpatients, and caregivers was thoroughly researched in a medical ward.
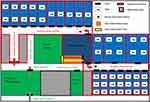
A teaching hospital at the tertiary level, Dalin Tzu Chi Hospital has 59 beds in the intensive care unit and 600 beds for acute care. In Taiwan’s Chiayi County, there are two COVID-19 screening and treatment hospitals. One of the two COVID-19 screening and treatment hospitals is our hospital. During the Omicron phase of the pandemic, we set up two COVID-19 isolation wards (ward 12B and ward 6B) with 92 COVID-19 general isolation beds. The COVID-19 isolation ward consisted of 22 rooms with ventilation fan which can generate negative pressure in patient rooms: two rooms for four patients, seven rooms for three patients, six rooms for two patients, and five single-patient rooms. The priority COVID-19 inpatient ward was 12B, and the spare COVID-19 inpatient ward was 6B. There was one point of entry to the COVID-19 isolation ward. The floor plan of the COVID-19 isolation ward is shown in Figure 1.
Our hospital offers outpatient and inpatient medical care for both general patients and COVID-19 patients. During the Omicron epidemic, our hospital provided telemedicine services to individuals under home quarantine. The following strategies were implemented to stop the spread of COVID-19 in our hospital prior to the outbreak: (1) Only two access doors to the hospital buildings, including the entrance door to the emergency room, were left open. (2) Throughout the day, just one car entrance was open. (3) A thermal infrared camera was used to measure the body temperatures of visitors to the hospital which were monitored by HCWs. Thermal sensitivity is less than 0.04°C. For spot measurements, the target is specified as the center of the forehead. The thermal infrared camera is set to a temperature of 38°C. All the febrile hospital visitors were transferred to the emergency room for further evaluation and management. (4) The use of surgical masks was required for everyone entering the hospital, and everyone’s hands had to be washed with 75% alcohol for hand hygiene. (5) The number and time of inpatient caregivers and visitors were restricted.
Definitions
Individuals with a positive polymerase chain reaction (PCR) test for SARS-CoV-2 from a nasopharyngeal swab sample were referred to as confirmed cases. Samples were processed and examined in our hospital’s microbiology laboratory. A cluster was a group of more than two cases that were epidemiologically linked, such as patients who shared a ward.
Outbreak Measure Implementation
There was an outbreak of COVID-19 in the medical ward on May 19, 2022. The implementation of preventive measures included the following: 1. Repeated PCR testing for SARS-CoV-2 and nasopharyngeal swab COVID-19 antigen (Ag) rapid testing (Abbott Rapid Diagnostics Jena GmbH) of patients, caregivers, and HCWs linked to the ward; 2. Training of HCWs on infection control and prevention measures; 3. Cleaning and disinfection of the COVID-19 isolation ward with 10% NaClO solution at least three times daily; 4. No relatives’ visits; 5. No new patient admission during the outbreak period; 6. Caregivers and HCWs who tested positive by PCR were quarantined at home depending upon the severity of COVID-19 infection; 7. Inpatients with positive PCR tests were transferred to priority COVID-19 isolation wards (12B); and 8. Closure of the affected ward and transfer of all negative PCR inpatients and caregivers to the spare COVID-19 isolation ward (6B).
Results
According to CECC strategies, all patients and caregivers had negative PCR tests for SARS-CoV-2 at the time of admission. On May 19, 2022, in the medical ward, a caregiver had fever and sore throat, the nasopharyngeal swab COVID-19 Ag rapid test was positive, and the SARS-CoV-2 PCR test confirmed that the caregiver had SARS-CoV-2 infection (Case 1). On the same day, nasopharyngeal swab PCR tests for SARS-CoV-2 were performed for 29 people, including patients, caregivers, cleaners, nurses, doctors, and other HCWs who were associated with the same room. One nurse, one student nurse, and one caregiver tested positive by PCR for SARS-CoV-2, and they were quarantined at home for seven days (Cases 2, 3, and 4).
The next day, screening SARS-CoV-2 PCR tests for all inpatients, caregivers, and HCWs who were associated with the medical ward were performed in the morning. One patient (Case 5) and two caregivers (Cases 6 and 7) had positive PCR test results for SARS-CoV-2. In the afternoon, the infection control team convened an epidemic prevention meeting and declared a nosocomial outbreak of the COVID-19. First, we closed the medical ward and initiated cleaning and disinfection. Second, to prevent incubation period transmission of asymptomatic and negative individuals, all patients and caregivers with negative test results were transferred to a spare COVID-19 isolation ward. Seven days of quarantine and isolation were initiated. Patients and caregivers had to wear surgical masks in the COVID-19 isolation ward all day except when eating. Visits by relatives were not allowed, and no new patient was admitted during the outbreak period. To prevent caregivers from contracting SARS-CoV-2 in the community, all civilian goods and three meals a day were supplied by the hospital. HCWs were retrained on wearing personal protective equipment (PPE), including an N95 mask, disposable cap, face shield, isolation gown, and gloves, enhanced techniques and practices of hand hygiene, cleaning and decontamination, social distancing, and self-monitoring of fever and respiratory symptoms. If an HCW had a positive PCR test for SARS-CoV-2, the HCW was suspended and quarantined at home for seven days until symptoms were alleviated and a negative PCR test for SARS-CoV-2 was obtained. Before entering the nurses’ station, HCWs had to don an N95 mask and disposable cap. Before entering the COVID-19 isolation ward, HCWs had to don N95 masks, disposable caps, face shields, isolation gowns, gloves, etc. Before leaving the COVID-19 isolation ward, HCWs had to clean their shoes and doff the face shield, isolation gown and gloves. HCWs were expected to dine in dedicated eating spaces (meeting room), seated at least 2 meters apart at tables with impermeable plastic partitions. HCWs were also encouraged not to attend social gatherings and to dine together after leaving work.
Seven days were devoted to the screening of all patients, caregivers, and HCWs. We performed nasopharyngeal swab PCR tests for SARS-CoV-2 on the 1st, 4th, and 7th days and nasopharyngeal Ag rapid testing on the 2nd, 3rd, 5th, and 6th days. Finally, on May 28, the nasopharyngeal PCR test results of all patients, caregivers, and HCWs were negative. There were no cases of severe infection or mortality. Quarantine and isolation were unnecessary. All patients and caregivers were transferred back to the medical ward for further therapy. The nosocomial outbreak was halted and contained in 10 days.
Discussion
The increase in the number of Omicron variant cases is a global issue. The literature has reported hospital COVID-19 outbreaks in different countries. It is difficult to prevent nosocomial outbreaks with the rapid spread of the COVID-19 Omicron variant in clinical situations, although many robust control and prevention transmission measures were practiced for the COVID-19 outbreak. The incubation period for COVID-19 lasts between 1 and 14 days.6 The estimated median incubation duration is approximately 5 days.7,8 Asymptomatic transmission of COVID-19 has also been documented.9–11 Therefore, on the day of admission, most hospitals perform universal SARS-CoV-2 PCR screening for inpatients and caregivers; the incubation period may have contributed to the negative results in our study. Notably, a negative SARS-CoV-2 PCR test at the time of admission and careful monitoring during the admission period are needed.
There was a nosocomial outbreak in a 16-room hematology ward in Korea. The outbreak occurred in a multipatient room with a shared bathroom. Six inpatients and three patient caregivers were infected. An airflow simulation demonstrated that the outbreak was triggered by presymptomatic transmission and facilitated by possible aerosol transmission from a shared bathroom to an adjacent room. The outbreak was controlled in 12 days in the study.12 In India, a nosocomial outbreak in an overwhelmed and overcrowded trauma ward was described. The team misplaced the first index positive result for 3 days. Twenty-five patients and 9 HCWs were infected, and there were no deaths. Most cases were identified around the corridor. The outbreak was controlled in 25 days in the study.13 A nosocomial outbreak in a medical ward in the United Kingdom was reported, and six patients and 23 HCWs were infected. Nine HCWs had direct exposure to the index patient who was possibly preinfected with SARS-CoV-2 within 3 days before admission. Three HCWs reported caring for patients without the use of proper PPE and close contact between HCWs while working and resting at a crowded main ward desk and in small break rooms. The outbreak was controlled within 38 days in the study.14 Another nosocomial outbreak occurred in a university hospital in Korea, where 2924 individuals were tested following 14 health care-associated COVID-19 cases. The hospital was closed for two weeks with inpatient isolation. The positivity rate was 0.1%, and no more HCWs contracted the illness. The outbreak was controlled in 17 days in the study.15 In Japan, there was a nosocomial outbreak in two general wards. Forty-two individual (30 HCWs and 12 patients) infections were confirmed. Among HCWs, transmission was thought to be associated with the use of a small break room and conference room without the use of masks. The outbreak was controlled within 27 days in the study.16 Another nosocomial outbreak caused by the Omicron variant occurred in the head and neck surgery ward. Fourteen patients and 12 HCWs were infected. Droplet and contact transmission may have been caused by sputum suction without proper PPE. The outbreak was controlled in 19 days in the study.17 It is crucial that hospitals establish efficient infection prevention and control measures to prevent further transmission, including cohort isolation, detailed evaluation of close contacts, universal screening, use of proper PPE, hand hygiene, social distancing, cleaning, and disinfection of the ward environment, etc. It is essential to break the transmission chain to terminate a nosocomial outbreak.
The impact of nosocomial outbreaks can be detrimental to vulnerable and comorbid inpatients, and mortality may be linked to advanced age and comorbidities. In Spain, a COVID-19 nosocomial outbreak occurred in a hematology ward with twenty-two COVID-19 cases (12 HCWs and 10 inpatients). Five inpatients presented moderate to serious disease and died, and one HCW required ICU admission. Measures controlled the outbreak in 33 days in that study.18 Another nephrology ward experienced 10 inpatient and five HCW infections, and five inpatients died. Positive individuals were moved to an isolation ward for COVID-19. Furthermore, a 14-day quarantine was implemented in the nephrology ward and enhanced twice-weekly infection control, disinfection, and cleaning training for all HCWs were performed. The outbreak was contained in 2 weeks.19 A COVID-19 outbreak in a gastrointestinal ward involved 15 patients and 3 HCWs. COVID-19 caused the deaths of four inpatients. The sequencing of the whole genomes of 12 patient strains and 1 HCW strain revealed an unexpected degree of complexity. Five different strains of SARS-CoV-2 were found. The outbreak was controlled in 27 days in the study.20 In France, a 40-bed geriatric ward reported COVID-19 nosocomial infections; 36 patients and 31 HCWs were infected, and 12 patients died. The ward was separated into COVID-19 and non-COVID-19 areas, and there were no more multipatient rooms. Both patients and HCWs underwent screening every five days. The outbreak was controlled in 62 days in the study.21 Fortunately, we succeeded in preventing further transmission and infection among other patients, caregivers, HCWs and hospital units. There were no cases of severe infection or mortality in our medical ward outbreak. This finding may be related to full vaccination, early detection, quarantine and isolation, HCW retraining and enhanced skills in the specific treatment and care of COVID-19 patients. On May 28, the PCR tests were negative for all inpatients, caregivers and HCWs. The nosocomial outbreak was halted and contained in 10 days, and there was no further nosocomial outbreak for 2 months. There were three important outbreak measures that were different among outbreak measures in the literature. 1. We transferred all negative SARS-CoV-2 inpatients and caregivers to the spare COVID-19 isolation ward for 7 days of strict isolation. We provided SARS-CoV-2-free areas for patients, caregivers and HCWs. 2. To prevent caregivers from contracting SARS-CoV-2 in the community, all caregivers were also quarantined for 7 days. We blocked all possible pathways of new SARS-CoV-2 infection. 3. All HCWs closely monitored their health and watched for new SARS-CoV-2 symptoms. Therefore, these measures controlled the outbreak in only 10 days in this study.
Limitations
This report had several limitations. First, statistical analysis was not performed due to the small sample size. We did not obtain genotype data or perform airflow simulations due to equipment limitations. Despite these limitations, our unique experience regarding the control of the outbreak may provide crucial information that could be useful to other health care facilities.
Conclusions
This outbreak occurred in a non-COVID-19 ward during the COVID-19 Omicron variant phase of the pandemic. This outbreak’s source of transmission was caregiver who became infected with SARS-CoV-2 in the community. Our strict implementation of outbreak measures halted and contained the nosocomial COVID-19 outbreak quickly. The implementation of outbreak measures and screening policies has varied in different countries, and the cost-effectiveness is unknown. Future studies are needed to establish a standard policy for COVID-19 outbreak measure implementation. We hope our experience will improve measures and reduce the risk of nosocomial COVID-19 outbreaks.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Research Ethics
This COVID-9 outbreak report included only the total number COVID-19 cases, as well as the measures implemented during the outbreak. We did not collect the detailed disease course of all COVID-19 cases in this study. Ethics approval was not necessary.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
There was no funding for this study.
Disclosure
The authors declare that they have no competing interests in this work.
References
1. World Health Organization. WHO Coronavirus (COVID-19) dashboard; 2022. Available from: https://covid19.who.int/table.
2. Wolter N, Jassat W, Walaza S, et al. Clinical severity of SARS-CoV-2 Omicron BA.4 and BA.5 lineages compared to BA.1 and Delta in South Africa. Nat Commun. 2022;13:5860. doi:10.1038/s41467-022-33614-0
3. Shiehzadegan S, Alaghemand N, Fox M, Venketaraman V. Analysis of the Delta Variant B.1.617.2 COVID-19. Clin Pract. 2021;11:778–784. doi:10.3390/clinpract11040093
4. Qu P, Evans JP, Faraone J, et al. Distinct neutralizing antibody escape of SARS-CoV-2 Omicron subvariants BQ.1, BQ.1.1, BA.4.6, BF.7 and BA.2.75.2. bioRxiv. 2022. doi:10.1101/2022.10.19.512891
5. Taiwan Centers for Disease Control. Starting today, CECC to adjust management measures for visitors, caregivers, and healthcare personnel in hospitals in response to new confirmed domestic Omicron cases; 2022. Available from: https://www.cdc.gov.tw/En/Category/ListContent/tov1jahKUv8RGSbvmzLwFg?uaid=9uDRucmQ-uRX43gHXj8cDA.
6. Lauer SA, Grantz KH, Bi Q, et al. The incubation period of Coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann Intern Med. 2020;172:577–582. doi:10.7326/M20-0504
7. Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382:1199–1207. doi:10.1056/NEJMoa2001316
8. Verity R, Okell LC, Dorigatti I, et al. Estimates of the severity of coronavirus disease 2019: a model-based analysis. Lancet Infect Dis. 2020;20:669–677. doi:10.1016/S1473-3099(20)30243-7
9. Mizumoto K, Kagaya K, Zarebski A, Chowell G. Estimating the asymptomatic proportion of coronavirus disease 2019 (COVID-19) cases on board the Diamond Princess cruise ship, Yokohama, Japan, 2020. Euro Surveill. 2020;25:2000180. doi:10.2807/1560-7917.ES.2020.25.10.2000180
10. Hu Z, Song C, Xu C, et al. Clinical characteristics of 24 asymptomatic infections with COVID-19 screened among close contacts in Nanjing, China. Sci China Life Sci. 2020;63:706–711. doi:10.1007/s11427-020-1661-4
11. Tong Z-D, Tang A, Li K-F, et al. Potential presymptomatic transmission of SARS-CoV-2, Zhejiang Province, China, 2020. Emerg Infect Dis. 2020;26:1052–1054. doi:10.3201/eid2605.200198
12. Jung J, Lee J, Jo S, et al. Nosocomial outbreak of COVID-19 in a hematologic ward. Infect Chemother. 2021;53:332–341. doi:10.3947/ic.2021.0046
13. Rana K, Sharma B, Lakshmi PVM, et al. Nosocomial outbreak of SARS-CoV-2 in a non-COVID zone of a tertiary care hospital of North India: need to upgrade infection control practices. J Prim Care Community Health. 2021;12:21501327211050753. doi:10.1177/21501327211050753
14. Asad H, Johnston C, Blyth I, et al. Health care workers and patients as Trojan Horses: a COVID19 ward outbreak. Infect Prev Pract. 2020;2:100073. doi:10.1016/j.infpip.2020.100073
15. Kim SW, Jo SJ, Lee H, et al. Containment of a healthcare-associated COVID-19 outbreak in a university hospital in Seoul, Korea: a single-center experience. PLoS One. 2020;15:e0237692. doi:10.1371/journal.pone.0237692
16. Sakamoto N, Ota M, Takeda T, et al. Nosocomial outbreak of coronavirus disease in two general wards during the initial wave of the pandemic in 2020, Tokyo, Japan. Western Pac Surveill Response J. 2022;13:1–5. doi:10.5365/wpsar.2022.13.1.906
17. Itoh N, Akazawa N, Ishikane M, et al. Lessons learned from an outbreak of COVID-19 in the head and neck surgery ward of a Japanese cancer center during the sixth wave by Omicron. J Infect Chemother. 2022;28:1610–1615. doi:10.1016/j.jiac.2022.08.010
18. Bestilleiro RS, Señaris DM, Rodríguez MJP, et al. Nosocomial infection outbreak due to SARS-COV-2 in a hospital unit of particularly vulnerable patients. Int J Med Sci. 2021;2118:2146–2154. doi:10.7150/ijms.53270
19. Montero MM, Hidalgo López C, López Montesinos I, et al. Impact of a nosocomial COVID-19 outbreak on a non-COVID-19 nephrology ward during the first wave of the pandemic in Spain. Antibiotics. 2021;10:619. doi:10.3390/antibiotics10060619
20. Pérez-Lago L, Martínez-Lozano H, Pajares-Díaz JA, et al. Overlapping of independent SARS-CoV-2 nosocomial transmissions in a complex outbreak. mSphere. 2021;6:e0038921. doi:10.1128/mSphere.00389-21
21. Cormier H, Brangier A, Lefeuvre C, Asfar M, Annweiler C, Legeay C. Lessons learnt from a nosocomial COVID-19 outbreak in a geriatric acute care ward with a high attack rate. Maturitas. 2021;149:34–36. doi:10.1016/j.maturitas.2021.05.001
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.